Abstract
Background
The World Health Organization (WHO) declared coronavirus disease-19 (COVID-19) as a pandemic on March 11, 2020. The impact of COVID-19 on urological services in different geographical areas is unknown.
Objective
To investigate the global impact of COVID-19 on urological providers and the provision of urological patient care.
Design, setting, and participants
A cross-sectional, web-based survey was conducted from March 30, 2020 to April 7, 2020. A 55-item questionnaire was developed to investigate the impact of COVID-19 on various aspects of urological services. Target respondents were practising urologists, urology trainees, and urology nurses/advanced practice providers.
Outcome measurements and statistical analysis
The primary outcome was the degree of reduction in urological services, which was further stratified by the geographical location, degree of outbreak, and nature and urgency of urological conditions. The secondary outcome was the duration of delay in urological services.
Results and limitations
A total of 1004 participants responded to our survey, and they were mostly based in Asia, Europe, North America, and South America. Worldwide, 41% of the respondents reported that their hospital staff members had been diagnosed with COVID-19 infection, 27% reported personnel shortage, and 26% had to be deployed to take care of COVID-19 patients. Globally, only 33% of the respondents felt that they were given adequate personal protective equipment, and many providers expressed fear of going to work (47%). It was of concerning that 13% of the respondents were advised not to wear a surgical face mask for the fear of scaring their patients, and 21% of the respondents were advised not to discuss COVID-19 issues or concerns on media. COVID-19 had a global impact on the cut-down of urological services, including outpatient clinic appointments, outpatient investigations and procedures, and urological surgeries. The degree of cut-down of urological services increased with the degree of COVID-19 outbreak. On average, 28% of outpatient clinics, 30% of outpatient investigations and procedures, and 31% of urological surgeries had a delay of >8 wk. Urological services for benign conditions were more affected than those for malignant conditions. Finally, 47% of the respondents believed that the accumulated workload could be dealt with in a timely manner after the COVID-19 outbreak, but 50% thought the postponement of urological services would affect the treatment and survival outcomes of their patients. One of the limitations of this study is that Africa, Australia, and New Zealand were under-represented.
Conclusions
COVID-19 had a profound global impact on urological care and urology providers. The degree of cut-down of urological services increased with the degree of COVID-19 outbreak and was greater for benign than for malignant conditions. One-fourth of urological providers were deployed to assist with COVID-19 care. Many providers reported insufficient personal protective equipment and support from hospital administration.
Patient summary
Coronavirus disease-19 (COVID-19) has led to significant delay in outpatient care and surgery in urology, particularly in regions with the most COVID-19 cases. A considerable proportion of urology health care professionals have been deployed to assist in COVID-19 care, despite the perception of insufficient training and protective equipment.
Keywords: Coronavirus disease-19, Severe acute respiratory syndrome coronavirus 2, Survey, Urology, Urological service, UroSoMe
Take Home Message
The coronavirus disease-19 (COVID-19) pandemic has imposed great challenges to the urological community globally. The impact of COVID-19 on urological services increased with the degree of outbreak, and resulted in significant delay in the delivery of urological care.
1. Introduction
The novel coronavirus was first reported in Wuhan City, Hubei Province of China, in December 2019 and has spread rapidly to >200 countries and territories around the world [1], [2]. The World Health Organization (WHO) declared the situation a public health emergency of international concern on January 30, 2020 and subsequently named this disease coronavirus disease-19 (COVID-19) on February 11, 2020. Since it has been declared as a pandemic by the WHO on March 11, 2020, the virus has resulted in 1 780 314 laboratory-confirmed cases and 106 827 deaths worldwide as of April 12, 2020 [3].
Hospitals and health care authorities have taken unprecedented and strict measures to curb the surge of COVID-19 patients. Many hospitals have been converted to dedicated facilities to manage these patients specifically. Hospital staff including doctors and nurses were diagnosed with COVID-19 despite taking protective measures to prevent the viral transmission. The insufficiency of personal protective equipment (PPE) provided to the front-line health care workers made the situation even worse [4]. Many providers irrespective of speciality have been deployed to manage patients with COVID-19. It is a critical moment that imposes enormous difficulties and challenges to urology health care professionals globally.
This global pandemic has led many urologists to make unprecedented decisions for striking a balance between providing optimal and high-quality urological care to their patients, while mitigating the risks of dispersing the infections among their own patients and health care workers. In hospitals that cater for managing COVID-19 patients, surgical departments might have been instructed to minimise or temporarily suspend all elective surgeries to cope with the devastating increment of COVID-19 cases. In addition to the effects on operations, it might also affect the out- as well as inpatient urological services [5], [6].
In light of this, we conducted an online survey to study the impact of COVID-19 on urological services from a global perspective. Our objective in this study was to elucidate how the urological community has been managing urological patients in the pandemic of COVID-19.
2. Patients and methods
2.1. Overview
We conducted a cross-sectional, web-based survey to investigate the impact of COVID-19 on urological services. Urology registrars, fellows, consultant urologists, urology nurse specialists, and advanced practice providers were invited to participate in this study. This study was approved by the Survey and Behavioural Research Ethics Committee of the Chinese University of Hong Kong (Reference No. SBRE-19-516).
2.2. Content of the survey
The structured questionnaire was developed with a modified Delphi method. The first draft of the questionnaire was developed by the steering committee (J.Y.C.T., W.L.K.O., D.G.P., D.C., J.D., H.Y.T., and S.L.) after reviewing the current literature regarding the effects of COVID-19 on health care services. A total of 72 questions were initially drafted and sent out to the UroSoMe working group. All feedback received was reviewed by the steering committee, and the questions were further refined until consensus was reached. At the end of the development process, a total of 55 questions were finalised for this survey. The final questionnaire comprised 55 items covering demographics (eight items), impact of COVID-19 on health care professionals and hospital policy (25 items), outpatient clinic (six items), outpatient investigations and procedures (six items), and urological surgeries (eight items), and attitudes towards the of COVID-19 (two items). The full questionnaire is presented in the Supplementary material.
2.3. Data collection
The survey was primarily distributed through the #UroSoMe platforms (website and Twitter) [7]. The first invitation to participate in the study was sent out on March 30, 2020. Organisations engaged in the field of urology, including Australian Young Urology Researchers Organisation, British Association of Urological Nurses, British Urology Researchers in Surgical Training, Canadian Urological Association, European Association of Urology (EAU), European Association of Urology European School of Urology, European Association of Urology Young Academics Urologists, Fight Bladder Cancer, International Continence Society, Malaysian Urological Association, Prostate Cancer Foundation, Saolta Urology/Continence Nurses Network, Society of Urological Surgery in Turkey, the Urological Society of Australia and New Zealand, UK Oncology Forum, Urology News, Urology Tweets, and UroToday, helped disseminate the survey invitation either by their Twitter accounts or by official mailing lists. Details regarding the number of followers of the Twitter accounts and the number of members in the mailing lists are summarised in the Supplementary material. As COVID-19 is a global emergency, we wish to provide a rapid report about the effects of COVID-19 on urological services during this critical time period. No additional reminders were sent by the time we concluded the survey.
By clicking on the survey link (https://www.surveymonkey.co.uk/r/8KJNSDH) participants accessed to a webpage that contained general information about the study. It was specified that this survey was intended only for urology nurses and urologists. We also included a question to confirm that the participants were “consultant/practising urologists”, “urology trainees/registrars/fellow”, or “urology nurse specialist/advanced practice providers”. Participants were implied to have consented to participate upon registration and providing responses to the survey. In order to avoid missing data, the online version required an answer to all survey questions. The participant responses were accrued through the Survey Monkey website. We implemented measures on IP restriction, that is, one IP address can complete the survey only once. All survey responses were accessible only to the investigators. We also obtained the cumulative number of new cases of COVID-19 for each country from the European Centre for Disease prevention and Control [8] and paired them with the respondents according to the date they completed the survey.
2.4. Data synthesis and statistical analysis
The primary outcome was the degree of reduction in urological services, which was further stratified by geographical location, degree of outbreak, and nature and urgency of urological conditions. The secondary outcome was the duration of delay in urological services. Demographic data and impact of COVID-19 on health care professionals and hospital policy were presented in a descriptive manner. Chi-square test was used for comparison between continents. Heat maps were created to analyse the global impact of COVID-19 on urological services by geographical location. Based on the respondents’ answers to the questions on cut-down of services (ie, 0%, 1–20%, 21–40%, 41–60%, 61–80%, and 81–100%), mean scores were calculated for each individual country and were presented in global maps with a scale of 0–100%. We made two assumptions for countries without any respondents: (1) they were assumed to have zero cut-down if there were no reported cases of COVID-19 in their countries and (2) they were assumed to have a similar degree of cut-down to the other countries within the same subgroup based on the WHO classification for global assessment of disease burden [9]. Next, we analysed the impact of COVID-19 on urological services by the degree of outbreak, which was determined by the cumulative number of new cases in each respondent's country at the time of the survey. The respondents were categorised into five groups based on their percentiles of COVID-19 cases (ie, 0–20, 21–40, 41–60, 61–80, and 81–100 percentile). The relationship between the cut-down of urological services and the degree of outbreak was presented using bar charts. We further analysed the impact of COVID-19 on urological services by the nature and urgency of urological conditions. Outpatient clinics, outpatient urological investigations and procedures, and urological surgeries were categorised as “benign and nonurgent”, “benign but potentially urgent”, and “malignant” based on the urological conditions of interest. “Ureteric stone” was classified as “benign but potentially urgent” because it may affect the kidney function if definitive treatment is delayed. “Renal transplantation” was classified as “benign but potentially urgent” because the availability of cadaveric graft kidney is unpredictable and organ harvest cannot be delayed. “Extracorporeal shock wave lithotripsy” (ESWL) was classified as “benign but potentially urgent” as it is a common treatment modality for ureteric stone. The results were illustrated using bar charts. Information on the delay of urological services and the attitudes of health care professionals towards the impact of delay were presented in a descriptive manner. We took reference from the literature and decided to use 8 wk as a cut-off for delay in urological services [10]. All demographic data were complete without missing data. We had missing data on the outcome variables, but we did not perform any regression analysis. Hence, we used complete case analysis as the primary analysis, and imputation was not performed [11], [12]. No weighting was considered in our data analysis.
3. Results
Between March 30, 2020 and April 7, 2020, a total of 1004 participants responded to the survey. Of them, 678 completed the whole survey, resulting in a complete response rate of 68%. The mean time spent to complete the survey was 8 min. Demographic details are summarised in Table 1 . The majority of the respondents were male and aged between 30 and 49 yr. In terms of the geographical distribution, the highest proportion of respondents was based in Asia, followed by Europe, North America, South America, Africa, and Australia and New Zealand. The majority of them were consultant urologists, based in teaching hospitals or academic institutions, and practising general urology.
Table 1.
Demographics of survey respondents
| n (N = 1004) | % | |
|---|---|---|
| Age (yr) | ||
| <30 | 69 | 6.9 |
| 30–39 | 460 | 46 |
| 40–49 | 272 | 27 |
| 50–59 | 151 | 15 |
| ≥60 | 52 | 5.2 |
| Gender | ||
| Male | 828 | 82 |
| Female | 176 | 18 |
| Continent | ||
| Asia | 411 | 41 |
| Australia and New Zealand | 15 | 1.5 |
| Africa | 25 | 2.5 |
| Europe | 321 | 32 |
| North America | 156 | 16 |
| South America | 76 | 7.6 |
| Types of hospital/institution | ||
| Teaching hospital/academic institution | 557 | 56 |
| Nonacademic public hospital | 164 | 16 |
| Private practice | 170 | 17 |
| Mixture of public and private practices | 113 | 11 |
| Level of training | ||
| Urology nurse specialists/advanced practice providers | 60 | 6.0 |
| Urology trainees/registrars/fellows | 227 | 23 |
| Consultants/practising urologists | 717 | 71 |
| Years of practice | ||
| <5 | 325 | 32 |
| 6–10 | 244 | 24 |
| 11–15 | 181 | 18 |
| 16–20 | 93 | 9.3 |
| >20 | 161 | 16 |
| Urology speciality | ||
| General urology | 716 | 71 |
| Benign prostatic hyperplasia | 478 | 48 |
| Female urology | 215 | 21 |
| Stones | 514 | 51 |
| Oncology | 505 | 50 |
| Infertility/sexual medicine | 196 | 20 |
| Paediatric urology | 125 | 12 |
| Renal transplantation | 109 | 11 |
3.1. Impact of COVID-19 on health care professionals and hospital policy
Based on the conclusion of this survey, 78% of the hospitals where respondents work were managing COVID-19 patients. Of the respondents, 41% reported that staff members in their hospitals had been diagnosed with COVID-19 infection, with a higher proportion in Europe and North America than in the other continents (p < 0.001); 26% reported that there was a need of deployment to take care of COVID-19 patients on either a voluntarily or a mandatory basis. Europe had a greater need of deployment than the other continents (p < 0.001). European respondents also cited the highest percentage of personnel shortage problem, followed by South America and Asia (p = 0.001).
Assessing urology providers’ attitudes, 47% of the health care professionals were scared to go to work, and 50% felt either very uncomfortable or uncomfortable with their training in infectious disease and respiratory care. Most of the respondents were provided PPE at work, mainly in the form of a surgical mask. The availability of N95 masks, body suits, face shields, and surgical goggles was low. Overall, only 33% of the respondents felt that they were given adequate PPE. About half of the respondents felt that their hospitals had adequate administration combating the pandemic of COVID-19. Meanwhile, 13% of the respondents were advised not to wear a surgical face mask for fear of scaring their patients, and 21% of the respondents were advised not to have media contact regarding COVID-19. Of the respondents, 60% were expecting a pay cut due to the COVID-19 pandemic. In the outpatient clinic setting, the patients were advised to wear a mask in 52% of the hospitals; health care professionals were advised to wear PPE in 56% of the hospitals. Patients were routinely asked about or checked for fever (75%), upper respiratory infection symptoms (80%), and travel, occupation, contact, and cluster (TOCC) history (66%) before consultation, urological investigations, and surgeries. In addition, COVID-19 caused cancellations of multidisciplinary team meetings, journal clubs, grand rounds, mortality and morbidity meetings, and x-ray meetings. The results are summarised in Table 2 .
Table 2.
Number (%) of respondents who responded affirmatively to each of the following questions, overall and by continent
| Total (n = 752) |
Africa (n = 21) | Asia (n = 319) | Australia and New Zealand (n = 13) | Europe (n = 224) | North America (n = 122) | South America (n = 53) | p value | ||
|---|---|---|---|---|---|---|---|---|---|
| N | % (95% CI) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | ||
| COVID-19+ | |||||||||
| Patients in hospital | 588 | 78 (75–81) | 11 (52) | 206 (65) | 7 (54) | 202 (90) | 114 (93) | 48 (91) | <0.001 |
| Staff tested + | 311 | 41 (38–45) | 4 (19) | 82 (26) | 4 (31) | 144 (64) | 62 (51) | 15 (28) | <0.001 |
| Need of deployment | |||||||||
| Voluntary basis | 87 | 12 (9–14) | 1 (4.8) | 34 (11) | 1 (7.7) | 32 (14) | 9 (7.4) | 7 (13) | <0.001 |
| Mandatory basis | 107 | 14 (12–17) | 4 (19) | 27 (8.5) | 0 (0) | 59 (26) | 9 (7.4) | 8 (15) | |
| Personnel shortage | 204 | 27 (24–31) | 3 (14) | 78 (24) | 1 (7.7) | 82 (37) | 24 (20) | 16 (30) | 0.001 |
| Perceptions | |||||||||
| Fearful going to work | 355 | 47 (44–51) | 10 (48) | 134 (42) | 5 (38) | 99 (44) | 74 (61) | 33 (62) | 0.007 |
| Infectious disease training | |||||||||
| Very uncomfortable/uncomfortable | 377 | 50 (47–54) | 11 (52) | 131 (41) | 9 (69) | 120 (54) | 77 (63) | 29 (55) | <0.001 |
| Neutral | 271 | 36 (33–40) | 8 (38) | 140 (44) | 3 (23) | 75 (33) | 31 (25) | 14 (26) | |
| Comfortable/very comfortable | 104 | 14 (11–17) | 2 (9.5) | 48 (15) | 1 (7.7) | 29 (13) | 14 (11) | 10 (19) | |
| PPE training | 243 | 32 (29–36) | 3 (14) | 111 (35) | 5 (38) | 85 (38) | 29 (24) | 10 (19) | 0.007 |
| PPE provided | |||||||||
| Surgical mask | 691 | 92 (90–94) | 19 (90) | 296 (93) | 11 (85) | 214 (96) | 104 (85) | 47 (89) | 0.021 |
| N95 mask | 320 | 43 (39–46) | 2 (9.5) | 138 (43) | 4 (31) | 81 (36) | 66 (54) | 29 (55) | <0.001 |
| Body suit | 213 | 28 (25–32) | 3 (14) | 113 (35) | 1 (7.7) | 69 (31) | 11 (9.0) | 16 (30) | <0.001 |
| Face shield | 312 | 41 (38–45) | 2 (9.5) | 137 (43) | 6 (46) | 98 (44) | 55 (45) | 14 (26) | 0.009 |
| Goggles | 301 | 40 (37–44) | 3 (14) | 128 (40) | 4 (31) | 97 (43) | 39 (32) | 30 (57) | 0.005 |
| “Adequate PPE” | 246 | 33 (29–36) | 5 (24) | 126 (39) | 4 (31) | 58 (26) | 42 (34) | 11 (21) | 0.042 |
| Hospital policy and administration | |||||||||
| Adequate administration | 384 | 51 (47–55) | 6 (29) | 184 (58) | 7 (54) | 97 (43) | 62 (51) | 28 (53) | 0.056 |
| Advised not to wear masks | 97 | 13 (11–16) | 3 (14) | 18 (5.6) | 3 (23) | 34 (15) | 30 (25) | 9 (17) | <0.001 |
| No media contact | 156 | 21 (18–24) | 1 (4.8) | 50 (16) | 0 (0) | 68 (30) | 29 (24) | 8 (15) | <0.001 |
| Pay cut expected | 453 | 60 (57–64) | 9 (43) | 206 (65) | 8 (62) | 109 (49) | 75 (61) | 46 (87) | <0.001 |
| Meetings cancelled | |||||||||
| Multidisciplinary | 483 | 64 (61–68) | 18 (86) | 209 (66) | 7 (54) | 137 (61) | 70 (57) | 42 (79) | 0.018 |
| X-ray | 272 | 36 (33–40) | 7 (33) | 131 (41) | 5 (38) | 72 (32) | 39 (32) | 18 (34) | 0.3 |
| Journal club | 393 | 52 (49–56) | 13 (62) | 181 (57) | 5 (38) | 106 (47) | 59 (48) | 29 (55) | 0.2 |
| M&M | 332 | 44 (41–48) | 10 (48) | 150 (47) | 6 (46) | 99 (44) | 53 (43) | 14 (26) | 0.2 |
| Grand rounds | 379 | 50 (47–54) | 10 (48) | 166 (52) | 8 (62) | 97 (43) | 67 (55) | 31 (58) | 0.2 |
| Policy for urological services | |||||||||
| Patients wear mask | 391 | 52 (48–56) | 7 (33) | 205 (64) | 2 (15) | 103 (46) | 52 (43) | 22 (42) | <0.001 |
| HCPs wear PPE | 422 | 56 (53–60) | 7 (33) | 189 (59) | 3 (23) | 130 (58) | 70 (57) | 23 (43) | 0.001 |
| Ask for fever/check temp | 562 | 75 (72–78) | 9 (43) | 269 (84) | 10 (77) | 144 (64) | 105 (86) | 25 (47) | <0.001 |
| Ask for URI symptoms | 604 | 80 (77–83) | 11 (52) | 270 (85) | 13 (100) | 168 (75) | 104 (85) | 38 (72) | <0.001 |
| Ask for TOCC history | 494 | 66 (62–69) | 12 (57) | 254 (80) | 10 (77) | 113 (50) | 83 (68) | 22 (42) | <0.001 |
CI = confidence interval; COVID-19 = coronavirus disease-19; HCP = health care professionals; M&M = morbidity and mortality; PPE = personal protective equipment; TOCC = travel, occupation, contact and cluster; URI = upper respiratory infection.
3.2. Impact of COVID-19 by geographical location
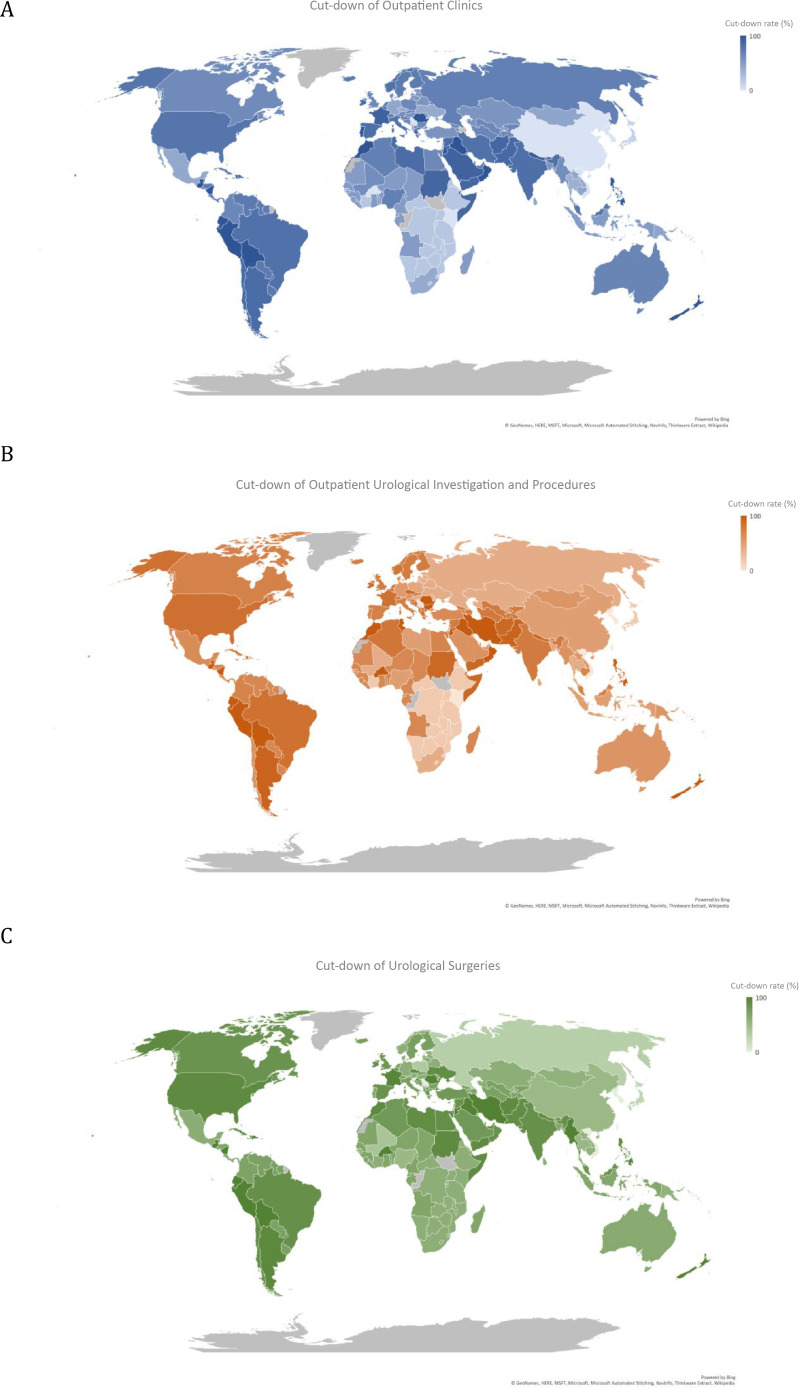
COVID-19 had a global impact on the cut-down of urological services, including outpatient clinic, outpatient investigations and procedures, and urological surgeries. In particular, all types of urological services appeared to be most affected in North America, South America, South Asia, West Asia, North Africa, West Africa, and some European countries. Australia and New Zealand also had a considerable cut-down of outpatient clinic appointments, outpatient investigations and procedures, and urological surgeries. North Asia had a considerable cut-down of outpatient clinic appointments, but outpatient urological investigations and procedures and urological surgeries appeared to be less affected. The heat maps on the cut-down of urological services are shown in Figure 1 . Detailed figures for each individual country are listed in the Supplementary material.
Fig. 1.
The impact of COVID-19 on (A) outpatient clinics, (B) outpatient urological investigations and procedures, and (C) urological surgeries, of individual countries (grey colour indicates countries with no available data). COVID-19 = coronavirus disease-19.
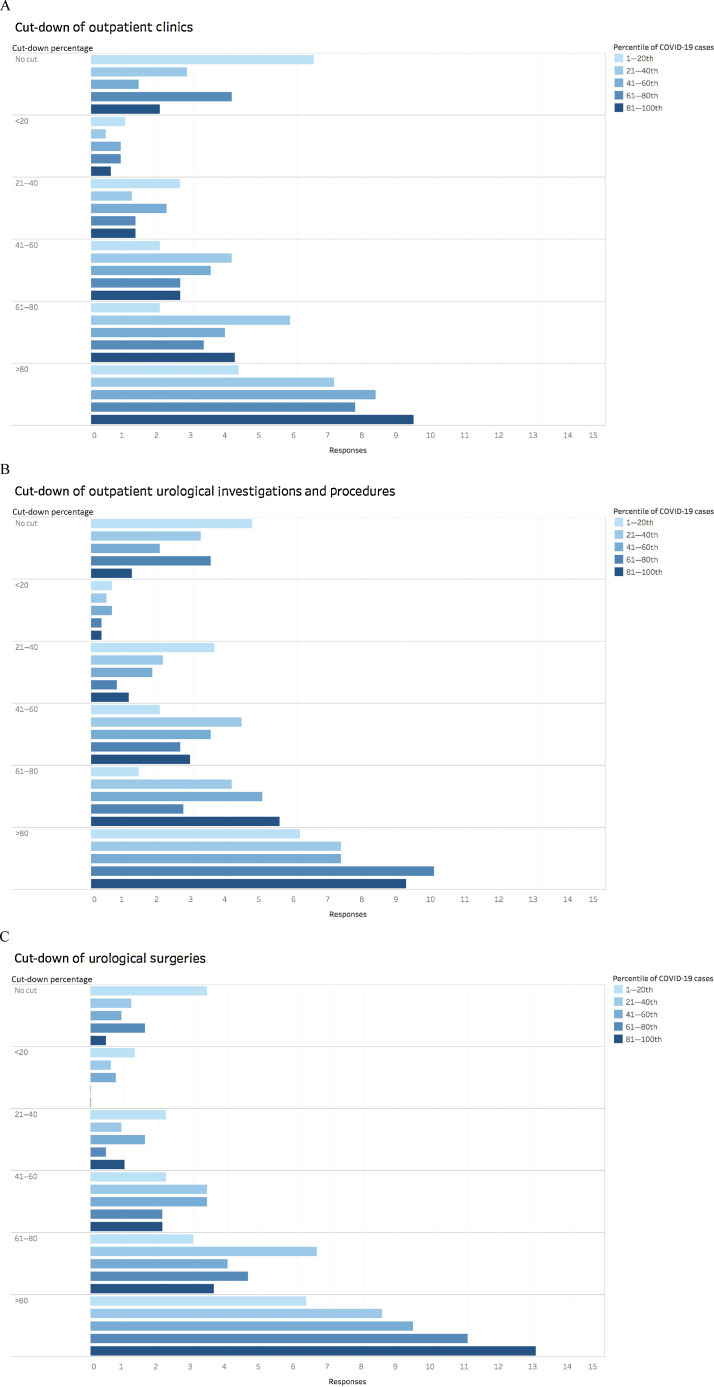
3.3. Impact of COVID-19 by the degree of outbreak
Overall, there was significant cut-down across different types of urological services (Fig. 2 ). Of note, there was 81–100% cut-down of outpatient clinic appointments in 37%, outpatient investigations and procedures in 40%, and urological surgeries in 48%, as reported by the respondents. The degree of cut-down of urological services also increased with the percentiles of COVID-19 cases. Respondents based in the lowest outbreak countries (1–20th percentile) had the highest proportion of no cut-down, and respondents based in the highest outbreak countries (81–100th percentile) had the highest proportion of cut-down. These observations were consistent across the various types of urological services.
Fig. 2.
The impact of COVID-19 on cut-down of (A) outpatient clinics, (B) outpatient investigations and procedures, and (C) urological surgeries, stratified by percentile of COVID-19 cases. COVID-19 = coronavirus disease-19.
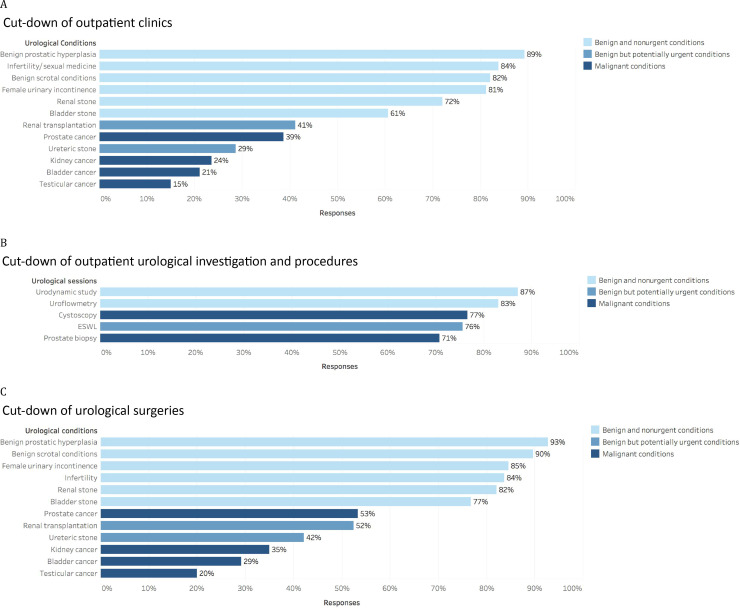
3.4. Impact of COVID-19 by the nature and urgency of urological conditions
Outpatient clinics for benign conditions including benign prostatic hyperplasia, infertility and sexual medicine, benign scrotal conditions, female urinary incontinence, renal stone, and bladder stone were most affected. However, benign but potentially urgent urological conditions such as renal transplantation and ureteric stone were less affected. Outpatient clinics for malignant conditions including prostate cancer, kidney cancer, bladder cancer, and testicular cancer were also less affected (Fig. 3A).
Fig. 3.
The impact of COVID-19 on cut-down of (A) outpatient clinics, (B) outpatient urological investigations and procedures, and (C) urological surgeries, by the nature and urgency of urological conditions. COVID-19 = coronavirus disease-19; ESWL = extracorporeal shock wave lithotripsy.
There was significant cut-down across various types of outpatient investigations and procedures (Fig. 3B). Prostate biopsy, ESWL, and cystoscopy were affected; other nonurgent outpatient investigations and procedures, such as urodynamic study and uroflowmetry, were affected even more.
Among urological surgeries, those for benign conditions were cut down the most (Fig. 3 C). In particular, surgeries for benign prostatic hyperplasia, benign scrotal conditions, female urinary incontinence, infertility, renal stones, and bladder stones had the highest rates of cut-down. Other urological surgeries for benign but potentially urgent conditions, such as renal transplantation and ureteric stone surgery, were less affected. Surgeries for urological cancers were also less affected.
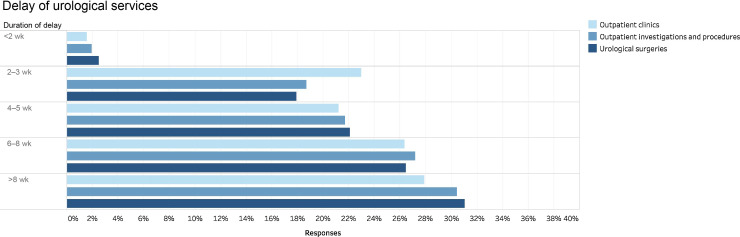
3.5. Impact of COVID-19 on delay of urological services
There was delay across the different types of urological services (Fig. 4 ). Of note, a delay of >8 wk was reported for 28% of outpatient clinics, 30% of outpatient investigations and procedures, and 31% of urological surgeries. Of the respondents, 47% believed that the accumulated workload could be dealt with in a timely manner after the COVID-19 outbreak, but 50% thought that the postponement of urological services would affect the treatment and survival outcomes of their patients.
Fig. 4.
The impact of COVID-19 on the delay of urological services. COVID-19 = coronavirus disease-19.
4. Discussion
To our knowledge, this is the first survey to examine the global impact of COVID-19 on urological care, including a large sample of urology professionals from six continents. Regarding the demographics of our survey respondents, 71% were consultants, 56% were in teaching hospital or academic institution, and 71% practised general urology. According to the workforce report by the British Association of Urological Surgeons [13], 77% of the urologists were consultants. According to the census report by the American Urological Association (AUA) [14], 46% of the urologists were practising under institutional settings and 60% were general urologists. According to a census report in China [15], 78% were practising urologists (nonresident) and 43% of the hospitals were tertiary institutions. Our survey respondents have reasonable representativeness globally in terms of the level of training, types of hospital and institution, and urology speciality. The majority of respondents indicated that their hospitals were taking care of COVID-19–positive patients, and 26% of urologists were deployed to assist with COVID-19 care.
Simultaneously, our survey revealed substantial disruptions in urological care and an overall reduction in clinical volume. As expected, the greatest cut-down was observed in geographical areas with the highest number of COVID-19 cases. Although the greatest reduction in outpatient clinical volume was observed for benign and nonurgent conditions, outpatient management of oncological and benign but potentially urgent conditions have also been delayed in multiple regions. Outpatient procedures such as prostate biopsy and cystoscopy were being delayed in most cases, which might raise concerns based on the assumption that these procedures are performed for suspected prostate cancer and bladder cancer.
We also observed substantial delay in surgical management, with the least delay for testicular and bladder cancer. All other surgical procedures were cut back in one-third or more of cases, including other uro-oncology procedures. Indeed, recent studies have suggested significant risk involved with elective surgery in the context of COVID-19. A retrospective cohort study of 34 asymptomatic patients who underwent elective surgery during the COVID-19 incubation period reported that 44% required intensive care and 20% died [16]. In addition to potential risks to the patient, the operative team may also be exposed to significant risk of infection. Some hospitals have adopted policies of testing patients prior to surgery; however, in other settings, rapid testing is not readily available. The long-term impact of these delays in surgical management will require future study.
Our study found that the number of COVID-19–related screening tests being performed on patients can be increased; 80% routinely ask patients about upper respiratory symptoms, 75% ask about fever, and only 66% ask about a TOCC history. Despite the fact that screening for symptoms is not universal and that asymptomatic transmission of COVID-19 is known to occur [17], only 56% of the providers wear PPE in their practice.
More than one-third of respondents reported COVID-positive staff at their institutions and nearly half of the participating urologists expressed fear of going to work. Recent reports have highlighted a significant impact on the mental health of health care workers involved in COVID-19 care. Among 1257 health care workers working at Chinese hospitals with COVID-19 cases, 50% reported depression, 45% had anxiety, 34% had insomnia, and 72% had distress, based on validated questionnaires [18]. Long-term effects on the mental health of health care workers remain to be seen but will likely to have profound effects in the future.
A recent study held listening sessions with different health care professionals about the sources of anxiety during COVID-19 [19]. The eight key themes that emerged were as follows: (1) having appropriate PPE, (2) exposing family members to the infection, (3) access to testing and fear of propagating the infection at work, (4) uncertainty that their organisation would take care of their needs if they become infected, (5) access to childcare during work hours, (6) support for other personal and family needs, (7) providing competent medical care if deployed to a new area, and (8) up-to-date information and communications [19]. Many of these themes were expressed by urologists in our survey. Most urologists did not feel that they had sufficient PPE. Only 32% received training in PPE and 14% were comfortable with their training in infectious disease. Only about half of urologists felt that their hospital administration's response to the situation was adequate. In addition, 60% of urologist respondents anticipate reduced compensation as a result of the COVID-19 pandemic.
Another consequence of COVID-19 for urologists is the cancellation of all major professional society meetings in the field for 2020. However, many groups such as the EAU and AUA have planned to conduct virtual activities in lieu of the in-person meetings. In the meantime, both societies have dedicated websites with COVID-19 resources. The EAU website includes free access to COVID-19-related publications in European Urology, EAU Rapid Reaction Recommendations, Robotic Guidelines from the European Robotic Urology Section, and patient information videos about COVID-19 available in multiple languages [20]. The AUA COVID-19 information centre has sections on how to implement telemedicine, triaging of urological surgery, and other timely topical issues [21].
COVID-19 has led to substantial interruption of other aspects of on-going urology education around the world, with nearly half of the respondents reporting cancellation of important meetings such as grand rounds and journal club. To address this issue, several online lecture series have been initiated to provide on-going education [22], [23]. For example, the Urology Collaborative Online Video Didactics (COVID) is a lecture series conducted on Zoom, in which urology faculty from participating programmes provide 1-h didactic sessions with questions and answers. Similarly, the New York section of the AUA has initiated the Educational Multi-institutional Program for Instructing Residents (EMPIRE) urology lecture series to engage residents in learning activities throughout the COVID-19 crisis.
On a positive note, many of these new electronic lecture series are being recorded to build a lasting resource for urology education. Similar activities are being conducted across a variety of medical specialities with positive results. For example, Kogan et al. [24] reported that their virtual orthopaedic conferences are recording higher attendance than under normal circumstances and have positive reviews. To the extent possible, every opportunity should be made to maintain or even improve upon urological educational opportunities even during periods of local quarantine to foster the forward progression of the speciality.
There are several limitations in our study. We recognised a strong representation from Asia, Europe, and North America, but limited representation from Africa, Australia, and New Zealand. The survey was available only in English, and this may introduce a biased representation of English-speaking countries. As this survey was conducted in the midst of the pandemic, it is also possible that urologists in some of the most heavily involved regions were involved in the emergency response and unable to participate. Furthermore, even within individual countries, there are large regional differences in COVID-19 prevalence. Unfortunately, our sample size precludes the ability to provide more granular data beyond the continent or country level. Moreover, cut-down of services may be a result of government shutdown polices, and this was not adequately covered by our survey. In order to provide a timely report on the current COVID-19 situation, we spent a total of 9 d only for data collection. Although we have collected >1000 responses, this number is considered low given the large number of organisations being involved in this survey. Despite these limitations, this study provides an initial global perspective on the impact of COVID-19 on urological practice and care. Future studies should be conducted to re-examine the impact of COVID-19 in urology with additional follow-up.
5. Conclusions
The COVID-19 pandemic has imposed great challenges to urology health care providers globally. The diversion of personnel in order to facilitate the COVID-19 emergency response has affected the maintenance of urology departmental activities. A substantial proportion of urologists reported insufficient training and protective equipment. In terms of patient care, significant cut-down was observed in urology clinics, outpatient procedures, and major surgeries, corresponding to the degree of outbreak. Benign urological conditions were more affected than malignant urological conditions. The long-term repercussions on the urological patients’ outcome from the deferred diagnosis and treatment remain to be defined.
Author contributions : Jeremy Yuen-Chun Teoh had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Teoh, Ong, Gonzalez-Padilla, Castellani, Dubin.
Acquisition of data: Teoh, Gonzalez-Padilla, Castellani, Dubin, Esperto, Campi, Gudaru, Wroclawski.
Analysis and interpretation of data: Teoh, Ong, Gonzalez-Padilla, Castellani, Dubin, Talwar.
Drafting of the manuscript: Teoh, Ong, Esperto, Campi, Okhunov.
Critical revision of the manuscript for important intellectual content: Teoh, Dubin, Ng, Jain, Gauhar, Wong, Loeb.
Statistical analysis: Teoh, Ong.
Obtaining funding: Teoh, Ng.
Administrative, technical, or material support: None.
Supervision: Teoh, Tanidir, Rivas, Tiong, Loeb.
Other: None. Financial disclosures: Jeremy Yuen-Chun Teoh certifies that all conflicts of interest, including specific financial interests and relationships and affiliations relevant to the subject matter or materials discussed in the manuscript (eg, employment/affiliation, grants or funding, consultancies, honoraria, stock ownership or options, expert testimony, royalties, or patents filed, received, or pending), are the following: Jeremy Yuen-Chun Teoh has received honorarium from Olympus and Boston Scientific, travel grants from Olympus and Boston Scientific, and research grants from Olympus and Storz. Stacy Loeb reports reimbursed travel from Sanofi and equity in Gilead. Funding/Support and role of the sponsor : Stacy Loeb is supported by the Edward Blank and Sharon Cosloy-Blank Family Foundation.
Associate Editor: James Catto
Footnotes
Supplementary data associated with this article can be found, in the online version, at https://doi.org/10.1016/j.eururo.2020.05.025.
Appendix A. Supplementary data
The following are the supplementary data to this article:
References
- 1.World Health Organization . World Health Organization; Geneva, Switzerland: April 12, 2020. Coronavirus disease (COVID-19) pandemic. [Google Scholar]
- 2.Bogoch I.I., Watts A., Thomas-Bachli A., Huber C., Kraemer M.U.G., Khan K. Pneumonia of unknown aetiology in Wuhan, China: potential for international spread via commercial air travel. J Travel Med. 2020;27:taaa008. doi: 10.1093/jtm/taaa008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Worldometer . Worldometer Web site; April 12, 2020. COVID-19 coronavirus pandemic. [Google Scholar]
- 4.World Health Organization . World Health Organization; Geneva, Switzerland: March 3, 2020. Shortage of personal protective equipment endangering health workers worldwide. [Google Scholar]
- 5.Chan MC, Yeo SEK, Chong YL, Lee YM. Stepping forward: urologists’ efforts during the COVID-19 outbreak in Singapore. Eur Urol. In press. 10.1016/j.eururo.2020.03.004. [DOI] [PMC free article] [PubMed]
- 6.Nowroozi A, Amini E. Urology practice in the time of COVID-19. Urol J. In press. 10.22037/uj.v0i0.6065. [DOI] [PubMed]
- 7.Gudaru K., Blanco L.T., Castellani D. Connecting the urological community: the #UroSoMe experience. J Endoluminal Endourol. 2019;2:e20–e29. [Google Scholar]
- 8.COntrol ECfDPa . April 13, 2020. Geographic distribution of COVID-19 cases worldwide. [Google Scholar]
- 9.World Health Organization . World Health Organization; Geneva, Switzerland: 2001. Quantifying environmental health impacts: subregional country groupings for the global assessment of disease burden. [Google Scholar]
- 10.American College of Surgeons . 2020. COVID-19: guidance for triage of non-emergent surgical procedures.https://www.facs.org/about-acs/covid-19/information-for-surgeons/triage [Google Scholar]
- 11.Sterne J.A., White I.R., Carlin J.B. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ. 2009;338:b2393. doi: 10.1136/bmj.b2393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jakobsen J.C., Gluud C., Wetterslev J., Winkel P. When and how should multiple imputation be used for handling missing data in randomised clinical trials—a practical guide with flowcharts. BMC Med Res Methodol. 2017;17:162. doi: 10.1186/s12874-017-0442-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.British Association of Urological Surgeons and The Specialist Advisory Committee in Urology . November 2017. Workforce report.https://www.baus.org.uk/_userfiles/pages/files/About/Governance/2017 Workforce Report.pdf [Google Scholar]
- 14.American Urological Association . 2019. The state of the urology workforce and practice in the United States.https://www.auanet.org/research/research-resources/aua-census/census-results [Google Scholar]
- 15.Sun Y., Zhou L., Zhang J. Census report on Chinese urological surgeons. Asian J Urol. 2020;7:149–160. doi: 10.1016/j.ajur.2019.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lei S, Jiang F, Su W, et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine. In press. 10.1016/j.eclinm.2020.100331. [DOI] [PMC free article] [PubMed]
- 17.Bai Y., Yao L., Wei T. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020;323:1406–1407. doi: 10.1001/jama.2020.2565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lai J., Ma S., Wang Y. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3:e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shanafelt T, Ripp J, Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA. In press. 10.1001/jama.2020.5893. [DOI] [PubMed]
- 20.European Association of Urology . 2020. COVID19 resources for urologists.https://uroweb.org/covid19-resources-for-urologists/ [Google Scholar]
- 21.American Urological Association Information Center . 2020. Coronavirus disease 2019.https://www.auanet.org/covid-19-info-center/covid-19-info-center [Google Scholar]
- 22.Amparore D, Claps F, Cacciamani GE, et al. Impact of the COVID-19 pandemic on urology residency training in Italy. Minerva Urol Nefrol. In press. 10.23736/S0393-2249.20.03868-0. [DOI] [PubMed]
- 23.Porpiglia F, Checcucci E, Amparore D, et al. Slowdown of urology residents’ learning curve during COVID-19 emergency. BJU Int. In press. 10.1111/bju.15076. [DOI] [PMC free article] [PubMed]
- 24.Kogan M, Klein SE, Hannon CP, Nolte MT. Orthopaedic education during the COVID-19 pandemic. J Am Acad Orthop Surg. In press. 10.5435/JAAOS-D-20-00292. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.