Abstract
Examining association between serial participation in youth organized sports (OS) and concurrent cardiometabolic risk factors, with long-term health status, will aid understanding the role of OS participation. Combining data from a prospective study and a follow-up survey, we aimed to determine association between youth OS participation and cardiometabolic risk factors with health and physical activity (PA) in young adulthood. Cardiometabolic risk factors were monitored yearly, and OS involvement through middle school, high school, and college, together with current status was recorded 12 years after the initial study began; 462 participants completed follow-up. Cardiometabolic risk factors included: body mass index (BMI), waist circumference, blood pressure, total cholesterol, high-density lipoprotein (HDL), low-density lipoprotein (LDL) cholesterol and triglycerides, fasting glucose and insulin. Participants continuing OS participation from middle to high school and/or college had significantly lower BMI/BMI z-scores [24.7 vs 27.4 (p < 0.05) and 0.51 vs 0.82 (p < 0.05), respectively] and significantly higher HDL [48.7 vs 45.4 (p ≤ 0.05)] than those without OS participation after middle school. Waist circumference of females was significantly smaller in those who participated in OS from middle to high school and/or college (84.9 cm) compared to those who had no OS (92.1 cm), (p < 0.05). Participants continuing OS from middle to high school and/or college reported significantly higher follow-up PA levels than those who had no OS after middle school (p < 0.001). This study provides novel data showing serial participation in OS from middle to high school and/or college was associated with a superior cardiometabolic health profile in school and increased PA levels at 12-year follow-up.
Keywords: Physical activity, Cardiometabolic, Risk factors, Diabetes, Health profile
1. Introduction
Definitions: Organized sport (OS): For this study, OS is defined as PA directed by adult or youth leaders, involving rules, formal practice, and competition. We include school and club sports.
Organized sports (OS) participation has many benefits in youth (Merkel, 2013, Logan and Cuff, 2019). Specifically, OS is associated with improved mental health (Vella et al., 2017), reduced risk taking behavior (Pate et al., 2000), improved cardiovascular fitness (Hardy et al., 2014, Silva et al., 2013), and may reduce the risk of overweight/obesity (Drenowatz et al., 2013) and cardiovascular disease (Hebert et al., 2017). Benefits, particularly in cardiovascular risk, are shown across childhood and adolescence. Participation in OS for approximately one year has been associated with reduced clustered cardiovascular risk and a 20% reduction of overweight/obesity in elementary school (Hebert et al., 2017). Similarly, OS participation 1–2 times a week was associated with a lower prevalence of overweight elementary school children (Drenowatz et al., 2013). In a study of OS participation in kindergarten and first-grade, participation in team sports and structured PA classes was associated with a slowed BMI increase, with effects demonstrated to age 10 (Dunton et al., 2012). In junior high and high school students, the likelihood of being overweight in early adulthood was associated with a 20–48% reduction by playing OS 3–4 times weekly (Menschik et al., 2008).
Longitudinal data indicate that for Finnish children and adolescents studied over a period of 21 years, those involved in OS had a reduced risk of developing metabolic syndrome in adulthood (Yang et al., 2009). Results from the National Longitudinal Study of Adolescent Health showed that participation in OS during adolescence improved subjective health and was associated with increased levels of moderate to vigorous PA (MVPA), compared to those who did not participate, when assessed six years later (Dodge and Lambert, 2009). Research has also shown that history of high school OS participation was associated with longer Bruce Protocol exercise time, metabolic equivalents (MET), and reported hours of weekly exercise in adults presenting for exercise testing (Angeli et al., 2017). Participation in OS during high school has even been associated with higher levels of PA in old age; a study of male World War II veterans 50 years after they had undergone a physical fitness assessment for military service showed that the strongest predictor of PA and level of health was whether they played a high school varsity sport (Dohle and Wansink, 2013).
Although OS are popular among children and adolescents, current trends in participation rates are of concern. Sport dropout was identified as a trajectory (as compared to consistent sport participants and sport nonparticipants) in over a third of both boys and girls in a large Australian study, with increased dropout from sport participation starting at age 14 (Howie et al., 2016). The dropout finding is similar to a recent study of American youth, where about 40% of subjects dropped out from OS; however, dropout started earlier, at approximately 11 years of age (Kwon et al., 2015). The effect of dropout is further reflected in the National Heart, Lung, and Blood Institute Growth and Health Study, which showed a steep decline in girls’ PA, as measured by the Habitual Activity Questionnaire (HAQ); over half of the African-American girls studied, and almost a third of the Caucasian girls studied, had HAQs scores of zero by the time they were 16–17 years old (Kimm et al., 2002). Furthermore, the 2014 U.S. Report Card on Physical Activity for Children and Youth gave a grade of C- for OS participation and a grade of D- for overall PA levels (Dentro et al., 2014). Injury rate may also play a role in dropout (Butcher et al., 2002), with more specialized athletes being injured more often (Bell et al., 2018). Burnout, negative parental behavior, and negative coaching behavior are other reasons young athletes drop out of sport (Logan and Cuff, 2019).
Research has indicated that participation in organized youth sports may be associated with improved body composition and PA levels, especially during adolescence (Telford et al., 2016). However, from a mechanistic perspective, the long-term effect of sports-driven PA on cardiometabolic risk, in the context of serial and persistent sport participation over middle school, high school, and college, is unknown. Additionally, the impact of OS participation throughout the school years on PA levels later in life also remains unclear. Therefore, the purpose of this study was 1) to determine the association of OS participation during adolescence with cardiometabolic risk factors, and 2) establish the long-term effects of OS participation on self-reported health status and PA level as a young adult.
2. Methods
2.1. Participants
This follow-up study used a survey with targeted recruitment from a cohort of 1243 participants who took part in a prior prospective longitudinal cohort study spanning 6 years (Princeton School District Study) (Dolan et al., 2005). Of 1083 potential subjects (ages 19–29 years), 830 were successfully contacted either by phone, text, email, mail, or social media, 12 years after the initial study procedures began. Of the 830 contacted, 509 participants responded and completed at least part of a follow up survey on youth OS participation and current health. Ultimately, 462 participants fully completed the survey (please see “Study Questionnaire” section below) and were included for analysis. The study spanned from the first survey invitation being sent in February 2013 to the final survey being completed in May 2014.
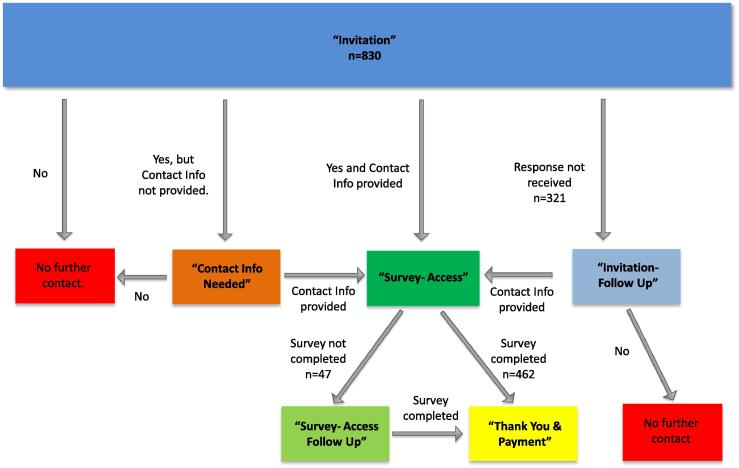
Fig. 1 provides a participant flow diagram for the study.
Fig. 1.
Participant flow diagram.
2.2. Procedures
The institutional review board of Cincinnati Children’s Hospital Medical Center approved the study design, consent forms and recruitment documents before data collection. The study involved only the completion of an online survey, thus a waiver of documentation of consent was obtained. The cohort of 1243 received “Invitation” correspondence inviting them to participate via various means (letter, email, social network message, phone call, text message). This correspondence explained that based on their prior study participation (Dolan et al., 2005). we were requesting voluntary participation in a new, related study. Participants wishing to participate were asked to contact us with their contact information so that we could verify their identity and send them the next phase of study correspondence (“Survey- Access”). Those not wanting to take part were instructed to contact us by a specified date indicating they did not wish to participate. They were informed that if we did not hear from them by the specified date, we would move forward with attempting to contact them. Those expressing interest were emailed a participant unique survey link and study ID via REDCap. The survey contained an introduction containing all elements of consent. Participants were then asked to select whether they agreed to take part in the study. If they agreed, they then began the survey. Participants received $15 for completing the online survey.
2.3. Measurements
2.3.1. Study questionnaire
We used REDCap (Harris et al., 2019), assessing the following areas: health history, detailed school sports participation (middle school, high school, college), year of sports cessation, sports related injuries, non-sports related injuries, current PA level (Marx Activity Rating Scale (MARS) (Marx et al., 2001), Tegner activity scale (Briggs et al., 2006), and participant contact information. Health history collected included cancer, cardiovascular disease, diabetes, high cholesterol, hypertension, kidney disease, fatty liver disease, and an open-ended question of other. There was also a space to respond “none of the diseases”.
2.3.2. Laboratory and health measures
Sex, race, biometric, and blood markers of cardiometabolic risk (Table 1) collected from the prospective longitudinal Princeton School District study were compared with school and non-school organized and recreational sports participation and with health status and physical activity at follow-up.
Table 1.
Demographics for those “Fully completing the survey” compared with those “Not fully completing the survey”.
| Variable (n = 1243) | Fully completed survey (n = 462) | Did not fully complete survey (n = 781) | p-value |
|---|---|---|---|
| Sex | <0.0001 | ||
| Female | 298 (64.5) | 377 (48.3) | |
| Male | 164 (35.5) | 404 (51.7) | |
| Race / Ethnicity | 0.10* | ||
| Asian | 10 (2.2) | 8 (1.0) | |
| African-American | 174 (37.7) | 316 (40.5) | |
| Hispanic | 2 (0.4) | 14 (1.8) | |
| Mixed | 6 (1.3) | 10 (1.3) | |
| Caucasian | 270 (58.4) | 431 (55.2) | |
| WI | 0 | 2 (0.3) | |
| African-American | 174 (37.7) | 316 (40.5) | 0.33 |
| Hispanic | 2 (0.4) | 14 (1.8) | 0.04* |
Data presented as n (%). Chi-square used for testing or *Fisher’s exact test.
Known cardiometabolic risk factors of body mass index (BMI), waist circumference, systolic and diastolic blood pressure, total cholesterol and high-density lipids (HDL), low-density lipids (LDL) and triglycerides, fasting glucose, and insulin were obtained from the original study (Dolan et al., 2005). Data was extracted from the last study visit; therefore, results reflected information closest to when the survey was completed for an individual. BMI z-score was calculated using the SAS® program available at the Centers for Disease Control and Prevention website. The triglyceride to HDL ratio was also calculated.
2.4. Sports participation grouping
Survey data were used to examine both school and recreational sports participation during middle school, high school and college. Sports participation was counted as positive if participation in either school or recreational sport was indicated. Questions asked for information regarding participation per grade, per sport [e.g., 1) When you were in middle school (grades 5–8) did you participate in any organized sports? 2) What organized/competitive sport(s) did you participate in during your middle school years (grades 5–8)? 3) Please select all that apply.]. The list of sports to select from was: Basketball (school), Basketball (recreational/AAU), Volleyball (school), Volleyball (recreational/JO), Soccer (school), Soccer (recreational/club), Softball/Baseball (school), Softball/Baseball (recreational/club), Football (school), Football (recreational), Lacrosse, Field Hockey, Track/Cross Country, Cheerleading/Gymnastics, Tennis, Golf, Wrestling, Swimming/Water Polo and Other. This was counted separately for middle school, high school and college. Participants were divided into three different sports participation groups, according to timing of involvement in OS: Group 1 (G1) included subjects who did not participate in sports in middle school, high school, or college; Group 2 (G2) incorporated those who participated in middle school but not high school or college sports; Group 3 (G3) combined respondents who participated in middle school and high school, but not college sports, and respondents who participated in OS at all levels of education (including college).
2.5. Statistical analysis
SAS®, version 9.4 (SAS Institute, Cary, NC) was used for analysis. Continuous data were checked for distributional properties and outliers. Variables that were outcome or dependent were examined for appropriate transformation if necessary. Chi-square, and general linear models were used to compare dependent variables of interest between groups, specifically SAS PROC MIXED was used to be able to include covariates. When examining the cardiometabolic risk factors and association with OS group; for BMI, waist circumference and the waist to height ratio (both measured in centimeters) the covariates included were age, sex and race. For blood pressure, cholesterols, triglycerides, glucose and insulin the covariates included were age, sex, race and BMI. Analyses were also repeated by sex as many of the outcome variables tend to differ by sex in adolescents; these had the same covariates included in the models except for sex. A Bonferroni correction was used for individual comparisons between categories, and the Tukey-Kramer adjustment was used for the continuous variables. For comparison between groups, least square means and the associated standard errors were reported. Due to the distribution of the ratio triglycerides/HDL, a log transformation was used for analysis, so back transformed geometric least square means and associated standard errors are reported. A p-value of <0.05 was considered statistically significant.
An additional analysis examining the association of middle school OS and cardiometabolic outcome at last visit was examined, with and without adjustment for concurrent OS (high school OS). The same covariates were included as in the main analysis, and again these were repeated by sex. Again a general linear model was used for analysis.
3. Results
Of the 1243 potential subjects, 830 were found and contacted for inclusion in the study. 321 (28.5%) potential subjects did not respond. 462 (37.2%) subjects fully completed the survey, and 47 subjects only partially completed the survey. We included subjects who we could not find, those who did not respond and subjects who did not fully complete the survey into one group of 781 (See Table 1). There were significantly more men than women (p ≤ 0.0001), and significantly more subjects with Hispanic ethnicity (p = 0.04) who did not fully complete the survey than did complete it (Table 1). Of the 462 subjects completing the survey, 124 (27%) were defined in G1 (no sports), 77 (17%) G2 (middle school sports only) and 261 (56%) G3 (middle school and high school ± college sports)
In this cohort, 62 individuals continued playing the same sport from middle school through college [21% of the females and 28% of the males (p = 0.15)]; 26% of the non-African-American subjects and 17% of African-American subjects (p = 0.13). The Tegner and MARS instruments do not include information on specific sports information at follow-up. We had four choices for quitting sports; High school graduation, College graduation, Injury and Other. There were significant distributional differences by sex (p < 0.0001) and by African-American race (p = 0.0008). The percentages for females and males respectively for quitting were College graduation (10.4% vs 26.8%), High school graduation (41.2% vs 39.0%, Injury (8.1% vs 12.2%) and Other (40.3% vs 22.0%). The percentages for non-African-American and African-American race respectively for quitting were College graduation (21.3% vs 5.8%), High school graduation (40.4% vs 40.4%, Injury (10.0% vs 8.6%) and Other (28.3% vs 45.2%).
Demographics and biometrics by participation group at last visit in the longitudinal study are presented in Table 2. In addition, the average years engaged in OS in each group was as follows: For G2, years of OS participation mean (sd) is 4.9 (2.6), and median (25th, 75th percentiles) is 4 (3, 5); for G3 mean (sd) is 8.7 (2.5), and median (25th, 75th percentiles) is 8 (7, 12). Within the final group of 462 subjects, participants in G3 (middle school and high school ± college sports) were less likely to be female than participants in G2 (middle school sports only) and were less likely to be African-American than participants in either G1 (no sports) or G2 (middle school sports only). Participants in G3 (middle school and high school ± college sports) had significantly lower BMI and BMI z-scores than participants in G1 (no sports). Waist circumference and waist to height ratio was significantly smaller for participants in G3 (middle school and high school ± college sports), compared to participants in both G1 (no sports) and G2 (middle school sports only) (overall p = 0.002); however, for waist circumference, when grouped by sex, significant between-group differences remained only for females (overall p = 0.008). Participants in G3 (middle school and high school ± college sports) had significantly higher HDL-C levels than participants in G1 (no sports). Blood pressure, total cholesterol, LDL cholesteral and triglyceride levels were not significantly different among groups.
Table 2.
Demographics and biometrics measures by OS participation.
| Total | Group 1 | Group 2 | Group 3 | p-value | |
|---|---|---|---|---|---|
| N | 462 | 124 | 77 | 261 | |
| Age at follow-up (years) | 26.2 (2.3) | 26.4 (2.3) | 26.1 (2.5) | 26.1 (2.2) | 0.31 |
| Sex (Female) | 298 (64.5%) | 84 (67.7%) | 59a (76.6%) | 155b (59.4%) | 0.01 |
| Race (African-American) | 174 (37.7%) | 69a (55.6%) | 35a (45.4%) | 70b (26.8%) | <0.0001 |
| BMI (kg/m2)Ϯ | 25.7 (0.34) | 27.4a (0.64) | 26.4 (0.82) | 24.7b (0.44) | 0.001* |
| BMI z-score | 0.66 (1.07) | 0.82a (1.17) | 0.79 (1.05) | 0.51b (0.99) | 0.01 |
| Waist circumference (cm)Ϯ | 87.6 (0.79) | 91.3a (1.47) | 90.5a (1.88) | 85.2b (1.00) | 0.0008* |
| Waist circumference (cm) -femalesϮ | 87.9 (0.93) | 92.1a (1.72) | 90.2 (2.06) | 84.9b (1.27) | 0.002** |
| Waist circumference (cm) -malesϮ | 87.3 (1.29) | 89.5 (2.61) | 91.9 (3.89) | 85.7 (1.60) | 0.22** |
| Systolic BP (mmHg)Ϯ | 115 (0.47) [n = 444] | 117 (0.91) [n = 113] | 115 (1.12) [n = 75] | 115 (0.60) [n = 181] | 0.21* |
| Diastolic BP (mmHg)Ϯ | 69.7 (0.33) [n = 444] | 70.0 (0.63) [n = 113] | 69.8 (0.79) [n = 75] | 69.5 (0.4) [n = 181] | 0.82* |
| Total Cholesterol (mg/dL)Ϯ | 148 (1.28) | 150 (2.41) | 148 (3.08) | 147 (1.65) | 0.64* |
| HDL cholesterol (mg/dL)Ϯ | 47.5 (0.57) | 45.4a (1.06) | 46.4 (1.35) | 48.7b (0.72) | 0.03* |
| LDL cholesterol (mg/dL)Ϯ | 84.0 (1.11) | 87.8a (2.07) | 85.0 (2.65) | 82.0b (1.42) | 0.06* |
| Triglycerides (mg/dL)Ϯ | 81.8 (1.95) | 82.0 (3.68) | 83.2 (4.71) | 81.3 (2.52) | 0.93* |
| Triglyceride/HDL-C Ratio | 1.61 (1.03) | 1.67 (1.05) | 1.68 (1.07) | 1.56 (1.04) | 0.56* |
| Fasting glucose (mg/dL)Ϯ | 83.4 (0.64) | 84.2 (1.12) | 82.3 (1.44) | 83.3 (0.88) | 0.59* |
| Fasting insulin (pmol/L)Ϯ | 160 (9.58) | 162 (16.8) | 173 (21.7) | 154 (13.2) | 0.75* |
Data presented as mean (standard deviation), least square mean (standard error) or n (%); least square means and associated standard error are reported when adjusting for age and sex or age only. The Triglyceride/HDL ratio is presented as geometric least square mean (geometric standard deviation) due to distribution necessitating analysis using log transformed data.
‘a’ denotes difference from ‘b’ p < 0.05, adjusted using Dunnett’s test (age and BMI z-score) or Tukey-Kramer adjustment (continuous variables except age and BMI z-score or Bonferroni (sex and race) as appropriate.
Group 1 – No, No, No (Middle, High School, and College); Group 2 – Yes, No, No; Group 3 – Yes, Yes, No and Yes, Yes, Yes.
BMI = Body Mass Index (weight (kg) / height (m)2).
Age and sex adjusted.
Age adjusted.
At the 12-year follow-up, there were no differences by group for reported health history (Table 3), but participants in G3 (middle school and high school ± college sports) and G2 (middle school sports only) reported significantly higher physical activity levels, as measured by MARS score (Marx et al., 2001) and Tegner activity scale (Briggs et al., 2006) than G1 (no sports), additionally G3 (middle school and high school ± college sports) reported significantly higher physical activity levels than G2 (middle school sports only) (Table 4).
Table 3.
Self-reported health history at follow-up by participation group.†
| Health history |
Total |
Group 1 |
Group 2 |
Group 3 |
p-value |
|---|---|---|---|---|---|
| N | 462 | 124 | 77 | 261 | |
| Cancer | 0 | 0 | 0 | 0 | |
| Cardiovascular disease | 0 | 0 | 0 | 0 | |
| Diabetes (any type) | 12 (2.6%) | 3 (2.4%) | 3 (3.9%) | 6 (2.3%) | 0.66* |
| High cholesterol | 23 (5.0%) | 7 (5.6%) | 5 (6.5%) | 11 (4.2%) | 0.59* |
| Hypertension | 26 (5.6%) | 9 (7.3%) | 4 (5.2%) | 13 (5.0%) | 0.64* |
| Kidney disease | 0 | 0 | 0 | 0 | |
| Fatty Liver disease | 1 (0.2%) | 1 (0.8%) | 0 | 0 | 0.44* |
| Other | 29 (6.3%) | 9 (7.3%) | 6 (7.8%) | 14 (5.4%) | 0.58* |
| None of above (response) | 375 (81.2%) | 96 (77.4%) | 59 (76.6%) | 220 (84.3%) | 0.15 |
| None (no “yes” to any of above) | 378 (81.8%) | 99 (79.8%) | 59 (76.6%) | 220 (84.3%) | 0.09 |
Data presented as mean (standard deviation) or n (%).
Group 1 – No, No, No (Middle, High School, and College); Group 2 – Yes, No, No; Group 3 – Yes, Yes, No and Yes, Yes, Yes.
p-value from Fisher’s exact test.
Table 4.
Current activity level by youth activity group.†
| N | Total |
Group 1 |
Group 2 |
Group 3 |
p-value |
|---|---|---|---|---|---|
| 462 | 124 | 77 | 261 | ||
| Total of MARS scores (0 to 16) | 6.33 (0.20) | 4.21a (0.40) | 5.92b (0.49) | 7.35c (0.26) | <0.0001* |
| Tegner activity scale (0 to 10) | 4.18 (0.09) | 3.15a (0.17) | 3.86b (0.21) | 4.69c (0.11) | <0.0001* |
Data presented as least square mean (standard error) or n (%); least square means and associated standard error are reported as measures are adjusted for age and sex.
MARS = Marx Activity Rating Scale.
*‘a’ different from ‘b’ different from ‘c’, all p < 0.05, adjusted using Tukey- Kramer
Group 1 – No, No, No (Middle, High School, and College); Group 2 – Yes, No, No; Group 3 – Yes, Yes, No and Yes, Yes, Yes.
4. Discussion
This study showed an association between persistent participation in OS from middle school through college or high school and lower BMI and waist circumference, and higher HDL-C levels at the end of high school, compared with those who did not participate at all in OS. This finding is noteworthy, given the association between BMI with cardiometabolic risk (Jago et al., 2010, Jago et al., 2013) and cardiovascular fitness (Baranowski et al., 2013) in youth. That OS participation served to promote positive cardiometabolic risk factors is reflective of previous research, which showed OS participation successfully decreased cardiovascular risk in young children (Hebert et al., 2017), slowed BMI increase in kindergarten and first-grade pupils (Dunton et al., 2012), and decreased risk for developing metabolic syndrome in adulthood (Yang et al., 2009). Unique to this study is that sport involvement was obtained at follow-up, and biophysical profile was recorded during assessment completed in grades 5–12, encompassing adolescence, which is acknowledged as a developmental stage when OS dropout is most prevalent (Howie et al., 2016, Eime et al., 2016). This study provides data on a racially diverse group, in contrast to Yang et al. (2009) who studied Finnish subjects in the early 1980s.
Additionally, this study’s follow-up data revealed that adolescents maintaining OS participation throughout school years reported significantly higher amounts of PA as young adults, relative to the non-sport cohort. This supports prior work indicating that early and continued OS engagement is important to circumvent the negative spiral of inactivity (Yang et al., 2009, Faigenbaum and Myer, 2012), especially in diverse and obesity-susceptible populations. African-Americans have a higher prevalence of obesity-related disease, including hypertension, stroke and type 2 diabetes than Caucasians (Hoffman, 2012); it would appear important that OS participation is promoted in this population. There were no significant between-group differences in diagnoses of chronic diseases (e.g. cancer, cardiovascular disease, diabetes, etc.) reported at follow-up.
There was significant difference between OS participation between girls and boys over time, which supports Howie et al., who found that boys join sports in adolescence, despite earlier non-participation; however, girls not involved prior to age 8 are not likely to become involved as they age (Howie et al., 2016). Promoting OS at earlier ages, with special attention paid to girls and African-American children, may be a strategy to increase PA. Community sport organizations partnering with schools on recreational sports, as opposed to competitive sports, may provide an avenue for increased access. One example is an after-school soccer program that included service and creative writing components, which increased MVPA in overweight 4th and 5th graders (Madsen et al., 2013).
The manner in which OS participation improves cardiovascular risk is likely related to enhanced cardiovascular fitness acquired through the opportunities for PA. Childhood and adolescent cardiovascular fitness has been strongly associated with cardiovascular disease risk factors in multiple studies, with a systematic review noting moderate evidence that it can predict the presence of metabolic syndrome in adulthood (Ruiz et al., 2009). OS most often provides more PA to participants than those not involved; however, some research shows that participation in sports does not guarantee that a young person will reach recommended PA levels (Marques et al., 2016, Sacheck et al., 2011). In addition, we note that cardiovascular fitness is also obtained through physical activity not associated with organized sports participation. Participation in a wide spectrum of physical activities can impact fitness and adiposity, as can other healthy habits such as fruit and vegetable consumption; we do not have full understanding of physical activity’s effect on long term disease (Araujo Fernandes et al., 2015).
This study showed that OS participation through high school and/or college led to significantly higher levels of reported PA at the 10-year follow-up. This finding is consistent with previous research that revealed weekly or twice-weekly sports participation was associated with high levels of PA in later life (Tammelin et al., 2003). Similarly, research has shown that adult PA levels (Bélanger et al., 2015) and body composition (Belanger et al., 2018) are positively associated with number of years participating in sports during adolescence. However, these studies relied on self-reported PA on an annual basis, while the outcome measures included only those relating to body composition.
Yang et al. studied whether persistent athletic participation, as opposed to those who were ‘starters’ or leavers’, had lower risk for adulthood metabolic syndrome (Yang et al., 2009). In 789 girls and 704 boys in Finland, ages 3–18 on enrollment and 24–39 on follow up, subjects were categorized ‘persistent athlete’, ‘starter’ (previous non-athlete who joined OS at least once a week), ‘leaver’ (previous athlete who stopped OS), and ‘non-athlete’ groups. Persistent athletes had the lowest odds ratios of metabolic syndrome in adulthood, with non-athletes and leavers having significantly higher odds ratios than the persistent athletes, in both men and women. However, those who were sport ‘starters’ also had significantly reduced risk of metabolic syndrome, although not as robust as the ‘persistent athlete’ group.
Howie et al. (2016) studied the effect of consistent OS participation on PA and body composition on 824 girls and 855 boys in Australia, from ages 5–17, asking parents if their child participated in OS outside school hours. A little over a third of both girls (34.3%) and boys (36.9%) were labeled ‘sport dropouts’, with around half of girls (47.5%) and boys (55.2%) labeled ‘consistent sport participators’. Consistent sports participation was associated with higher lean mass in girls and higher lean mass, higher PA, and lower body fat in boys. Any sports participation was associated with higher lean mass, despite sport dropout. Similar to Howie et al. (2016), the current study shows that even some sport participation has health benefits. However, not all research shows clear obesity or cardiovascular risk reduction. Notably, a systematic review of OS participation and weight status did not show a definite association, reviewing 19 studies that measured sport participation and BMI (Nelson et al., 2011). However, that study did not present meta-analytical data to objectively determine strength of associations.
Certain study limitations should be noted. Firstly, the use of self-reporting questionnaires to obtain information on health history and physical activity levels carries inherent risk of information recall bias (Althubaiti, 2020); however, self-reported questionnaires are commonly used in health-based research and were deemed appropriate for this study, due to both sample size and timespan prior to follow-up. Secondly, OS participation during the initial Princeton School District study was defined generally, without taking into account differences in duration, frequency, and intensity of training and competition. There was low known/diagnosed chronic disease in our population; no differences were noted between OS participation groups. However, this study was completed in young adulthood, in a relatively underserved population.
Despite these limitations, the current study makes an original and significant contribution to the literature. Capitalizing on data from the cohort from the original longitudinal investigation, follow-up provides supportive data that serial sports participation during middle school, high school, and college is associated with superior health biomarkers in high school and continued higher PA in young adulthood. It provides novel data in a racially diverse population during adolescence, a time when many drop out of sport. Sports participation through middle school and high school may play an important role in controlling concurrent BMI and HDL-C levels. It also shows that ‘activity breeds activity’: youth engaging in more PA may engage in more adult PA, potentially positively affecting cardiovascular disease risk later in life. However, this did not affect the frequency of known chronic disease, although the follow-up interval may be too soon to identify an effect.
5. Declaration
The results of the study are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation.
CRediT authorship contribution statement
Kelsey Logan: Conceptualization, Data curation, Methodology, Writing - original draft, Writing - review & editing. Rhodri S. Lloyd: Data Analysis and interpretation, Visualization, Writing - review & editing. Tara Schafer-Kalkhoff: Conceptualization, Ddata curation, Investigation, Methodology, Project administration, Supervision, Writing - original draft, Writing - review & editing. Jane C. Khoury: Conceptualization, Data curation, Formal analysis, Methodology, Validation, Writing - original draft, Writing - review & editing. Shelley Ehrlich: Formal analysis, Methodology, Writing - original draft, Writing - review & editing. Lawrence M. Dolan: Conceptualization, Data curation, Investigation, Methodology, Funding acquisition, Resources, Supervision, Validation, Visualization, Writing - review & editing. Amy S. Shah: Investigation, Methodology, Visualization, Writing - review & editing. Gregory D. Myer: Conceptualization, Data curation, Investigation, Methodology, Funding acquisition, Project administration, Supervision, Visualization, Resources, Writing - original draft, Writing - review & editing.
Funding
None.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgements
Gregory D. Myer consults with Commercial entities to support application to the US Food and Drug Administration but has no financial interest in the commercialization of the products. Dr. Myer’s institution receives current and ongoing grant funding from National Institutes of Health/NIAMS Grants U01AR067997, R01 AR070474, and industry sponsored research funding related to brain injury prevention and assessment with Q30 Innovations, LLC, and ElMinda, Ltd. Dr. Myer receives author royalties from Human Kinetics and Wolters Kluwer. Dr. Myer is an inventor of biofeedback technologies (2017 Non Provisional Patent Pending- Augmented and Virtual reality for Sport Performance and Injury Prevention Application filed 11/10/2016 (62/420,119), Software Copyrighted.) designed to enhance rehabilitation and prevent injuries and has potential for future licensing royalties.
The other authors have indicated they have no financial relationships relevant to this article to disclose.
References
- Althubaiti A. Information bias in health research: definition, pitfalls, and adjustment methods. J. Multidiscip. Healthc. 2016;9:211–217. doi: 10.2147/JMDH.S104807. Epub 2016/05/25. PubMed PMID: 27217764; PubMed Central PMCID: PMCPMC4862344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angeli S., Angeli D., Eichman N., Sielski M., Amundson M. Relationship between high school athletic participation and adult fitness and metabolic health. J. Am. Coll. Cardiol. 2017;69(11):1779. PubMed PMID: WOS:000397342302501. [Google Scholar]
- Araujo Fernandes R., Joao Coelho-e-Silva M., Carlos Spiguel Lima M., Ungari Cayres S., Sanches Codogno J. Possible underestimation by sports medicine of the effects of early physical exercise practice on the prevention of diseases in adulthood. Curr. Diabetes Rev. 2015;11(3):201–205. doi: 10.2174/1573399811666150401104515. [DOI] [PubMed] [Google Scholar]
- Baranowski T., Chen T.A., Mendoza J.A., O’Connor T., Baranowski J., Jago R. Prospective BMI category change associated with cardiovascular fitness change. Med. Sci. Sports Exercise. 2013;45(2):294–298. doi: 10.1249/MSS.0b013e3182703774. Epub 2012/09/01. PubMed PMID: 22935738; PubMed Central PMCID: PMCPMC3552042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belanger M., Katapally T.R., Barnett T.A., O’Loughlin E., Sabiston C.M., O’Loughlin J. Link between physical activity type in adolescence and body composition in adulthood. Med. Sci. Sports Exercise. 2018;50(4):709–714. doi: 10.1249/MSS.0000000000001503. Epub 2017/12/07. PubMed PMID: 29210917. [DOI] [PubMed] [Google Scholar]
- Bélanger M., Sabiston C.M., Barnett T.A., O’Loughlin E., Ward S., Contreras G., O’Loughlin J. Number of years of participation in some, but not all, types of physical activity during adolescence predicts level of physical activity in adulthood: results from a 13-year study. Int. J. Behav. Nutr. Phys. Act. 2015;12:76. doi: 10.1186/s12966-015-0237-x. Epub 2015/06/11. PubMed PMID: 26058349; PubMed Central PMCID: PMCPMC4464637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell D.R., Post E.G., Biese K., Bay C., Valovich McLeod T. Sport specialization and risk of overuse injuries: a systematic review with meta-analysis. Pediatrics. 2018;142(3) doi: 10.1542/peds.2018-0657. PubMed PMID: 30135085. [DOI] [PubMed] [Google Scholar]
- Briggs K.K., Kocher M.S., Rodkey W.G., Steadman J.R. Reliability, validity, and responsiveness of the Lysholm knee score and Tegner activity scale for patients with meniscal injury of the knee. J. Bone Joint Surg. Am. 2006;88(4):698–705. doi: 10.2106/JBJS.E.00339. Epub 2006/04/06. PubMed PMID: 16595458. [DOI] [PubMed] [Google Scholar]
- Butcher J., Lindner K.J., Johns D.P. Withdrawal from competitive youth sport: a retrospective ten-year study. J. Sport Behav. 2002;25(2):145–163. [Google Scholar]
- Dentro K.N., Beals K., Crouter S.E., Eisenmann J.C., McKenzie T.L., Pate R.R. Results from the United States' 2014 report card on physical activity for children and youth. J. Phys. Activity Health. 2014;11(Suppl 1):S105–S112. doi: 10.1123/jpah.2014-0184. Epub 2014/11/27. PubMed PMID: 25426905. [DOI] [PubMed] [Google Scholar]
- Dodge T., Lambert S.F. Positive self-beliefs as a mediator of the relationship between adolescents' sports participation and health in young adulthood. J. Youth Adolesc. 2009;38(6):813–825. doi: 10.1007/s10964-008-9371-y. Epub 2009/07/29. PubMed PMID: 19636783. [DOI] [PubMed] [Google Scholar]
- Dohle S., Wansink B. Fit in 50 years: participation in high school sports best predicts one’s physical activity after age 70. BMC Public Health. 2013;13:1100. doi: 10.1186/1471-2458-13-1100. PubMed PMID: 24289060; PubMed Central PMCID: PMCPMC3909353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolan L.M., Bean J., D'Alessio D., Cohen R.M., Morrison J.A., Goodman E. Frequency of abnormal carbohydrate metabolism and diabetes in a population-based screening of adolescents. J Pediatr. 2005;146(6):751–758. doi: 10.1016/j.jpeds.2005.01.045. PubMed PMID: 15973311. [DOI] [PubMed] [Google Scholar]
- Drenowatz C., Steiner R.P., Brandstetter S., Klenk J., Wabitsch M., Steinacker J.M. Organized sports, overweight, and physical fitness in primary school children in Germany. J. Obes. 2013;2013:935245. doi: 10.1155/2013/935245. Epub 2013/03/28. PubMed PMID: 23533728; PubMed Central PMCID: PMCPMC3603420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunton G., McConnell R., Jerrett M., Wolch J., Lam C., Gilliland F. Organized physical activity in young school children and subsequent 4-year change in body mass index. Arch. Pediatr. Adolesc. Med. 2012;166(8):713–718. doi: 10.1001/archpediatrics.2012.20. Epub 2012/08/08. PubMed PMID: 22869403; PubMed Central PMCID: PMCPMC3415326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eime R.M., Harvey J.T., Charity M.J., Casey M.M., Westerbeek H., Payne W.R. Age profiles of sport participants. BMC Sports Sci. Med. Rehabil. 2016;8:6. doi: 10.1186/s13102-016-0031-3. PubMed PMID: 26973792; PubMed Central PMCID: PMCPMC4788892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faigenbaum Avery D., Myer Gregory D. Exercise deficit disorder in youth: play now or pay later. Curr. Sports Med. Rep. 2012;11(4):196–200. doi: 10.1249/JSR.0b013e31825da961. Epub 2012/07/11. PubMed PMID: 22777330. [DOI] [PubMed] [Google Scholar]
- Hardy L.L., O'Hara B.J., Rogers K., St George A., Bauman A. Contribution of organized and nonorganized activity to children's motor skills and fitness. J. School Health. 2014;84(11):690–696. doi: 10.1111/josh.12202. PubMed PMID: 25274168. [DOI] [PubMed] [Google Scholar]
- Harris P.A., Taylor R., Minor B.L., Elliott V., Fernandez M., O'Neal L. The REDCap consortium: building an international community of software platform partners. J. Biomed. Informat. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hebert J.J., Klakk H., Moller N.C., Grontved A., Andersen L.B., Wedderkopp N. The prospective association of organized sports participation with cardiovascular disease risk in children (the CHAMPS study-DK). Mayo Clin. Proc. 2017;92(1):57–65. doi: 10.1016/j.mayocp.2016.08.013. Epub 2016/11/21. PubMed PMID: 27865444. [DOI] [PubMed] [Google Scholar]
- Hoffman R.P. Effect of adolescent obesity on cardiometabolic risk in African-Americans and caucasians. ISRN Obesity. 2012;2012:603205. doi: 10.5402/2012/603205. Epub 2012/01/01. PubMed PMID: 24533206; PubMed Central PMCID: PMCPMC3914275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howie E.K., McVeigh J.A., Smith A.J., Straker L.M. Organized sport trajectories from childhood to adolescence and health associations. Med. Sci. Sports Exercise. 2016;48(7):1331–1339. doi: 10.1249/MSS.0000000000000894. PubMed PMID: 27314410. [DOI] [PubMed] [Google Scholar]
- Jago R., Drews K.L., McMurray R.G., Thompson D., Volpe S.L., Moe E.L. Fatness, fitness, and cardiometabolic risk factors among sixth-grade youth. Med. Sci. Sports Exercise. 2010;42(8):1502–1510. doi: 10.1249/MSS.0b013e3181d322c4. Epub 2010/02/09. PubMed PMID: 20139783; PubMed Central PMCID: PMCPMC2921216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jago R., Drews K.L., McMurray R.G., Baranowski T., Galassetti P., Foster G.D. BMI change, fitness change and cardiometabolic risk factors among 8th grade youth. Pediatr. Exercise Sci. 2013;25(1):52–68. doi: 10.1123/pes.25.1.52. Epub 2013/02/15. PubMed PMID: 23406707; PubMed Central PMCID: PMCPMC3702158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimm S.Y., Glynn N.W., Kriska A.M., Barton B.A., Kronsberg S.S., Daniels S.R. Decline in physical activity in black girls and white girls during adolescence. N. Engl. J. Med. 2002;347(10):709–715. doi: 10.1056/NEJMoa003277. Epub 2002/09/06. 10.1056/NEJMoa003277 PubMed PMID: 12213941. [DOI] [PubMed] [Google Scholar]
- Kwon S., Janz K.F., Letuchy E.M., Burns T.L., Levy S.M. Developmental trajectories of physical activity, sports, and television viewing during childhood to young adulthood: Iowa bone development study. JAMA Pediatr. 2015;169(7):666–672. doi: 10.1001/jamapediatrics.2015.0327. PubMed PMID: 25984811; PubMed Central PMCID: PMCPMC4596396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logan K., Cuff S. Organized sports for children, preadolescents, and adolescents. Pediatrics. 2019 doi: 10.1542/peds.2019-0997. Epub 2019/05/22. PubMed PMID: 31110166. [DOI] [PubMed] [Google Scholar]
- Logan K., Cuff S. Organized sports for children, preadolescents, and adolescents. Pediatrics. 2019;143(6) doi: 10.1542/peds.2019-0997. [DOI] [PubMed] [Google Scholar]
- Madsen K., Thompson H., Adkins A., Crawford Y. School-community partnerships: a cluster-randomized trial of an after-school soccer program. JAMA Pediatr. 2013;167(4):321–326. doi: 10.1001/jamapediatrics.2013.1071. PubMed PMID: 23440308; PubMed Central PMCID: PMCPMC3667387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marques A., Ekelund U., Sardinha L.B. Associations between organized sports participation and objectively measured physical activity, sedentary time and weight status in youth. J. Sci. Med. Sport. 2016;19(2):154–157. doi: 10.1016/j.jsams.2015.02.007. Epub 2015/03/15. PubMed PMID: 25766508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marx R.G., Stump T.J., Jones E.C., Wickiewicz T.L., Warren R.F. Development and evaluation of an activity rating scale for disorders of the knee. Am. J. Sports Med. 2001;29(2):213–218. doi: 10.1177/03635465010290021601. PubMed PMID: 11292048. [DOI] [PubMed] [Google Scholar]
- Menschik D., Ahmed S., Alexander M.H., Blum R.W. Adolescent physical activities as predictors of young adult weight. Arch. Pediatr. Adolesc. Med. 2008;162(1):29–33. doi: 10.1001/archpediatrics.2007.14. PubMed PMID: 18180409. [DOI] [PubMed] [Google Scholar]
- Merkel D.L. Youth sport: positive and negative impact on young athletes. Open Access J. Sports Med. 2013;4:151–160. doi: 10.2147/OAJSM.S33556. PubMed PMID: 24379720; PubMed Central PMCID: PMCPMC3871410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson T.F., Stovitz S.D., Thomas M., LaVoi N.M., Bauer K.W., Neumark-Sztainer D. Do youth sports prevent pediatric obesity? A systematic review and commentary. Curr. Sports Med. Rep. 2011;10(6):360–370. doi: 10.1249/JSR.0b013e318237bf74. PubMed PMID: 22071397; PubMed Central PMCID: PMCPMC4444042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pate R.R., Trost S.G., Levin S., Dowda M. Sports participation and health-related behaviors among US youth. Arch. Pediatr. Adolesc. Med. 2000;154(9):904–911. doi: 10.1001/archpedi.154.9.904. PubMed PMID: 10980794. [DOI] [PubMed] [Google Scholar]
- Ruiz J.R., Castro-Pinero J., Artero E.G., Ortega F.B., Sjostrom M., Suni J. Predictive validity of health-related fitness in youth: a systematic review. British J. Sports Med. 2009;43(12):909–923. doi: 10.1136/bjsm.2008.056499. PubMed PMID: 19158130. [DOI] [PubMed] [Google Scholar]
- Sacheck J.M., Nelson T., Ficker L., Kafka T., Kuder J., Economos C.D. Physical activity during soccer and its contribution to physical activity recommendations in normal weight and overweight children. Pediatr. Exercise Sci. 2011;23(2):281–292. doi: 10.1123/pes.23.2.281. Epub 2011/06/03 PubMed PMID: 21633140. [DOI] [PubMed] [Google Scholar]
- Silva G., Andersen L.B., Aires L., Mota J., Oliveira J., Ribeiro J.C. Associations between sports participation, levels of moderate to vigorous physical activity and cardiorespiratory fitness in children and adolescents. J. Sports Sci. 2013;31(12):1359–1367. doi: 10.1080/02640414.2013.781666. PubMed PMID: 23631663. [DOI] [PubMed] [Google Scholar]
- Tammelin T., Nayha S., Hills A.P., Jarvelin M.R. Adolescent participation in sports and adult physical activity. Am. J. Prevent. Med. 2003;24(1):22–28. doi: 10.1016/s0749-3797(02)00575-5. Epub 2003/01/30 PubMed PMID: 12554020. [DOI] [PubMed] [Google Scholar]
- Telford R.M., Telford R.D., Cochrane T., Cunningham R.B., Olive L.S., Davey R. The influence of sport club participation on physical activity, fitness and body fat during childhood and adolescence: the LOOK longitudinal study. J. Sci. Med. Sport/Sports Med. Aust. 2016;19(5):400–406. doi: 10.1016/j.jsams.2015.04.008. Epub 2015/06/27. PubMed PMID: 26111721. [DOI] [PubMed] [Google Scholar]
- Vella S.A., Swann C., Allen M.S., Schweickle M.J., Magee C.A. Bidirectional associations between sport involvement and mental health in adolescence. Med. Sci. Sports Exercise. 2017;49(4):687–694. doi: 10.1249/MSS.0000000000001142. PubMed PMID: 27801745. [DOI] [PubMed] [Google Scholar]
- Yang X., Telama R., Hirvensalo M., Viikari J.S., Raitakari O.T. Sustained participation in youth sport decreases metabolic syndrome in adulthood. Int. J. Obes. (London) 2009;33(11):1219–1226. doi: 10.1038/ijo.2009.171. Epub 2009/09/02. PubMed PMID: 19721447. [DOI] [PubMed] [Google Scholar]