Abstract
Gout is a metabolic disease that occurs either because of increased uric acid production or decreased uric acid secretion. It most commonly affects middle-aged to elderly men and postmenopausal women. Chronic tophaceous gout frequently occurs after 10 years or more of recurrent polyarticular gout. Gouty tophi are deposition of monosodium urate (MSU) crystals in and around joints as well as soft tissues. We present a case of chronic tophaceous gout in a 21-year-old male, which occurred after 4 years of onset of gouty arthritis. The patient presented with tophaceous gout in four forms, that is, periarticular subcutaneous tophi, disseminated intradermal tophi, ulcerative form, and miliarial tophi along with multiple sinuses discharging chalky white material. The case was diagnosed as chronic tophaceous gout on the basis of raised serum uric acid, imprint smear showing needle-shaped crystals and negatively birefringent crystals on polarized microscopy. The case is interesting for varied morphological forms of tophaceous gout in a patient at an early age and shorter interval between onset of gouty arthritis and tophaceous gout.
Keywords: Atypical, gouty arthritis, miliarial tophi, sinus, tophaceous gout, ulcer
Introduction
Gout is a metabolic disease that can manifest as acute or chronic arthritis. There occurs deposition of monosodium urate (MSU) crystals in joints, bones, and different body tissues, including the skin and soft tissues. Gouty tophi are deposition of MSU crystals in and around joints as well as soft tissues. They commonly appear as firm, pink nodules or fusiform swellings.[1,2] We are reporting a case of chronic tophaceous gout which presented with multiple yellowish-red subcutaneous swellings and nodules over periarticular areas, along with miliary nodules over nonarticular areas and oral mucosa and multiple sinuses, ulcers discharging chalky white material.
Case Report
A 21-year-old male patient presented to the dermatology outpatient department with painful red, swollen large joints, small joints along with multiple painful subcutaneous swellings discharging chalky white material over wrist area and extremities. Joint pain and swelling had started since 3 years, initially involving large joints such as elbow, knee, ankle followed by metatarsophalangeal (MTP) and metacarpophalangeal (MCP) joints. Skin involvement occurred since last 6 months. The patient was taking on and off oral prednisolone dose ranging from 10 to 30 mg on daily basis for joint pain since three years without improvement. There was no history of any neuropsychiatric problems and renal symptoms.
Dermatological examination revealed multiple yellowish-white tender swellings and nodules around bilateral wrist, hip, elbow, MCP and proximal interphalangeal (PIP) joints, dorsum of right foot, tips of fingers and toes [Figure 1a-d]. There were multiple sinuses and ulcers present over wrists, buttocks, and dorsum of foot discharging whitish toothpaste-like material [Figure 2a-d]. Musculoskeletal examination revealed swelling, erythema, and tenderness over both knees, elbows, wrists, ankles, MTP and MCP joints.
Figure 1.

(a) Subcutaneous swellings and nodules around the bilateral wrist and metacarpophalangeal and proximal interphalangeal (PIP) joints. (b) Miliary nodules on palm and tip of fingers. (c) Subcutaneous nodules around hip joint. (d) Subcutaneous nodules around elbow joint
Figure 2.

(a) Ulcer discharging chalky white material. (b) Ulcers on buttocks. (c) Sinus discharging chalky white material on the dorsum of hand. (d) Multiple sinuses on the dorsum of foot
On the basis of history and examination, rheumatoid arthritis with calcinosis cutis and gouty arthritis with tophi were kept as differential diagnosis and the patient was subjected to further investigation.
Complete blood count (Hb = 12.4 g/dl, TLC = 5500/μl, total platelets = 3 lacs/μl), liver function tests (SGOT = 26U/L, SGPT = 36U/L, ALP = 62U/L, Albumin = 3.5 g/dl, total bilirubin = 0.8 mg/dl), kidney function tests (serum creatinine = 0.8 mg/dl, urea = 16 mg/dl) were normal. Serum calcium (9 mg/dl) and parathyroid (PTH) levels (26 pg/ml, normal range = 10–65 pg/ml) were within normal limits. Rheumatoid factor was weakly positive but anti-cyclic citrullinated peptide (anti-CCP) came negative. Serum uric acid was 16.2 mg/dl. X-ray of the bilateral foot showed destruction of bilateral MTP joints and first IP joint of right foot. There were multiple juxta-articular joint erosions with sclerosis and overhanging margin [Figure 3]. Imprint smear from the discharging toothpaste-like material and fine-needle aspiration cytology from subcutaneous swellings revealed needle-shaped crystals in hematoxylin and eosin (H and E) stain [Figure 4a]. Von Kossa stain was negative for calcium. Negatively birefringent needle-shaped crystals were seen in polarizing microscopy [Figure 4b]. Ultrasonography of of abdomen and pelvis was normal. On the basis of clinical findings, biochemical results, radiological, cytological and polarized microscopic findings, a diagnosis of chronic tophaceous gout with extensive subcutaneous tophi was made. Indomethacin 75 mg twice a day and Allopurinol at 200 mg/day were added in the prescription. Prednisolone was tapered to 5 mg. After 10 days of intake of 200 mg of allopurinol serum uric acid came down to 7.6 mg/dl along with improvement in joint pain. The patient was lost to follow-up subsequently.
Figure 3.

X-ray of the bilateral foot: destruction of bilateral metatarsophalangeal (MTP) joints and first IP joint of right foot with multiple juxta-articular joint erosions, sclerosis, and overhanging margin
Figure 4.
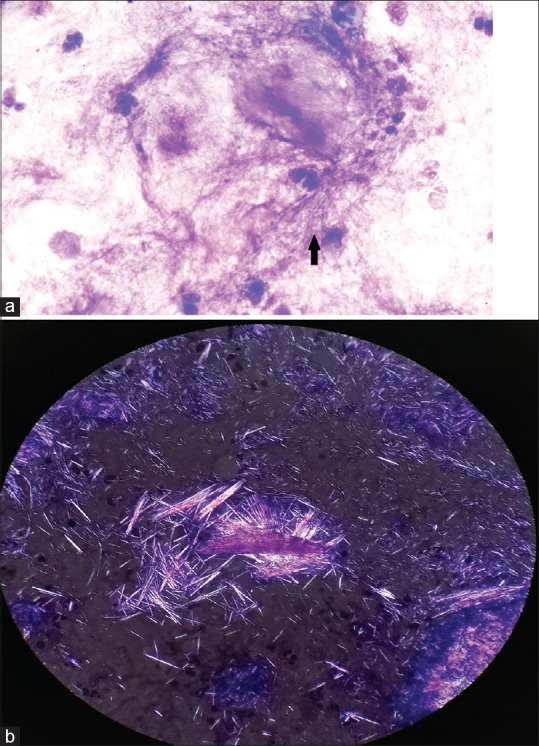
(a) 100X, hematoxylin and eosin (H and E) stain: Imprint smear showing needle-shaped crystals. (b) Negatively birefringent crystals in polarized microscopy
Discussion
Gout is a common systemic disorder caused due to abnormal uric acid metabolism. The uric acid crystallizes and gets deposited in the joints resulting in recurrent arthritis. Older age, male sex, postmenopausal women, and black race are at higher risk of developing gout.[3] Untreated gouty arthritis can result in intradermal and subcutaneous deposition of MSU crystals in the skin usually over joints or on the ears resulting in chronic cutaneous tophaceous gout. Various forms of chronic tophaceous gout have been described: classic periarticular subcutaneous tophi, disseminated intradermal tophi, an ulcerative form, and gouty panniculitis.[4] Miliarial gout is an extremely rare form of tophaceous gout which manifests as ''milia-like'' widely distributed papules containing white to cream-colored material on an erythematous base.[4,5] Our case had four forms, that is, periarticular subcutaneous tophi, disseminated intradermal tophi, ulcerative form, and miliarial tophi. “Chronic tophaceous gout frequently occurs after 10 years or more of recurrent polyarticular gout with tophi.”[6] In our case, history was quite short with extensive tophi in skin occurring within 3–4 years of onset of arthritis. Kim et al. reported disseminated miliarial gout in a 34-year-old male, which occurred 4 years after onset of gouty arthritis.[7] Jung et al. reported a case of disseminated gout in the form of nodules that appeared after 10 years of gouty arthritis.[8] Aguayo et al. described an unusual unilateral presentation of miliarial cutaneous gout in a 51-year-old male patient with chronic joint disease.[5] However, in the above mentioned cases, except miliarial tophi and subcutaneous nodules, other forms such as ulcers, sinuses, and subcutaneous swellings were absent like the current case. Triggering factors to the development of intradermal gout include renal insufficiency, hypertension, chronic diuretic therapy, long duration of disease and lack of consistent use of urate-lowering therapy, and intake of corticosteroids.[5,6,7,8,9] In the present case, delay in initiation of urate-lowering therapy and prolonged intake of oral prednisolone were risk factors for miliarial and disseminated cutaneous gout.
Diagnosis of cutaneous gout can be done by seeing amorphous crystalline material in histopathology and negatively birefringent needle-like crystals in polarized microscopy. Gouty arthritis is diagnosed based upon raised serum uric acid and X-ray findings, first MTP involvement, juxta-articular erosions with sclerotic margins and overhanging edges and relative preservation of joint spaces in early stage of the disease.[9] In our case, there was destruction of bilateral MTP joints and first IP joint of right foot along with multiple juxta-articular joint erosions, sclerosis, and overhanging margin.
Gouty arthritis involving large joints can be confused with rheumatoid arthritis and tophi with calcinosis cutis. However, both entities can be differentiated by serological, biochemical, and radiological investigations. In our patient, rheumatoid arthritis with calcinosis cutis was ruled out due to normal serum calcium and PTH levels along with negative anti-CCP and von Kossa stain. The diagnosis of gouty arthritis was made basing upon raised serum uric acid and X-ray findings and tophaceous gout was diagnosed by imprint smear showing needle-shaped crystals and negatively birefringent crystals in polarizing microscopy.
The treatment of chronic gout aims to prevent gout progression, gout flares, to eliminate any urate deposits, and to reverse tophus formation. Urate-lowering agents are cornerstones in the management of chronic gout. Xanthine oxidase inhibitors are the first-line treatment followed by uricosuric agents as second-line options. The leading xanthine oxidase inhibitor and uricosuric agents are allopurinol and probenecid, respectively.[10] In addition, there have been reports of good response of military tophi to allopurinol.[4] In our case, allopurinol was prescribed as urate-lowering agent along with nonsteroidal anti-inflammatory drugs (indomethacin) to control joint inflammation and pain. We are reporting the case for its extensive cutaneous involvement at an early age with short duration of gouty arthritis, atypical cutaneous presentation in the form of multiple sinuses, ulcers as well as miliarial tophi in the skin and oral mucosa in addition to the periarticular subcutaneous nodules and swellings.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Fam AG, Assad D. Intradermal urate tophi. J Rheumatol. 1997;24:1126–31. Schumacher HR Jr, Becker MA, Palo WA, Striet J, MacDonald PA, Josef-Ridge N Tophaceous gout: Quantitative evaluation by direct physical measurement J Rheumatol 2005;32:2368-72. [PubMed] [Google Scholar]
- 2.Li EK. Gout: A review of its aetiology and treatment. Hong Kong Med J. 2004;10:261–70. [PubMed] [Google Scholar]
- 3.Shukla R, Vender RB, Alhabeeb A, Salama S, Murphy F. Miliarial gout (a new entity) J Cutan Med Surg. 2007;11:31–4. doi: 10.2310/7750.2007.00002. [DOI] [PubMed] [Google Scholar]
- 4.Aguayo RS, Baradad M, Soria X, Abal L, Sanmartín V, Egido R, et al. Unilateral milia-type intradermal tophi associated with underlying urate subcutaneous deposition: An uncommon cutaneous presentation of gout. Clin Exp Dermatol. 2013;38:622–5. doi: 10.1111/ced.12084. [DOI] [PubMed] [Google Scholar]
- 5.Wortmann RL, Kelley WN. Gout and hyperuricemia. In: Harris ED, Budd RC, Genovese MC, Firestein GS, Sargent JS, Sledge CB, editors. Kelley's Textbook of Rheumatology. 7th ed. Philadelphia, Pennsylvania, USA: Elsevier Saunders; 2005. pp. 1402–29. [Google Scholar]
- 6.Iacobellis G. A rare and asymptomatic case of mitral valve tophus associated with severe gouty tophaceous arthritis. J Endocrinol Invest. 2004;27:965–6. doi: 10.1007/BF03347542. [DOI] [PubMed] [Google Scholar]
- 7.Kim M, Lee SI, Cheon YH. Unusual milia-type intradermal tophi in a patient with gout? Korean J Intern Med. 2018:31. doi: 10.3904/kjim.2018.352. doi: 10.3904/kjim. 2018.352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jung HY, Yu DS, Kim JW, Jang ED. Disseminated cutaneous gout: A rare clinical presentation. Indian J Dermatol Venereol Leprol. 2016;82:204–5. doi: 10.4103/0378-6323.164220. [DOI] [PubMed] [Google Scholar]
- 9.Girish G, Melville DM, Kaeley GS, Brandon CJ, Goyal JR, Jacobson JA, et al. Imaging appearances in gout. Arthritis. 2013;2013:673401. doi: 10.1155/2013/673401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Engel B, Just J, Bleckwenn M, Weckbecker K. Treatment options for gout. Dtsch Arztebl Int. 2017;114:215–22. doi: 10.3238/arztebl.2017.0215. [DOI] [PMC free article] [PubMed] [Google Scholar]


