Abstract
Background
Chronic obstructive pulmonary disease (COPD) is a major cause of morbidity and mortality, especially in low- and middle-income countries (LMICs) such as India. Medicine costs are a key issue in LMICs, with typically high patient co-payments. In addition, pharmacists are underutilised in LMICs, including India. However, pharmacist-led educational interventions may improve the care of patients with COPD, as well as reduce medicine costs. Consequently, the objective of this study was to assess the effectiveness of a pharmacist-led intervention in reducing medicine costs.
Methodology
We assessed the impact of a pharmacist intervention on direct medicine costs in COPD patients (medicine costs and pharmacist time) in a randomised controlled study involving an intervention and control group, conducted at a tertiary care teaching hospital in India.
Results
The 6-monthly cost of medicines at baseline increased with disease severity, from a maximum of US$29.46 for those with mild COPD to US$63.28 for those with very severe COPD. Substantial savings in medical costs were achieved with the pharmacist-led programme, to a maximum of US$20.49 over 6 months for very severe patients. This equates to a reduction of 30.6% in medicine costs (p < 0.001), reduced to 26.1% when pharmacists’ time (US$3.00/patient) was included.
Conclusion
There could be a key role for pharmacists as educators for COPD patients in LMICs, to improve care and reduce costs, including patient co-payments.
Key Points for Decision Makers
| Chronic obstructive pulmonary disease is the fourth leading cause of death globally. Moreover, 90% of COPD-related deaths typically occur in low- and middle-income countries (LMICs), including India. |
| In India, medicine costs currently represent a major proportion of the total healthcare costs (approximately 38%). Consequently, there is a need to address this, especially if most medicine costs are out-of-pocket. |
| A clinical pharmacist-led intervention reduced the costs of medicines for patients with COPD by up to 30.6%, while improving medication adherence and health-related quality of life, with savings marginally lower once the costs of pharmacist’s time were included |
| This intervention is feasible and pragmatic and could potentially be implemented across India and in other LMICs given concerns regarding the paucity of physicians, availability of pharmacists, and cost savings, as India and other LMICs move towards universal access. |
Introduction
Chronic obstructive pulmonary disease (COPD) is a preventable and treatable disease characterised by airflow limitation and obstruction [1, 2]. It is not fully reversible (unlike asthma) and is usually progressive [1]. However, early diagnosis and treatment, including smoking cessation, reduces the rate of decline in lung function and is seen as beneficial [3, 4].
Interest in COPD has grown in recent years across countries, including India, with an estimated global prevalence of 210 million people, and rising, and with prevalence rates in India averaging 4.2%, ranging from 1 to 10% or higher depending on the State [2, 5–9]. COPD is a major cause of morbidity and mortality [2, 6, 10, 11], and is currently the fourth leading cause of death globally, and likely to become the third leading cause by 2020 [4, 10, 12]. Overall, 90% of COPD-related deaths typically occur in low- and middle-income countries (LMICs), with India and China accounting for two-thirds of these [2, 13]. Currently in India, chronic respiratory diseases are the third highest cause of mortality, accounting for 11% of all deaths [6, 14], with COPD the greatest contributor at 8.7% of all deaths, resulting in over 400,000 deaths a year [6, 8]. As a result, deaths due to COPD in India are over four times higher than that seen among developed countries [10, 15]. In LMICs such as India, lower socioeconomic status, including poor nutrition and childhood poverty, limited education and health literacy, as well as higher exposure to particulate matter in the air, are major causes of increased mortality due to COPD [16–21]. In 2005, Murthy and Sastry reported that the incidence of COPD is higher in rural vs. urban India, with lower socioeconomic status being one of the major causes [22].
Of the total global disability-adjusted life-years (DALYs) due to chronic respiratory diseases, 32.0% currently occur in India [6], with COPD in India currently accounting for 4.8% of the total worldwide DALYs [6]. COPD is also associated with considerable economic burden, which is increasing [23–27]. In the US in 2010, the projected annual cost of COPD was $49.9 billion, including $29.5 billion of direct medical costs [24]. In China, current annual direct medical costs for COPD are US$30.30 billion, direct non-medical costs are US$1.36 billion, and indirect costs are US$5.28 billion, with hospitalisations accounting for 56.7% of total costs [25]. In Korea, the estimated costs for COPD in 2018 were approximately US$1.245 billion, with direct medical costs accounting for approximately 20% of this cost [23]. In Germany, the annual excess cost of COPD per patient in 2012, compared with healthy subjects, varied on average from €2595 for Global Initiative for Chronic Obstructive Lung Disease (GOLD) grade 1 patients to €8924 for grade 4 patients for direct costs, and €8621 for GOLD grade 1 patients, rising to an average of €27,658 for grade 4 patients, for indirect costs [27]. In Italy, the average healthcare costs for patients with severe COPD is €6700 per patient per year, a substantial proportion of which are hospitalisations (over 60%) [28], while, in Spain, the average healthcare cost of COPD per patient per year is approximately €2000, with medicines comprising approximately 40% of costs [29, 30].
The current economic burden of COPD in India is largely unknown [8], although Patel et al. calculated direct medical costs were up to Indian Rupees (INR) 5876.00 (US$88.23) per patient from admission to discharge among hospitalised patients, with the cost of medicines constituting a substantial proportion, at over five times the hospital charges [31]. This is very different to the situation in higher-income countries. Naveed et al. calculated an average annual total direct cost per patient for COPD of INR5000 (US$75.08) to INR25,000 (US$375.38), which is considerably higher than the direct medical costs for asthma, at INR1000–20,000 (US$15.02–300.30) [32]. A substantial proportion of these costs in India will be out-of-pocket [8, 33].
The morbidity, mortality and costs associated with COPD are enhanced if patients with COPD face both adherence and inhaler use barriers [34–38]. As a result, multifactorial approaches that include comprehensive health education for COPD patients in all aspects of care should be considered [1]. As mentioned, effective integrated interventions in ambulatory care, including earlier diagnosis and instigating strategies to help prevent disease progression, can reduce the rate of exacerbations and hospitalisations and the rising economic burden of COPD [39–43]. In the GOLD report of 2018, pharmacists are considered as key healthcare professional collaborators assisting in the management of COPD through educational strategies [1]. Pharmacists can help with medication management strategies as well as assist with addressing barriers to the use of, and adherence with, prescribed inhalers. Consequently, community pharmacists can potentially help reduce the morbidity, mortality and costs associated with COPD and delay its progression [44–47].
This is particularly important in India, given concerns with the number of physicians, especially in rural areas, due to a variety of issues [48–50]. As a result, counselling of COPD patients in terms of prevention strategies and inhaler techniques, as well as the use of spirometry for diagnosis, is typically limited [51]. This is a concern given the high levels of co-payment in India, which can have a devastating effect on families [8, 52, 53], as well as the current high burden of COPD in India [2, 6, 13]. Consequently, effective strategies are needed to address this, including the improved use of medicines to reduce subsequent co-payments [22]. We and others have shown that structured pharmacist-led interventions can improve the care of patients with COPD and help reduce costs [46, 54–58]. This is important, with the role of non-physician healthcare professionals growing in India to compensate for the lack of physicians [59]. Currently, there are over 1 million pharmacists in India, with a clinically oriented Doctor of Pharmacy (PharmD) programme introduced in 2008 to help train pharmacists to provide patient-related care. This includes patient counselling and therapeutic interventions, which should help to improve the care of patients with chronic diseases in India [53]. However, there are limited data regarding the economic impact of pharmacists’ involvement in the management of patients with COPD in India, especially with respect to medicine costs.
Consequently, we undertook this study to address this by evaluating the impact of clinical pharmacists’ intervention on the costs of medicines for patients with COPD, in a randomised trial, coupled with the costs of pharmacists’ time, to provide future guidance as India moves towards providing universal healthcare [60]. We concentrated on these two direct medical costs initially since the costs of medicines currently account for approximately 38% of total healthcare costs in India vs. approximately 10% of total healthcare costs among developed countries, much of which is out-of-pocket [33, 53, 61, 62]. In addition, as mentioned, costs of medicines for patients with COPD is currently appreciably higher than hospital charges [31].
Patients and Methods
Study Design and Subjects
The study was carried out as part of a larger study evaluating the impact of structured pharmacist-led interventions on improving medication adherence in patients with COPD, and the subsequent impact on their health-related quality of life [44, 46].
An open-label, randomised controlled study was conducted at Kasturba Medical College Hospital, Manipal, India, a tertiary care teaching hospital, over a 3-year period. Study subjects were selected based on the inclusion criteria (confirmed diagnosis of COPD as per the GOLD guidelines) and participants’ informed consent. Patients were randomised (by sealed envelope method) into two groups—the intervention group (IG) and the control group (CG)—to ensure, as far as possible, matching between the two groups.
Sample Size
Based on previous published literature [54, 55], we estimated a minimum sample size (based on measures of variation) of 100 patients in each group in order to demonstrate minimum clinical significance of 5% (power = 80%). The target sample size was estimated to be 260 patients (130 CG and 130 IG), taking into account a 30% potential dropout rate.
Treatment Costs
Medicine costs collected before and after the intervention were based on the data collected from case record forms (CRFs) and personal interviews. The cost of medicines included the cost of glucocorticoids, anticholinergics, antibiotics, methylxanthines and bronchodilators, excluding any medicines that were returned and could be re-used. The cost of medicines used to treat non-respiratory conditions were also excluded as we wanted to concentrate solely on the cost of medicines for COPD.
Medicine costs for each patient were collected from the billing system in the hospital. These were collated from the hospital pharmacy billing system for the three data collection time points, and recorded on the CRFs as total combined costs, without being broken down into their respective components (different inhalers and oral medicines). In addition, during the patient interviews, information regarding over-the-counter (OTC) medicines and their costs were collected, as well as the cost of any other medicines purchased from outside the hospital, to ensure all medicines costs were included. Costs were collected for the fiscal year 2012–2014, in INR, and inflated to 2017 costs using current Indian inflation rates [63]. These costs were subsequently converted to 2017 US$ using an average exchange rate of US$1 = INR66.60). The costs were grouped into periods of 6 months for comparative purposes (6 months prior to the documented time, i.e. 6 months before baseline, as well as the 6-month period prior to 12 and 24 months). A 6-month period was chosen to cover possible monthly fluctuations in inhaler use.
Since variation in the severity of COPD disease may affect the median estimated direct costs for patients in each group, the cost difference in the median estimated costs between the two groups was also assessed using the cost ranges in each group via box plots.
The cost of the clinical pharmacy input was also calculated to provide a more complete picture of overall potential cost savings. This was based on an average monthly salary of a clinical pharmacist in India in 2017 being approximately INR28,000 (US$420), although it may vary according to the clinical pharmacist’s qualifications and experience [64]. Typically, a clinical pharmacist in India works 8 h/day for 25 days a month, equating to 200 working hours a month. This corresponds to INR140 (US$2)/h.
As mentioned, no attempt was made to look at the impact of any changes in medicine use on longer-term costs, including future hospitalisations due to exacerbations, as the main emphasis was on the cost of medicines (the principal cost component) [31], much of which will be out-of-pocket [8, 33].
In addition, we had previously shown that this structured pharmacist-led intervention significantly improved medication adherence in COPD patients, which has been shown to decrease the number of emergency department visits and and the length of stay in hospitals among patients with chronic respiratory diseases [46, 65].
Assessments
The baseline data for each patient were collected using a custom-designed and validated CRF that we have previously used and discussed [46]. The collected data included demographic measures, clinical characteristics, and respiratory and non-respiratory medication regimens. Follow-up assessments were repeated at 12 and 24 months in both the CG and IG cohorts.
Structured Pharmacist Intervention
Patients recruited in the IG were educated by the principal clinical pharmacist (SAb). The counselling sessions (typically 15–20 min) and patient information leaflets (PILs) emphasised the following: (1) the importance of medication compliance; (2) the dose and frequency of the prescribed medicines; (3) the need for smoking cessation; (4) the need for simple exercise; (5) the proper use of prescribed inhaler devices; and (6) the need for timely monitoring by the Pulmonary Medicine Department. Five counselling sessions were conducted during the 2-year follow-up period.
Each patient was followed up for a period of 2 years, and adherence was re-assessed every 6 months. PILs describing the above techniques had been developed, validated, and supplied to patients for reinforcing the content delivered through counselling [66]. Patients were further contacted by telephone each month to enhance medication adherence and timely follow-up. During the follow-up, patients in the IG were further trained regarding the proper use of inhaler devices, and motivated regarding the need for medication adherence.
The control patients received normal care in the clinic, without any pharmacy counselling and follow-up by the clinical pharmacy team.
Data Analysis
SPSS version 20.0 (IBM Corporation, Armonk, NY, USA) was used for statistical analyses (data screening, descriptive statistics and univariate analysis). A p value < 0.05 was considered statistically significant.
Results
Patient Flow and Baseline Characteristics
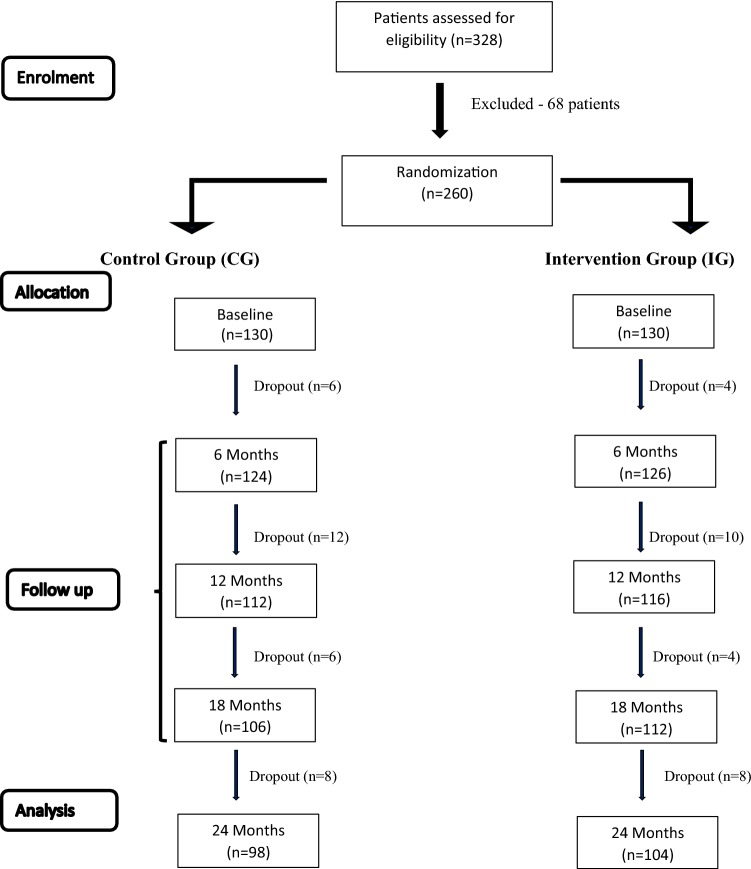
Of the 328 COPD patients screened during the study period, 260 were recruited, of whom 202 completed the follow-up (98 in the CG and 104 in the IG). The reasons for dropping out, in decreasing order of events, were: [1] lost to follow-up (18 in the CG and 11 in the IG); [2] death (8 in the CG vs. 9 in the IG); and [3] withdrawal at different stages of the study (5 in the CG vs. 3 in the IG). Figure 1 indicates the number of patients at different stages of the study.
Fig. 1.
Flow chart indicating patient numbers at different stages of the study
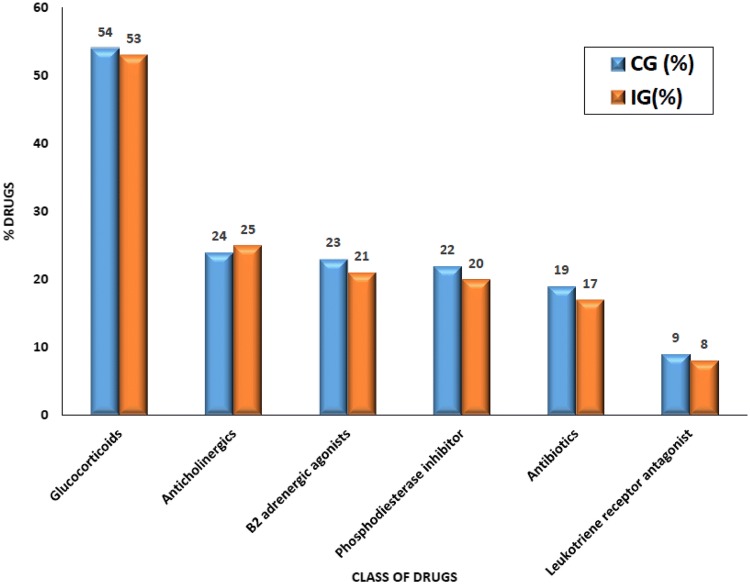
The randomisation process ensured the CG and IG cohorts were matched for baseline, sociodemographic and clinical characteristics (Table 1), including (1) mean age (61.1 ± 8.4 vs. 60.6 ± 7.9 years); (2) male sex (94.4 vs. 96.9%); (3) duration of COPD (15.3 ± 5.7 vs. 14.6 ± 6.6 years); (4) mean forced expiratory volume in 1 s (FEV1) percentage (41.9 ± 14.7 vs. 44.4 ± 14.5); (5) average number of medicines used (7.2 ± 2.1 vs. 6.3 ± 1.7); (6) comorbidity rate (74% vs. 69%); and (7) current smoking status (53.8% vs. 56.9%). The groups were also matched in terms of baseline medicines (Fig. 2).
Table 1.
Baseline characteristics of the study population
| Characteristics | CG | IG | p value |
|---|---|---|---|
| Male sex (%)a | 94.4 | 96.9 | 0.08 |
| Age, years (mean ± SD)b | 61.1 ± 8.4 | 60.6 ± 7.9 | 0.67 |
| Age category, yearsa | 0.12 | ||
| 40–50 | 20 | 15 | |
| 50–60 | 32 | 47 | |
| 60–70 | 78 | 68 | |
| Socioeconomic status (%)a | 0.73 | ||
| Lower | 35.8 | 37.4 | |
| Upper lower | 30.5 | 29.8 | |
| Middle | 23.7 | 20.6 | |
| Upper middle | 7.1 | 6.4 | |
| Upper | 2.9 | 5.8 | |
| FEV1 % predictedc (mean ± SD)b | 41.9 ± 14.7 | 44.4 ± 14.5 | 0.16 |
| Severity as per GOLD (%)a | 0.34 | ||
| Mild | 12.7 | 13.8 | |
| Moderate | 21.9 | 20.1 | |
| Severe | 45.4 | 47.6 | |
| Very severe | 20.0 | 18.5 | |
| Pack years (mean ± SD)b | 21.7 ± 12.6 | 23.2 ± 11.4 | 0.42 |
| Smoking status (%)a | 0.24 | ||
| Ex-smoker | 43.1 | 46.2 | |
| Current smoker | 56.9 | 53.8 | |
| Duration of COPD (mean ± SD)b | 15.3 ± 5.7 | 14.6 ± 6.6 | 0.36 |
| Comorbid conditions (%)a | 74 | 69 | 0.64 |
| No. of medications (mean ± SD)b | 7.2 ± 2.1 | 6.3 ± 1.7 | 0.68 |
IG intervention group, CG control group, SD standard deviation, FEV1 forced expiratory volume in 1 s, COPD chronic obstructive pulmonary disease, GOLD Global Initiative for Chronic Obstructive Lung Disease
aData were analysed using the Chi square test
bData were analysed using the t test
cFEV1 was calculated based on spirometry
Fig. 2.
Medicines prescribed in each group (CG and IG) as a percentage of the total medicines prescribed (items). CG control group, IG intervention group
As per Kuppuswamy’s socioeconomic classification [67], the largest proportion of patients belonged to the upper lower category in both groups (CG 30.5% vs. IG 29.8%). The ‘smoking score’ (pack-years) was estimated to be 21.7 ± 12.6 in the CG and 23.2 ± 11.4 in the IG. The largest proportion of patients belonged to the GOLD III (severe) category (45.4 vs. 47.6%). The socioeconomic status of patients was based on published classifications [18].
Medicine Costs in Chronic Obstructive Pulmonary Disease (COPD) Patients
At baseline, the average medicine costs of the enrolled patients were highly correlated with disease severity. Box 1 lists the medicines prescribed/dispensed in both groups of patients to treat their COPD, with Fig. 2 giving a further breakdown showing similar use of the different medicine types between both groups at baseline. Typically, these were different inhalers (short- and long-acting β2-agonists, corticosteroids and anticholinergics).
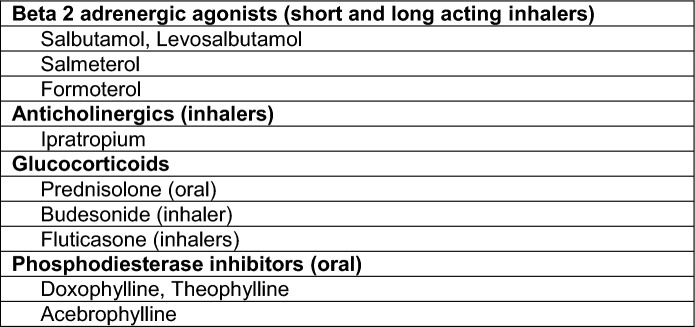
Box 1.
List of medicines most commonly prescribed/dispensed among patients with COPD
COPD chronic obstructive pulmonary disease
Mild COPD cost the least per patient for medicine costs at baseline (CG = US$29.46 vs. IG = US$27.44). Predictably, patients with very severe COPD incurred the highest medicine costs initially (CG = US$62.00 vs. IG = US$63.28) (Table 2).
Table 2.
Medicine costs (median) in COPD patients over a 6-month period, at baseline and prior to 24 months
| Severity of COPD | Baseline (US$) | 24 months (US$) | Medicine costs saved by a structured pharmacist-led intervention [US$ (%)] | Statistical significance of the reductions at 24 months | ||
|---|---|---|---|---|---|---|
| CG | IG | CG | IG | IGa (24 months) | p value (t test) | |
| Stage I (mild) | 29.46 | 27.44 | 41.47 | 31.46 | 10.01 (− 24.1) | < 0.001 |
| Stage II (moderate) | 35.41 | 38.35 | 42.28 | 35.03 | 7.25 (− 17.1) | < 0.001 |
| Stage III (severe) | 53.69 | 52.00 | 58.24 | 43.00 | 15.24 (− 26.2) | < 0.001 |
| Stage IV (very severe) | 62.00 | 63.28 | 66.94 | 46.45 | 20.49 (− 30.6) | < 0.001 |
CG control group, IG intervention group, COPD chronic obstructive pulmonary disease
aCompared with CG (24 months)
The cost of medicines decreased significantly after the pharmacist intervention in the IG for all COPD severity levels. For patients with mild COPD, the average 6-monthly medicine costs at 24 months were US$41.47 for the CG and US$31.46 per patient for the IG. For those with very severe COPD, the medicine costs were US$66.94 for the CG and US$46.45 per patient for the IG. Overall, the structured pharmacist-led intervention saved US$10.01 per patient for medicine costs over a 6-month period prior to 24 months for those patients with mild COPD vs. US$20.49 for those patients with very severe COPD, equating to a reduction ranging from 17.1% (moderate) to 30.6% (very severe) (Table 2).
Comparative Analysis of Medicine Costs Among COPD Patients
The cost differences in estimated medicine costs between the two groups were assessed using the cost ranges in each group, as shown in the box plots.
Estimated Median Medicine Costs Among COPD Patients at Baseline
The median estimated direct medicine costs at baseline were similar between the CG and IG cohorts (US$52.63 vs. US$51.73; p = 0.916). The medicine costs ranged from a minimum of US$26.84 in the CG and US$25.81 in the IG, to a maximum of US$62.13 (CG) and US$63.33 (IG). Figure 3 shows the box plot of the cost comparison between the CG and IG cohorts at baseline.
Fig. 3.
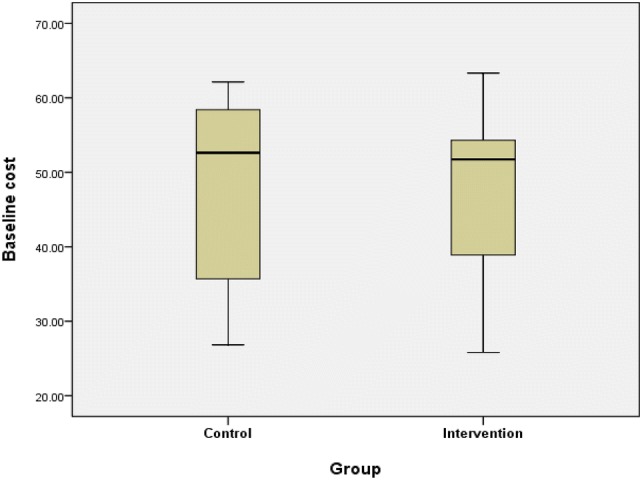
Box plot of medicine cost comparisons between the intervention and control groups at baseline [median (IQR)]. IQR interquartile range
Estimated Median Medicine Costs (US$) Among COPD Patients at 12 Months
The median estimated medicine costs at 12 months were significantly higher for the CG than the IG (US$56.09 vs. US$46.79; p < 0.001). The medicine costs ranged from a minimum of US$32.15 in the CG and US$26.45 in the IG, to a maximum of US$67.82 (CG) and US$60.01 (IG). Figure 4 shows the box plot of cost comparisons between the CG and IG cohorts at 12 months.
Fig. 4.
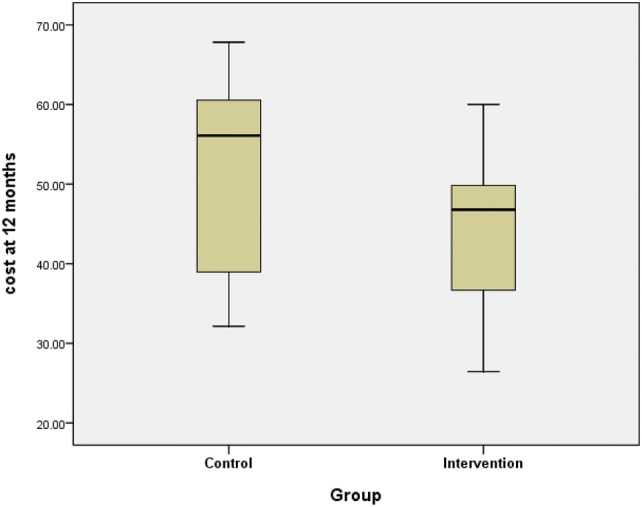
Box plot of medicine cost comparison between the intervention and control groups at 12 months [median (IQR)]. IQR interquartile range
Estimated Median Medicine Cost (US$) of COPD Patients at 24 Months
The median estimated medicine costs at 24 months were significantly higher for the CG than the IG (US$57.82 vs. US$41.29; p < 0.001). The medicine costs ranged from a minimum of US$39.09 in the CG and US$29.21 in the IG, to a maximum of US$68.09 (CG) and US$48.98 (IG). Overall, median medicine costs were reduced by 28.6% in the IG vs. CG cohorts. Figure 5 shows the box plot of cost comparisons between the CG and IG at 24 months.
Fig. 5.
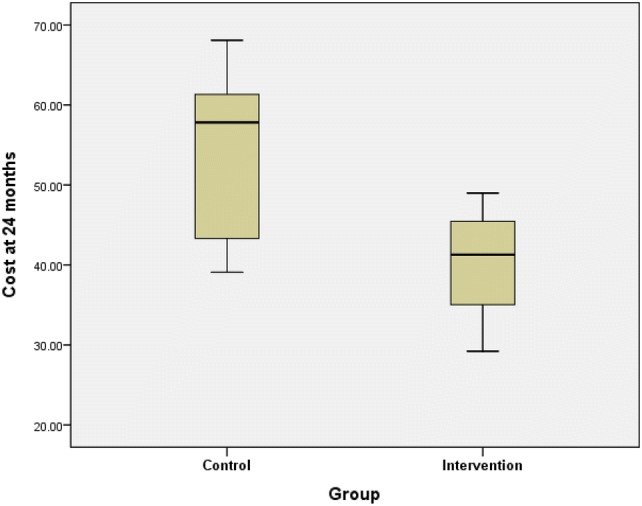
Box plot of medicine cost comparison between the intervention and control groups at 24 months [median (IQR)]. IQR interquartile range
Costs of Clinical Pharmacist Time
The time for counselling each COPD patient was found to be 20 min per patient, on average, during the five counselling sessions conducted in the study period. Consequently, the estimated average counselling time for each patient was 1 h 40 min (over the 2 years), which equates to INR200 (US$3) per COPD patient. The inclusion of these costs reduces potential savings, however they are still substantial (Table 3).
Table 3.
Potential direct medicine cost savings from the pharmacist intervention programme
| Severity of COPD | Median medicine cost saved by structured pharmacist-led intervention (US$) (Table 2) | Pharmacist costs (US$) | Overall savings (US$) | Overall percentage cost reduction from CG costs (Table 2) |
|---|---|---|---|---|
| Stage I (mild) | 10.01 | 3.00 | 7.01 | − 16.9 |
| Stage II (moderate) | 7.25 | 3.00 | 4.25 | − 10.1 |
| Stage III (severe) | 15.24 | 3.00 | 12.24 | − 21.0 |
| Stage IV (very severe) | 20.49 | 3.00 | 17.49 | − 26.1 |
CG control group, IG intervention group, COPD chronic obstructive pulmonary disease
Discussion
To the best of our knowledge, we believe this is the first randomised controlled study from India to evaluate the impact of a pharmacist-led intervention on the cost of medicines to treat patients with COPD. The savings can be substantial, reducing 6-monthly medicine costs among those with very severe COPD by US$20.49 to US$46.45, i.e. 30.6% (Table 2), with lower savings with milder COPD. These savings are still high at US$17.49 (a reduction of 26.1%) when factoring in clinical pharmacy time (Table 3), with a percentage reduction at 30.6% for those with very severe disease if we had evaluated medicine costs over 12 months rather than 6 months. The findings that the costs of medicines increase with disease severity is expected, similar to those of Hilleman and others [27, 31, 68]. These savings in medicine costs are important given the extent of co-payments for medicines for patients with COPD in both India and other LMICs [8, 33, 52, 53]. In India, most COPD patients are from rural areas, and, consequently, the cost of therapy remains a high burden for patients and their families. Affordability of medicines is a key issue in LMICs, with their costs accounting for up to 70% of total healthcare costs, most of which will be out-of-pocket and potentially catastrophic for patients and their families if family members become ill [52, 69].
By investing INR200 (US$3), per COPD patient, in pharmacist-led interventions, approximately US$7–US$18 can be saved in medicine costs in cases of mild and very severe disease, respectively (Table 3), but could be greater if we had evaluated medicine costs over 12 months rather than 6 months. Encouragingly, care appears not to be compromised with these savings. If anything, care appears to be improved with this pharmacist-led intervention, with findings from other parts of this research project showing improved adherence to medicines, as well as improved HRQOL in patients with COPD following the intervention [44, 46]. This is encouraging given the extent of COPD in India, and its current impact on morbidity, mortality and costs [5, 6, 8, 10, 15, 31].
Our study corroborates previous reports that demonstrate the value of pharmacist-driven patient educational activities among patients with COPD, reinforcing that medication adherence and inhaler technique are very important issues to discuss with patients at every follow-up visit, to improve their care and help reduce overall costs [47, 54, 55, 70]. In agreement with our study results (Table 2), other authors have also demonstrated that the introduction of self-management plans in COPD patients have economic benefits [57, 71]. Pharmacist led self-management plans can also minimise or help prevent medicine-related problems, avoiding unnecessary hospital admissions in patients with COPD [47]. From previous studies [29, 44–47, 65], it is clear that adherence to medication in patients with COPD leads to improved disease control, reducing drug dosages and frequency as well as the use of emergency medicines and hospitalisations. This ultimately reduces costs, including medicine costs. In contrast, poorly controlled COPD, which is typically associated with failure to use inhaled medications correctly, was estimated to increase costs in patients with COPD in Italy by at least €9 billion per year, with costs falling substantially with appropriate inhaler and other care [28, 72]. This is not surprising as adherence to inhaler therapy is typically low in routine care [73–75]. As a result, in the GOLD guidelines [1], COPD management is described as 10% medication and 90% education, with only 17% of patients achieving perfect medication adherence without assistance [76]. Consequently, based on our findings and those of others, we believe there is a potential role for pharmacists to educate patients about the importance of medication adherence to manage their COPD when dispensing the different inhalers and other prescribed medicines to treat their disease. This in turn will help to stabilise their disease and decrease overall medicines costs as well as overall costs (including pharmacists’ costs). This is particularly important in LMICs, with their high patient co-payments and current burden of COPD.
This should be of help to key stakeholder groups in India, with pharmacists currently a major healthcare work force, with over 1 million in practice in India [53]. Pharmacists are ideally placed in the healthcare system as they act as a link between patients and physicians, and are often the first healthcare professional that patients in LMICs approach with health-related problems [77]. They can also help review the quality of prescribing (including prescribing against agreed national guidance), which is currently being underutilised in India [78–81]. In addition, pharmacists can help address concerns with generics to reduce co-payments [82], as well as help limit tobacco smoking to reduce COPD [83–86], alongside other policies to reduce smoking. Other initiatives include increasing the cost of cigarettes and, through greater enforcement of legislation, prohibiting smoking in public places [22]. Consequently, we believe that our study endorses expanding the role of pharmacists as an economically viable strategy in India, as well as improving patient care, and we will be monitoring this in the future. This may also apply to other LMICs, especially those where there is currently high morbidity, mortality and costs due to COPD.
We are aware of a number of limitations with this study. The major limitation is that this study was conducted in only one centre in India, which could affect the generalisation of study findings to other institutions. However, we believe that in view of the robustness of the study design and the fact that pharmacy counselling skills are easily transferable, our findings are valid and provide future direction to others. We are also aware that we focused only on medicine costs in this study. In addition, we did not breakdown the medicine costs into different drug components (different inhalers and oral treatments). However, as mentioned, previous studies in India have shown that medicine costs are a substantial part of the overall costs of treating patients with COPD with typically low salaries, unlike high-income countries. Medicine costs can account for over 70% of total healthcare costs in LMICs, and, in India, much of this will be out-of-pocket, putting considerable strain on families when family members become ill, especially those in rural areas. Consequently, initiatives to reduce medicine costs while improving the care of patients with COPD should be welcomed.
Conclusions
We believe our study demonstrates a potentially pivotal role of pharmacists in reducing the direct medicine costs in COPD patients through a structured educational intervention. These savings can be achieved with minimal costs in terms of pharmacists’ time. Consequently, we believe our findings will be of interest to the authorities in both India and other LMICs with high morbidity, mortality and costs due to COPD.
Acknowledgements
The authors are grateful to Manipal College of Pharmaceutical Sciences, Manipal Kasturba Hospital, and Manipal Academy of Higher Education, Manipal, India, for their support during this study.
Author Contributions
SAb, MKU, MKM, SAl, AAAlr and AAAlf developed the concept for the study. SAb, MKU, and AAAlr undertook data collection and initial analysis, with further input from MKM, SAl, APM, and BBG. SAb, MKU, AAAlr and BBG undertook the initial draft of the manuscript, with all authors subsequently contributing to further drafts. All authors approved the final manuscript submitted for publication.
Data Availability
Further data are available upon reasonable request.
Compliance with Ethical Standards
Funding
No external funding was used for this study.
Conflict of interest
Suhaj Abdulsalim, Mazhuvancherry Kesavan Unnikrishnan, Mohan K. Manu, Saud Alsahali, Alian A. Alrasheedy, Antony P. Martin, Brian Godman, and Abubakr A Alfadl declare that they have no conflicts of interest.
Ethical standards
Institutional ethical clearance (IEC 88/2012) was obtained prior to commencement of the study, and the study was registered with the Indian Clinical Trial Registry (CTRI/2014/08/004848). Patients gave informed consent prior to enrolment, and patient confidentiality was maintained throughout the study in accordance with clinical trial practices.
Contributor Information
Suhaj Abdulsalim, Email: a.suhaj@gmail.com.
Mazhuvancherry Kesavan Unnikrishnan, Email: unnikrishnan.mk@nationalcollegeofpharmacy.org.
Mohan K. Manu, Email: manumohan73@gmail.com
Saud Alsahali, Email: ph-sms@hotmail.com.
Alian A. Alrasheedy, Email: alian-a@hotmail.com
Antony P. Martin, Email: a.p.martin@liverpool.ac.uk, Email: antony.martin@hcdeconomics.com
Brian Godman, Email: Brian.Godman@liverpool.ac.uk, Email: brian.godman@strath.ac.uk, Email: Brian.Godman@ki.se.
Abubakr A. Alfadl, Email: abubakr13@yahoo.com
References
- 1.GOLD. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. 2018 Report. https://goldcopd.org/wp-content/uploads/2017/11/GOLD-2018-v6.0-FINAL-revised-20-Nov_WMS.pdf. Accessed 28 Dec 2018.
- 2.Rajkumar P, Pattabi K, Vadivoo S, Bhome A, Brashier B, Bhattacharya P, et al. A cross-sectional study on prevalence of chronic obstructive pulmonary disease (COPD) in India: rationale and methods. BMJ Open. 2017;7(5):e015211. doi: 10.1136/bmjopen-2016-015211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Csikesz NG, Gartman EJ. New developments in the assessment of COPD: early diagnosis is key. Int J Chronic Obstruct Pulm Dis. 2014;9:277–286. doi: 10.2147/COPD.S46198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Welte T, Vogelmeier C, Papi A. COPD: early diagnosis and treatment to slow disease progression. Int J Clin Pract. 2015;69(3):336–349. doi: 10.1111/ijcp.12522. [DOI] [PubMed] [Google Scholar]
- 5.Jindal SK, Aggarwal AN, Gupta D, Agarwal R, Kumar R, Kaur T, et al. Indian study on epidemiology of asthma, respiratory symptoms and chronic bronchitis in adults (INSEARCH) Int J Tuberc Lung Dis. 2012;16(9):1270–1277. doi: 10.5588/ijtld.12.0005. [DOI] [PubMed] [Google Scholar]
- 6.The burden of chronic respiratory diseases and their heterogeneity across the states of India: the Global Burden of Disease Study 1990–2016. Lancet Glob Health. 2018;6(12):e1363–74. [DOI] [PMC free article] [PubMed]
- 7.Lopez-Campos JL, Tan W, Soriano JB. Global burden of COPD. Respirology. 2016;21(1):14–23. doi: 10.1111/resp.12660. [DOI] [PubMed] [Google Scholar]
- 8.Hossain MM, Sultana A, Purohit N. Burden of chronic obstructive pulmonary disease in India: status, practices and prevention. Int J Pulm Res Sci. 2018;2(5).
- 9.Landis SH, Muellerova H, Mannino DM, Menezes AM, Han MK, van der Molen T, et al. Continuing to Confront COPD International Patient Survey: methods, COPD prevalence, and disease burden in 2012–2013. Int J Chron Obstruct Pulm Dis. 2014;9:597–611. doi: 10.2147/COPD.S61854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stephen P, Mahalakshmy T, Manju R, Laksham KB, Subramani S, Panda K, et al. High prevalence of chronic respiratory symptoms among autorickshaw drivers of urban Puducherry, South India. Indian J Occup Environ Med. 2018;22(1):40–44. doi: 10.4103/ijoem.IJOEM_163_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jones PW, Brusselle G, Dal Negro RW, Ferrerd M, Kardose P, Levy ML, et al. Health-related quality of life in patients by COPD severity within primary care in Europe. Respir Med. 2011;105(1):57–66. doi: 10.1016/j.rmed.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 12.WHO. Global Health Observatory (GHO) data. Mortality and global health estimates; 2016. http://who.int/gho/mortality_burden_disease/en/. Accessed 28 Dec 2018.
- 13.Salvi SS, Manap R, Beasley R. Understanding the true burden of COPD: the epidemiological challenges. Prim Care Respir J. 2012;21(3):249–251. doi: 10.4104/pcrj.2012.00082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.WHO. Noncommunicable Diseases (NCD) Country Profiles: India; 2016. https://www.who.int/nmh/countries/ind_en.pdf?ua=1. Accessed 28 Dec 2018.
- 15.Lopez AD, Shibuya K, Rao C, Mathers CD, Hansell AL, Held LS, et al. Chronic obstructive pulmonary disease: current burden and future projections. Eur Respir J. 2006;27(2):397–412. doi: 10.1183/09031936.06.00025805. [DOI] [PubMed] [Google Scholar]
- 16.Prescott E, Lange P, Vestbo J. Socioeconomic status, lung function and admission to hospital for COPD: results from the Copenhagen City Heart Study. Eur Respir J. 1999;13(5):1109–1114. doi: 10.1034/j.1399-3003.1999.13e28.x. [DOI] [PubMed] [Google Scholar]
- 17.Grigsby M, Siddharthan T, Chowdhury MA, Siddiquee A, Rubinstein A, Sobrino E, et al. Socioeconomic status and COPD among low- and middle-income countries. Int J Chron Obstruct Pulm Dis. 2016;11:2497–2507. doi: 10.2147/COPD.S111145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lange P, Marott JL, Vestbo J, Ingebrigtsen TS, Nordestgaard BG. Socioeconomic status and prognosis of COPD in Denmark. COPD. 2014;11(4):431–437. doi: 10.3109/15412555.2013.869580. [DOI] [PubMed] [Google Scholar]
- 19.Lawlor DA, Ebrahim S, Davey Smith G. Association between self-reported childhood socioeconomic position and adult lung function: findings from the British Women’s Heart and Health Study. Thorax. 2004;59(3):199–203. doi: 10.1136/thorax.2003.008482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sehgal IS, Dhooria S, Agarwal R. Chronic obstructive pulmonary disease and malnutrition in developing countries. Curr Opin Pulm Med. 2017;23(2):139–148. doi: 10.1097/MCP.0000000000000356. [DOI] [PubMed] [Google Scholar]
- 21.Ture DA, Demirci H, Sengoren Dikis O. The relationship between health literacy and disease specific costs in subjects with chronic obstructive pulmonary disease (COPD). The Aging Male (Epub 29 Sep 2018). [DOI] [PubMed]
- 22.Murthy KJ, Sastry JG. Economic burden of chronic obstructive pulmonary disease. National Commission on Macroeconomics and Health background papers – burden of disease in India; 2005. p. 268–88. http://www.who.int/macrohealth/action/NCMH_Burden%20of%20disease_(29%20Sep%202005).pdf. Accessed 28 Dec 2018.
- 23.Kim C, Kim Y, Yang DW, Rhee CK, Kim SK, Hwang YI, et al. Direct and indirect costs of chronic obstructive pulmonary disease in Korea. Tuberc Respir Dis. 2019;82(1):27–34. doi: 10.4046/trd.2018.0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mannino DM, Higuchi K, Yu TC, Zhou H, Li Y, Tian H, et al. Economic burden of COPD in the presence of comorbidities. Chest. 2015;148(1):138–150. doi: 10.1378/chest.14-2434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen X, Wang N, Chen Y, Xiao T, Fu C, Xu B. Costs of chronic obstructive pulmonary disease in urban areas of China: a cross-sectional study in four cities. Int J Chron Obstruct Pulm Dis. 2016;11:2625–2632. doi: 10.2147/COPD.S118523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lewis A, Torvinen S, Dekhuijzen PN, Chrystyn H, Watson AT, Blackney M, et al. The economic burden of asthma and chronic obstructive pulmonary disease and the impact of poor inhalation technique with commonly prescribed dry powder inhalers in three European countries. BMC Health Serv Res. 2016;16:251. doi: 10.1186/s12913-016-1482-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wacker ME, Jorres RA, Schulz H, Heinrich J, Karrasch S, Karch A, et al. Direct and indirect costs of COPD and its comorbidities: results from the German COSYCONET study. Respir Med. 2016;111:39–46. doi: 10.1016/j.rmed.2015.12.001. [DOI] [PubMed] [Google Scholar]
- 28.Dal Negro RW, Bonadiman L, Turco P, Tognella S, Iannazzo S. Costs of illness analysis in Italian patients with chronic obstructive pulmonary disease (COPD): an update. ClinicoEconomics Outcomes Res. 2015;7:153–159. doi: 10.2147/CEOR.S77504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Darbà J, Ramírez G, García-Rivero JL, Mayoralas S, Pascual JF, Vargas D, et al. Estimating the economic consequences of an increased medication adherence due to a potential improvement in the inhaler technique with Spiromax® compared with Turbuhaler® in patients with moderate-to-severe chronic obstructive pulmonary disease in Spain. ClinicoEconomics Outcomes Res. 2017;9:127–137. doi: 10.2147/CEOR.S125301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.de Miguel Diez J, Carrasco Garrido P, Garcia Carballo M, Gilde Miguel A, Rejas Gutierrez J, Bellon Cano JM, et al. Determinants and predictors of the cost of COPD in primary care: a Spanish perspective. Int J Chron Obstruct Pulm Dis. 2008;3(4):701–712. doi: 10.2147/copd.s2427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Patel KD, Lalwani T, Shah K. Economic burden in direct cost of chronic obstructive pulmonary disease at a tertiary care teaching hospital: a prospective observational cohort study. Indian J Pharm Pract. 2014;7(3):61–68. [Google Scholar]
- 32.Naveed A, Ali SA, Parveen A, Yousuf S, Ahmed A, Hashmi MA, et al. Prescription patterns and cost of illness in asthma and chronic obstructive pulmonary disease patients. Int J Acad Med. 2016;2:173–178. [Google Scholar]
- 33.Ministry of Health and Family Welfare, Government of India. National Health Accounts Estimates for India 2014–2015; 2017. https://mohfw.gov.in/sites/default/files/National%20Health%20Accounts%20Estimates%20Report%202014-15.pdf. Accessed 4 Jan 2019.
- 34.Lavorini F, Magnan A, Dubus JC, Voshaar T, Corbetta L, Broeders M, et al. Effect of incorrect use of dry powder inhalers on management of patients with asthma and COPD. Respir Med. 2008;102(4):593–604. doi: 10.1016/j.rmed.2007.11.003. [DOI] [PubMed] [Google Scholar]
- 35.Chrystyn H, van der Palen J, Sharma R, Barnes N, Delafont B, Mahajan A, et al. Device errors in asthma and COPD: systematic literature review and meta-analysis. NPJ Prim Care Respir Med. 2017;27(1):22. doi: 10.1038/s41533-017-0016-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sanchis J, Gich I, Pedersen S. Systematic review of errors in inhaler use: has patient technique improved over time? Chest. 2016;150(2):394–406. doi: 10.1016/j.chest.2016.03.041. [DOI] [PubMed] [Google Scholar]
- 37.Price D, Keininger DL, Viswanad B, Gasser M, Walda S, Gutzwiller FS. Factors associated with appropriate inhaler use in patients with COPD: lessons from the REAL survey. Int J Chron Obstruct Pulm Dis. 2018;13:695–702. doi: 10.2147/COPD.S149404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sulaiman I, Cushen B, Greene G, Seheult J, Seow D, Rawat F, et al. Objective assessment of adherence to inhalers by patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2017;195(10):1333–1343. doi: 10.1164/rccm.201604-0733OC. [DOI] [PubMed] [Google Scholar]
- 39.Vestbo J, Anderson JA, Calverley PMA, Celli B, Ferguson GT, Jenkins C, et al. Adherence to inhaled therapy, mortality and hospital admission in COPD. Thorax. 2009;64(11):939–943. doi: 10.1136/thx.2009.113662. [DOI] [PubMed] [Google Scholar]
- 40.Carron T, Bridevaux PO, Lorvall K, Parmentier R, Moix JB, Beytrison V, et al. Feasibility, acceptability and effectiveness of integrated care for COPD patients: a mixed methods evaluation of a pilot community-based programme. Swiss Med Wkly. 2017;147:w14567. doi: 10.4414/smw.2017.14567. [DOI] [PubMed] [Google Scholar]
- 41.Kruis AL, Smidt N, Assendelft WJ, Gussekloo J, Boland MR, Rutten-van Molken M, et al. Integrated disease management interventions for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2013;(10):CD009437. [DOI] [PubMed]
- 42.Halpern M.T., Stanford R.H., Borker R. The burden of COPD in the U.S.A.: results from the confronting COPD survey. Respiratory Medicine. 2003;97:S81–S89. doi: 10.1016/s0954-6111(03)80028-8. [DOI] [PubMed] [Google Scholar]
- 43.Britton M. The burden of COPD in the U.K.: results from the confronting COPD survey. Respiratory Medicine. 2003;97:S71–S79. doi: 10.1016/s0954-6111(03)80027-6. [DOI] [PubMed] [Google Scholar]
- 44.Suhaj A, Manu MK, Unnikrishnan MK, Vijayanarayana K, Mallikarjuna Rao C. Effectiveness of clinical pharmacist intervention on health-related quality of life in chronic obstructive pulmonary disorder patients: a randomized controlled study. J Clin Pharm Ther. 2016;41(1):78–83. doi: 10.1111/jcpt.12353. [DOI] [PubMed] [Google Scholar]
- 45.Faheemuddin MD, Ramaiah B, Kiran SS, Kumari BS, Vijayalaxmi M. Evaluation of medication adherence in COPD patients and their drug utilisation pattern. Chron Obstruct Pulm Dis. 2016;1:17. [Google Scholar]
- 46.Abdulsalim S, Unnikrishnan MK, Manu MK, Alrasheedy AA, Godman B, Morisky DE. Structured pharmacist-led intervention programme to improve medication adherence in COPD patients: a randomized controlled study. Res Soc Admin Pharm. 2018;14(10):909–914. doi: 10.1016/j.sapharm.2017.10.008. [DOI] [PubMed] [Google Scholar]
- 47.Bourbeau J, Julien M, Maltais F, Rouleau M, Beaupre A, Begin R, et al. Reduction of hospital utilization in patients with chronic obstructive pulmonary disease: a disease-specific self-management intervention. Arch Intern Med. 2003;163(5):585–591. doi: 10.1001/archinte.163.5.585. [DOI] [PubMed] [Google Scholar]
- 48.Ghose D. India suffering critical shortage of doctors: NMC Bill may finally give rural poor access to affordable healthcare; 2018. https://www.firstpost.com/india/india-suffering-critical-shortage-of-doctors-nmc-bill-may-finally-give-rural-poor-access-to-affordable-healthcare-4285483.html. Accessed 4 Jan 2019.
- 49.Singh D, Bose A. Tackling doctors’ shortage. The Pioneer 2018. https://www.dailypioneer.com/2018/columnists/tackling-doctors-shortage.html. Accessed 4 Jan 2019.
- 50.Kumar R. The leadership crisis of medical profession in India: ongoing impact on the health system. J Fam Med Prim Care. 2015;4(2):159–161. doi: 10.4103/2249-4863.154621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ladhani S. COPD—an Indian perspective. J Lung Pulm Respir Res. 2016;3(1):24–25. [Google Scholar]
- 52.Cameron A, Ewen M, Ross-Degnan D, Ball D, Laing R. Medicine prices, availability, and affordability in 36 developing and middle-income countries: a secondary analysis. Lancet. 2009;373(9659):240–249. doi: 10.1016/S0140-6736(08)61762-6. [DOI] [PubMed] [Google Scholar]
- 53.Abdulsalim S, Unnikrishnan MK, Manu MK, Alrasheedy AA, Godman B, Morisky DE. Authors’ response to the comments to “Structured pharmacist-led intervention programme to improve medication adherence in COPD patients: a randomized controlled study”. Res Soc Admin Pharm. 2018;14(4):402–403. doi: 10.1016/j.sapharm.2017.12.008. [DOI] [PubMed] [Google Scholar]
- 54.Khdour MR, Kidney JC, Smyth BM, McElnay JC. Clinical pharmacy-led disease and medicine management programme for patients with COPD. Br J Clin Pharmacol. 2009;68(4):588–598. doi: 10.1111/j.1365-2125.2009.03493.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jarab AS, Alqudah SG, Khdour M, Shamssain M, Mukattash TL. Impact of pharmaceutical care on health outcomes in patients with COPD. Int J Clin Pharm. 2012;34(1):53–62. doi: 10.1007/s11096-011-9585-z. [DOI] [PubMed] [Google Scholar]
- 56.Gallefoss F, Bakke PS. How does patient education and self-management among asthmatics and patients with chronic obstructive pulmonary disease affect medication? Am J Respir Crit Care Med. 1999;160(6):2000–2005. doi: 10.1164/ajrccm.160.6.9901028. [DOI] [PubMed] [Google Scholar]
- 57.Gallefoss F. The effects of patient education in COPD in a 1-year follow-up randomised, controlled trial. Patient Educ Counsel. 2004;52(3):259–266. doi: 10.1016/S0738-3991(03)00100-9. [DOI] [PubMed] [Google Scholar]
- 58.Suhaj A, Unnikrishnan MK, Mohan MK, Kunhikkatta V, Rao CM. PRS2: effectiveness of clinical pharmacist intervention on direct medical cost in chronic obstructive pulmonary disorder patients—a randomized controlled study. Value Health. 2016;19:A807–A918. doi: 10.1111/jcpt.12353. [DOI] [PubMed] [Google Scholar]
- 59.Sharma A, Ladd E, Unnikrishnan MK. Healthcare inequity and physician scarcity empowering non-physician healthcare. Econ Polit Wkly. 2013;48(13):112–117. [Google Scholar]
- 60.Garg S. Universal health coverage in India: newer innovations and the role of public health. Indian J Public Health. 2018;62:167–170. doi: 10.4103/ijph.IJPH_221_18. [DOI] [PubMed] [Google Scholar]
- 61.Godman B, Oortwijn W, de Waure C, Mosca I, Puggina A, Specchia ML, et al. Links between pharmaceutical R&D models and access to affordable medicines. A study for the ENVI Committee. http://www.europarl.europa.eu/RegData/etudes/STUD/2016/587321/IPOL_STU(2016)587321_EN.pdf. Accessed 4 Jan 2019.
- 62.OECD. Health at a glance 2017. https://www.oecd-ilibrary.org/docserver/health_glance-2017-en.pdf?expires=1531413926&id=id&accname=guest&checksum=656327F799B10217DD2D80F463DAB8732017. Accessed 4 Jan 2019.
- 63.Triami Media BV. Historic inflation—CPI inflation year pages; 2017. www.inflation.eu.
- 64.Payscale. Average Clinical Pharmacist Salary. https://www.payscale.com/research/IN/Job=Clinical_Pharmacist/Salary. Accessed 20 Dec 2018.
- 65.Balkrishnan R, Christensen DB. Inhaled corticosteroid use and associated outcomes in elderly patients with moderate to severe chronic pulmonary disease. Clin Ther. 2000;22(4):452–469. doi: 10.1016/S0149-2918(00)89013-X. [DOI] [PubMed] [Google Scholar]
- 66.Suhaj A, Mohan MK, Mohapatra A, et al. Development and readability assessment of patient information leaflets for chronic obstructive pulmonary disease. Asian J Pharm Health Sci. 2015;5:1237–1241. [Google Scholar]
- 67.Ravi Kumar BP, Dudala SR, Rao AR. Kuppuswamy’s socio-economic status scale: a revision of economic parameter for 2012. Int J Res Dev Health. 2013;1(1):2–4. [Google Scholar]
- 68.Hilleman DE, Dewan N, Malesker M, Friedman M. Pharmacoeconomic evaluation of COPD. Chest. 2000;118(5):1278–1285. doi: 10.1378/chest.118.5.1278. [DOI] [PubMed] [Google Scholar]
- 69.Ofori-Asenso R, Agyeman AA. Irrational use of medicines—a summary of key concepts. Pharmacy. 2016;4:35. doi: 10.3390/pharmacy4040035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wright D, Twigg M, Barton G, Thornley T, Kerr C. An evaluation of a multi-site community pharmacy-based chronic obstructive pulmonary disease support service. Int J Pharm Pract. 2015;23(1):36–43. doi: 10.1111/ijpp.12165. [DOI] [PubMed] [Google Scholar]
- 71.Bourbeau J, Bartlett SJ. Patient adherence in COPD. Thorax. 2008;63(9):831–838. doi: 10.1136/thx.2007.086041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Dal Negro RW, Tognella S, Tosatto R, Dionisi M, Turco P, Donner CF. Costs of chronic obstructive pulmonary disease (COPD) in Italy: the SIRIO study (Social Impact of Respiratory Integrated Outcomes) Respir Med. 2008;102(1):92–101. doi: 10.1016/j.rmed.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 73.Charles MS, Blanchette CM, Silver H, Lavallee D, Dalal AA, Mapel D. Adherence to controller therapy for chronic obstructive pulmonary disease: a review. Curr Med Res Opin. 2010;26(10):2421–2429. doi: 10.1185/03007995.2010.516284. [DOI] [PubMed] [Google Scholar]
- 74.Cramer JA, Bradley-Kennedy C, Scalera A. Treatment persistence and compliance with medications for chronic obstructive pulmonary disease. Can Respir J. 2007;14(1):25–29. doi: 10.1155/2007/161652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Bender BG, Pedan A, Varasteh LT. Adherence and persistence with fluticasone propionate/salmeterol combination therapy. J Allergy Clin Immunol. 2006;118(4):899–904. doi: 10.1016/j.jaci.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 76.Brown P, Bluml BM, Kritzler R, Petryna M, Polley CM, Tietze KJ, et al. White paper on expanding the role of pharmacists in chronic obstructive pulmonary disease. J Am Pharm Assoc. 2011;51(2):203–211. doi: 10.1331/JAPhA.2011.11513. [DOI] [PubMed] [Google Scholar]
- 77.Bojanic L, Markovic-Pekovic V, Skrbic R, Stojakovic N, Ethermanovic M, Bojanic J, et al. Recent initiatives in the Republic of Srpska to enhance appropriate use of antibiotics in ambulatory care; their influence and implications. Front Pharmacol. 2018;9:442. doi: 10.3389/fphar.2018.00442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mohan MK, Vineetha R. Medical insurance: promoting unethical practices? Indian J Med Ethics. 2011;8(4):261. doi: 10.20529/IJME.2011.101. [DOI] [PubMed] [Google Scholar]
- 79.Gustafsson LL, Wettermark B, Godman B, Andersen-Karlsson E, Bergman U, Hasselstrom J, et al. The ‘wise list’—a comprehensive concept to select, communicate and achieve adherence to recommendations of essential drugs in ambulatory care in Stockholm. Basic Clin Pharmacol Toxicol. 2011;108(4):224–233. doi: 10.1111/j.1742-7843.2011.00682.x. [DOI] [PubMed] [Google Scholar]
- 80.Meyer JC, Schellack N, Stokes J, Lancaster R, Zeeman H, Defty D, et al. Ongoing initiatives to improve the quality and efficiency of medicine use within the public healthcare system in South Africa: a preliminary study. Front Pharmacol. 2017;8:751. doi: 10.3389/fphar.2017.00751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Niaz Q, Godman B, Massele A, Campbell S, Kurdi A, Kagoya HR, et al. Validity of World Health Organisation prescribing indicators in Namibia’s primary healthcare: findings and implications. Int J Qual Health Care. 2019;31(5):338–345. doi: 10.1093/intqhc/mzy172. [DOI] [PubMed] [Google Scholar]
- 82.Cameron A, Mantel-Teeuwisse AK, Leufkens HG, Laing RO. Switching from originator brand medicines to generic equivalents in selected developing countries: how much could be saved? Value Health. 2012;15(5):664–673. doi: 10.1016/j.jval.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 83.Alrasheedy AA, Hassali MA, Wong ZY, Saleem F. Pharmacist-managed medication therapy adherence clinics: the Malaysian experience. Res Soc Admin Pharm. 2017;13(4):885–886. doi: 10.1016/j.sapharm.2017.02.011. [DOI] [PubMed] [Google Scholar]
- 84.Cheng HM, Liu WC, Chua G, Liew CF, Li W, Choo W, et al. Impact of a pharmacy-led smoking cessation clinic in a dermatology centre. Singapore Med J. 2019;60(1):31–33. doi: 10.11622/smedj.2018063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Bock BC, Hudmon KS, Christian J, Graham AL, Bock FR. A tailored intervention to support pharmacy-based counseling for smoking cessation. Nicotine Tob Res. 2010;12(3):217–225. doi: 10.1093/ntr/ntp197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Twigg MJ, Wright DJ. Community pharmacy COPD services: what do researchers and policy makers need to know? Integr Pharm Res Pract. 2017;6:53–59. doi: 10.2147/IPRP.S105279. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Further data are available upon reasonable request.