Abstract
Objective
Faulty neuromuscular and biomechanical deficits of the knee are nearly ubiquitous in athletes following anterior cruciate ligament (ACL) reconstruction (ACLR). Knee biomechanical deficits are directly associated with an increased risk of second ACL injury, which typically occurs during a sports-related movement on a single-limb. To date, the biomechanical effects of a neuromuscular training (NMT) program on knee biomechanics during a single-leg landing task has not been investigated.
Design
Prospective Cohort Study
Setting
Controlled laboratory setting
Participants
Eighteen ACLR and ten control athletes.
Interventions
Neuromuscular training
Main Outcome Measures
Knee kinematics and kinetics.
Results
There were no significant interactions of session and limb (p>0.05) for the athletes with ACLR after training. However, there were several significant main effects of session (p<0.05) for knee kinematics and kinetics during the single-leg landing task. After training, the athletes with ACLR landed with greater knee flexion angles, decreased knee abduction angles, increased knee flexion range of motion, and decreased knee excursion. Also, the ACLR athletes landed with lower knee flexion moments, greater knee adduction moments, and lower peak vertical ground reaction force. Post-training comparison of the ACLR and control cohorts found no significant interactions of group and limb (p>0.05) and only a significant main effect of group (p<0.05) for frontal plane knee angle at initial contact. The athletes with ACLR landed with greater knee adduction angles than the control group.
Conclusions
Deficits in knee biomechanics which are associated with an increased risk of ACL injury are attenuated after completion of this NMT program.
INTRODUCTION
Anterior cruciate ligament (ACL) injuries disproportionately occur in young, active athletes who participate in sports that involve dynamic single-leg landing and pivoting movements. These injured athletes frequently elect to undergo ACL reconstruction (ACLR) to prevent further injury to structures within the knee, recover functional knee stability, and return to their previous level of activity. Despite surgical intervention and post-operative rehabilitation, athletes often struggle to return to previous levels of activity and the risk of further ACL or knee injury is more than double than that of their initial injury risk.1, 2 Furthermore, progressive degeneration of the articular cartilage occurs as early as 10 to 20 years after the ACL injury.3–5 These complications in athletes with ACLR are commonly associated with lower extremity neuromuscular and biomechanical deficits.6–8
Sports-related activity requires athletes to perform a combination of dynamic and explosive maneuvers on a single leg, which include landing, cutting, pivoting and jumping movements. Video analysis of ACL injuries indicates that athletes are vulnerable to injury when performing these single-leg movements.9–11 These reports have found that athletes typically sustain an ACL injury when landing on a single leg with the knee close to full extension followed by a dynamic valgus collapse of the knee.9, 12, 13 In addition, abnormal limb loading strategies continue to persist in these athletes after ACLR, and faulty neuromuscular and biomechanical adaptations during single-limb tasks may increase risk of further knee injury.14–17 These deleterious movement patterns observed post-ACLR indicate that these athletes may benefit from movement training.
Neuromuscular training (NMT) programs improve lower extremity biomechanics and mitigate the risk of primary ACL injuries.18–20 Hewett and colleagues18 conducted a seminal study in a group of young, uninjured athletes and compared landing mechanics of athletes who underwent the training and a control group. The athletes who underwent the training demonstrated a decrease in impact forces and lower knee abduction and adduction moments. Other similar studies have also found that uninjured athletes demonstrate an improvement in performance and lower-extremity biomechanics after completion of training.21, 22 Such training programs demonstrate numerous other benefits, which include enhanced performance measures and increased lower extremity strength.23, 24 However, currently there is a paucity of studies that have investigated the effects of a NMT program on single-leg landing mechanics in an ACLR cohort just prior to returning to sport. Therefore, the primary purpose of the study is to determine if an NMT program can change single-leg landing knee biomechanics within the group of athletes with ACLR. The first hypothesis tested was that after completion of the NMT program the athletes with ACLR would demonstrate greater knee flexion angles, lower knee abduction angles, greater sagittal plane excursion, lower external knee flexion moments, lower external abduction moments, and lower peak vertical ground reaction force (vGRF) during the single-leg landing task. The secondary purpose of this study was to compare the post-training single-leg landing knee mechanics between the ACLR cohort and an uninjured, control cohort. The second hypothesis tested was that post-training single-leg landing knee biomechanics would be not be significantly different between the athletes with ACLR and the control group of athletes.
METHODS
Athletes for this study were recruited from a university Sports Medicine Clinic or from high schools and sports team that were covered medically by the Department of Sports Medicine. Some of the athletes with ACLR were recommended to participate in the study by their clinical care team that included a Sports Medicine Physician or Physical Therapist. The University’s Institutional Review Board approved the study, and written informed consent was received from all athletes over 18 years of age while parental permission and written assent were received from any of the athletes younger than 18. To ensure the safety of each athlete who participated in the study, a licensed physical therapist or athletic trainer performed clinical tests prior to participation in baseline testing and the NMT program. The series of clinical tests included measurements of knee joint effusion, active and passive knee joint range of motion, isokinetic knee extensor and flexor strength test (Biodex System 3, Boidex, Shirley, NY) at 60 deg/sec, and five continuous bilateral single-leg hops for maximum vertical height. To successfully pass the clinical tests and participate in the study, each participant (regardless of cohort) had to demonstrate: (1) trace or no knee joint effusion,25 (2) pain free range of motion, (3) <30% knee extensor isokinetic strength deficit, and (4) repetitive singe-leg hops in place without any pain. Based on their clinical judgement, the testing clinician did not allow the athlete to participate in the study if the athlete demonstrated high risk movements during the single-leg vertical jump that included a lack of body control or excessive frontal plane motion of the knee.
The training program consisted of 12 sessions that were supervised by members of the research team. The trainers in this study were either: a certified athletic trainer, strength and conditioning coach, or graduate student. The trainers received written and verbal instruction and supervised program implementation from a board-certified physical therapist prior to beginning the study to ensure consistency in program implementation. The training program was implemented from the program described by Di Stasi et al 26 and consisted of seven different exercise progressions that focus on single-leg tasks, bilateral jumping, posterior chain activation, and core and trunk strengthening.26 A detailed table of the training program and exercises can be found in Nagelli et al.27 The exercises all had four levels of progressive difficulty. An athlete’s ability to progress to the next level of exercise difficulty was determined by the trainer who was administering the training program and was based on the athlete’s ability to repetitively demonstrate proper form throughout the exercise duration. Due to these performance-based progression criteria, not all athletes achieved the same performance levels for each progression by their twelfth session. However, the athletes who participated in the study completed all 12 of the training sessions.
Two identical biomechanical analyses were conducted with all of the athletes. The athletes were tested prior to and within a week of completion of the NMT program. The athletes were outfitted with 55 retro-reflective markers28, and motion analysis of five single-leg drop landings (SLD) of both limbs off of a 30.5 cm plyometric box onto embedded force plates (Bertec Corp, Columbus, OH) was performed. Marker trajectories were sampled at 240Hz by a 12-camera motion-capture system (Motional Analysis Corporation, Santa Rosa, CA); ground reaction force data were collected for each limb at 1200Hz.
All motion capture data were post-processed using standardized methods for quality control. Marker position gaps that were within 24 consecutive frames during the SLD task were filled using a cubic spline function in Cortex motion capture software (Cortex version 4.1, Motion Analysis Corp., Santa Rosa, CA). After markers were labeled and the gaps were filled, the marker position data and the ground reaction force data were low-pass filtered using a bi-directional Butterworth filter at 12Hz and 50Hz, respectively.29 Kinematic and kinetic data calculations were performed using custom codes in Visual 3D (C-motion Inc. Germantown, MD) and Matlab (Mathworks Inc Natick, MA). Kinematic variables were calculated using Cardan-Euler sequence for local coordinate systems (X-Y-Z) and kinetic variables were calculated using inverse dynamics. Initial contact (IC) was defined when the vertical component of the ground reaction force (vGRF) exceeded 10 N. All data were time-normalized to 100% of stance.
Sagittal and frontal plane knee angles and moments at initial contact, knee joint excursions from initial contact to the point of peak knee flexion, and vGRF were the primary variables of interest. The first hypothesis was tested using a repeated measure analysis of variance (ANOVA) was performed to assess interactions and main effects of session (pre- and post-training) and limb (involved and uninvolved). The second hypothesis was tested using a two-way ANOVA to assess interactions and main effects of group (ACLR and control) and limb (involved/dominant and uninvolved/non-dominant) from the post-training session. The dominant and non-dominant limbs of the control group were matched with the involved and uninvolved limbs of the ACLR group, respectively. If significant interactions were found, post-hoc t-tests were used to test for significant differences. Main effects were reported in the absence of interactions. Welch’s t-test was used compare demographic data between groups. The alpha level was set to 0.05 a priori to determine significant results (SPSS Statistics Software, IBM Corp., Armonk, New York).
RESULTS
Eighteen athletes with ACLR (8 males and 10 females; 1.7±0.1 height (m); 72.3±1.53 weight (kg); 19.4±7.2 years old) and ten uninjured, control athletes (4 males and 6 females, 1.6±0.1 height (m); 73.1±24.4 weight (kg); 16.4±3.6 years old) were completed the study. Four athletes who enrolled in the study did not meet at least one of the clinical criteria to participate in the study. There were 5 athletes with ACLR who did not return for post-training biomechanics testing of the single-leg landing. There were no significant differences in age (p=0.12), height (p=0.93), or weight (p=0.62) between the ACLR and control groups. Fourteen athletes sustained a non-contact ACL injury which was defined as an ACL injury without a direct blow to the knee and four had a contact injury. The entire ACL-injured cohort who participated in the study in this study received a hamstring tendon autograft during ACLR. The same group of surgeons performed the surgery using standardized surgical techniques and post-operative rehabilitation was completed at the same institution. The ACLR athletes were an average of 7.7 ± 3.7 months post-operative at the time of enrollment.
Effect of Neuromuscular Training on Single-leg Knee Biomechanics in Athletes with ACLR
A summary of the pre- and post-training knee kinematics and kinetics for the athletes with ACLR are presented in Table 1.
Table 1:
Pre- and post-training knee kinematics and kinetics for the ACLR group during the single-leg landing task
| ACLR GROUP | |||||||
|---|---|---|---|---|---|---|---|
| Biomechanical Variables | Pre-Training | Post-Training | Interactions/ Main effects & P-values | Desired Outcome | Result Found | ||
| Involved | Uninvolved | Involved | Uninvolved | ||||
| Knee flexion angle° | 9.8 ± 5.5 | 9.4 ± 4.1 | 12.2 ± 5.4 | 11.9 ± 6.1 | Session: P<0.02 | Increase Flexion | Increase Flexion |
| Knee sagittal plane excursion° | 49.7 ± 9.5 | 51.6 ± 9.7 | 52.0 ± 8.9 | 56.7± 8.4 | Session: p=0.024 | Increase ROM | Increase ROM |
| Knee flexion moment (Nm/kg) | 0.51 ± 0.1 | 0.50 ± 0.1 | 0.40 ± 0.1 | 0.39 ± 0.1 | Session: P<0.01 | Decrease Flexion Moment | Decrease Flexion Moment |
| Knee frontal plane angle° | −0.61 ± 3.2 | 0.11 ± 2.0 | 0.33 ± 3.4 | 0.75 ± 1.9 | Session: P<0.01 | Neutral or Decrease Knee abduction | Increase Adduction |
| Knee frontal plane excursion° | 6.42 ± 3.0 | 6.27 ± 2.5 | 5.4 ± 1.4 | 4.69 ± 1.8 | Session: P<0.01 | Decrease Excursion | Decrease Excursion |
| Knee frontal plane moment (Nm/kg) | 0.07 ± 0.07 | 0.12 ± 0.07 | 0.13 ± 0.04 | 0.12 ± 0.05 | Session: p<0.01 Limb: p<0.04 | Neutral or Decrease Knee abduction | Increase Adduction Moment |
| Vertical Ground Reaction Force (N/kg) | 37.3 ± 8.3 | 37.0 ± 8.1 | 33.1 ± 5.4 | 32.6 ± 4.6 | Session: p=0.003 | Decrease vGRF | Decrease vGRF |
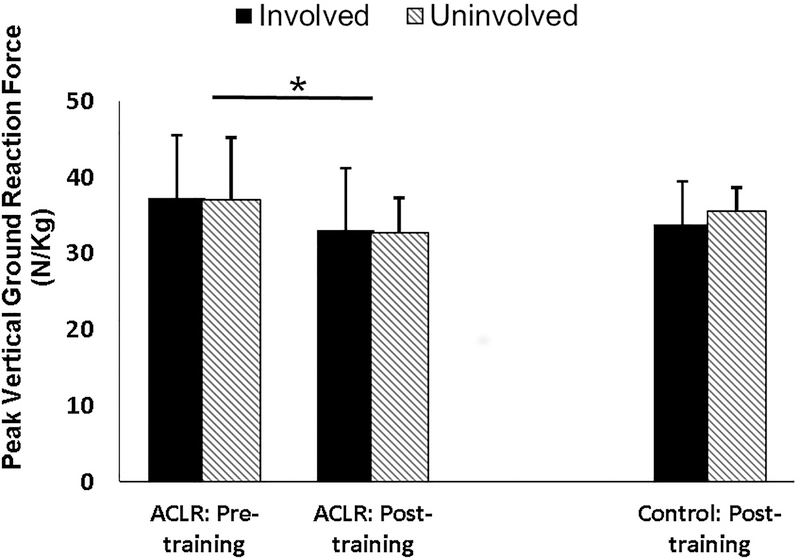
There were no significant interactions (p>>/=0.05) between session and limb for any sagittal plane knee kinematics and kinetics. However, there was a significant main effect of session for knee flexion angle (p=0.02) and sagittal knee excursion (p=0.02). After training, the athletes with ACLR landed with a greater knee flexion angle and sagittal knee excursion. In addition, there was a significant main effect of session for knee flexion moment (p=0.001) and peak vertical ground reaction force (vGRF; p=0.003). The athletes with ACLR landed with a lesser knee flexion moment and decreased vertical ground reaction force (Figure 1) after training.
Figure 1:
Differences in peak vertical ground reaction force (vGRF). A significant main effect of training session *(p=0.003) was found for peak vGRF; the athletes with ACLR demonstrated a decrease in peak vGRF after training. There were no significant differences in post-training peak vGRF between the ACLR and control cohorts.
There were no significant interactions (p>>/=0.05) between session and limb for any frontal plane knee kinematics and kinetics. However, there was a significant main effect of session for frontal knee angle (p<0.01) and frontal knee excursion (p<0.01). After training, the athletes with ACLR landed with greater knee adduction angle and less frontal plane knee excursion. Further, there was a significant main effect of session (p<0.01) and limb (p<0.04) for frontal knee moment. The athletes with ACLR landed with greater knee adduction moment after training, and the involved limbs overall demonstrated a lesser knee adduction moment than the uninvolved limbs.
Post-Training Differences in Single-Leg Landing Knee Mechanics between ACLR and Control Athletes
A summary of the post-training knee kinematics and kinetics for the athletes with ACLR and control groups are presented in Table 2.
Table 2:
Post-training comparison of knee kinematic and kinetic variables between the ACLR and control group
| ACLR Group | Control Group | ||||
|---|---|---|---|---|---|
| Biomechanical Variables | Involved | Uninvolved | Dominant | Non-Dominant | Interactions/Main effects & P-values |
| Knee flexion angle° | 12.2 ± 5.4 | 11.9 ± 6.1 | 13.8 ± 6.5 | 10.6 ± 6.3 | |
| Knee sagittal plane excursion° | 51.9 ± 8.9 | 56.7 ± 8.4 | 49.2 ± 8.9 | 51.8 ± 9.7 | |
| Knee flexion moment (Nm/kg) | 0.37 ± 0.08 | 0.39 ± 0.07 | 0.42 ± 0.10 | 0.41 ± 0.07 | |
| Knee frontal plane angle° | 0.33 ± 3.4 | 0.75 ± 1.9 | −1.7 ± 2.2 | −1.9 ± 3.0 | Group: p=0.003 |
| Knee frontal plane excursion° | 5.4 ± 1.4 | 4.6 ± 1.7 | 4.9 ± 2.3 | 4.5 ± 2.0 | |
| Knee frontal plane moment (Nm/kg) | 0.13 ± 0.04 | 0.11 ± 0.05 | 0.10 ± 0.03 | 0.11± 0.02 | |
| Vertical ground reaction force (N/kg) | 33.1 ± 5.4 | 32.6 ± 4.6 | 33.8 ± 5.6 | 35.5 ± 3.1 | |
There were no significant interactions (p>/=0.05) for group and limb for post-training measures of sagittal plane knee kinematics and kinetics. In addition, there were no significant main effects of group (p>/=0.05) or limb (p>/=0.05) for sagittal plane knee kinematics. There were no observed significant interactions (p>/=0.05) for group and limb for post-training measures of frontal plane knee kinematics and kinetics. However, there was a significant main effect of group for frontal knee angle at initial contact (p=0.003). The athletes with ACLR landed with greater knee adduction angle than the control group post-training.
DISCUSSION
This purpose of this study was to quantify the effect of an evidence-based NMT program on knee biomechanics during a single-leg landing task in athletes after ACLR. The athletes with ACLR demonstrated a marked improvement in single-leg landing knee kinematics and kinetics with the training, as demonstrated by the greater knee flexion angle, increased sagittal plane knee excursion, lower frontal plane knee excursion, lower knee flexion moments, and lesser vertical ground reaction force observed after the training. In addition, the athletes with ACLR post-training demonstrated similar knee kinematics and kinetics compared with a group of uninjured athletes who completed the same NMT program.
Previous research has documented abnormal knee mechanics during a SLD task in athletes with ACLR at the time they return to activity and after they have resumed sport. Although our study did not compare strength in our study but instead had a strict criteria (<30% knee extension deficit), Ithurburn and colleagues17 studied the influence of quadriceps strength asymmetry on single-leg landing mechanics in athletes with ACLR. Regardless of the magnitude of the quadriceps strength deficits, athletes who had undergone ACLR demonstrated greater limb asymmetry in knee flexion excursion, peak knee extension, and peak trunk flexion angle when compared with healthy age- and sex-matched controls.17 Delahunt et al.30 compared hip and knee joint kinematics during a single-limb diagonal jump landing task in ACLR athletes who were greater than 4 years out from surgery and a control group. The results of the study indicate that aberrant hip and knee joint movements were still persistent in the ACLR group that may influence future injury risk.30 A recent systematic review and meta-analysis of thirty-five studies on lower limb biomechanics during single-leg landings (both forward hopping and drop landings) after ACLR found that athletes demonstrate a reduction in peak sagittal plane knee kinematics and kinetics compared with both the contralateral limb and an uninjured, control group.31 Overall, a knee-stiffening strategy is described in the literature by ACLR athletes during a single-leg landing movement. These movement patterns potentially expose the knee joint to higher forces and likely an increased risk of injury.
Several studies have evaluated SLD biomechanics in athletes but only one has provided a comparable data set due to similarities in the methods.32–35 Webster et al.35 investigated the effect of fatigue on single-leg landing biomechanics in athletes with ACLR, and these authors reported baseline SLD knee kinematics from a 30 cm tall box prior to the athlete participating in the fatigue protocol. A significant difference between the studies was that the athletes from the Webster et al35 study were 15–19 months from their ACLR while the athletes from our study were approximately 8 months post-ACLR. The Webster et al35 study reported average baseline knee flexion angle at initial contact for the ACLR limbs and the contralateral limbs to be 13.9° and 14.5°, respectively.35 In comparison, our cohort pre-training demonstrated average knee flexion angles of 9.8° and 9.4° (Table 1) at the same time point of the ACLR limbs and the contralateral limbs, respectively. After training, these demonstrated average knee flexion angles at initial contact of 12.2 and 11.9 of the ACLR limbs and contralateral limbs, respectively. The post-training knee flexion angles of the athletes in our study were comparable to the athletes from the Webster et al35 study who were significantly further out from ACLR than our athletes. Importantly, the findings of our study indicate that this single leg, stiffening landing strategy may be corrected with a NMT program. After training, the athletes with ACLR landed with more knee flexion and went through greater sagittal plane knee excursion. Interestingly, the athletes with ACLR did not significantly differ from the uninjured, control athletes in their sagittal plane landing mechanics after training. Movement training can be effective in correcting aberrant biomechanics that is associated with an increased risk of ACL injury in these athletes.
To the best of the authors’ knowledge, this is the first study to investigate the effects of a NMT program on knee biomechanics during a single-leg landing task in a group of athletes following ACLR. There is limited evidence on the efficacy of NMT programs designed to address biomechanical and neuromuscular deficits in athletes following ACLR. Cappin et al.36 found no differences in biomechanical gait variables between a group of men that post-operatively underwent strength, agility, and secondary prevention (SAP) training along with perturbation training or a group that only underwent SAP training. Although the gait asymmetries did improve from 1 to 2 years, the authors found that meaningful asymmetries still persisted.36 In comparison to our study, we included a mixed cohort of males and females athletes with ACLR and the NMT mainly focused on plyometric exercises and core strength and stability. Regardless, we found that the NMT can augment post-operative rehabilitation and address single-leg landing knee biomechanical deficits. Further research on knee deficits during a SLD task and its association with second ACL injury is warranted. A recent review found that nearly 1 in 4 young athletes who return to high-risk sport will go on to sustain another ACL injury almost immediately after returning to sport.2 Importantly, the high rate of second ACL injury in young ACLR athletes equates to a 30 to 40 times greater risk of an ACL injury compared with their uninjured counterparts.2
The effect of NMT on lower extremity biomechanics has been previously reported on cohorts of uninjured athletes. A recent systematic review and meta-analysis sought to understand the effect of training programs on the biomechanics of landing tasks. The majority of these studies evaluated young female athletes (24 studies out of 28 included) and bilateral landing tasks (22 studies out of 28 included). These authors found that after participating in the training program there was a significant decrease in peak knee flexion moment and peak knee abduction moment but peak vGRF did not change. In addition, athletes demonstrated a significant increase in hip flexion angle at initial contact, peak hip flexion angle, and peak knee flexion angle, while knee flexion at initial contact did not change. In comparison to our athletes with ACLR performing a unilateral landing task, we observed an increase in sagittal plane knee kinematics (knee flexion angle at initial contact and knee excursion) and a decrease in knee flexion moment at initial contact. In addition, we found a decrease in knee adduction angle and moment at initial contact and a decrease in knee frontal plane excursion. We did not find significant changes in knee abduction angles or moments possibly due to our strict criteria to participate in the study which screened for athletes with large frontal plane movements. These studies together suggest that these training programs can improve landing biomechanics in both injured and uninjured athletes.
This study is not without limitations. The SLD task off a 31 cm tall box may not reflect a movement that occurs during a game, practice, or match. However, this particular task may expose biomechanical deficits which may not be readily apparent during a bilateral landing task. As mentioned above, further research on lower extremity biomechanics during a SLD and its association to ACL injury is required. For this particular study’s purpose, the SLD was utilized to understand if a NMT program can modifies the task’s biomechanics in a cohort of athletes with ACLR. It would have been preferable to compare the control group to both the pre- and post-NMT data of the group with athletes with ACLR, but as this was a secondary analysis of this cohort, we felt we were already running the risk of underpowering the analysis. In our study, the change in SLD knee biomechanics was statistically significant and in the direction of change that is theorized to be more protective against knee joint injury (i.e. increased flexion), but we did not report patient reported outcomes or minimal clinically important difference. This will be an area of focus for future studies. Intervention in a clinical population highlights the difficulty of balancing safety for the athletes and testing to capture the representative population. Therefore, we implemented strenuous clinical criteria for participation in the study. This may also have selectively biased our cohort of study by selection of the athletes who functioned at a superior baseline level. However, the ACLR athletes still demonstrated an improvement in knee biomechanics after participation in the NMT program prior to return-to-sport. These findings indicate that even athletes who demonstrate high baseline function with few clinical limitations can significantly benefit from a NMT program. In addition, these athletes finished 12 NMT sessions with an athletic trainer, graduate student, or strength and conditioning coach which suggest that this training can be implemented effectively in different athlete settings. The adherence of our study was that the athlete completes all 12 training sessions and pre/post-biomechanics testing sessions to be included. We did not record how far each athlete progressed in each exercise progression. Future studies will investigate how biomechanical improvements are associated with exercise progression and compliance. Athletes were followed-up within one week of completion of the NMT program; hence, the retention of the effects of this program are unknown in these athletes. Furthermore, we did not evaluate the effect of the training program on the control group despite this group completing the study. With a large sample of control athletes, sufficient statistical power would be achieved to investigate how the control group changes relative to our athletes with ACLR. However, the beneficial effects of an NMT program on a cohort of control athletes are reported in the literature. The current study also did not include age- and sex-matched controls for these athletes with ACLR. This would have allowed the current study to control for differences between sex and age in landing biomechanics. However, we did test for group differences post-training and did not find any. Future studies will address the current limitations in our study. However, the overall aim of this first study was to understand the change in single-leg landing knee biomechanics due to a NMT program in athletes with ACLR.
CONCLUSION
In this study, a NMT program effectively addressed knee biomechanical and neuromuscular deficits during a single-leg landing task in ACLR athletes. Furthermore, it was demonstrated that after NMT, normative knee biomechanics and neuromuscular control were established in an ACLR cohort. These results indicate that a NMT program may have the potential to reduce the risk of second ACL injury as athletes return to sport. In addition, this training program may augment post-operative rehabilitation protocols to effectively address residual knee movement impairments. Further directions for these studies will be to follow athletes longitudinally to determine levels of retention of the training effects as they return to sports and whether the training program reduces second ACL injury rates.
ACKNOWLEDGEMENTS
The authors would like to thank the researchers and staff at Mayo Clinic and The Ohio State University for their support. We acknowledge support from the National Institute of Arthritis and Musculoskeletal and Skin Diseases: T32AR56950 for CVN and R01AR056259 and R01AR055563 to TEH.
FUNDING: We acknowledge support from the Sports Physical Therapy Section of the American Physical Therapy Association. We acknowledge CVN was supported by T32AR56680 and R01AR056259 and R01AR055563 to TEH.
Footnotes
ETHICAL CONSIDERATIONS
There are no ethical considerations for this particular study.
REFERENCES
- 1.Ardern CL, Taylor NF, Feller JA, et al. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48(21):1543–1552. [DOI] [PubMed] [Google Scholar]
- 2.Wiggins AJ, Grandhi RK, Schneider DK, et al. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2016;44(7):1861–1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Daniel DM, Stone ML, Dobson BE, et al. Fate of the ACL-injured patient. A prospective outcome study. Am J Sports Med. 1994;22(5):632–644. [DOI] [PubMed] [Google Scholar]
- 4.Myklebust G, Holm I, Maehlum S, et al. Clinical, functional, and radiologic outcome in team handball players 6 to 11 years after anterior cruciate ligament injury: a follow-up study. Am J Sports Med. 2003;31(6):981–989. [DOI] [PubMed] [Google Scholar]
- 5.Lohmander LS, Ostenberg A, Englund M, et al. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum. 2004;50(10):3145–3152. [DOI] [PubMed] [Google Scholar]
- 6.Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38(10):1968–1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Andriacchi TP, Mundermann A, Smith RL, et al. A framework for the in vivo pathomechanics of osteoarthritis at the knee. Ann Biomed Eng. 2004;32(3):447–457. [DOI] [PubMed] [Google Scholar]
- 8.Chaudhari AM, Briant PL, Bevill SL, et al. Knee kinematics, cartilage morphology, and osteoarthritis after ACL injury. Med Sci Sports Exerc. 2008;40(2):215–222. [DOI] [PubMed] [Google Scholar]
- 9.Hewett TE, Torg JS, Boden BP. Video analysis of trunk and knee motion during non-contact anterior cruciate ligament injury in female athletes: lateral trunk and knee abduction motion are combined components of the injury mechanism. Br J Sports Med. 2009;43(6):417–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Boden BP, Torg JS, Knowles SB, et al. Video Analysis of Anterior Cruciate Ligament Injury. The American Journal of Sports Medicine. 2009;37(2):252–259. [DOI] [PubMed] [Google Scholar]
- 11.Krosshaug T, Nakamae A, Boden BP, et al. Mechanisms of anterior cruciate ligament injury in basketball: video analysis of 39 cases. Am J Sports Med. 2007;35(3):359–367. [DOI] [PubMed] [Google Scholar]
- 12.Olsen OE, Myklebust G, Engebretsen L, et al. Injury mechanisms for anterior cruciate ligament injuries in team handball: a systematic video analysis. Am J Sports Med. 2004;32(4):1002–1012. [DOI] [PubMed] [Google Scholar]
- 13.Boden BP, Torg JS, Knowles SB, et al. Video analysis of anterior cruciate ligament injury: abnormalities in hip and ankle kinematics. Am J Sports Med. 2009;37(2):252–259. [DOI] [PubMed] [Google Scholar]
- 14.Salem GJ, Salinas R, Harding FV. Bilateral kinematic and kinetic analysis of the squat exercise after anterior cruciate ligament reconstruction. Arch Phys Med Rehabil. 2003;84(8):1211–1216. [DOI] [PubMed] [Google Scholar]
- 15.Hoshino Y, Fu FH, Irrgang JJ, et al. Can joint contact dynamics be restored by anterior cruciate ligament reconstruction? Clin Orthop Relat Res. 2013;471(9):2924–2931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Delahunt E, Sweeney L, Chawke M, et al. Lower limb kinematic alterations during drop vertical jumps in female athletes who have undergone anterior cruciate ligament reconstruction. J Orthop Res. 2012;30(1):72–78. [DOI] [PubMed] [Google Scholar]
- 17.Ithurburn MP, Paterno MV, Ford KR, et al. Young Athletes With Quadriceps Femoris Strength Asymmetry at Return to Sport After Anterior Cruciate Ligament Reconstruction Demonstrate Asymmetric Single-Leg Drop-Landing Mechanics. Am J Sports Med. 2015;43(11):2727–2737. [DOI] [PubMed] [Google Scholar]
- 18.Hewett TE, Stroupe AL, Nance TA, et al. Plyometric Training in Female Athletes Decreased Impact Forces and Increased Hamstring Torques. The American Journal of Sports Medicine. 1996;24(6):765–773. [DOI] [PubMed] [Google Scholar]
- 19.Myklebust G, Engebretsen L, Braekken IH, et al. Prevention of anterior cruciate ligament injuries in female team handball players: a prospective intervention study over three seasons. Clin J Sport Med. 2003;13(2):71–78. [DOI] [PubMed] [Google Scholar]
- 20.Hewett TE, Lindenfeld TN, Riccobene JV, et al. The effect of neuromuscular training on the incidence of knee injury in female athletes. A prospective study. Am J Sports Med. 1999;27(6):699–706. [DOI] [PubMed] [Google Scholar]
- 21.Myer GD, Ford KR, Palumbo JP, et al. Neuromuscular training improves performance and lower-extremity biomechanics in female athletes. J Strength Cond Res. 2005;19(1):51–60. [DOI] [PubMed] [Google Scholar]
- 22.Myer GD, Ford KR, Brent JL, et al. Differential neuromuscular training effects onACL injury risk factors in”high-risk” versus “low-risk” athletes. BMC Musculoskelet Disord. 2007;8(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Noyes FR, Barber Westin SD. Anterior cruciate ligament injury prevention training in female athletes: a systematic review of injury reduction and results of athletic performance tests. Sports Health. 2012;4(1):36–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sugimoto D, Myer GD, Bush HM, et al. Effects of compliance on trunk and hip integrative neuromuscular training on hip abductor strength in female athletes. J Strength Cond Res. 2014;28(5):1187–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sturgill LP, Snyder-Mackler L, Manal TJ, et al. Interrater reliability of a clinical scale to assess knee joint effusion. J Orthop Sports Phys Ther. 2009;39(12):845–849. [DOI] [PubMed] [Google Scholar]
- 26.Di Stasi S, Myer GD, Hewett TE. Neuromuscular training to target deficits associated with second anterior cruciate ligament injury. J Orthop Sports Phys Ther. 2013;43(11):777–792, a771–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nagelli C, Wordeman S, Di Stasi S, et al. Biomechanical Deficits at the Hip in Athletes With ACL Reconstruction Are Ameliorated With Neuromuscular Training. Am J Sports Med. 2018;46(11):2772–2779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bates NA, Schilaty ND, Nagelli CV, et al. Novel mechanical impact simulator designed to generate clinically relevant anterior cruciate ligament ruptures. Clin Biomech (Bristol, Avon). 2017;44:36–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Roewer BD, Ford KR, Myer GD, et al. The ‘impact’ of force filtering cut-off frequency on the peak knee abduction moment during landing: artefact or ‘artifiction’? Br J Sports Med. 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Delahunt E, Prendiville A, Sweeney L, et al. Hip and knee joint kinematics during a diagonal jump landing in anterior cruciate ligament reconstructed females. J Electromyogr Kinesiol. 2012;22(4):598–606. [DOI] [PubMed] [Google Scholar]
- 31.Johnston PT, McClelland JA, Webster KE. Lower Limb Biomechanics During Single-Leg Landings Following Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-Analysis. Sports Med. 2018;48(9):2103–2126. [DOI] [PubMed] [Google Scholar]
- 32.Antolic V, Strazar K, Pompe B, et al. Increased muscle stiffness after anterior cruciate ligament reconstruction--memory on injury? Int Orthop. 1999;23(5):268–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Webster KE, Gonzalez-Adrio R, Feller JA. Dynamic joint loading following hamstring and patellar tendon anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2004;12(1):15–21. [DOI] [PubMed] [Google Scholar]
- 34.Webster KE, Feller JA. Tibial rotation in anterior cruciate ligament reconstructed knees during single limb hop and drop landings. Clin Biomech (Bristol, Avon). 2012;27(5):475–479. [DOI] [PubMed] [Google Scholar]
- 35.Webster KE, Santamaria LJ, McClelland JA, et al. Effect of fatigue on landing biomechanics after anterior cruciate ligament reconstruction surgery. Med Sci Sports Exerc. 2012;44(5):910–916. [DOI] [PubMed] [Google Scholar]
- 36.Capin JJ, Zarzycki R, Arundale A, et al. Report of the Primary Outcomes for Gait Mechanics in Men of the ACL-SPORTS Trial: Secondary Prevention With and Without Perturbation Training Does Not Restore Gait Symmetry in Men 1 or 2 Years After ACL Reconstruction. Clinical Orthopaedics and Related Research®. 2017;475(10):2513–2522. [DOI] [PMC free article] [PubMed] [Google Scholar]