We read with great interest the article by Foster and colleagues,1 recently published in the Journal of the American College of Surgeons, regarding a draping technique meant to protect healthcare providers (HCP) during tracheostomy. In addition to congratulating the authors, we would like to thank them for this contribution to the safety of the healthcare community. We, too, have developed a similar draping technique for aerosol-generating medical procedures (AGMPs) with a modification that may be of additional benefit.
AGMPs can increase the spread of COVID-19 infection from patients to HCPs.2 , 3 Airway-manipulating procedures, such as tracheostomy, bronchoscopy, and endoscopic sinonasal procedures, are high risk because of the high viral loads in these tissues.4 Given the anticipated duration of the pandemic, limitations in screening availability, and sensitivity, urgent high-risk AGMPs are inevitable, and strategies to protect HCPs are required. Matava and colleagues5 showed that clear plastic drapes effectively limited aerosolization and droplet spray during extubation using a Glo-germ model. Surgical manipulation of the upper airway, however, leads to prolonged exposure of HCPs to viral particles and greater time for dispersal through the operating room (OR). Some centers have resorted to using powered-air purifying respirators to protect HCPs during these procedures, but these are not readily available in many institutions. Although this protects HCPs intraoperatively, the coronavirus can remain viable on contaminated surfaces throughout the OR for hours.3 , 6
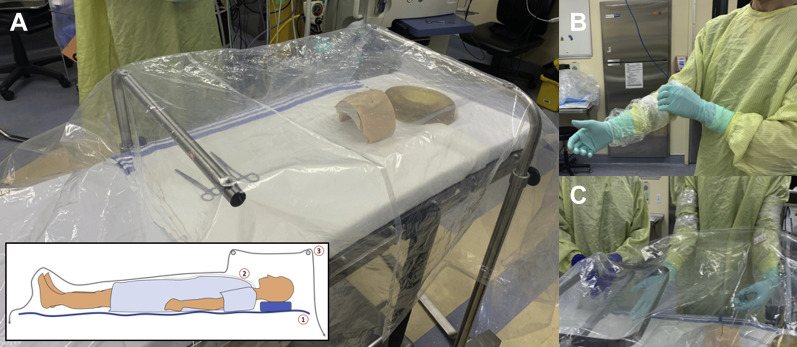
The draping technique proposed by Foster and colleagues1 presents an excellent method to address these issues. However, it has been shown that nosocomial infection is often the result of self-contamination during doffing of personal protective equipment (PPE).3 , 7 In Foster and colleagues'1 technique, although the arms are covered by the surgical gown, the contaminated arms are still withdrawn from the field and can put HCPs at risk. Since the onset of the COVID-19 outbreak, we have used a draping technique similar to that described by Foster and coworkers, with the addition of 2 disposable arm sleeves (Fig. 1 A) that can be left in the field. To allow access to the patient, small holes cut into the drapes allow the HCP's arms to enter the field. The practitioner's arms were further draped in disposable plastic telescope drapes so that they may be left inside the field and discarded with the drapes (Figs. 1B and C). We propose that this technique may serve as an adjunct method to help reduce the amount of droplet spread during urgent high-risk airway procedures.
Figure 1.
The enhanced draping technique. (A) The draping technique consists of 3 layers. 1. Bed drape. 2. Over-body drape. 3. Tent drape suspended over 2 adjustable-height Mayo stand bars. These bars can also be draped if sterility is required. The Mayo stand bars can be rotated and positioned to avoid obstructing access to the patient. A modified extracorporeal membrane oxygenation (ECMO) cover drape (Uline S12308 60 × 60 2mm polybag) or a Lap ped-neonatal clear drape (Medline) are sufficiently large for the tent drape. Two suctions are secured under the tent drape and left on full suction. (B) In addition to appropriate personal protective equipment (PPE), the healthcare providers (HCP) cover their arms in disposable sleeves. Gown sleeves (Medline), video camera drapes (Microtek AEF 9604, LOT190904F), or ultrasound drapes can be used. (C) Two small holes are then cut into the drapes at appropriate distances so that the HCPs can comfortably move their arms without excessively luffing the drapes.
This technique was simulated in the OR by 8 HCPs from otolaryngology, anesthesia, nursing, infection control, and medical engineering. One otolaryngologist donned personal protective equipment (PPE) for AGMPs, in addition to the plastic sleeves, and placed both arms through the drapes to simulate surgery for 5 minutes. During this time, 3M fit test solution (FT-12) was sprayed under the drapes, as is performed during N95 mask fit testing. Six HCPs could not taste the FT-12 from various positions around the drape for 10 minutes, but all could when the drape was lifted. This technique has been used more than 10 times for multiple procedures including rigid bronchoscopy and esophagoscopy for foreign body removal, tracheostomy tube change, and endoscopic sinus surgery for intracranial abscess. The inevitability of urgent upper airway procedures will continue to put HCPs at risk of infection, and innovations such as this will be increasingly necessary as the situation evolves. Step-by-step instructions for this draping method can be found at www.ORLPED.com. This technique is proposed as an adjunct to correctly donned and doffed PPE for high-risk procedures involving the upper airway during COVID-19 pandemic.
Footnotes
Disclosure Information: Nothing to disclose.
Supplementary Data
References
- 1.Foster P., Cheung T., Craft P. Novel approach to reduce transmission of COVID-19 during tracheostomy. J Am Coll Surg. 2020 April 10 doi: 10.1016/j.jamcollsurg.2020.04.014. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang D., Hu B., Hu C. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vukkadala N., Qian Z.J., Holsinger F.C. COVID-19 and the otolaryngologist - preliminary evidence-based review. Laryngoscope. 2020 March 26 doi: 10.1002/lary.28672. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 4.Zou L., Ruan F., Huang M. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382:1177–1179. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Matava C.T., Yu J., Denning S. Clear plastic drapes may be effective at limiting aerosilization and droplet spray during extubation: implications for COVID-19. Canadian J Anesthesia. April 2020 doi: 10.1007/s12630-020-01649-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.van Doremalen N., Bushmaker T., Morris D.H. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Verbeek J.H., Rajamaki B., Ijaz S. Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff. Cochrane Work Group, ed. Cochrane Database Syst Rev. 2020;4:CD011621. doi: 10.1002/14651858.CD011621.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.