Highlights
-
•
Assessment tools have progressed from measuring specific components, to more comprehensive assessments.
-
•
Performance-based tools, has the potential to include an EF index as part of the test scoring.
-
•
Most researchers either chose short versions of the assessment tools to address the subjects' attentional capacities.
-
•
Using more than one evaluation method enabled to draw a more precise picture of the function.
1. Introduction
The National Institute of Mental Health (2019) defined severe mental illness (SMI) as “a mental, behavioral, or emotional disorder resulting in serious functional impairment, which substantially interferes with or limits one or more major life activities.” It is an umbrella term for chronic psychiatric disorders, such as schizophrenia and schizoaffective, delusional, major depressive, and bipolar disorders (Galletly and Rigby, 2013; Ramsey and Swarbrick, 2014). According to the Diagnostic and Statistical Manual of Mental Disorders (American Psychiatric Association, 2013), most individuals with schizophrenia and related diagnoses experience dysfunction in several areas of daily living, such as self-care, but these difficulties differ among individuals and according to illness severity. Changes in the mental health system (e.g., new services), as well as rehabilitation possibilities in the community (e.g., technological solutions), have expanded opportunities for the population of individuals with SMI. These changes now enable therapists to expand their evaluation plan for daily living activities and interpret more accurate findings out of it (James and Pitonyak, 2019).
The mental health literature typically uses the term everyday life, adding more specific terms, to address activities or tasks that individuals perform daily as part of their self-routines. Each term refers to a different set of activities and often includes domains such as leisure or social participation that elsewhere are considered independent domains (James and Pitonyak, 2019). In this review, we use the term everyday life to address activities that individuals perform regularly in the community.
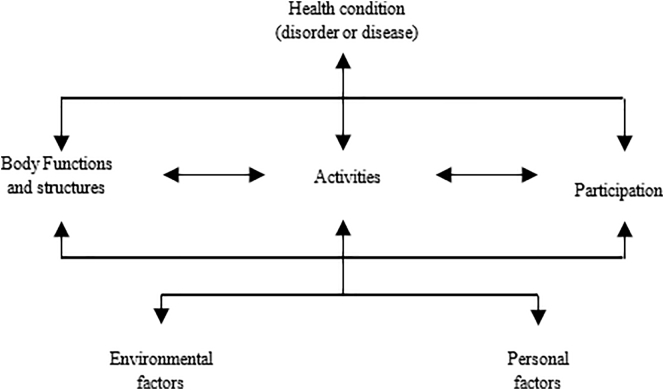
Regarding everyday life, several performance predictors can be classified according to the International Classification of Functioning, Disability, and Health (ICF; World Health Organization, 2001) taxonomy, which aims to provide a unified and standard language and framework to describe health and health-related states. As Fig. 1 shows, the ICF taxonomy describes outcome measures, quality of life, or environmental factors with a common language among a wide range of health disciplines. In this review, the domains discussed relate to three ICF taxonomy components: The SMI domain relates to the health-condition component, everyday life to activities, and executive functions (EF) to body functions.
Fig. 1.
International Classification of Functioning, Disability and Health (ICF).
The EF are defined as higher-order mental functions required to perform complex and novel nonroutine tasks. These functions refer to a wide range of skills, including initiation, inhibition, working memory, and cognitive flexibility (Connor and Maeir, 2011; Toglia and Katz, 2018). Loewenstein and Acevedo (2010) stated that understanding the EFs of people with SMI through functional assessment of everyday life is an initial part of integrating information to establish treatment plans. Therefore, this review focuses on EFs and how they are measured while evaluating everyday life in the SMI population.
Previous review studies raised questions about some issues within the scope of the current review. Overdorp et al. (2016) systematically examined relationships between neuropsychological deficits and instrumental activities of daily living (IADL) for an aging population. They found both memory and EF to be associated with present IADL impairment and predictive of future decline in IADL (in 66.7% of the studies they reviewed). Cramm et al. (2013) conducted a scoping review to reveal the use of EF evaluation in occupational therapy treatment with varied populations. They referred to evaluation of EF components together with complex activities and stated that EF evaluation should be established as a dynamic analysis of performance in real-life contexts. Recently, Josman and Meyer (2019) conducted a scoping review to describe occupational therapy evaluation of EF within pediatric and youth populations. They highlighted the importance of choosing precise assessment tools to define intervention goals for each individual. In our review, we analyzed assessment tools according to Harvey et al.'s (2007) classification, which address the usefulness of performance-based measurements in clinical treatment of schizophrenia by five assessment types.
In this systematic review, we aim to capture characteristics of both everyday life and EF evaluation processes for people with SMI in international research across professions. We do this by reviewing articles that address the evaluation of both. Specifically, we examine: (a) EF components reflected in the evaluation of everyday life for clients with SMI; (b) primary everyday-life tasks that are examined as part of the evaluation process of clients with SMI; (c) assessment tools used for EF and everyday life; and (d) how EF and everyday life performance are used and examined in the evaluation process.
2. Material and methods
2.1. Search strategy
The protocol and results reporting in this review are based on PRISMA recommendations for systematic reviews (Moher et al., 2009). The review protocol is registered with PROSPERO (CRD42018105538). Relevant searches were conducted in the following electronic bibliographic databases: PubMed, CINAHL, Cochrane Library, Web of Science, PsycINFO, EDS (EBSCO Discovery Service), OTDBASE, Scopus, and ProQuest for Dissertations and Theses. MeSH terms are used for PubMed, CINAHL, Cochrane Library, and PsycINFO (full search terms are available at https://www.crd.york.ac.uk/PROSPEROFILES/105538_STRATEGY_20180817.pdf). The search was last updated in February 2020 and authors contacted regarding possible duplication (e.g., thesis and article by the same author).
The search strategy terms related to population (SMI), functional domain (everyday life), and cognitive features (EF). Quantitative research articles were included. These studies examined cognitive and metacognitive evaluation that address EF as well as everyday life. Qualitative studies and non-English-language articles were excluded. Studies set in community and hospital environments were included.
We entered the results obtained from the search into the Covidence software program (Babineau, 2014). Two independent reviewers reviewed the articles by first scanning titles and abstracts and then assessing full-text copies of relevant articles. Disagreements between the reviewers about particular studies were resolved by discussion and involvement of a third review author when necessary.
2.2. Study eligibility
Eligibility criteria were specified using the population-intervention-comparison-outcomes approach. Population included adults with SMI, defined as schizophrenia and schizoaffective, major depressive, or bipolar disorders. People with other mental diagnoses, such as Alzheimer's disease or anxiety, and minors (under 18 years old) were excluded. Because the focus of this review is on evaluating assessment tools for both EF and everyday life, interventions were included only for their baseline evaluation, although treatment that did not include specific attention to daily functioning was excluded. The comparison component included the population of people not diagnosed with SMI or evaluations not focused on everyday life. Outcome covered the evaluation process; that is, assessments that measured everyday life and EF were selected and addressed according to Harvey et al.'s (2007) five categories: global rating scales, self-report instruments, direct observation of behavior, informant reports, and performance-based measures of functional skills.
2.3. Data extraction
Two reviewers analyzed the following data to assess study quality and for evidence synthesis: authors, author disciplines, keywords, publication year, purpose (e.g., assessment, intervention), literature source (e.g., journal article, book chapter), population description, research setting and location, assessment tool, and key findings relating to EF and everyday life.
2.4. Quality assessment
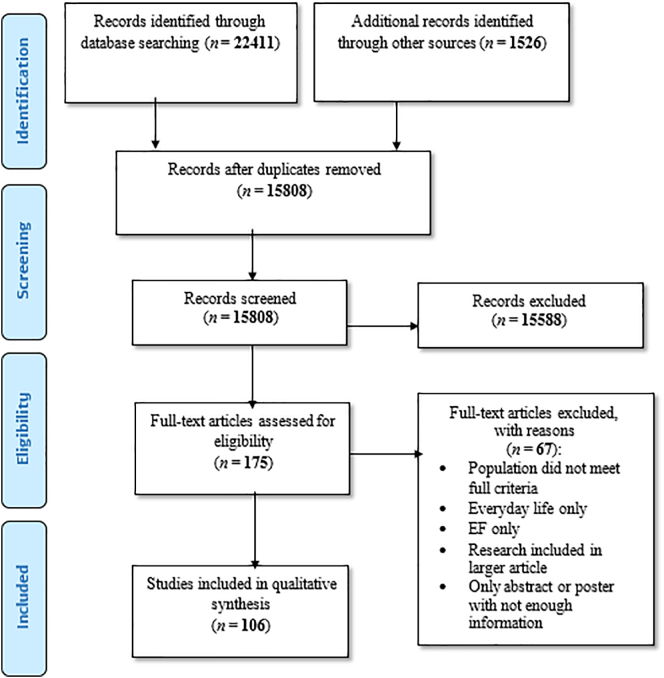
Because this systematic review addressed the evaluation process, we based the quality assessment of bias risk on Hayden and Co's (2006) recommendations but modified according to our research questions. Those questions examined the domains of study participation, domain measured, and confounders for studies with two groups. The process of describing the risk of bias with these domains enabled us to label the evaluation process accurately (Fig. 2).
Fig. 2.
PRISMA flow diagram for studies included in the systematic review.
3. Results
3.1. Selected studies
A total of 15,808 articles were identified from the literature search once duplicates were removed. Two reviewers independently screened titles and abstracts and excluded articles that met the exclusion criteria as defined above, mainly because they used pharmacological interventions. Further exclusions were made for articles that addressed adolescent and child populations or focused on neurologic disorders such as dementia and Alzheimer's disease. The remaining 175 full-text articles were then reviewed for eligibility. Of them, 106 studies were confirmed as eligible for inclusion in this study (see Appendix A for full bibliography of included studies).
3.2. Study characteristics
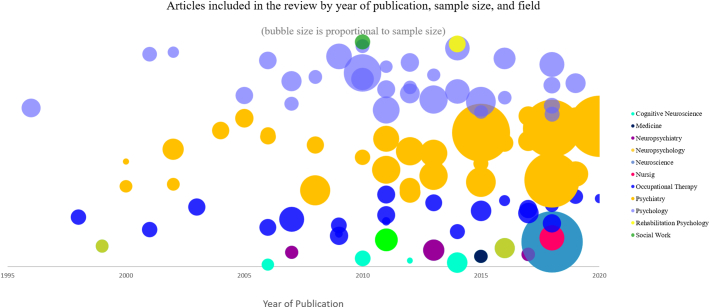
Among the eligible articles, study designs included 14 randomized control trials, two nonrandomized trials, one case report; and 20 case-control, 23 cross-sectional, and 46 descriptive studies. Fifty-one studies were conducted in the United States, 21 in Europe, 10 in Canada, nine in Israel, nine in East Asia, four in Australia, and two in South America. Subjects were inpatients in 17 studies and both in- and outpatients in 12 studies. The majority (78) of studies were conducted on outpatient subjects. Most (55) addressed schizophrenia diagnoses; 31 added a schizoaffective diagnosis to schizophrenia. Thirteen articles examined affective diagnoses, and seven defined the population in general or as SMI. Studies ranged from sample sizes of nine to 921 (an Italian cross-sectional study conducted as part of the Italian Network for Research on Psychoses). Notably, other studies cited or reported on the same projects. For example, nine studies reported the U.S. National Institutes of Health-supported Validation of Everyday Real-Life Outcomes Project. All but one study (Bowie et al., 2012) included male and female participants. Fig. 3 depicts the different research fields among the studies and their sample sizes on a chronological timeline.
Fig. 3.
Articles reviewed by year, sample size, and field.
3.3. Study quality
We evaluated risk of bias according to Hayden and Co's (2006) recommendations concerning participants, measurements, and confounders. For study participation, most studies declared their population and sample clearly. For factor measurement, we defined the strength of assessments according their scope. Specifically, we rated an instrument's representation of a domain as 1 if it fully addressed the domain and 0.5 if the domain was only part of the outcome measure (see next section). For EF, we addressed assessment as a range measuring EF as a global score as opposed to EF-specific components, such as working memory, categorization, problem-solving, impulsivity, or planning. Thirty-seven studies measured EF with a global score (e.g., the MATRICS Consensus Cognitive Battery), and 69 reported specific EF-component scores (e.g., working memory). We considered instruments to be everyday life assessments if they were defined as measuring a specific activity, such as meal preparation, shopping, or driving. We found that 78 studies addressed everyday life as a separate component, whereas the rest measured it as part of a larger topic (e.g., everyday behavior, which included work status; Bowie et al., 2012). In sum, 55 studies examined both EF and everyday life in full scope. For confounders, 33 studies had a control group, and all reported and controlled the appropriate confounders.
3.4. Everyday life assessments
Table 1 lists the 64 assessment tools used to measure everyday life in the reviewed studies, sorted according to Harvey et al.'s (2007) five categories: 26 performance-based measures of everyday life (10 of which incorporated an EF index in the test), 18 self-report instruments, 11 informant reports, five direct observations of behavior, and four global rating scales. There were no dominant or typical instruments used in the studies. The most-frequently used instrument (41 studies) was the University of California San Diego Performance-Based Skills Assessment (UPSA) and its brief version, followed by the Global Assessment of Functioning in 12 studies. The remaining instruments were scattered within studies, with each tool used one to eight times. Some studies used multiple assessment tools to measure the same activity in different ways. For example, Rempfer and Fowler (2018) examined performance skills under both simulated and naturalistic conditions with the UPSA, Knowledge of Grocery Shopping Skills Test, and Test of Grocery Shopping Skills. Other studies used everyday life assessments to understand the subject's global functioning in the community, usually by the subject or an informant completing a questionnaire (e.g., the Independent Living Skill Survey). Ten performance-based instruments scored EF performance as part of a test's index.
Table 1.
Everyday life assessment tools.
| # | Assessment tool (# articles using tool) | Example article using the tool | Everyday life activity measured by assessment |
|---|---|---|---|
| Direct observation of behavior | |||
| 1 | ADL script and task (1) | Godbout et al., 2007 | Going to restaurant\doctor\hairdresser\wedding\cinema; shopping for groceries |
| 2 | Apparel purchase decision task (1) | Kim et al., 2019 | Clothing shopping |
| 3 | Food preparation task (1) | Knight, 2000 | Two food preparation activities: one simple (tuna sandwich); one complex (macaroni and cheese) |
| 4 | Kitchen behavioral video task with researcher-built script (1) | Semkovska et al., 2002 | Cooking a meal |
| 5 | Three ADL tasks (1) | Semkovska et al., 2004 | Choosing a menu, shopping for ingredients, cooking a meal |
| Global rating scales | |||
| 6 | Global Assessment of Functioning (12) | Holt et al., 2011 | Global functioning |
| 7 | Health of the Nation Scale (1) | Roberts, 2004 | Global functioning |
| 8 | Reintegration to Normal Living Index (1) | Katz and Keren, 2011 | Global functioning |
| 9 | Social and Occupational Functioning Scale (1) | Velligan et al., 2016 | Global functioning |
| Informant | |||
| 10 | Basic Everyday Living Skills (1) | Power et al., 2013 | Basic living skills |
| 11 | Direct Assessment of Functional Status, revised (1) | Vizzotto et al., 2016 | Skills for time orientation, communication, dealing with finances, shopping, grooming, eating |
| 12 | Disability Assessment Schedule (1) | Ojeda et al., 2012 | Self-care management, social competence, vocational outcome, family contact |
| 13 | Independent Living Skill Survey, informant version (3) | Harvey et al., 2013 | Completing everyday tasks within the last 30 days |
| 14 | Multnomah Community Abilities Scale (3) | Tan and King, 2013 | Health, adaptation, social skills, behavior |
| 15 | Personal and Social Performance Scale (2) | Inchausti et al., 2018 | Self-care, activities, relationships, behavior |
| 16 | Rehabilitation Evaluation Hall and Baker (1) | Takahashi et al., 2005 | General behavior |
| 17 | Social Autonomy Scale (1) | Bulzacka et al., 2016 | Personal hygiene, everyday life management, resource management, outside functioning, affective life/social interaction |
| 18 | Specific Levels of Functioning (14) | Bowie et al., 2008 | Community activities, interpersonal skills, work skills |
| 19 | Strauss-Carpenter Levels of Functioning Scale (1) | Dickinson and Coursey, 2002 | Hospitalization frequency, social contacts, employment and productive activities, symptomatology |
| 20 | Routine Assessment of Patient Progress (1) | Thornton et al., 2010 | Daily functioning: socialization skills, leisure activities, budgeting skills, and social problem-solving |
| Performance-based | |||
| 21 | Executive Functions Performance Testa (3) | Katz and Keren, 2011 | Simple cooking, telephone use, medication management, bill payment |
| 22 | Assessment of Motor and Process Skillsa (1) | Träger et al., 2017 | Personal ADL (PADL) and IADL |
| 23 | Cognitive Screening for Medication Self-Managementa (1) | Johnson, 1998 | Medication self-management |
| 24 | Computerized Shopping Task (2) | Laloyaux et al., 2013 | Shopping task |
| 25 | Driving simulator (1) | Miyata et al., 2018 | Driving |
| 26 | Everyday Functioning Battery (1) | Harvey et al., 2011 | Financial management |
| 27 | Familiarity with Meal Preparation Task questionnaire (2) | Aubin et al., 2014 | Meal preparation |
| 28 | Independent Living Scales (3) | Tan and King, 2013 | Memory/orientation, managing money, managing home and transportation, health and safety, social adjustment |
| 29 | Jentig50 Driving Simulator (1) | Fuermaier et al., 2019 | Driving |
| 30 | Kitchen Task Assessmenta (3) | Lipskaya-Velikovsky et al., 2015 | Cooking task |
| 31 | Knowledge of Grocery Shopping Skills Test (1) | Rempfer and Fowler, 2018 | Grocery shopping |
| 32 | Medication Management Ability Assessment (2) | Kurtz et al., 2007 | Medication management |
| 33 | Multiple Errands Testa (1) | Bulzacka et al., 2016 | Unpredictable situations and interpersonal interactions |
| 34 | Naturalistic Action Test (4) | Iampietro et al., 2012 | (a) Preparing a slice of toast and a cup of coffee (b) wrapping a gift while (c) packing a lunchbox, and packing a schoolbag |
| 35 | Observed Tasks of Daily Living, revised (3) | Lipskaya-Velikovsky et al., 2017 | Taking medications, using the telephone, managing finances |
| 36 | Perceive, Recall, Plan, and Perform system of task analysisa (3) | Aubin et al., 2014 | Meal preparation |
| 37 | Performance Assessment of Self-Care Skills (1) | Gildengers et al., 2013 | Money management: shopping, bill paying by check, checkbook balancing; medication management; current events: obtaining critical information from auditory and visual media; home maintenance: small repairs; environmental awareness: home safety; meal preparation: stovetop and sharp utensil use |
| 38 | Plan-a-Daya (1) | Holt et al., 2011 | Day planning scenarios in a work setting |
| 39 | Test of Everyday Attentiona (1) | O'Shea et al., 2010 | Map search, elevator counting, visual elevator, telephone search, lottery |
| 40 | Test of Grocery Shopping Skills (6) | Zayat et al., 2011 | Grocery shopping |
| 41 | UCSD Performance-Based Skills Assessment (20) | Holshausen et al., 2014 | Planning, finance, communication, transportation, household skills |
| 42 | UCSD Performance-Based Skills Assessment, brief version (21) | Durand et al., 2015 | Communication and finances |
| 43 | Virtual Action Planning-Supermarketa (2) | Josman et al., 2009 | Shopping task |
| 44 | Virtual Reality Apartment Medication Management Assessment (1) | Kurtz et al., 2007 | Medication management |
| 45 | Virtual Reality Functional Capacity Assessment Test (2) | Harvey et al., 2019 | Meal preparation, travel and transit, shopping, financial skills |
| 46 | Weekly Calendar Planning Assessmenta (1) | Kaizerman-Dinerman et al., 2018 | Scheduling meetings |
| Self-report instruments | |||
| 47 | Activity Card Sort (2) | Katz and Keren, 2011 | Percentage of activities an individual retained |
| 48 | Canadian occupational performance measure (1) | Kaizerman-Dinerman et al., 2018 | Self-care, productivity, leisure |
| 49 | Daily Activity Report (1) | Velligan et al., 2016 | Daily report of activities |
| 50 | Executive Personal Finance Scale (1) | Cheema et al., 2015 | Financial management |
| 51 | Functioning Assessment Short Test (2) | Jiménez-López et al., 2018 | Autonomy, occupational functioning, cognitive functioning, financial issues, interpersonal relationships, leisure time. |
| 52 | Independent Living Skill Survey, self-report (8) | Bryce et al., 2018 | Completion of everyday tasks within the last 30 days |
| 53 | Independent Living Skills Inventory (2) | Keefe et al., 2006 | Personal management, hygiene and grooming, clothing, basic skills (e.g., personal phone number), interpersonal skills, home maintenance, money management, cooking, resource utilization, general occupational skills, medication management |
| 54 | IADL questionnaire (1) | Hadas-Lidor et al., 2001 | IADL |
| 55 | Life Skills Profile (2) | Keller and Hayes, 1998 | Communication, nonturbulence, responsibility, self-care, social contact (six items; e.g., abuse of alcohol and drugs, taking offense readily, violence toward others) |
| 56 | Routine Task Inventory (2) | Katz and Keren, 2011 | Basic ADL, IADL, communication, work readiness |
| 57 | Schizophrenia Objective Functioning Instrument (1) | Velligan et al., 2016 | Living situation, instrumental skills, productivity, social functioning |
| 58 | Social Adjustment Scale-II (1) | Eack et al., 2010 | Work affinity, primary/family relations in household, social functioning outside the home, interpersonal anguish, sexual relations, social leisure, self-care |
| 59 | Major Role Adjustment Inventory (1) | Eack et al., 2010 | Vocational, social, household role functioning |
| 60 | Quality of Life Scale (1) | Gould et al., 2013 | Vocational, social, everyday living skills |
| 61 | Social Functioning Scale (2) | Dickerson et al., 1996 | Activation-engagement, interpersonal communication, ADL frequency; recreational and social activities, ADL competence, employment-occupational activity |
| 62 | Time Use Survey (1) | Reeder et al., 2017 | Hours per week over the past month spent in employment, education, voluntary work, voluntary and structured leisure activities, housework and chores, childcare, sports and hobbies |
| 63 | Instrumental Activities of Daily Living (1) | Kim et al., 2020 | Shopping, transportation, ability to handle finances, housekeeping, preparing food, ability to use a telephone, responsibility for own medication, recent memory, hobbies, watching television, and fixing things around the house |
| 64 | Satisfaction With Daily Occupations measure (1) | Holmefur et al., 2019 | Domestic tasks and self-care occupations |
Groupings: Global rating scale = rating tools scored by clinicians about the global function of the subject; self-report instruments = questionnaires, interviews, daily records, etc.; informant = caregiver, family member, personal therapist who rates the subject's routine and behavior in daily life; performance-based measures of functional skills = subject's capacity is measured while performing a standardized task; direct observation of behavior = subject performs a daily task and observer analyzes it.
See full reference list in Appendix A.
Performance-based tools that examine both everyday life and EF; ADL = activities of daily living; IADL = instrumental ADL.
3.5. EF and component assessments
Table 2 identifies the 30 assessment tools that measured EF in the review studies. The table lists EF assessment tools and what each measured according to how it was presented in the study. In cases where the article did not provide explanation, we obtained the specific EF from the assessment tool's manual. Together, the tools assessed 19 features that covered a vast range of EF, including the key components of initiation, inhibition, working memory, and cognitive flexibility. Within the types of assessment tools, 23 were tabletop (i.e., a task carried out in a controlled environment), four were performance-based (i.e., involved performing the task in a naturalistic environment), and three were self-report questionnaires. Some tools, such as the Wisconsin Card Sorting Test, were applied as stand-alone tools to examine global EF components, whereas others, such as the Neurobehavioral Cognitive Status Examination, measured separate EF components within its subtests. Still other tests, such as the Behavioral Assessment of the Dysexecutive Syndrome, were included as a single type in one study and subsequently as subtests (e.g., the key search subtest) in another study.
Table 2.
Executive function (EF) assessment tools classification.
| # | EF assessment tool (# articles using tool) | EF measured according to article or manual |
|---|---|---|
| Performance-based | ||
| 1 | Behavioral Assessment of the Dysexecutive Syndrome, key search task, zoo mapa (12) | Organization, planning |
| 2 | Kitchen Task Assessment (3) | Initiation, organization, sequencing, judgment |
| 3 | Months Ordering Test of Working Memory (1) | Organization |
| 4 | Perceive, Recall, Plan, and Perform task analysis system (3) | Working memory, plan |
| Tabletop | ||
| 5 | Stocking of Cambridge (1) | Plan, strategy |
| 6 | Allen Cognitive Level Test (2) | Cognitive level |
| 7 | Assessment of Time Management Skills (1) | Time management skills, organization and planning, and regulation of emotion |
| 8 | Brief Assessment of Cognition in SCZa (6) | Reasoning, problem-solving, working memory |
| 9 | Brief Cognitive Assessmenta (1) | Executive functioning |
| 10 | Cambridge Neuropsychological Test Automated Batterya (4) | Working memory, plan |
| 11 | Delis–Kaplan Executive Function System (4) | Executive functioning |
| 12 | Hayling Sentence Completion Test (2) | Inhibition |
| 13 | Letter Number Sequencing test (1) | Working memory |
| 14 | MATRICS Consensus Cognitive Battery (includes EF subtests: BACS, Category Fluency, Trail Making Test Part A, CPT-IP Working Memory, WMS-III, Mazes)a (23) | Problem-solving, working memory |
| 15 | Neurobehavioral Cognitive Status Examination (3) | Orientation, naming, judgment, comprehension |
| 16 | Penn Conditional Exclusion Test (1) | Problem-solving |
| 17 | Phonological fluency tests (6) | Initiation, inhibition |
| 18 | Porteus Mazes Test (2) | Plan |
| 19 | Rey Osterreith Complex Figure Test (6) | Organization, plan, working memory |
| 20 | Screen for Cognitive Impairment in Psychiatrya (1) | Working memory |
| 21 | Short Category Test (1) | Problem-solving |
| 22 | Stroop Interference Task (7) | Cognitive flexibility |
| 23 | Tower of London (5) | Executive functioning, plan, working memory, problem-solving |
| 24 | Trail Making Test (30) | Executive functioning |
| 25 | Wechsler Adult Intelligence Scale, various versions and parts (37) | Working memory |
| 26 | Wisconsin Card Sorting Test (28) | Reasoning, problem-solving, executive functioning |
| 27 | Working Memory N-Back Test (2) | Working memory |
| Self-report questionnaire | ||
| 28 | Behavior Rating Inventory of Executive Function, adult versionb (2) | Inhibition, shift, emotional control, self-monitor, initiation, working memory, plan/organize, task monitor, organize materials |
| 29 | Barratt Impulsiveness Scale (1) | Inhibition |
| 30 | Metacognitive Assessment Scale (2) | Metacognition |
Battery.
Self-report and informant classifications.
3.6. Everyday life and EF assessments
Descriptions of the indices evaluated were not always consistent between the studies and the manuals for everyday life and EF assessment tools. In compiling both Table 1, Table 2, we included the assessment purpose as the manual described in cases where the purpose was either unclear in or conflicted with the article's stated purpose. The aim of most studies was broader than merely the relationships between EF and everyday life. Instead, they sought to understand quality-of-life measures, social participation, cognition, illness status, and so forth. Hence, the studies' outcomes were low or moderate in terms of our research question or they reached conclusions based on other hypotheses. For example, Knight and Baune (2018) found that EF and spatial cognition mediated issues in leisure time and reached a conclusion from this effect about psychosocial function.
4. Discussion
In this systematic review, we searched for information about both EF and everyday assessment tools that can help therapists choose the best tool in each person's varied life situations, in the scope of everyday life tasks. The focus on everyday life, especially for the SMI population, is crucial because there is a hidden gap between individuals' intelligence and knowledge and their actual performance. Understanding that EF are interrupted and no longer manage the unexpected or novel situations—and being able to identify the exact missing or less efficient function—may be the beginning of the work to establish meaningful and efficient strategies that will compensate toward full function. In the evaluation process, the clinician must conduct a clinical reasoning and decide which assessment tools would best capture the nature of the client's needs to reach the therapeutic goals. This process should be combined with evidence-based knowledge and professional experience.
For the SMI population, in which the range of difficulties is wide and reasons for dysfunction in routine are varied, it is essential to use the most compatible assessment tool to gather the information. For example, a self-report questionnaire about daily participation might lack information because of the patient's low self-esteem. The same tool and questions, answered together with a family member or therapist, could brighten the picture and lead the therapist to detect meaningful and reasonable goals.
As presented in Table 1, Table 2, many assessment tools currently are available for both EF and everyday life outcomes. They have progressed from measuring specific components, such as memory, to more comprehensive assessments that often use a test battery to comprehend functional cognition from several elements. Moreover, performance-based tools, which enable measuring everyday life in specific tasks, more likely include an EF index as part of the scoring. For example, the Virtual Action Planning-Supermarket (Josman et al., 2009) was developed to evaluate shopping skills, as well as the use of EF (Josman and Regev, 2018). Such tools hold many advantages. First, their ecological validity is high due to their naturalistic or close-to-real-world environments. Second, EF are more evident when they are impaired (Connor and Maeir, 2011) and, therefore, task performance is an effective method to observe the dysfunction. Assessment tools similar to the Test of Grocery Shopping Skills have the potential to measure EF (Zayat et al., 2011) but do not have standardized and specific scoring. It would be efficient to upgrade these assessment tools for use as both everyday life and as EF measurements.
Screening the assessments with understanding of SMI properties, it became noticeable that most researchers either chose short versions of the tools or shortened the tools to address the subjects' attentional capacities, as well as a combination of the tools. Using more than one evaluation method to provide related information (Rogers and Holm, 2016), such as a self-report and an informant questionnaire, enabled them to draw a more precise picture of the function—the combination considers both the objective presentation and the individual's subjective perception and self-efficacy.
In addition to evaluation methods, outcome measures have changed. In the past, independence was a main index; sometimes, safe behavior was measured. Now, indexes also can include difficulty, competency, importance, and patient satisfaction (Rogers and Holm, 2016). Performance-based assessments usually serve as everyday life assessments, although tool developers or later researchers often add an EF index as part of scoring some tests. The ability of these assessments to capture the naturalistic nature of functional EF use is strong. They can reveal the most about performance in real life and provide insight into the impact of EF on everyday-life task performance.
This study's categorization, evaluation, and presentation of current assessment tools has implications for both clinicians and researchers. Specifically, it assists them to choose the assessment tools that are most appropriate for their clients and study participants using evidence-based decisions about the lists provide in this study. They may search and compare instruments according to the categories and components each assessment tool explores. For example, for a meal preparation task in a performance-based method, the most studied assessment was the Perceive, Recall, Plan, and Perform system of task analysis.
4.1. Limitations and future research
The ambiguous concepts and varied research types noted within this review limited our ability to group and reach conclusions from the extant relevant literature. However, we organized the data in a way that would be efficient for use in the evaluation process. Future studies might evaluate the accuracy of our findings by focusing the search strategy on a specific EF or everyday life task such as meal preparation. Nevertheless, the indefinite, as well as broader, search terms reached sources from multiple disciplines, enabling understanding of the phenomenon and enrichment of multi-disciplinary discussions on these issues.
4.2. Conclusion
In summary, this review contributes to the existing evidence-based knowledge regarding the evaluation process of EF and everyday life. For both domains, it identifies and organizes the assessment tools presently used in SMI research. Tracking assessment tool development over the last decades and classifying them by method will enable clinicians and researchers to make well-established decisions regarding which method and assessment tool best suits their interventions or answers their research questions. Future studies might use this information to expand interventions about these topics.
Contributors
SR wrote the manuscript as part of her doctoral research. She did the literature review and read the journal articles and selected the relevant articles for the review manuscript. Then, reviewed the articles together with HC, a research assistant. Co-author NJ supervised and edited during the whole process. All authors contributed to and have approved the final manuscript.
Role of funding source
No official funding was provided to conduct this meta-analysis.
Declaration of competing interest
The authors have no conflicts of interest to report.
Acknowledgement
This article is part of the first author's fulfilments toward the PhD degree.
Contributor Information
Sivan Regev, Email: sivreg@gmail.com.
Naomi Josman, Email: njosman@univ.haifa.ac.il.
Appendix A. Bibliography of the 106 articles in the analysis
Allen, D.N., Bello, D.T., Thaler, N.S., 2015. Neurocognitive predictors of performance-based functional capacity in bipolar disorder. J. Neuropsychol. 9, 159–171. doi:10.1111/jnp.12042.
Aubin, G., Chapparo, C., Gélinas, I., Stip, E., Rainville, C., 2009. Use of the perceive, recall, plan and perform system of task analysis for persons with schizophrenia: a preliminary study. Aust. Occup. Ther. J. 56, 189–199. doi:10.1111/j.1440-1630.2007.00725.x.
Aubin, G., Lamoureux, J., Gélinas, I., Chapparo, C., Stip, E., Rainville, C., 2014. Daily task performance and information processing among people with schizophrenia and healthy controls: a comparative study. Br. J. Occup. Ther. 77, 466–474. doi:10.4276/030802214X14098207541117.
Aubin, G., Stip, E., Gélinas, I., Rainville, C., Chapparo, C., 2009. Daily functioning and information-processing skills among persons with schizophrenia. Psychiatr. Services. 60, 817–822. doi:10.1176/ps.2009.60.6.817.
Bowie, C.R., Leung, W.W., Reichenberg, A., McClure, M.M., Patterson, T.L., Heaton, R.K., Harvey, P.D., 2008. Predicting schizophrenia patients' real-world behavior with specific neuropsychological and functional capacity measures. Biol. Psychiatry. 63, 505–511. doi:10.1016/j.biopsych.2007.05.022.
Bowie, C.R., McGurk, S.R., Mausbach, B., Patterson, T.L., Harvey, P.D., 2012. Combined cognitive remediation and functional skills training for schizophrenia: effects on cognition, functional competence, and real-world behavior. Am. J. Psychiatry. 169, 710–718. doi:10.1176/appi.ajp.2012.11091337.
Brissos, S., Palhava, F., Marques, J.G., Mexia, S., Carmo, A.L., Carvalho, M., Dias, C., Franco, J.D., Mendes, R., Zuzarte, P., Carita, A.I., Molodynski, A., Figueira, M.L., 2012. The Portuguese version of the Personal and Social Performance Scale (PSP): reliability, validity, and relationship with cognitive measures in hospitalized and community schizophrenia patients. Soc. Psychiatry Psychiatr. Epidemiol. 47, 1077–1086. doi:10.1007/s00127-011-0412-6.
Bryce, S.D., Rossell, S.L., Lee, S.J., Lawrence, R.J., Tan, E.J., Carruthers, S.P., Ponsford, J.L., 2018. Neurocognitive and self-efficacy benefits of cognitive remediation in schizophrenia: a randomized controlled trial. J. Int. Neuropsychol. Soc. 24, 549–562. doi:10.1017/s1355617717001369.
Bulzacka, E., Delourme, G., Hutin, V., Burban, N., Méary, A., Lajnef, M., Leboyer, M., Schürhoff, F., 2016. Clinical utility of the Multiple Errands Test in schizophrenia: a preliminary assessment. Psychiatry Res. 240, 390–397. doi:10.1016/j.psychres.2016.04.056.
Cheema, M.K., MacQueen, G.M., Hassel, S., 2015. Assessing personal financial management in patients with bipolar disorder and its relation to impulsivity and response inhibition. Cogn. Neuropsychiatry. 20, 424–437. doi:10.1080/13546805.2015.1076722.
Couture, S.M., Granholm, E.L., Fish, S.C., 2011. A path model investigation of neurocognition, theory of mind, social competence, negative symptoms and real-world functioning in schizophrenia. Schizophr. Res. 125, 152–160. doi:10.1016/j.schres.2010.09.020.
Czaja, S.J., Loewenstein, D.A., Lee, C.C., Fu, S.H., Harvey, P.D., 2017. Assessing functional performance using computer-based simulations of everyday activities. Schizophr. Res. 183, 130–136. doi:10.1016/j.schres.2016.11.014.
Dickerson, F.B., Ringel, N., Parente, F., Boronow, J.J., 1996. Neurocognitive deficits and social functioning in outpatients with schizophrenia: a two-year follow-up. Schizophr. Res. 29, 56. doi:10.1016/0920-9964(96)00040-0.
Dickinson, D., Coursey, R.D., 2002. Independence and overlap among neurocognitive correlates of community functioning in schizophrenia. Schizophr. Res. 56, 161–170. doi:10.1016/S0920-9964(01)00229-8.
Durand, D., Strassnig, M., Sabbag, S., Gould, F., Twamley, E.W., Patterson, T.L., Harvey, P.D., 2015. Factors influencing self-assessment of cognition and functioning in schizophrenia: implications for treatment studies. Eur. Neuropsychopharmacol. 25, 185–191. doi:10.1016/j.euroneuro.2014.07.008.
Eack, S.M., Greenwald, D.P., Hogarty, S.S., Keshavan, M.S., 2010. One-year durability of the effects of cognitive enhancement therapy on functional outcome in early schizophrenia. Schizophr. Res. 120, 210–216. doi:10.1016/j.schres.2010.03.042.
Elliott, C.S., Fiszdon, J.M., 2014. Comparison of self-report and performance-based measures of everyday functioning in individuals with schizophrenia: implications for measure selection. Cogn. Neuropsychiatry. 19, 485–494. doi:10.1080/13546805.2014.922062.
Fuermaier, A.B.M., Piersma, D., Huntjens, R.J.C., de Waard, D., Westermann, C., Bossert, M., Lange, K.W., Weisebrod, M., Bruggeman, R., Aschenbrenner, S., Tucha, O., 2019. Simulated car driving and its association with cognitive abilities in patients with schizophrenia. Schizophr. Res. 204, 171–177. doi:10.1016/j.schres.2018.09.005.
Galderisi, S., Rucci, P., Kirkpatrick, B., Mucci, A., Gibertoni, D., Rocca, P., Rossi, A., Bertolino, A., Strauss, G.P., Aguglia, E., Bellomo, A., Belvederi Murri, M. Bucci, P., Carpiniello, B., Comparelli, A., Cuomo, A., De Berardis, D., Dell'Osso, L., Di Fabio, F., Gelao, B., Marchesi, C. Monteleone, P., Montemagni, C. Orsenigo, G., Pacitti, F., Roncone, R., Santonastaso, P., Siracusano, A., Vignapiano, A., Vita, A., Zeppegno, P., Maj, M., 2018. Interplay among psychopathologic variables, personal resources, context-related factors, and real-life functioning in individuals with schizophrenia: a network analysis. JAMA Psychiatry. 75, 396–404. doi:10.1001/jamapsychiatry.2017.4607.
Galderisi, S., Rucci, P., Mucci, A., Rossi, A., Rocca, P., Bertolino, A., Aguglia, E., Amore, M., Bellomo, A., Bozzatello, P., Bucci, P., Carpiniello, B., Collantoni, E., Cuomo, A., Dell'Osso, L., Di Fabio, F., di Giannantonio, M., Gibertoni, D., Giordano, G. M., Marchesi, C., Monteleone, P., Oldani, L., Pompili, M., Ronconi, R., Rossi, R., Siracusano, A., Vita, A., Zappegno, P., Maj, M., Italian Network for Research on Psychoses, 2020. The interplay among psychopathology, personal resources, context-related factors and real-life functioning in schizophrenia: stability in relationships after 4 years and differences in network structure between recovered and non-recovered patients. World Psychiatry, 19, 81–91. doi:10.1002/wps.20700.
Gildengers, A.G., Chisholm, D., Butters, M.A., Anderson, S.J., Begley, A., Holm, M., Rogers, J.C., Reynolds, C.F., Mulsant, B.H., 2013. Two-year course of cognitive function and instrumental activities of daily living in older adults with bipolar disorder: evidence for neuroprogression? Psychol. Med., 43, 801–811. doi:10.1017/S0033291712001614.
Godbout, L., Limoges, F., Allard, I., Braun, C.M.J., Stip, E., 2007. Neuropsychological and activity of daily living script performance in patients with positive or negative schizophrenia. Compr. Psychiatry. 48, 293–302. doi:10.1016/j.comppsych.2007.01.003.
Gould, F., McGuire, L.S., Durand, D., Sabbag, S., Larrauri, C., Patterson, T.L., Twamley, E.L., Harvey, P.D., 2015. Self-assessment in schizophrenia: accuracy of evaluation of cognition and everyday functioning. Neuropsychol. 29, 675–682. doi:10.1037/neu0000175.
Gould, F., Sabbag, S., Durand, D., Patterson, T.L., & Harvey, P.D., 2013. Self-assessment of functional ability in schizophrenia: milestone achievement and its relationship to accuracy of self-evaluation. Psychiatry Res. 207, 19–24. doi:10.1016/j.psychres.2013.02.035.
Green, M.F., Schooler, N.R., Kern, R.S., Frese, F.J., Granberry, W., Harvey, P.D., Karson, C.N., Peters, N., Stewart, M., Seidman, L.J., Sonnenberg, J., Stone, W.S., Walling, D., Stover, E., Marder, S.R., 2011. Evaluation of functionally meaningful measures for clinical trials of cognition enhancement in schizophrenia. Am. J. Psychiatry. 4, 400–407. doi:10.1176/appi.ajp.2010.10030414.
Greenwood, K.E., Landau, S., Wykes, T., 2005. Negative symptoms and specific cognitive impairments as combined targets for improved functional outcome within cognitive remediation therapy. Schizophr. Bull. 31, 910–921. doi:10.1093/schbul/sbi035.
Greenwood, K E., Morris, R., Smith, V., Jones, A.M., Pearman, D., Wykes, T., 2016. Virtual shopping: a viable alternative to direct assessment of real life function? Schizophr. Res. 172, 206–210. doi:10.1016/j.schres.2016.02.029.
Gupta, M., Bassett, E., Iftene, F., Bowie, C.R., 2012. Functional outcomes in schizophrenia: Understanding the competence-performance discrepancy. J. Psychiatr. Res. 46, 205–211. doi:10.1016/j.jpsychires.2011.09.002.
Hadas-Lidor, N., Katz, N., Tyano, S., Weizmann, A., 2001. Effectiveness of dynamic cognitive intervention in rehabilitation of clients with schizophrenia. Clin. Rehabil. 15, 349–359. doi:10.1191/026921501678310153.
Harvey, P.D., Khan, A., Atkins, A., Keefe, R.S., 2019. Virtual reality assessment of functional capacity in people with schizophrenia: associations with reduced emotional experience and prediction of functional outcomes. Psychiatry Res. 277, 58–63. doi:10.1016/j.psychres.2019.01.045.
Harvey, P.D., Paschall, G., Depp, C., 2015. Factors influencing self-assessment of cognition and functioning in bipolar disorder: a preliminary study. Cogn. Neuropsychiatry. 20, 361–371. doi:10.1080/13546805.2015.1044510.
Harvey, P.D., Raykov, T., Twamley, E.W., Vella, L., Heaton, R.K., Patterson, T.L., (2011). Validating the measurement of real-world functional outcomes: Phase I results of the VALERO study. Am. J. Psychiatry.168, 1195–1201. doi:10.1176/appi.ajp.2011.10121723.
Harvey, P.D., Stone, L., Lowenstein, D., Czaja, S.J., Heaton, R.K., Twamley, E.W., Patterson, T.L., 2013. The convergence between self-reports and observer ratings of financial skills and direct assessment of financial capabilities in patients with schizophrenia: more detail is not always better. Schizophr. Res. 147, 86–90. doi:10.1016/j.schres.2013.02.018.
Henry, B.L., Minassian, A., Perry, W., 2013. Everyday functional ability across different phases of bipolar disorder. Psychiatry Res. 210, 850–856. doi:10.1016/j.psychres.2013.04.006.
Holmefur, M., Lidström-Holmqvist, K., Roshanay, A. H., Arvidsson, P., White, S., Janeslätt, G., 2019. Pilot study of let's get organized: a group intervention for improving time management. Am. J. Occup. Ther. 73, 7305205020. doi:10.5014/ajot.2019.032631.
Holshausen, K., Bowie, C.R., Mausbach, B.T., Patterson, T.L., Harvey, P.D., 2014. Neurocognition, functional capacity, and functional outcomes: the cost of inexperience. Schizophr. Res. 152, 430–434. doi:10.1016/j.schres.2013.08.004.
Holt, D.V., Rodewald, K., Rentrop, M., Funke, J., Weisbrod, M., Kaiser, S., 2011. The plan-a-day approach to measuring planning ability in patients with schizophrenia. J. Int. Neuropsychol. Soc. 17, 327–335. doi:10.1017/s1355617710001712.
Iampietro, M., Giovannetti, T., Drabick, D.A.G., Kessler, R.K., 2012. Empirically defined patterns of executive function deficits in schizophrenia and their relation to everyday functioning: a person-centered approach. Clin. Neuropsychol. 26, 1166–1185. doi:10.1080/13854046.2012.721399.
Inchausti, F., García-Poveda, N.V, Ballesteros-Prados, A., Ortuño-Sierra, J., Sánchez-Reales, S., Prado-Abril, J., Aldaz-Armendáriz, J.A., Mole, J., Dimaggio, G., Ottavi, P., Fonesca-Pedrero, E., 2018. The effects of metacognition-oriented social skills training on psychosocial outcome in schizophrenia-spectrum disorders: A randomized controlled trial. Schizophr. Bull. 44, 1235–1244. doi:10.1093/schbul/sbx168.
Jahshan, C., Vinogradov, S., Wynn, J.K., Hellemann, G., Green, M.F., 2019. A randomized controlled trial comparing a “bottom-up” and “top-down” approach to cognitive training in schizophrenia. J. Psychiatr. Res. 109, 118–125. doi:10.1016/j.jpsychires.2018.11.027.
Jiménez-López, E., Sánchez-Morla, E.M., Aparicio, A.I., López-Villarreal, A., Martínez-Vizcaíno, V., Rodriguez-Jimenez, R., Vieta, E., Santos, J.L., 2018. Psychosocial functioning in patients with psychotic and non-psychotic bipolar I disorder. A comparative study with individuals with schizophrenia. J. Affect. Disord. 229, 177–185. doi:10.1016/j.jad.2017.12.094.
Johnson, K.E., 1998. Medication management in individuals with persistent schizophrenia (Unpublished doctoral dissertation). Drexel University, Pennsylvania.
Josman, N., Katz, N., 2006. Relationships of categorization on tests and daily tasks in patients with schizophrenia, post-stroke patients and healthy controls. Psychiatry Res. 141, 15–28. doi:10.1016/j.psychres.2004.03.015.
Josman, N., Schenirderman, A.E., Klinger, E., Shevil, E., 2009. Using virtual reality to evaluate executive functioning among persons with schizophrenia: a validity study. Schizophr. Res. 115, 270–277. doi:10.1016/j.schres.2009.09.015.
Kaizerman-Dinerman, A., Roe, D., Josman, N., 2018. An efficacy study of a metacognitive group intervention for people with schizophrenia. Psychiatry Res. 270, 1150–1156. doi:10.1016/j.psychres.2018.10.037.
Katsumi, A., Hoshino, H., Fujimoto, S., Yabe, H., Ikebuchi, E., Nakagome, K., Niwa, S.I., 2017. Effects of cognitive remediation on cognitive and social functions in individuals with schizophrenia. Neuropsychol. Rehabil. Advance online publication. doi:10.1080/09602011.2017.1409639.
Katz, N., Keren, N., 2011. Effectiveness of occupational goal intervention for clients with schizophrenia. Am. J. Occup. Ther. 65, 287–296. doi:10.5014/ajot.2011.001347.
Katz, N., Tadmor, I., Felzen, B., Hartman-Maeir, A., 2007. The Behavioural Assessment of the Dysexecutive Syndrome (BADS) in schizophrenia and its relation to functional outcomes. Neuropsychol. Rehabil. 17, 192–205. doi:10.1080/09602010600685053.
Keefe, R.S.E., Poe, M., Walker, T.M., Harvey, P.D., 2006a. The relationship of the Brief Assessment of Cognition in Schizophrenia (BACS) to functional capacity and real-world functional outcome. J. Clin. Exp. Neuropsychol. 28, 260–269. doi:10.1080/13803390500360539.
Keefe, R.S.E., Poe, M., Walker, T.M., Kang, J.W., Harvey, P.D., 2006b. The Schizophrenia Cognition Rating Scale: an interview-based assessment and its relationship to cognition, real-world functioning, and functional capacity. Am. J. Psychiatry. 163, 426–432. doi:10.1176/appi.ajp.163.3.426.
Keller, S., Hayes, R., 1998. The relationship between the Allen Cognitive Level Test and the Life Skills Profile. Am. J. Occup. Ther. 52, 851–856. https://psycnet.apa.org/doi/10.5014/ajot.52.10.851.
Kessler, R.K., Giovannetti, T., MacMullen, L.R., 2007. Everyday action in schizophrenia: Performance patterns and underlying cognitive mechanisms. Neuropsychol. 21, 439–447. doi:10.1037/0894-4105.21.4.439.
Kim, S.-J., Hong, Y.-J., Kim, M.-W., Jung, Y.-H., Min, S.-R., Kim, J.-J., 2019. Inflexible eye fixation pattern in schizophrenia affecting decision-making on daily life. Psychiatr. Res. 274, 414–420. doi:10.1016/j.psychres.2019.02.063.
Kim, Y.-S., Park, J.-H., Lee, S.-A., 2020. Is a program to improve grocery-shopping skills clinically effective in improving executive function and instrumental activities of daily living of patients with schizophrenia? Asian J. Psychiatr. 48, 101,896. doi:10.1016/j.ajp.2019.101896.
Kim, S.-J., Shim, J.-C., Kong, B.-G., Kang, J.-W., Moon, J.-J., Jeon, D.-W., Seo, Y.-S., Oh, M.-K., Jung, D.-U., 2015. Differences in cognitive function and daily living skills between early- and late-stage schizophrenia. Int. J. Psychiatry Clin. Pract. 19, 245–251. doi:10.3109/13651501.2015.1084328.
Knight, M.J., Baune, B.T., 2018. Executive function and spatial cognition mediate psychosocial dysfunction in major depressive disorder. Front. Psychiatry. 9, 3–6. doi:10.3389/fpsyt.2018.00539.
Knight, M.M., 2000. Cognitive function and food preparation ability in schizophrenia (Unpublished doctoral dissertation). University of Rhode Island. https://digitalcommons.uri.edu/dissertations/AAI9988223.
Kurtz, M.M., Baker, E., Pearlson, G.D., Astur, R.S., 2007. A virtual reality apartment as a measure of medication management skills in patients with schizophrenia: a pilot study. Schizophr. Bull. 33, 1162–1170. doi:10.1093/schbul/sbl039.
Kurtz, M.M., Jeffrey, S.B., Rose, J., 2010. Elementary neurocognitive function, learning potential and everyday life skills in schizophrenia: what is their relationship? Schizophr. Res. 116, 280–288. doi:10.1016/j.schres.2009.08.011.
Kurtz, M.M., Wexler, B.E., Fujimoto, M., Shagan, D.S., Seltzer, J.C., 2008. Symptoms versus neurocognition as predictors of change in life skills in schizophrenia after outpatient rehabilitation. Schizophr. Res. 102, 303–311. doi:10.1016/j.schres.2008.03.023.
Laloyaux, J., Pellegrini, N., Mourad, H., Bertrand, H., Domken, M.A., Van der Linden, M., Larøi, F., 2013. Performance on a computerized shopping task significantly predicts real world functioning in persons diagnosed with bipolar disorder. Psychiatry Res. 210, 465–471. doi:10.1016/j.psychres.2013.06.032.
Larøi, F., Canlaire, J., Mourad, H., Van der Linden, M., 2010. Relations between a computerized shopping task and cognitive tests in a group of persons diagnosed with schizophrenia compared with healthy controls. J. Int. Neuropsychol. Soc. 16, 180–189. doi:10.1017/s1355617709991159.
Leifker, F.R., Patterson, T.L., Bowie, C.R., Mausbach, B.T., Harvey, P.D., 2010. Psychometric properties of performance-based measurements of functional capacity: Test-retest reliability, practice effects, and potential sensitivity to change. Schizophr. Res. 119, 246–252. doi:10.1016/j.schres.2010.03.021.
Levaux, M.-N., Fonteneau, B., Larøi, F., Offerlin-Meyer, I., Danion, J.-M., Van der Linden, M., 2012. An individualized and everyday life approach to cognitive rehabilitation in schizophrenia: a case illustration. Rehabil. Res. Pract. 2012, 1–9. doi:10.1155/2012/928294.
Levaux, M.-N., Larøi, F., Malmedier, M., Offerlin-Meyer, I., Danion, J.-M., Van der Linden, M., 2012. Rehabilitation of executive functions in a real-life setting: Goal management training applied to a person with schizophrenia. Case Rep. Psychiatry. 2012, 503,023. doi:10.1155/2012/503023.
Lipskaya, L., Jarus, T., Kotler, M., 2011. Influence of cognition and symptoms of schizophrenia on IADL performance. Scand. J. Occup. Ther. 18, 180–187. doi:10.3109/11038128.2010.490879.
Lipskaya-Velikovsky, L., Jarus, T., Kotler, M., 2017. Prediction of the intensity and diversity of day-to-day activities among people with schizophrenia using parameters obtained during acute hospitalization. Disabil. Rehabil. 39, 1300–1306. doi:10.1080/09638288.2016.1194896.
Lipskaya-Velikovsky, L., Kotler, M., Easterbrook, A., Jarus, T., 2015. From hospital admission to independent living: Is prediction possible? Psychiatry Res. 226, 499–506. doi:10.1016/j.psychres.2015.01.027.
Lysaker, P.H., McCormick, B.P., Snethen, G., Buck, K.D., Hamm, J.A., Grant, M., Nicolò, G., Dimaggio, G., 2011. Metacognition and social function in schizophrenia: associations of mastery with functional skills competence. Schizophr. Res. 131, 214–218. doi:10.1016/j.schres.2011.06.011.
Mahmood, Z., Burton, C.Z., Vella, L., Twamley, E.W., 2018. Neuropsychological predictors of performance-based measures of functional capacity and social skills in individuals with severe mental illness. J. Psychiatr. Res. 102, 201–206. doi:10.1016/j.jpsychires.2018.04.011.
Martino, D.J., Igoa, A., Marengo, E., Scápola, M., Strejilevich, S.A., 2011. Neurocognitive impairments and their relationship with psychosocial functioning in euthymic bipolar II disorder. J. Nerv. Ment. Dis. 199, 459–464. doi:10.1097/NMD.0b013e3182214190.
Miyata, A., Iwamoto, K., Kawano, N., Aleksic, B., Ando, M., Ebe, K., Fujita, K., Yokoyama, M., Akiyama, T., Igarashi, Y., Ozaki, N., 2018. Driving performance of stable outpatients with depression undergoing real-world treatment. Psychiatr. Clin. Neurosci., 72, 399–408. doi:10.1111/pcn.12648.
Ojeda, N., Peña, J., Sánchez, P., Bengoetxea, E., Elizagárate, E., Ezcurra, J., Gutiérrez Fraile, M., 2012. Efficiency of cognitive rehabilitation with REHACOP in chronic treatment resistant Hispanic patients. Neurorehabil. 30, 65–74. doi:10.3233/NRE-2011-0728.
Olsson, A.-K., Hjarthag, F., & Helldin, L. (2019). Overestimated function in patients with schizophrenia: A possible risk factor for inadequate support? Schizophrenia Research, 206, 194–199. doi:10.1016/j.schres.2018.11.027.
O'Shea, R., Poz, R., Michael, A., Berrios, G.E., Evans, J.J., Rubinsztein, J.S., 2010. Ecologically valid cognitive tests and everyday functioning in euthymic bipolar disorder patients. J. Affect. Disord. 125, 336–340. doi:10.1016/j.jad.2009.12.012.
Pattanayak, R.D., Sagar, R., Mehta, M., 2012. Neuropsychological performance in euthymic Indian patients with bipolar disorder type I: Correlation between quality of life and global functioning. Psychiatry Clin. Neurosci. 66, 553–563. doi:10.1111/j.1440-1819.2012.02400.x.
Perivoliotis, D., 2006. Self-reported and performance-based functioning in middle-aged and older outpatients with schizophrenia (Doctoral dissertation). ProQuest Dissertations and Theses database (UMI No. 3212024).
Power, B.D., Dragović, M., Rock, D., 2013. Clusters according to patient need in a long-stay inpatient population with schizophrenia: Does executive dysfunction underpin needs-directed care? Soc. Psychiatry Psychiatr. Epidemiol. 48, 621–630. doi:10.1007/s00127-012-0579-5.
Pratt, S.I., Mueser, K.T., Bartels, S.J., Wolfe, R., 2013. The impact of skills training on cognitive functioning in older people with serious mental illness. Am. J. Geriatr. Psychiatry. 21, 242–250. doi:10.1016/j.jagp.2013.01.002.
Reeder, C., Huddy, V., Cella, M., Taylor, R., Greenwood, K., Landau, S., Wykes, T., 2017. A new generation computerised metacognitive cognitive remediation programme for schizophrenia (CIRCuiTS): A randomised controlled trial. Psychol. Med. 47, 2720–2730. doi:10.1017/S0033291717001234.
Rempfer, M.V., Fowler, C.A., 2018. Relationships among functional capacity, cognition, and naturalistic skill performance in people with serious mental illness. Psychiatry Res. 270, 453–458. doi:10.1016/j.psychres.2018.10.016.
Rempfer, M.V., Hamera, E.K., Brown, C.E., Cromwell, R.L., 2003. The relations between cognition and the independent living skill of shopping in people with schizophrenia. Psychiatry Res. 117, 103–112. doi:10.1016/S0165-1781(02)00318-9.
Rempfer, M.V., McDowd, J.M., & Brown, C.E., 2017. Measuring learning potential in people with schizophrenia: A comparison of two tasks. Psychiatry Res. 258, 316–321. doi:10.1016/j.psychres.2017.08.057.
Revheim, N., Schechter, I., Kim, D., Silipo, G., Allingham, B., Butler, P., Javitt, D.C., 2006. Neurocognitive and symptom correlates of daily problem-solving skills in schizophrenia. Schizophr. Res. 83, 237–245. doi:10.1016/j.schres.2005.12.849.
Rispaud, S.G., Rose, J., Kurtz, M.M., 2016. The relationship between change in cognition and change in functional ability in schizophrenia during cognitive and psychosocial rehabilitation. Psychiatry Res. 244, 145–150. doi:10.1016/j.psychres.2016.07.033.
Roberts, K.H., 2004. Longitudinal examination of neurocognitive function and community functioning in patients with recent onset and chronic schizophrenia (Unpublished doctoral dissertation). University of Hull, England.
Rocca, P., Galderisi, S., Rossi, A., Bertolino, A., Rucci, P., Gibertoni, D., Montemagni, C., Bellino, S., Aguglia, E., Amore, M., Bellomo, A., Biondi, M., Carpiniello, B., Cuomo, A., D'Ambrosio, E., dell'Osso, L., Girardi, P., Marchesi, C., Monteleone, P., Montemitro, C., Oldani, L., Pacitti, F., Roncone, R., Siracusano, A., Tenconi, E., Vita, A., Zeppegno, P., Steardo, L., Jr., Vignapiano, A., Goracci, A., Members of the Italian Network for Research on Psychoses, 2018. Disorganization and real-world functioning in schizophrenia: results from the multicenter study of the Italian Network for Research on Psychoses. Schizophr. Res. 201, 105–112. doi:10.1016/j.schres.2018.06.003.
Ruse, S.A., Harvey, P.D., Davis, V.G., Atkins, A.S., Fox, K.H., Keefe, R.S.E., 2014. Virtual reality functional capacity assessment in schizophrenia: Preliminary data regarding feasibility and correlations with cognitive and functional capacity performance. Schizophr. Res. Cogn. 1, e21–e26. doi:10.1016/j.scog.2014.01.004.
Sabbag, S., Twamley, E.W., Vella, L., Heaton, R.K., Patterson, T.L., Harvey, P.D., 2012. Predictors of the accuracy of self-assessment of everyday functioning in people with schizophrenia. Schizophr. Res. 137, 190–195. doi:10.1016/j.schres.2012.02.002.
Sablier, J., Stip, E., Jacquet, P., Giroux, S., Pigot, H., Mobus Group, Franck, N., 2012. Ecological assessments of activities of daily living and personal experiences with Mobus, an assistive technology for cognition: a pilot study in schizophrenia. Assist. Technol. 24, 67–77. doi:10.1080/10400435.2012.659324.
Savla, G.N., 2009. Executive functions in schizophrenia: defining and refining the constructs (Doctoral dissertation). ProQuest Dissertations and Theses database (UMI No. 3349662).
Semkovska, M., Bédard, M.A., Godbout, L., Limoge, F., Stip, E., 2004. Assessment of executive dysfunction during activities of daily living in schizophrenia. Schizophr. Res. 69, 289–300. doi:10.1016/j.schres.2003.07.005.
Semkovska, M., Stip, E., Godbout, L., Paquet, F., Bédard, M.A., 2002. Behavioral disorganization in schizophrenia during a daily activity: the Kitchen Behavioral Scoring Scale. Brain Cogn. 48, 546–553.
Sestito, N., 2010. Improving everyday action through executive training in schizophrenia (Unpublished doctoral dissertation). Drexel University, Pennsylvania.
Seter, C., Giovannetti, T., Kessler, R.K., Worth, S., 2011. Everyday action planning in schizophrenia. Neuropsychol. Rehabil. 21, 224–249. doi:10.1080/09602011.2010.544519.
Strassnig, M.T., Bowie, C., Pinkham, A.E., Penn, D., Twamley, E.W., Patterson, T.L., Harvey, P.D., 2018. Which levels of cognitive impairments and negative symptoms are related to functional deficits in schizophrenia? J. Psychiatr. Res. 104, 124–129. doi:10.1016/j.jpsychires.2018.06.018.
Strassnig, M.T., Raykov, T., O'Gorman, C., Bowie, C.R., Sabbag, S., Durand, D., Patterson, T.L., Pinkham, A., Penn, D.L., Harvey, P.D., 2015. Determinants of different aspects of everyday outcome in schizophrenia: the roles of negative symptoms, cognition, and functional capacity. Schizophr. Res. 165, 76–82. doi:10.1016/j.schres.2015.03.033.
Sumiyoshi, C., Takaki, M., Okahisa, Y., Patterson, T.L., Harvey, P.D., Sumiyoshi, T., 2014. Utility of the UCSD Performance-based Skills Assessment-Brief Japanese version: Discriminative ability and relation to neurocognition. Schizophr. Res. Cogn. 1, 137–143. doi:10.1016/j.scog.2014.08.002.
Takahashi, H., Iwase, M., Nakahachi, T., Sekiyama, R., Tabushi, K., Kajimoto, O., Shimizu, A., Takeda, M., 2005. Spatial working memory deficit correlates with disorganization symptoms and social functioning in schizophrenia. Psychiatry Clin. Neurosci. 59, 453–460. doi:10.1111/j.1440-1819.2005.01398.x.
Tan, B.-L., King, R., 2013. The effects of cognitive remediation on functional outcomes among people with schizophrenia: a randomised controlled study. Aust. N. Z. J. Psychiatry. 47, 1068–1080. doi:10.1177/0004867413493521.
Thornton, A.E., Kristinsson, H., DeFreitas, V.G., Thornton, W.L., 2010. The ecological validity of everyday cognition in hospitalized patients with serious mental illness. J. Clin. Exp. Neuropsychol. 32, 299–308. doi:10.1080/13803390903002209.
Träger, C., Decker, L., Wæhrens, E.E., Knorr, U., Miskowiak, K., Vinberg, M., 2017. Influences of patient informed cognitive complaints on activities of daily living in patients with bipolar disorder: an exploratory cross-sectional study. Psychiatry Res. 249, 268–274. doi:10.1016/j.psychres.2016.12.058.
Twamley, E.W., Doshi, R.R., Nayak, G.V, Palmer, B.W., Golshan, S., Heaton, R.K., Patterson, T.L., Jeste, D.V., 2002. Generalized cognitive impairments, ability to perform everyday tasks, and level of independence in community living situations of older patients with psychosis. Am. J. Psychiatry. 159, 2013–2020. doi:10.1176/appi.ajp.159.12.2013.
Twamley, E.W., Savla, G.N., Zurhellen, C.H., Heaton, R.K., Jeste, D.V., 2008. Development and pilot testing of a novel compensatory cognitive training intervention for people with psychosis. Am. J. Psychiatr. Rehabil. 11, 144–163. doi:10.1080/15487760801963678.
Twamley, E.W., Woods, S.P., Zurhellen, C.H., Vertinski, M., Narvaez, J.M., Mausbach, B.T., Patterson, T.L., Jeste, D.V., 2008. Neuropsychological substrates and everyday functioning implications of prospective memory impairment in schizophrenia. Schizophr. Res. 106, 42–49. doi:10.1016/j.schres.2007.10.030.
Velligan, D.I., Bow-Thomas, C.C., Mahurin, R.K., Miller, A.L., 2000. Do specific neurocognitive deficits predict specific dimensions of outcome in schizophrenia? Schizophr. Res. 29, 63. doi:10.1016/s0920-9964(97)88454-x.
Velligan, D.I., Mintz, J., Sierra, C., Martin, M.L., Fredrick, M., Maglinte, G.A., Corey-Lisle, P.K., 2016. The Daily Activity Report (DAR) a novel measure of functional outcome for serious mental illness. Schizophr. Bull., 42, 579–587. doi:10.1093/schbul/sbv185.
Vizzotto, A.D.B., Celestino, D.L., Buchain, P.C., Oliveira, A.M., Oliveira, G.M.R., Di Sarno, E.S., Napolitano, I.C., Elkis, H., 2016. A pilot randomized controlled trial of the Occupational Goal Intervention method for the improvement of executive functioning in patients with treatment-resistant schizophrenia. Psychiatry Res. 245, 148–156. doi:10.1016/j.psychres.2016.05.011.
Zayat, E., Rempfer, M., Gajewski, B., Brown, C.E., 2011. Patterns of association between performance in a natural environment and measures of executive function in people with schizophrenia. Psychiatry Res. 187, 1–5. doi:10.1016/j.psychres.2010.11.011.
References
- American Psychiatric Association . fifth edition. American Psychiatric Association; Washington, DC: 2013. Diagnostic and Statistical Manual of Mental Disorders. [DOI] [Google Scholar]
- Babineau J. Product review: covidence (systematic review software) J. Can. Heal. Libr. Assoc. 2014;35:68. doi: 10.5596/c14-016. [DOI] [Google Scholar]
- Bowie C.R., McGurk S.R., Mausbach B., Patterson T.L., Harvey P.D. Combined cognitive remediation and functional skills training for schizophrenia: effects on cognition, functional competence, and real-world behavior. Am. J. Psychiatry. 2012;169:710–718. doi: 10.1176/appi.ajp.2012.11091337. [DOI] [PubMed] [Google Scholar]
- Connor L.T., Maeir A. Putting executive performance in a theoretical context. OTJR Occup. Particip. Heal. 2011;31:S3–S7. doi: 10.3928/15394492-20101108-02. [DOI] [PubMed] [Google Scholar]
- Cramm H.A., Krupa T.M., Missiuna C.A., Lysaght R.M., Parker K.H. Executive functioning: a scoping review of the occupational therapy literature. Can. J. Occup. Ther. 2013;80:131–140. doi: 10.1177/0008417413496060. [DOI] [PubMed] [Google Scholar]
- Galletly C., Rigby A. An overview of cognitive remediation therapy for people with severe mental illness. ISRN Rehabil. 2013;2013:1–6. doi: 10.1155/2013/984932. [DOI] [Google Scholar]
- Harvey P.D., Velligan D.I., Bellack A.S. Performance-based measures of functional skills: usefulness in clinical treatment studies. Schizophr. Bull. 2007;33:1138–1148. doi: 10.1093/schbul/sbm040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayden J.A., Co P. Evaluation of the quality of prognosis studies in systematic reviews. Ann. Intern. Med. 2006;144:427–437. doi: 10.7326/0003-4819-144-6-200603210-00010. [DOI] [PubMed] [Google Scholar]
- James A.B., Pitonyak J.S. Activities of daily living and instrumental activities of daily living. In: Boyt Schell B.A., Gillen G., editors. Willard and Spackman’s Occupational Therapy. 13th edition. Wolters Kluwer; Philadelphia: 2019. pp. 714–752. [Google Scholar]
- Josman N., Meyer S. Conceptualisation and use of executive functions in paediatrics: a scoping review of occupational therapy literature. Aust. Occup. Ther. J. 2019;66:77–90. doi: 10.1111/1440-1630.12525. [DOI] [PubMed] [Google Scholar]
- Josman N., Regev S. Dynamic interactional model in severe mental illness: strategy-based intervention. In: Toglia J., Katz N., editors. Cognition, Occupation, and Participation Across the Lifespan. fourth edition. AOTA Press; Bethesda: 2018. pp. 387–403. [Google Scholar]
- Josman N., Schenirderman A.E., Klinger E., Shevil E. Using virtual reality to evaluate executive functioning among persons with schizophrenia: a validity study. Schizophr. Res. 2009;115:270–277. doi: 10.1016/j.schres.2009.09.015. [DOI] [PubMed] [Google Scholar]
- Knight M.J., Baune B.T. Executive function and spatial cognition mediate psychosocial dysfunction in major depressive disorder. Front. Psychiatry. 2018;9:3–6. doi: 10.3389/fpsyt.2018.00539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loewenstein D., Acevedo A. The relationship between instrumental activities of daily living and neuropsychological performance. In: Marcotte T.D., Grant I., editors. Neuropsychology of Everyday Functioning. Guilford Press; New York: 2010. pp. 93–112. [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J. Clin. Epidemiol. 2009;62:1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- National Institute of Mental Health Health and education: mental illness. 2019. https://www.nimh.nih.gov/health/statistics/mental-illness.shtml#part_154784
- Overdorp E.J., Kessels R.P.C., Claassen J.A., Oosterman J.M. The combined effect of neuropsychological and neuropathological deficits on instrumental activities of daily living in older adults: a systematic review. Neuropsychol. Rev. 2016;26:92–106. doi: 10.1007/s11065-015-9312-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramsey R., Swarbrick P. Providing occupational therapy services for persons with psychiatric disabilities: promoting recovery and wellness. In: Boyt Schell B.A., Gillen G., Scaffa M.E., editors. Willard and Spackman’s Occupational Therapy. 12th edition. Wolters, Kluwer; Philadelphia: 2014. pp. 936–945. [Google Scholar]
- Rempfer M.V., Fowler C.A. Relationships among functional capacity, cognition, and naturalistic skill performance in people with serious mental illness. Psychiatry Res. 2018;270:453–458. doi: 10.1016/j.psychres.2018.10.016. [DOI] [PubMed] [Google Scholar]
- Rogers J.C., Holm M.B. Functional assessment in mental health: lessons from occupational therapy. Dialogues Clin. Neurosci. 2016;18:145–154. doi: 10.31887/DCNS.2016.18.2/jrogers. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toglia J., Katz N., editors. Cognition, Occupation, and Participation Across the Lifespan. fourth edition. AOTA Press; Bethesda: 2018. Executive functioning: prevention and health promotion for at-risk populations and those with chronic disease; pp. 129–142. [Google Scholar]
- World Health Organization . World Health Organization; Geneva: 2001. International Classification of Functioning, Disability and Health. [Google Scholar]
- Zayat E., Rempfer M., Gajewski B., Brown C.E. Patterns of association between performance in a natural environment and measures of executive function in people with schizophrenia. Psychiatry Res. 2011;187:1–5. doi: 10.1016/j.psychres.2010.11.011. [DOI] [PubMed] [Google Scholar]