Abstract
Lactobacilli are commensal bacteria in the normal flora of the oral cavity, gastrointestinal and genital tract. However, few cases of lactobacilli-induced bacteremia or endocarditis have been reported, particularly in immunocompromised patients. We reported a rare case of a 57-year-old man with a Lactobacillus rhamnosus endocarditis without immunodeficiency in his medical history. He received a dental scaling one year before. Clinical presentation included weight loss, heart murmur, ankle arthritis and splinter hemorrhage. Echocardiography showed a mitral prolapse and a 16 mm vegetation associated with a valvular perforation. All blood cultures were positive for Lactobacillus rhamnosus. Antibacterial regimen with amoxicillin and gentamicin led to recovery without surgery. We present a literature review of the lactobacillary endocarditis cases published since 1992. Valvulopathy, dental or invasive procedures and probiotics use were the main underlying conditions, in contrary to immunodeficiency. Diagnosis of lactobacillary endocarditis should be more considered and a treatment with penicillin and aminoglycoside should be promptly introduced in life-threatening cases.
Keywords: Lactobacillus rhamnosus, endocarditis, immunocompetent
Introduction
Lactobacilli are rod-shaped bacteria, facultatively anaerobic, found in the normal flora of the oral cavity, gastrointestinal and genital tract. The organisms are used as probiotic bacteria or in fermented food product. Previously considered as a contaminant, the evidence was made that Lactobacillus is able to induce severe infections like endocarditis in a rat model (1) and in human (2,3). More than one hundred Lactobacillus endocarditis (LE) cases have been described in the literature and already collected in different reviews of cases ([3], [4], [5]). We report a rare case of endocarditis caused by Lactobacillus rhamnosus in a patient without immunodeficiency. We reviewed all reported cases since the introduction of the Duke’s criteria in 1992, reopening and completing the series of Salvana et al. from 1992 to 2005 (5). All the reports were studied, even papers in Spanish after translation. We assessed patients’ characteristics, Lactobacillus species, treatments and outcome.
Case presentation
A 57-year-old man was admitted in the unit of internal medicine for a persistent inflammatory syndrome, fatigue and a right ankle arthritis. He was machine operator in the steel industry, retired one year before. His medical history included an interatrial communication surgery in 2003 and a teeth scaling one year before. He has experienced an extreme fatigue for 9 months. 6 months before, a first laboratory investigation demonstrated elevated CRP and ESR. He related only one episode of hyperthermia (38 °C) and no night sweats. 3 months before, he presented a left ankle arthritis with cutaneous eruption described as petechiae. He received amoxicillin during one week and the symptoms disappeared. He went on losing weight without anorexia or intestinal symptoms. CRP and ESR had varied but always above normal levels. A thoracic-abdominal-pelvic CT was performed and any infectious lesion or tumor was found. 3 weeks before hospitalization, he presented a new swelling of his right ankle and large joint arthralgia. He was referred to our unit.
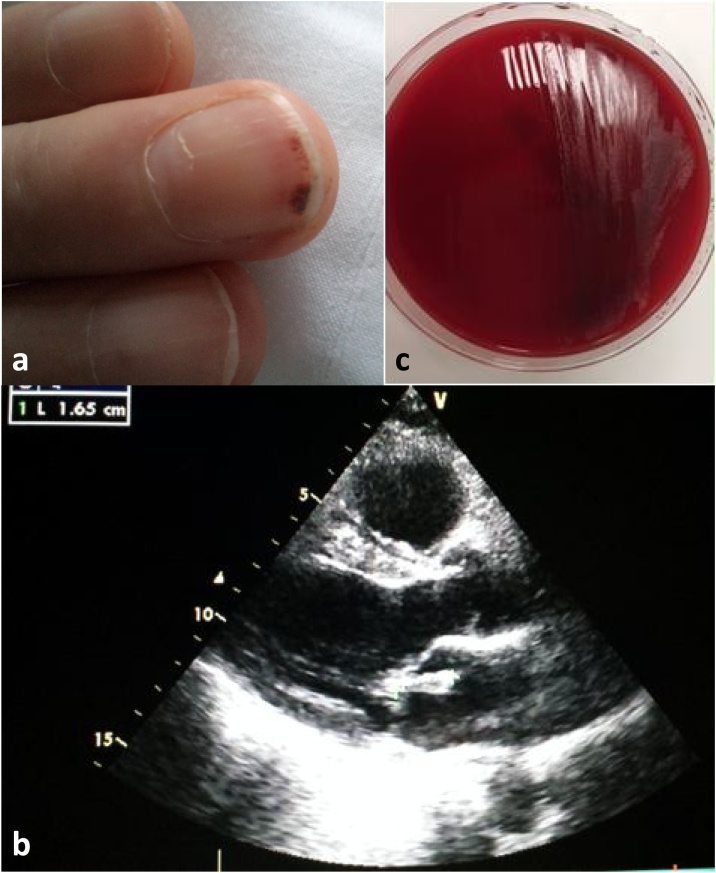
Clinical examination showed no fever, a total weight loss of 4 kg, an isolated swollen ankle, a nail with a splinter hemorrhage (Fig. 1A) and a systolic, 1/6 intensity heart murmur. He had no signs of heart failure or severe sepsis. A transthoracic echocardiography was rapidly performed and revealed a mitral valvular vegetation of 16 mm associated with a valvular perforation and a grade II leak (Fig. 1B). In addition, a mitral prolapse was seen. It was supposed that the prolapse was anterior to the infectious process because the subvalvular tract was not involved. Empiric intravenous antimicrobial treatment was immediately started by amoxicillin 12 g per day and gentamicin 3 mg/kg after three sets of blood cultures drawn at 30 minute intervals. All of them were positive for Lactobacillus rhamnosus after 46 hours. Lactobacillus rhamnosus was identified by Matrix-Assisted Laser Desorption Ionization - Time of Flight (MALDI-TOF) Mass Spectrometry with the MALDI Biotyper® from Bruker Corporation© (Fig. 1C). The sensitivity profile allowed us to continue the same antibacterial regimen. The ankle swelling disappeared after two days, the blood inflammation markers rapidly decreased and the blood cultures were negative after one week. The embolic risk was high and a surgery was planned 15 days later. But two days before the surgery, a transoesophageal echocardiography showed that the mitral vegetation almost completely disappeared, thus the surgery was cancelled. Gentamicin was stopped after 2 weeks, switched by orally rifampin. Amoxicillin and rifampin were continued 4 more weeks. During this period, he consulted a dentist and several teeth extractions were decided.
Fig. 1.
Splinter hemorrhage (a). Transthoracic echocardiography: mitral valvular vegetation (b). Bacterial growth on Columbia blood agar with sheep blood (c).
Discussion
Since 1992, 50 cases of LE were reported ([6], [7], [8], [9], [10], [11], [12], [13], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25],5,[26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45], [46], [47], [48], [49], [50]). Their characteristics were summarized in the Table 1. The mean age of patients was 52.4 years [16-85]. 68% of them were male. Concerning underlying conditions, a valvulopathy was reported in 64% of patients and 14% of endocarditis occurred on a prosthetic valve. A dental procedure or an invasive procedure were found in 34% and 22% of cases, respectively. 22% of patient used probiotics. Immunosuppression involved only 16% of them. After fever or chills, experienced by 72% of patients, the most common symptoms were a new murmur (30%), respiratory signs (30%, such as dyspnea or crackles) and weight loss (28%). LE affected aortic and mitral valve in the same proportion (22%). Tricuspid valve was involved in only 2 cases (4%) and any cases with pulmonary valve endocarditis has been reported. Lactobacillus rhamnosus was the most isolated species (24%) following by L. acidophilus (18%), L. paracasei (12%) and L. casei (12%). Surgery was needed in half of the cases (54%). Mortality rate remained high (10%). Antimicrobial susceptility was available in 26 studies (5,9,10,17,18,[20], [21], [22], [23], [24], [25],[28], [29], [30], [31],[34], [35], [36], [37],39,41,44,[46], [47], [48]), including ours (Table 2). Lactobacilli are highly sensitive to penicillin G (86%), aminopenicillins (amoxicillin 86%, ampicillin 83%), clindamycin (100%), rifampin (90%), aminoglycosides such as gentamicin (79%) but most of time resistant to vancomycin and cefotaxime (sensitivity in 21% and 43% of cases, respectively). In cases reported here, a large number of different antibacterials were used, often in combination, showing that no consensual treatment exists (Table 3). Penicillin G, ampicillin and gentamicin were the most given drugs in first line (36%, 18% and 42%, respectively). Double antimicrobial therapy was proposed in first line in 58% of cases. 40% of patients were treated with only one line of antimicrobial, meaning that first line was continued after results of antibacterial susceptibility. Changes were needed in 36% of cases. Mean of duration was 44.7 days, and median was 42 days. In conclusion, lactobacilli were proved to be responsible for severe infection like endocarditis, with a common use of surgery and a substantial mortality rate. Valvulopathy appeared as the main predisposing factor. Dental or invasive procedures but also probiotics intake could be associated with LE. As patients were mostly immunocompetent, LE diagnosis should be considered more often. High-dose penicillin, combined with an aminoglycoside should be recommended in first line and clindamycin should be prefered to vancomycin in penicillin-allergic patients. Antimicrobial duration should be at least 6 weeks. Guidelines for the management of LE are needed.
Table 1.
Summary of patients’ characteristics.
| Characteristic | All cases | Characteristic | All cases | |
|---|---|---|---|---|
| n = 50 | n = 50 | |||
| Age (years) | Valve, n (%) | |||
| Mean | 52.4 | Aortic | 22 (44) | |
| Median | 56.5 | Mitral | 22 (44) | |
| Range | 16-85 | Pulmonary | 2 (4) | |
| Tricuspid | 0 | |||
| Sex, n (%) | ||||
| Female | 19 (38) | Embolus, n (%) | ||
| Male | 31 (62) | Yes | 15 (30) | |
| No | 23 (46) | |||
| Medical history, n (%) | Unknown | 12 (24) | ||
| Valvulopathy | 32 (64) | |||
| Valve prothesis | 7 (14) | Species, n (%) | ||
| Dental procedure | 17 (34) | L. rhamnosus | 12 (24) | |
| Invasive procedure | 11 (22) | L. acidophilus | 9 (18) | |
| Probiotics use | 11 (22) | L. spp | 7 (14) | |
| Immunosuppression | 8 (16) | L. paracasei | 6 (12) | |
| L. casei | 6 (12) | |||
| Symptoms, n (%) | L. jensenii | 5 (10) | ||
| Weight loss | 14 (28) | L. garvieae | 1 (2) | |
| Malaise | 5 (10) | L. gasseri | 1 (2) | |
| Fever/chills | 36 (72) | L. zeae | 1 (2) | |
| New murmur | 15 (30) | L. curvatus | 1 (2) | |
| Respiratory signs | 15 (30) | L. fermentum | 1 (2) | |
| Edema | 4 (8) | |||
| Arthritis | 8 (16) | Surgery, n (%) | ||
| Myalgia | 8 (16) | Yes | 27 (54) | |
| Cutaneous signs | 10 (20) | No | 20 (40) | |
| Abdominal pain | 3 (6) | Unknown | 3 (6) | |
| Hepato/splenomegaly | 6 (12) | |||
| Splinter hemorrhage | 3 (6) | Death, n (%) | 5 (10) | |
| Chest pain | 3 (6) | |||
| Neurological signs | 7 (14) | |||
| Unusual sweats | 5 (10) | |||
Table 2.
Antimicrobial susceptibility
| Antibiotic agents | Percent sensitive, % (n) |
|---|---|
| penicillin G | 86% (n = 21) |
| ampicillin | 86% (n = 7) |
| amoxicillin | 83% (n = 6) |
| erythromycin | 100% (n = 11) |
| clindamycin | 100% (n = 18) |
| rifampicin | 90% (n = 10) |
| vancomycin | 21% (n=19) |
| cefotaxime | 43% (n = 7) |
| gentamicin | 79% (n = 14) |
| imipenem | 73% (n = 11) |
| ciprofloxacin | 57% (n = 7) |
Table 3.
Antimicrobial use in Lactobacillus endocarditis (type, associations, number of lines and duration).
| azithromycin | 1 (2) | − | |
|---|---|---|---|
| clindamycin | 3 (6) | 4 (8) | |
| Other | |||
| vancomycin | 8 (16) | 4 (8) | |
| teicoplanin | 2 (4) | 2 (4) | |
| linezolid | − | 1 (2) | |
| rifampicin | 2 (4) | 4 (8) | |
| cotrimoxazole | 1 (2) | − | |
| daptomicin | 1 (2) | 1 (2) | |
| doxycyclin | 1 (2) | − | |
| chloramphenicol | 1 (2) | 1 (2) | |
| probenicid | − | 1 (2) | |
| Monotherapy | 6 (12) | 13 (26) | |
| Bitherapy | 29 (58) | 27 (54) | |
| Tritherapy | 7 (14) | 4 (8) | |
| Number of lines | |||
| 1 | 20 (40) | ||
| 2 | 18 (36) | ||
| 3 | 7 (14) | ||
| 4 | 1 (2) | ||
| Antibiotic duration (d) | |||
| Mean | 44.7 | ||
| Median | 42 | ||
| Range | 5-93 | ||
Patient’s consent statement
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
CRediT authorship contribution statement
J. Campagne: Writing - original draft. J.F. Guichard: Writing - review & editing. M.C. Moulhade: Writing - reviewing & editing. H. Kawski: Writing - review & editing. F. Maurier: Writing - review & editing, Supervision.
Declaration of Competing Interest
The authors declare that this work was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.Vankerckhoven V., Moreillon P., Piu S., Giddey M., Huys G., Vancanneyt M. Infectivity of Lactobacillus rhamnosus and Lactobacillus paracasei isolates in a rat model of experimental endocarditis. J Med Microbiol. 2007;56(Pt 8):1017–1024. doi: 10.1099/jmm.0.46929-0. [DOI] [PubMed] [Google Scholar]
- 2.Jones JW, Paull SN. Effect of biofilm culture on antibiotic susceptibility of lactobacilli causing endocarditis. J Infect. 1995;31(1):80–81. doi: 10.1016/s0163-4453(95)91736-5. [DOI] [PubMed] [Google Scholar]
- 3.Cannon J.P., Lee T.A., Bolanos J.T., Danziger L.H. Pathogenic relevance of Lactobacillus: a retrospective review of over 200 cases. Eur J Clin Microbiol Infect Dis Off Publ Eur Soc Clin Microbiol. 2005;24(1):31–40. doi: 10.1007/s10096-004-1253-y. [DOI] [PubMed] [Google Scholar]
- 4.Griffiths J.K., Daly J.S., Dodge R.A. Two cases of endocarditis due to Lactobacillus species: antimicrobial susceptibility, review, and discussion of therapy. Clin Infect Dis Off Publ Infect Dis Soc Am. 1992;15(2):250–255. doi: 10.1093/clinids/15.2.250. [DOI] [PubMed] [Google Scholar]
- 5.Salvana EMT, Frank M. Lactobacillus endocarditis: case report and review of cases reported since 1992. J Infect. 2006;53(1):e5–10. doi: 10.1016/j.jinf.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 6.Verani D.A., Carretto E., Bono L., Moggio G., Marone P. Lactobacillus casei endocarditis in an intravenous heroin drug addict: a case report. Funct Neurol. 1993;8(5):355–357. [PubMed] [Google Scholar]
- 7.Puleo J.A., Shammas N.W., Kelly P., Allen M. Lactobacillus isolated pulmonic valve endocarditis with ventricular septal defect detected by transesophageal echocardiography. Am Heart J. 1994;128(6 Pt 1):1248–1250. doi: 10.1016/0002-8703(94)90761-7. [DOI] [PubMed] [Google Scholar]
- 8.Gallemore G.H., Mohon R.T., Ferguson D.A. Lactobacillus fermentum endocarditis involving a native mitral valve. J Tenn Med Assoc. 1995;88(8):306–308. [PubMed] [Google Scholar]
- 9.Bessis D., Le Quellec A., Sotto A., Perez C., Ciurana A.J. Lactobacillus acidophilus endocarditis after an appendectomy. Clin Infect Dis Off Publ Infect Dis Soc Am. 1995;20(3):724–725. doi: 10.1093/clinids/20.3.724. [DOI] [PubMed] [Google Scholar]
- 10.Monterisi A., Dain A.A., Suárez de Basnec M.C., Roca G., Trucchia R., Bantar C. [Native-valve endocarditis produced by Lactobacillus casei sub. rhamnosus refractory to antimicrobial therapy] Medicina (Mex). 1996;56(3):284–286. [PubMed] [Google Scholar]
- 11.Vaghjimal A., Lutwick L.I., Chapnick E.K. Endocarditis caused by Lactobacillus. Postgrad Med J. 1997;73(855):61–62. doi: 10.1136/pgmj.73.855.61-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Husni R.N., Gordon S.M., Washington J.A., Longworth D.L. Lactobacillus bacteremia and endocarditis: review of 45 cases. Clin Infect Dis Off Publ Infect Dis Soc Am. 1997;25(5):1048–1055. doi: 10.1086/516109. [DOI] [PubMed] [Google Scholar]
- 13.Penot J.P., Lagrange P., Darodes N., Ploy M.C., Violet T., Virot P. [Lactobacillus acidophilus endocarditis] Presse Medicale Paris Fr. 1983;27(21):1009–1012. [PubMed] [Google Scholar]
- 14.Vogt HB, Hoffman WW. A case of Lactobacillus acidophilus endocarditis successfully treated with cefazolin and gentamicin. S D J Med. 1998;51(5):153–156. [PubMed] [Google Scholar]
- 15.Ruiz E., Alemán C., Alegre J., Planes A., Fernández de Sevilla T. Endocarditis caused by Lactobacillus casei. Apropos of a case. Enferm Infecc Microbiol Clin. 1998;16(3):154–155. [PubMed] [Google Scholar]
- 16.Feldmesser M., Gordon G.M., Robbins N. Lactobacillus endocarditis: a case report of outpatient management. Heart Dis Hagerstown Md. 1999;1(4):208–209. [PubMed] [Google Scholar]
- 17.Mackay A.D., Taylor M.B., Kibbler C.C., Hamilton-Miller JMT. Lactobacillus endocarditis caused by a probiotic organism. Clin Microbiol Infect Off Publ Eur Soc Clin Microbiol Infect Dis. 1999;5(5):290–292. doi: 10.1111/j.1469-0691.1999.tb00144.x. [DOI] [PubMed] [Google Scholar]
- 18.Mitchell AR, Hayek LJ. Lactobacillus endocarditis. J Infect. 1999;38(3):200–201. doi: 10.1016/s0163-4453(99)90255-4. [DOI] [PubMed] [Google Scholar]
- 19.Schmidt V, Wolter M, Lenschow U, Kienast W. Lactobacillus paracasei endocarditis in an 18-yeard-old patient with trisomy 21, atrioventricular septal defect and Eisenmenger complex: therapeutic problems. Klin Padiatr. 2001;213(1):35–38. doi: 10.1055/s-2001-11272. [DOI] [PubMed] [Google Scholar]
- 20.Avlami A., Kordossis T., Vrizidis N., Sipsas N.V. Lactobacillus rhamnosus endocarditis complicating colonoscopy. J Infect. 2001;42(4):283–285. doi: 10.1053/jinf.2001.0793. [DOI] [PubMed] [Google Scholar]
- 21.Presterl E., Kneifel W., Mayer H.K., Zehetgruber M., Makristathis A., Graninger W. Endocarditis by Lactobacillus rhamnosus due to yogurt ingestion? Scand J Infect Dis. 2001;33(9):710–714. doi: 10.1080/00365540110026953. [DOI] [PubMed] [Google Scholar]
- 22.Wallet F., Dessein R., Armand S., Courcol R.J. Molecular diagnosis of endocarditis due to Lactobacillus casei subsp. rhamnosus. Clin Infect Dis Off Publ Infect Dis Soc Am. 2002;35(10):e117–119. doi: 10.1086/344181. [DOI] [PubMed] [Google Scholar]
- 23.Soleman N., Laferl H., Kneifel W., Tucek G., Budschedl E., Weber H. How safe is safe?--a case of Lactobacillus paracasei ssp. paracasei endocarditis and discussion of the safety of lactic acid bacteria. Scand J Infect Dis. 2003;35(10):759–762. doi: 10.1080/00365540310015872. [DOI] [PubMed] [Google Scholar]
- 24.Romero-Pérez Jc, Padilla-Salazar Ml, Romero-Garrido R, Batista-Díaz N. Endocarditis due to Lactobacillus acidophilus in a patient with structural heart disease. Enferm Infecc Microbiol Clin. 2003;21(10):599–600. [PubMed] [Google Scholar]
- 25.Zé-Zé L., Tenreiro R., Duarte A., Salgado M.J., Melo-Cristino J., Lito L. Case of aortic endocarditis caused by Lactobacillus casei. J Med Microbiol. 2004;53(Pt 5):451–453. doi: 10.1099/jmm.0.05328-0. [DOI] [PubMed] [Google Scholar]
- 26.Makaryus A.N., Yang R., Hahn R.T., Kort S. A rare case of Lactobacillus acidophilus presenting as mitral valve bacterial endocarditis. Echocardiogr Mt Kisco N. 2005;22(5):421–425. doi: 10.1111/j.1540-8175.2005.04054.x. [DOI] [PubMed] [Google Scholar]
- 27.Yagi S., Akaike M., Fujimura M., Ise T., Yoshida S., Sumitomo Y. Infective endocarditis caused by lactobacillus. Intern Med Tokyo Jpn. 2008;47(12):1113–1116. doi: 10.2169/internalmedicine.47.0744. [DOI] [PubMed] [Google Scholar]
- 28.Cabrera J.J., Moreno E., Miranda C., Pérez M.D. Endocarditis due to Lactobacillus casei/paracasei. Enferm Infecc Microbiol Clin. 2010;28(7):474–475. doi: 10.1016/j.eimc.2009.09.013. [DOI] [PubMed] [Google Scholar]
- 29.Fradiani P.A., Petrucca A., Ascenzioni F., Di Nucci G., Teggi A., Bilancini S. Endocarditis caused by Lactobacillus jensenii in an immunocompetent patient. J Med Microbiol. 2010;59(Pt 5):607–609. doi: 10.1099/jmm.0.017764-0. [DOI] [PubMed] [Google Scholar]
- 30.Suárez-García I., Sánchez-García A., Soler L., Malmierca E., Gómez-Cerezo J. Lactobacillus jensenii bacteremia and endocarditis after dilatation and curettage: case report and literature review. Infection. 2012;40(2):219–222. doi: 10.1007/s15010-011-0182-9. [DOI] [PubMed] [Google Scholar]
- 31.Nishijima T, Teruya K, Yanase M, Tamori Y, Mezaki K, Oka S. Infectious endocarditis caused by Lactobacillus acidophilus in a patient with mistreated dental caries. Intern Med Tokyo Jpn. 2012;51(12):1619–1621. doi: 10.2169/internalmedicine.51.7294. [DOI] [PubMed] [Google Scholar]
- 32.Franko B., Vaillant M., Recule C., Vautrin E., Brion J.-P., Pavese P. Lactobacillus paracasei endocarditis in a consumer of probiotics. Med Mal Infect. 2013;43(4):171–173. doi: 10.1016/j.medmal.2013.01.007. [DOI] [PubMed] [Google Scholar]
- 33.Marciniak A, Karapanagiotidis Gt, Sarsam M, Sharma R. Postpartum Lactobacillus jensenii endocarditis in patient with bicuspid aortic valve. J Thorac Cardiovasc Surg. 2014;148(5):219–221. doi: 10.1016/j.jtcvs.2014.05.096. [DOI] [PubMed] [Google Scholar]
- 34.Botros M., Mukundan D. Lactobacillus endocarditis with prosthetic material: a case report on non-surgical management with corresponding literature review. Infect Dis Rep. 2014;6(3):5497. doi: 10.4081/idr.2014.5497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Patnaik S., Davila C.D., Chennupati A., Rubin A. Endocarditis of the native aortic valve caused by Lactobacillus jensenii. BMJ Case Rep. 2015;2015 doi: 10.1136/bcr-2014-206288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kato K., Funabashi N., Takaoka H., Kohno H., Kishimoto T., Nakatani Y. Lactobacillus paracasei endocarditis in a consumer of probiotics with advanced and severe bicuspid aortic valve stenosis complicated with diffuse left ventricular mid-layer fibrosis. Int J Cardiol. 2016;224:157–161. doi: 10.1016/j.ijcard.2016.09.002. [DOI] [PubMed] [Google Scholar]
- 37.Felekos I, Lazaros G, Tsiriga A, Pirounaki M, Stavropoulos G, Paraskevas J. Lactobacillus rhamnosus endocarditis: An unusual culprit in a patient with Barlow’s disease. Hell J Cardiol HJC Hell Kardiologike Epitheorese. 2016;57(6):445–448. doi: 10.1016/j.hjc.2016.11.011. [DOI] [PubMed] [Google Scholar]
- 38.Kestler M., Muñoz P., Marín M., Goenaga M.A., Idígoras Viedma P., de Alarcón A. Endocarditis caused by anaerobic bacteria. Anaerobe. 2017;47:33–38. doi: 10.1016/j.anaerobe.2017.04.002. [DOI] [PubMed] [Google Scholar]
- 39.Encarnacion C.O., Loranger A.M., Bharatkumar A.G., Almassi G.H. Bacterial Endocarditis Caused by Lactobacillus acidophilus Leading to Rupture of Sinus of Valsalva Aneurysm. Tex Heart Inst J. 2016;43(2):161–164. doi: 10.14503/THIJ-15-5121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Noreña I, Cabrera-Marante O, Fernández-Ruiz M. Endocarditis due to Lactobacillus rhamnosus in a patient with bicuspid aortic valve: Potential role for the consumption of probiotics? Med Clin (Barc) 2017;149(4):181–182. doi: 10.1016/j.medcli.2017.03.021. [DOI] [PubMed] [Google Scholar]
- 41.Aaron J.G., Sobieszczyk M.E., Weiner S.D., Whittier S., Lowy F.D. Lactobacillus rhamnosus Endocarditis After Upper Endoscopy. Open Forum Infect Dis. 2017;4(2) doi: 10.1093/ofid/ofx085. ofx085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Stroupe C., Pendley J., Isang E., Helms B. Persistent bacteremia secondary to delayed identification of Lactobacillus in the setting of mitral valve endocarditis. IDCases. 2017;10:132–134. doi: 10.1016/j.idcr.2017.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Martin W., Galligan J., Adams H., Palmer S. Lactobacillus acidophilus, A Probiotic or a Problem? A Case of Endocarditis Associated with Probiotic Use. Heart Lung Circ. 2017;26:S297. [Google Scholar]
- 44.Recio R, Chaves F, Reyes Ca, Orellana M.Á. Infective endocarditis due to Lactobacillus rhamnosus: Risks of probiotic consumption in a patient with structural heart disease. Enferm Infecc Microbiol Clin. 2017;35(9):609–610. doi: 10.1016/j.eimc.2017.02.004. [DOI] [PubMed] [Google Scholar]
- 45.Elikowski W., Małek-Elikowska M., Lisiecka M., Bodora A., Wiśniewska K., Oko-Sarnowska Z. Lactobacillus gasseri endocarditis on the aortic valve bioprosthesis - a case report. Pol Merkur Lek Organ Pol Tow Lek. 2017;43(257):220–223. [PubMed] [Google Scholar]
- 46.Boumis E., Capone A., Galati V., Venditti C., Petrosillo N. Probiotics and infective endocarditis in patients with hereditary hemorrhagic telangiectasia: a clinical case and a review of the literature. BMC Infect Dis. 2018;18(1):65. doi: 10.1186/s12879-018-2956-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lim S.M., Wong B., Cross G.B., Merchant R. Lactobacillus garvieae endocarditis presenting with leg cramps. IDCases. 2018;13 doi: 10.1016/j.idcr.2018.e00427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Naqvi Ssb, Nagendra V, Hofmeyr A. Probiotic related Lactobacillus rhamnosus endocarditis in a patient with liver cirrhosis. IDCases. 2018;13:e00439. doi: 10.1016/j.idcr.2018.e00439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Groga-Bada P., Mueller I.I., Foschi F., Gawaz M., Eick C. Mitral Valve Endocarditis due to Lactobacillus. Case Rep Med. 2018;2018:8613948. doi: 10.1155/2018/8613948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zeba F., Yirerong J., Assali M., Tewary G., Noska A. A Double Whammy: Lactobacillus acidophilus Bacteremia and Subsequent Lactobacillus rhamnosus Prosthetic Valve Infective Endocarditis in an Elderly Diabetic Patient. R I Med J. 2013;101(9):32–35. [PubMed] [Google Scholar]