Abstract
Inadequate care during early childhood can lead to long-term deficits in skill development. Parenting programs are promising tools for improving parenting practices and opportunities for healthy development. We implemented a non-masked cluster-randomized controlled trial in rural China in order to assess the effectiveness of an integrated home-visitation program that includes both psychosocial stimulation and health promotion at fostering development and health outcomes of infants and toddlers in rural China. All 6–18 month-old children of two rural townships and their main caregiver were enrolled. Villages were stratified by township and randomly assigned to intervention or control. Specifically, in September 2015 we assigned 43 clusters to treatment (21 villages, 222 caregiver-child dyads) or control (22 villages, 227 caregiver-child dyads). In the intervention group, community health workers delivered education and training on how to provide young children with psychosocial stimulation and health care (henceforth psychosocial stimulation and health promotion) during bi-weekly home visits over the period of one year. The control group received no home visits. Primary outcomes include measures of child development (i.e. the Bayley Scales of Infant and Toddler Development, third edition—or Bayley-III) and health (i.e. measures of morbidity, nutrition, and growth). Secondary outcomes are measures of parenting practices. Intention-to-treat (ITT) effects show that the intervention led to an improvement of 0·24 standard deviations (SD) [95% CI 0·04 SD-0·44 SD] in cognitive development and to a reduction of 8·1 [95% CI 3·8–12·4] percentage points in the risk of diarrheal illness. In addition, we find positive effects on parenting practices mirroring these results. We conclude that an integrated psychosocial stimulation and health promotion program improves development and health outcomes of infants and toddlers (6 to 30 month-old children) in rural China. Because of low incremental costs of adding program components (that is, adding health promotion to psychosocial stimulation programs), integrated programs may be cost-effective.
Keywords: Early childhood development, integrated parenting program, psychosocial stimulation, health promotion, randomized controlled trial, rural China
Introduction
250 million children below the age of five in low and middle income countries are currently at risk of not achieving their full developmental potential due to risk factors such as poverty, malnutrition and non-stimulating home environments (Engle et al., 2007; Grantham-McGregor et al., 2007; Black et al., 2017). The threat of large losses of human potential due to inequality of opportunity for children to develop healthily due to their circumstances during early childhood—the period when the neurobiological capacity for change in the foundations of the hierarchical processes of skill development and brain malleability is the highest—provides a strong economic and neurobiological rationale for investment in the developmental opportunities of disadvantaged children (Heckman, 2013). Caregivers can exert a major influence on child development and health (including nutrition) via provision of a nurturing and safe home environment with sufficient learning opportunities that is stable and sensitive to children’s health needs (Ngure et al., 2014; Britto et al., 2017). This study aims to contribute to the intervention literature on the impact of parenting training on the developmental potential of disadvantaged populations. Over the past 15 years, efficacy trials of parenting training programs (henceforth, psychosocial stimulation and health promotion interventions) in low- and middle-income countries have provided evidence of short-term and long-term effects on development and health outcomes. In the short run, parenting programs targeting psychosocial stimulation have consistently been linked to better cognitive development (Attanasio et al., 2014; Aboud & Yousafzai, 2015; Sylvia et al., 2018); health interventions (including those that primarily target nutrition) have been found to have positive but inconsistent effects on child cognitive development (Rao et al., 2014), nutritional outcomes (e.g. anemia) (Grantham-McGregor, Fernald, Kagawa, & Walker, 2014; Aboud & Yousafzai, 2015; Pérez-Escamilla & Moran, 2017), and the incidence of diarrheal illness (Luby et al., 2018); and programs targeted at hygiene and sanitation (e.g. handwashing) have the potential to reduce child morbidity (Fewtrell et al., 2005; Mistry et al., 2012; Seguin & Zarazúa, 2015). In the long run, pioneering parenting training programs have been linked to lasting effects on a range of lifelong human capital outcomes including academic attainment, earnings, responsible citizenship, and health later in life (Heckman & Kautz, 2014).
While the efficacy of parenting programs in low- and middle-income countries is well established, a significant policy challenge is how programs can be delivered cost-effectively and at scale. One suggested approach has been to integrate early childhood development (ECD) programs (that we label as ‘psychosocial stimulation’ programs in this study) with health programs (Gowani, Yousafzai, Armstrong, & Bhutta, 2014; Yousafzai, Rasheed, Rizvi, Armstrong, & Bhutta, 2014; Hamadani et al., 2019). Integrated programs targeted at multiple risk factors have the potential to minimize the odds of developmental delay for disadvantaged populations, while they can be more cost-effective than single-objective programs (Richter et al., 2017). Integrating programs can lead to gains in cost-effectiveness because of complementarities among different domains of child development and health (Attanasio, Cattan, Fitzsimons, Meghir & Rubio-Codina, 2015). Health has been identified as a particularly important input for cognition (Attanasio, Meghir & Nix, 2015). In addition, joint delivery of program components may facilitate cost-saving complementarities on the implementation side since the costs common to interventions (e.g., hiring parenting trainers and installing a monitoring system) can be shared. Similar arguments have been used to rationalize the practice of delivering health and nutrition programs through schools (Ran, Chattopadhyay & Hahn, 2016; Bundy, de Silva, Horton, Jamison & Patton, 2018). Systematic reviews of ECD interventions concluded that integrated psychosocial stimulation and nutrition (only) programs can maintain the effects of each program component, but the existence of additivities between stimulation and nutrition components is unsure (Hurley, Yousafzai, & Lopez-Boo, 2016). Earlier home-visitation programs combined psychosocial stimulation with nutrition supplementation, but did not deliver a program to provide parents with information on child health more broadly defined (Grantham-McGregor, Fernald, Kagawa, & Walker, 2014; Hurley et al., 2016). To the best of our knowledge, large-scale empirical evidence on the effectiveness of programs integrating training on psychosocial stimulation with health promotion (through the provision of information services) does not exist.
In collaboration with the non-governmental organizations Save The Children Beijing and Save the Children Hong Kong, we aimed to assess the effectiveness of a home visitation program combining parental training of child psychosocial stimulation with training on child health promotion. In this study, child psychosocial stimulation refers to engagement in interactive caregiver-child activities that benefit cognitive and social-emotional skill development (e.g., reading books to child); and child health promotion refers to the provision and use of adequate and appropriate child nutrition, hygiene habits, and other health-promoting behavior (e.g., oral hygiene of infants) by the primary caregiver. The parenting training of both components was delivered by local community health workers.
This intervention study was implemented in rural China. Despite a spectacular rise in overall well-being in China over the past four decades, many rural children are still born and raised in poverty, which puts them at a large disadvantage as compared to children that grow up in more well-off urban areas. Approximately 46% and 55% of infants growing up in poor rural areas were found to be developmentally delayed by the age of 1 and 2, respectively (Wang et al., 2019). In line with international research findings, this high prevalence of developmental delay has been linked to insufficiently stimulating learning environments and poor health promotion, including poor feeding practices, in remote rural areas (Luo et al., 2017; Sylvia et al., 2018). For example, a large-scale field study showed that, respectively, no more than 9% and 18% of poor, rural Chinese one year olds were engaged in interactive caregiver-child reading activities or story-telling during the previous day (Wang et al., 2019). Moreover, a large fraction (more than 30%) of them were found to be anemic according to the WHO definition of anemia (Luo et al., 2015). This high prevalence of micronutrient deficiency was linked to poor feeding practices such as the provision of an overly plain diet low in iron-rich foods (Luo et al., 2014). Finally, no more than 76·6% of the rural caregivers in a large-scale survey reported that they always washed hands after changing a diaper. Respectively, only 25·1% and 51·3% of the respondents reported that they would always use soap and running water for handwashing (Tao, Cheng, Lu, Hu, & Cheng, 2013). The absence of certain parenting practices may at least partly be caused by the fact that rural Chinese caregivers have no access to standard-of-care programs that are specifically designed to deliver information on psychosocial stimulation or child health. Lacking access to health services has been linked to a lower likelihood for caregivers’ to seek care from a (trained) care provider for their children (Haque, Parr & Muhidin, 2019). This type of community disadvantage (i.e. lacking access to quality health services) was found to be negatively associated with physical development of children in rural China (Lei, 2017). Furthermore, the overall quality of primary care that is available in rural Chinese communities is poor (Sylvia et al., 2015).
On the basis of a literature review of common, but problematic parenting practices in rural China (Luo et al., 2014; Wang et al., 2019) and in other low-resource regions (Ngure et al., 2014; Britto et al., 2017), a structured curriculum was designed to address parenting practices related to psychosocial stimulation and health promotion, including nutrition. We postulate that the integrated intervention will benefit child development and health outcomes as a result of intervention-induced adjustments in parenting skills and practices.
Methods
Study design
We designed the intervention as a cluster-randomized controlled trial covering all 43 villages in two rural townships in Yunnan and Hebei Province, China. These two townships, one in each province, were selected in consultation with local authorities from a list containing all poor, rural townships in the respective provinces. We randomized at the village level to reduce the risk of contamination across experimental groups. The intervention was implemented for one year beginning in October 2015. Follow-up data were collected in late September/October 2016. Approval for the study was obtained from the provincial offices of the National Health Commission (NHC) in Yunnan and Hebei in 2017, and from the ethics committee of Stanford University (USA, number 25734) on October 26, 2012 and renewed annually.
Participants
Sample households were selected based on a list of all registered births in the selected clusters provided by the local office of the NHC. All children aged 6–18 months on September 15, 2015 were enrolled in the study together with their primary caregivers. On average, 10 children were enrolled in each cluster. The resulting baseline sample includes 449 caregiver-child dyads from 43 villages. Due to internal migration, 13·8% of the caregiver-child dyads attritted by September 2016. As a consequence, follow-up data were collected for 390 children living in 42 villages. The caregivers of all children gave oral informed consent before enrolment and baseline data collection. Using Zelen’s randomized consent design, we sought participant consent conditional on the assigned treatment status (Zelen, 1979). All caregivers were asked to give their informed consent for data collection. Prior to the start of the intervention, caregivers assigned to the intervention group were then additionally asked to give consent for participation in the parenting intervention.
Randomization and masking
In September 2015 the clusters were randomly assigned to control and treatment within two strata (one township in Yunnan Province and another in Hebei Province) using a computerized random number generator. Though complete masking was not possible in this study, caregivers were unaware that they were involved in an experiment and control group households were unaware of the intervention.
Procedures
All children and caregivers residing in clusters of the intervention group were enrolled for a home-based parenting program targeting child psychosocial stimulation and health promotion. During each of the fortnightly home visits over the period of one year, community health workers trained caregivers on interactive caregiver-child activities and provided them with information on child health and nutrition. All interactive caregiver-child activities were stage-based and fully scripted in an ECD curriculum. This curriculum was loosely based on the curriculum developed for a pioneering parenting intervention in Kingston, Jamaica and adapted to Chinese settings by local child development psychologists and ECD experts (Sylvia et al., 2018). Each activity focused on one of the following four types of skills: cognition, language, motor, or social-emotional skills. During each bi-weekly visit two new skill-activities were introduced (that is, parents were given training in the activities) such that caregivers would encounter a new activity that was designed to promote each of the four targeted developmental skills each month.
During each visit, caregivers also received information on child health promotion through structured conversations about age-appropriate nutrition and health topics. These structured conversations were developed by experts of the Capital Institute of Pediatrics (CIP) of the Chinese Academy of Medical Sciences (CAMS). Nutrition topics included age-appropriate feeding practices, dietary diversity, meal frequency, and nutritional supplementation. Health information covered issues related to immunization, hygiene, and healthy eating and sleeping behavior. During each training session the child was measured and weighed. In cases where health workers observed deviating growth trajectories, important developmental delays or potentially serious illnesses, they would advise the caregiver to consult a medic.
Home visits were delivered by community health workers in service of the NHC. To provide the local health workers with necessary knowledge, skills and tools to deliver quality parenting training in psychosocial stimulation and health promotion, they received a copy of the fully-scripted ECD curriculum for instructions on interactive play activities, an ECD toolkit (including a growth chart, development check list, counselling materials and user handbook), and a manual with stage-based structured conversations on child health issues. In addition, all trainers (n=36, see table 2) participated in a one-week intensive training course on the basic theories of ECD and on communication, coaching and counselling skills taught by three ECD experts. The training program consisted of 5 days of classroom-based instruction in combination with 2 days of field practice. Fully-scripting the curriculum obviated the need for more extensive training of the community health workers, reducing overall program costs significantly.
Table 2:
Intervention activities
| Number | |
|---|---|
| Eligible children | 449 |
| Trained parenting instructors | 36 |
| Total number of home visits | 3387 |
| Average number of home visits per household | 15·3 |
To monitor service quality, a carefully designed supervisory system was set up and implemented by the government. First, the compliance of the community health care workers was tracked by a mobile app which requested the workers to log into at the start of each home visit. Second, county-level or township-level officials of the NHC randomly conducted unannounced supervision of a home visit of each instructor every 3 months and provided feedback and reinforcement training. Third, phone interviews were conducted to invite caregivers to give feedback on the quality of home visits. All intervention households received phone calls on a revolving basis. Every two months, a third of the enrolled primary caregivers in each village were called. Course content of the reinforcement training sessions was adjusted according to caregiver feedback.
Outcomes
Primary outcomes of interest are measures of child development and health, including the incidence of illness, nutrition and physical growth. First, child development was assessed at baseline (at 6–18 months) and follow-up (at 18–30 months) using the third edition of the Bayley Scales of Infant and Toddler Development (Bayley-III; Bayley, 2006). The four scales for cognition, language, motor, and social-emotional skill development of the Bayley-III questionnaire were translated into Mandarin Chinese and adapted to Chinese settings. Earlier versions of the Bayley scale have been used in China and reported in the papers of other research teams (Luo et al., 2015; Luo et al., 2017; Sylvia et al., 2018; Wang et al., 2019). The language scale consists of two subscales measuring receptive and expressive language development; the motor scale comprises the subscales of fine and gross motor skills. Bayley-III tests were administered at home by trained enumerators. All enumerators attended a one-week training course including 2·5 days of experiential learning in the field at baseline and follow-up. We use Bayley-III raw scores instead of normed composite scores to construct measures of early skill development. An official reference population distribution for normalization of Bayley-III scores has not been established for China yet, hence we standardize Bayley-III raw scores using the observed sample distribution of scores. Given that Bayley-III raw scores are increasing in age, we eliminated the age effect by internally standardizing raw scores within age (month) groups. This is done by first estimating age-conditional means and standard deviations using non-parametric regression and then using these estimated statistics to compute age-adjusted internal z-scores for each subscale. This non-parametric standardization procedure has the advantage that it is less sensitive to outliers and small sample sizes within age categories than parametric procedures (Attanasio, Cattan, Fitzsimons, Meghir & Rubio-Codina, 2015; Rubio-Codina, Araujo, Attanasio, Muñoz & Grantham-McGregor, 2016).
Second, child nutritional status was evaluated based on hemoglobin (Hb) measures collected by finger prick blood tests. Third, child health outcomes were obtained by caregiver-reported survey answers of child health status undertaken by trained enumerators. The risk of diarrheal illness and respiratory tract infections were assessed based on caregiver-reported incidence of diarrheal illness and symptoms of respiratory tract infection, i.e. coughing or having a cold during the two weeks prior to the survey. Fourth, child height and weight were measured by trained enumerators. We used a scale to weigh children with minimal clothing. We did tared weighing of children below the age of two and children over age two who wouldn’t stand still. Height was assessed with a child measure mat.
We further collected information on secondary outcomes that might mediate intervention effects on primary outcomes. Secondary outcomes of interest in this study are measures of parenting practices and parental beliefs related to child psychosocial stimulation and health promotion (e.g., ability to read books to child, engagement of caregiver in interactive play with child) and measures of health promoting feeding practices (e.g., provision of iron rich foods for child). All measures were collected during a comprehensive household interview questionnaire administered to each child’s main caregiver.
Statistical Analysis
We calculated the target sample size to detect a 0·25 standardized effect on Bayley-III cognition scores – the main outcome variable of interest. Based on evidence from an earlier field experiment (Sylvia et al., 2018), we assumed an adjusted intraclass correlation coefficient (ICC) of 0·01 and that baseline scores would account for 60% of the variation in scores at follow-up. We further assumed an average cluster size of 10 children of 6–18 months of age with a coefficient of variation of cluster sizes of 0·5. Based on these parameters, we calculated that we required 19 clusters (n=190 children) per treatment group to detect an effect size of 0·25 SD at 80% power given a two-sided significance level of 0·05. Additional villages were enrolled to overpower the study and allow for potential attrition.
We conducted the statistical analysis using Stata version 14.2. We used an analysis of covariance (ANCOVA) model to estimate intention-to-treat (ITT) effects of the intervention on our primary and secondary outcomes. We used the most parsimonious model, where we regressed the outcome variables on an indicator that takes the value of 1 if the household was assigned to the intervention group and the value of 0 otherwise, the baseline value of the outcome variable, and stratum (township) fixed effect. Enumerator fixed effects were included for estimation of ITT effects on Bayley-III scores. All individuals (n=390) with baseline and endline data were included in the analysis. P-values reported refer to two-tailed tests for the impact of the intervention.
Given multiple outcomes, we account for multiple hypothesis testing in the analysis. In order to limit the probability of falsely rejecting a test, we aggregate outcome measures within each domain into a summary index and estimate ITT effects on these summary indices (Fitzsimons, Malde, Mesnard, & Vera-Hernandez, 2016). Each index is computed as a weighted mean of the standardized values of the outcome variables (with outcome variables re-defined such that higher values translated into a more desirable outcome). This summary index is an efficient Generalized Least Squares (GLS) estimator. The GLS weights are calculated to maximize efficiency by giving less weighted to outcomes that are highly correlated with each other, while outcomes that are uncorrelated and thus contain new information receive more weight. To obtain meaningful ITT estimates, we internally standardize the summary indices within age (month) group. This trial is registered with the ISRCTN registry, number ISRCTN72589193.
Role of funding source
The National Science Foundation of China, the Data Center of Management Science NSFC-PKU and Save the Children Hong Kong financed the trial. The National Science Foundation of China, the Data Center of Management Science NSFC-PKU and Save the Children Hong Kong had no role in study design, data collection, data analysis, data interpretation, or writing of the report. Save the Children Beijing was involved in management and monitoring of the trial. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
Baseline data were collected between September 15 and October 15, 2015. 43 clusters were stratified by township and randomly assigned to intervention (21 clusters, 222 caregiver-child dyads) or control (22 clusters, 227 caregiver-child dyads; figure 1). 59 children (27 in intervention group, 32 in control group) were lost to follow-up. 390 children (190 in intervention group, 200 in control group) with follow-up data collected between September 15 and October 15, 2016 were included in the intention-to-treat analysis.
Fig. 1.
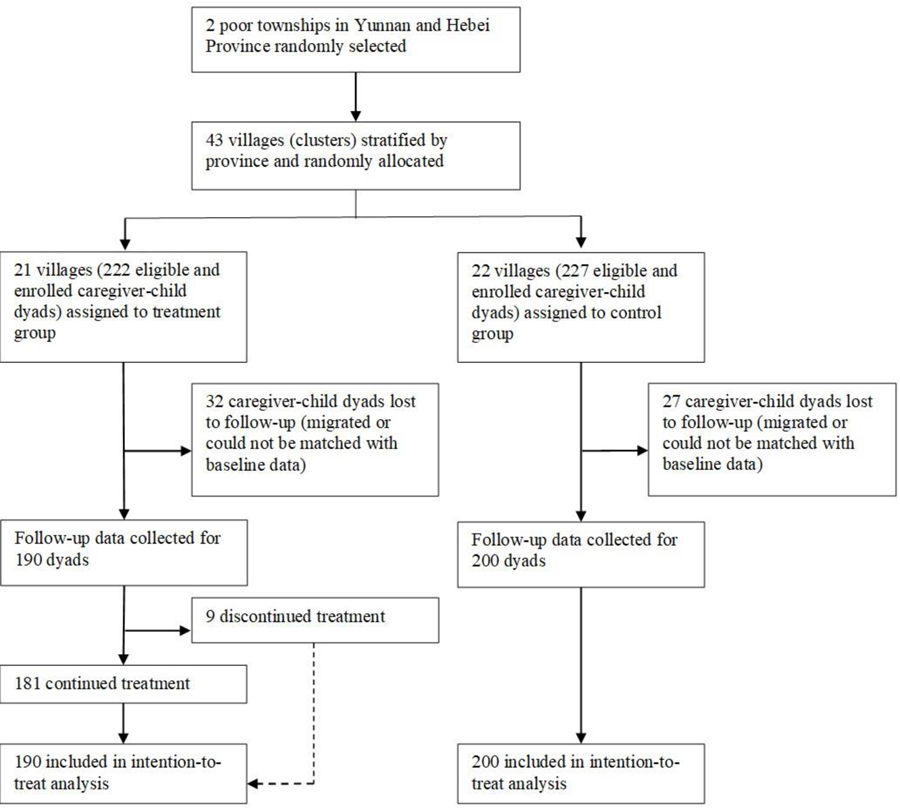
Trial profile.
Table 1 shows descriptive statistics on child development, health, nutrition, and growth at baseline. 29·7% of the baseline sample didn’t achieve a Bayley-III composite cognition score of 92 - the age-appropriate cut-off score for cognitive delays (Wang et al., 2019). Descriptive statistics on baseline demographics, parenting skills and practices are shown in tables A.1, A.2, and A.3, respectively, of the online appendix. These tables also include tests for balance across the control and intervention arms. Differences across most of the individual characteristics are insignificant. An omnibus test across all baseline covariates (in tables 1, A.1, A.2, and A.3) shows that the two groups are well balanced at baseline. We test this by regressing treatment status on the baseline characteristics and testing whether the coefficients were jointly equal to zero (p-value = 0·301). After accounting for attrition, our sample remains balanced (see table A.4). Table 2 gives an overview of the realisation and completion of intervention activities.
Table 1:
Baseline development, health, nutrition, and growth outcomes of intention-to-treat population
| Control (n=227) | Intervention (n=222) | P-value | |
|---|---|---|---|
| Child development# | |||
| Cognition score | 41·6 (9·0) | 40·6 (7·9) | 0·43 |
| Receptive language score | 14·0 (4·4) | 13·8 (4·0) | 0·89 |
| Expressive language score | 14·2 (5·3) | 13·6 (4·9) | 0·53 |
| Fine motor score | 28·9 (5·7) | 28·8 (5·0) | 0·75 |
| Gross motor score | 41·0 (10·7) | 40·6 (9·5) | 0·86 |
| Social-emotional score | 69·3 (13·5) | 68·7 (12·5) | 0·99 |
|
Child health | |||
| Diarrhea in past month | |||
| Yes | 61 (27%) | 46 (21%) | 0·21 |
| No | 166 (73%) | 176 (79%) | |
| Symptoms of respiratory tract infection in past month | |||
| Yes | 130 (57%) | 123 (55%) | 0·96 |
| No | 97 (43%) | 99 (45%) | |
| Number of times ill in past month | 1·0 (0·9) | 0·9 (0·9) | 0·30 |
|
Child nutrition and growth | |||
| Hemoglobin (g/L)§ | 106·6 (95·0–118·0) | 107·2 (98·0–117·0) | 0·93 |
| Anemic§ | |||
| Yes | 120 (54%) | 118 (56%) | 0·51 |
| No | 102 (46%) | 94 (44%) | |
| Height (cm)* | 76·2 (72·5–80·0) | 75·6 (72·0–79·0) | 0·48 |
| Weight (kg)* | 9·7 (8·7–10·7) | 9·6 (8·6–10·4) | 0·91 |
| Weight for age* | 0·16 (1·08) | 0·11 (1·14) | 0·76 |
| Underweight* | |||
| Yes | 10 (4%) | 5 (2%) | 0·13 |
| No | 213 (96%) | 211 (98%) | |
| Length for age* | 0·24 (1·22) | 0·03 (1·36) | 0·30 |
| Weight for length* | 0·10 (1·16) | 0·15 (1·13) | 0·33 |
Data are mean (SD), n (%), or median (IQR). ‘Anemic’ is a dummy variable = 1 if altitude-adjusted hemoglobin concentration < 110 g/L. ‘Underweight’ is a dummy variable = 1 if child’s weight-for-age z-score is more than two SD below the mean of the WHO reference population. P-values for difference in means across control and intervention group are adjusted for clustering at the village level.
Expressed in Bayley-III raw scores. Baseline Bayley-III scores are missing for 1 child.
Hemoglobin values are missing for 15 children at baseline.
Height and weight are missing for 9 children.
We find that the integrated parenting intervention had a significant effect on the summary index of skill development (effect size 0·17 SD, 95% CI 0·02 SD-0·33 SD, see table 3 and figure 2). We further find that the effect on the summary index was largely driven by the effect on cognitive development. The estimated ITT effect of the intervention on Bayley-III cognition scores was 0·24 SD [95% CI 0·04–0·44]. We find no effect on (receptive or expressive) language, (gross or fine) motor or social-emotional development that is significantly different from zero. Second, we find that the intervention improved overall caregiver-reported child health (effect size 0·29 SD, CI 95% 0·13 SD-0·46 SD). The intervention led to a reduction of 8·1 [95% CI 3·8–12·4] percentage points in the risk that the child had an episode of diarrhea during the two-week period prior to the survey. We find no significant effect on the number of times the child was ill during the past two weeks or the probability that the child displayed symptoms of respiratory tract infection over the past two weeks.
Table 3:
Estimated effects of intervention on child development, health, nutrition, and growth
| Outcomes | Intervention |
|||
|---|---|---|---|---|
| No. | β (95% CI) | P-value | Mean of control group at follow-up | |
| Panel A: Skill development | ||||
| Summary index§ | 385 | 0·17 (0·02–0·33) | 0·04 | −0·08 |
| Cognition score | 386 | 0·24 (0·04–0·44) | 0·01 | −0·11 |
| Receptive language score | 386 | −0·01 (−0·17–0·15) | 0·89 | −0·02 |
| Expressive language score | 386 | 0·14 (−0·03–0·32) | 0·09 | −0·04 |
| Gross motor score | 385 | 0·14 (−0·04–0·32) | 0·12 | −0·09 |
| Fine motor score | 386 | 0·13 (−0·03–0·29) | 0·09 | −0·06 |
| Social-emotional score | 386 | 0·10 (−0·07–0·27) | 0·24 | −0·01 |
|
Panel B: Health | ||||
| Summary index§ | 390 | 0·29 (0·13–0·46) | 0·001 | −0·15 |
| Diarrhea in past 2 weeks | 390 | −0·08 (−0·12– −0·04) | <0·001 | 0·12 |
| Symptoms of respiratory tract infection in past 2 weeks | 390 | −0·08 (−0·18–0·02) | 0·10 | 0·49 |
| Number of times ill in past 2 weeks | 390 | −0·08 (−0·23–0·07) | 0·27 | 0·72 |
|
Panel C: Nutrition and growth | ||||
| Hemoglobin (g/L) | 367 | −0·22 (−3·96–3·52) | 0·91 | 116·5 |
| Anemic | 367 | 0·01 (−0·11–0·12) | 0·92 | 0·27 |
| Summary index of physical growth§ | 380 | 0·07 (−0·08–0·22) | 0·33 | −0·03 |
| Length/height for age | 380 | 0·01 (−0·16–0·19) | 0·87 | −0·07 |
| Healthy length/height for age | 380 | 0·02 (−0·02–0·05) | 0·36 | 0·94 |
| Healthy weight for height | 380 | 0·02 (−0·03–0·07) | 0·38 | 0·92 |
| Healthy weight for age | 380 | −0·004 (−0·04–0·03) | 0·80 | 0·93 |
Diarrhea in past 2 weeks’ and ‘symptoms of respiratory tract infection in past 2 weeks’ are dummies = 1 if the child had diarrhea and coughed or had a cold over the past 2 weeks, respectively; 0 otherwise. ‘Length/height for age’ is a standardized z-score relative to the WHO reference population. ‘Healthy height for age’ is a dummy indicating that the child’s height for age is not more than two standard deviations below the mean of the WHO reference population. ‘Healthy weight for height’ and ‘healthy weight for age’ are dummies indicating that the scores are no more than two standard deviations above or below the respective means of the WHO reference populations.
The ‘summary index’ in panel A is the weighted average of the measures in rows 2–7. The ‘summary index’ in panel B is the weighted average of the absolute value of the measures in rows 2–4 of panel B. The ‘summary index’ in panel C is the weighted average of the measures in rows 5–7.
When we use the Romano-Wolf stepdown procedure to adjust the p-values of all variables (except for the summary indices) for the family-wise error rate, the ITT effects on cognition scores and the risk of diarrheal illness remain significant at the 5% level.
Fig. 2.
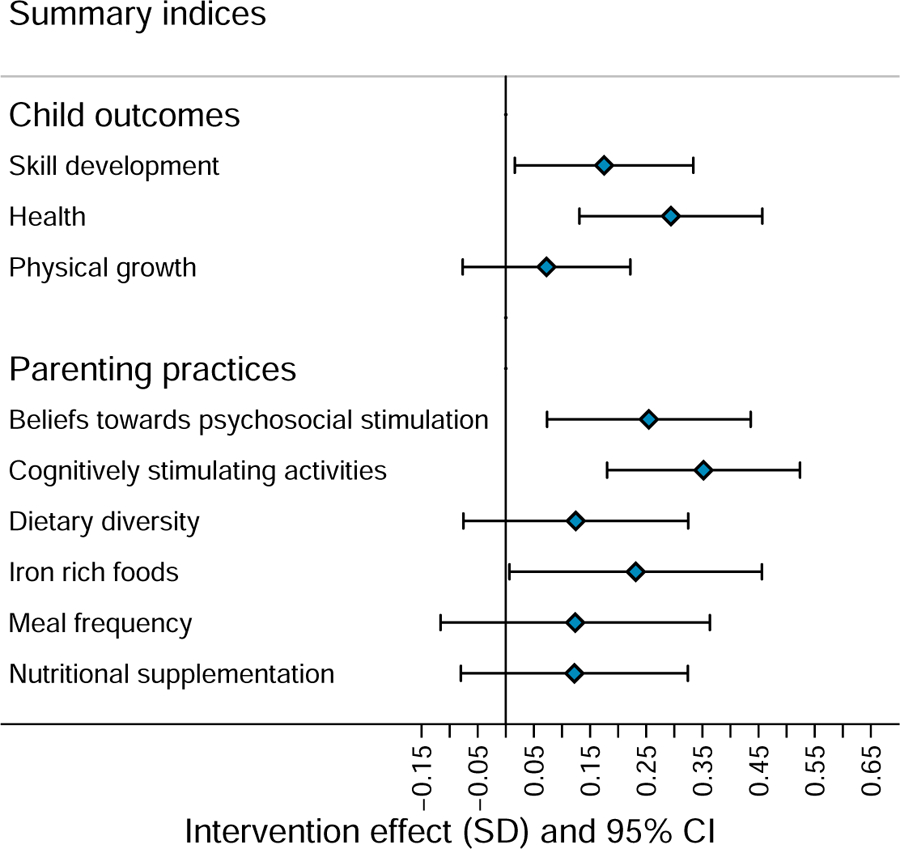
Estimated effect of intervention on summary indices.
The effects on child development and health may have been mediated by adjustments in parenting practices. First, we find that the intervention led to a significant improvement in parenting beliefs and practices related to child psychosocial stimulation (see table A.5). The parenting program led to an increase in the summary index of positive caregiver beliefs towards psychosocial stimulation (effect size 0·25 SD, 95% CI 0·07 SD-0·44 SD) and the summary index of child cognitively stimulating parenting practices (effect size 0·35 SD, 95% CI 0·18 SD-0·52 SD). More specifically, with regards to caregiver beliefs, we find an increase of 11·7 [95% CI 1·9–21·5] percentage points in the probability that a caregiver reported to know how to read to a child at the end of the intervention. Furthermore, with regard to the investment of caregivers in child psychosocial stimulation, we find that caregiver engagement in play activities with toys increased with 13·8 [95% CI 1·7–25·9] percentage points. We also observe a significant increase in the probability that a child had its own play area in the household (effect size 11·3 percentage points, 95% CI 3·3–19·4). Finally, we find a positive effect on the provision of an iron-rich diet for the child (effect size 0·23 SD, 95% CI 0·01 SD-0·46 SD, see table A.6). We find no effect on the nutrition supplementation index.
Discussion
Using a cluster-randomized controlled trial, we assessed the effectiveness of an integrated parenting program that combined training of child psychosocial stimulation with training of child health promotion. First, we found a small to moderate effect size of 0·24 SD on standardized Bayley-III cognition raw scores. This indicates that the program maintained the positive effect size on cognitive skill development typically observed in the literature for single-objective psychosocial stimulation programs (Britto et al., 2017). Should the size of the effect on cognition scores found in this study be considered large? In fact, the impact on Bayley-III cognition scores found in this study (of 0·24 SD) is on par with previous intervention studies deemed highly successful, particularly in this field of education in developing countries (McEwan, 2012). Additionally, a 0·24 SD increase in standardized Bayley-III cognition scores is a sizeable effect for an ECD intervention delivered at scale. Specifically, the effect size we detected is well in line with the effect of 0·26 SD and 0·27 SD observed in earlier home-based psychosocial stimulation interventions that were delivered to mimic an at-scale intervention in Colombia and rural China, respectively (Attanasio et al., 2014; Sylvia et al., 2018). It is true that earlier parenting intervention studies found effect sizes that were larger. In our study (as well as in the studies of Attanasio et al. (2014) and Sylvia et al. (2018)), the authors opted to administer the Bayley test—which is widely viewed as the gold standard for assessment of ECD outcomes. The earlier studies that found higher measured impacts not only used other measures to assess ECD outcomes, they also had different designs (e.g., smaller sample sizes; designs to test efficacy rather than effectiveness) (Aboud & Yousafzai, 2019; Hamadani et al., 2019). Hence, it may be that these changes in study design may explain why smaller effects were observed on Bayley cognition scores in more recent at scale interventions as compared to in earlier studies.
Second, we found no significant effect on child nutrition or growth outcomes. On the one hand, this can be due to a rather limited impact of the intervention on caregivers’ feeding behavior. We found a significant positive effect on the provision of an iron rich diet for the child, but not on overall dietary diversity or feeding frequency. On the other hand, considering the positive or insignificant effects on nutrition and growth outcomes observed in earlier single-objective nutrition interventions (Grantham-McGregor et al., 2014; Aboud & Yousafzai, 2015; Pérez-Escamilla & Moran, 2017), this finding of a null result is also not unexpected. The failure to find an effect on anemia is in line with findings from earlier nutrition interventions in rural China (Luo et al., 2017) and Colombia (Attanasio et al., 2014; Andrew, Attanasio, Fitzsimons & Rubio-Codina, 2016). For example, an earlier large-scale home-based micronutrient supplementation intervention in rural China led to an improvement in hemoglobin levels after six months, but the researchers found no evidence indicating that the effect on anemia persisted one year after the end of the intervention (Luo et al., 2017). As argued by the authors of these papers, the absence of detectable effects of nutrition interventions on anemia in these regions may be caused by the changing nature of the causes of low hemoglobin levels and rapid natural decreases in anemia rates during the second year of life. The hemoglobin level in the control group of our sample increased approximately with ten milligrams per liter between baseline and follow-up. This contrasts to nutrition programs that were found to have a significant and positive effect on hemoglobin levels in other regions, where less rapid increases in the hemoglobin levels of the control group were observed (see, for example, Soofi et al. (2013)). The failure to find an effect on physical growth outcomes can also be explained by the low rates of growth failure among 0–3 year olds in rural China (Wang et al., 2018). In our sample, respectively, no more than 4·5% and 2·3% of the sample children were stunted and wasted (according to the WHO’s Child Growth Standards). Moreover, it is possible that nutrition education programs are no effective tool to raise child physical growth in food secure regions. Systematic reviews found an uncertain impact of nutrition education interventions in food secure regions on child physical growth (Dewey & Adu-Afarwuah, 2008; Bentley, Wasser & Creed-Kanashiro, 2011; Lassi, Zahid, Das & Bhutta, 2013; Grantham-McGregor et al., 2014; Aboud & Yousafzai, 2015; Pérez-Escamilla & Moran, 2017). Finally, the failure to find an effect on growth in this study is strongly in line with Aboud, Singla, Nahil and Borisova (2013) who also found no significant effect on the physical development of one-year olds as a result of an at scale integrated parenting program in rural Bangladesh.
Third, we observed a reduction in children’s risk of diarrheal illness. Research on the effects of promoting changes in health-related parenting practices (e.g. handwashing and complementary feeding practices) indicates that health promotion interventions can lead to a reduction in the risk of influenza transmittable by hand, including diarrheal illness and respiratory tract infections, two main causes of morbidity and mortality among children below five (Fewtrell et al., 2005; Mistry et al., 2012; Seguin & Zarazúa, 2015; Luby et al., 2018). A systematic review of non-clinical interventions found that changing health-related parenting practices can lead to a reduction in the risk of diarrheal illness ranging from 13·3 to 61·0 percentage points among children in developing countries (Seguin & Zarazúa, 2015). This means that the effect of 8·1 percentage points observed in our study is comparatively small. This study is the first intervention study conducted in rural China that relates education on nutrition and health to a reduction in the risk of influenza transmittable by hand.
In terms of mechanisms, we find evidence that the effects on primary outcomes may have been mediated by improved parenting practices. This argument is supported by our finding of positive intervention effects on parenting beliefs and practices related to psychosocial stimulation. This finding is in line with earlier studies showing that enriching the home learning environment with more interactive play activities and materials can be a promising trajectory for promotion of ECD (Attanasio et al., 2014; Sylvia et al., 2018). We observed a positive adjustment in caregivers’ feeding practices. More specifically, we found that caregivers in the intervention group provided, on average, a more iron-rich diet for the child. Our findings on parental behavior change are well in line with Aboud et al. (2013) who detected positive intervention effects of an integrated parenting training program in rural Bangladesh on cognitively stimulating parenting practices and child dietary intake. Findings on the importance of good parenting practices will be disseminated as they may contribute to the spread of better parenting practices in the long run.
Finally, this integrated psychosocial stimulation and health promotion parenting program has the potential to be cost-effective and scalable. Cost-effectiveness comparisons are not straightforward due to incomparability of evidence across programs stemming from differences in data availability, data quality, duration of treatment, frequency of home-visits, length of follow-up, and other situational characteristics. Moreover, implementing parenting programs for a fine-grained comparative cost-effectiveness analysis comes at a very high cost. As a consequence, evidence on the cost-effectiveness of parenting training programs is very scarce. An exception was an intervention study in rural Pakistan showing that integrated parenting curricula combining nutritional supplementation with stimulation can be more cost-effective than mere nutrition or stimulation curricula separately (Gowani et al., 2014). In-depth comparative cost-effectiveness analyses are needed to guide policy makers interested in the scaling up of parenting programs. In this study, we do not have sufficient data to conduct such analysis. However, considering that the program produced gains across different domains, we argue that integration of program components can produce significant cost savings relative to single-objective programs as long as the incremental cost of adding a program component is low.
The strengths of this study include the application of a carefully developed parenting curriculum and data collection of a comprehensive set of child development and health outcomes. However, our study also faces several limitations. First, the study took place in only two townships in two Chinese provinces. Second, we estimated ITT effects at one point in time. Longer-run follow-up of sample children will be necessary to determine whether the observed gains will persist over time. Third, in the absence of clinically assessed health measures, we measured child health using caregiver-reported health-status questions. Fourth, approximately 13·1% (n=59) of children attritted from our sample between baseline and follow-up. This is unlikely to have significantly affected our estimates of program impact, however, given that attrition is balanced across experimental groups.
We also note that compliance to the intervention was relatively low. On average 15·3 visits out of 24 planned visits took place. To put this in perspective, on average 16·4 visits out of 24 planned visits were completed in an earlier psychosocial stimulation intervention in rural China (Sylvia et al., 2018). Low compliance may have attenuated the effects of the intervention. To examine how the effect of the program may improve with better compliance, we estimated the dose-response relationship between the number of visits completed and the main outcomes. Specifically, we used control functions to estimate relationships between the number of completed home visits and the summary indices of child development and health. We did this first assuming a linear relationship and then allowing for a concave relationship by adding a squared term for the number of completed household visits. We instrument the number of visits with treatment assignment, the distance from the home to the nearest center of the NHC, and the interaction between these two variables. As shown in table A.7, we find up to 26 household visits (full compliance) evidence for a linear relationship between the number of home visits and both of these indices. We estimated that each completed session increased child skill development scores by 0·010 SD [95% CI 0·001–0·020] and child health scores by 0·019 SD [95% CI 0·008–0·030]. As shown in columns (2) of table A.7, we didn’t find empirical evidence for concavity in the dose-response relationships. Assuming a linear relationship up to 26 household visits, our estimates suggest that under full compliance skill development and health scores would on average have increased by 0·24 SD and 0·46 SD, respectively. These effects are larger than the estimated ITT effects (see table 3). These estimates suggest that treatment effects of the intervention could increase with improved compliance, however, the ITT effects may better reflect the effect of the intervention at scale as non-compliance would likely occur in an at-scale program. Compliance has generally been found to be higher in shorter, more intense programs than in longer, less intense ones (Yousafzai & Aboud, 2014). Moreover, it is possible that this lower compliance rate as compared to the compliance rate in Sylvia et al. (2018) resulted in part from the longer duration of home visits due to the integration of two intervention components. Future studies should analyze whether home visit duration affects compliance and, if so, whether integrated programs can be delivered in a way that maintains high levels of compliance.
Our results provide evidence in favor of integration of multiple program components in early childhood home-visiting programs. We have shown that an integrated program with both psychosocial stimulation and health promotion can lead to improved outcomes across multiple domains. More specifically, we found that the home-based integrated parenting program: (1) maintained the positive effect on cognitive development found generally in single-objective psychosocial stimulation programs and (2) simultaneously led to an improvement in health as measured by a reduction in episodes of diarrheal illness. As long as the monetary benefits of a program component exceed the incremental costs associated with it, integration of the component in an existing program may lead to substantial gains in cost-effectiveness. Considering that offices of the NHC are present in all rural areas in China, parenting training on psychosocial stimulation and health promotion would be highly scalable when integrated with the existing service infrastructure of the NHC.
Supplementary Material
Footnotes
Declaration of interests: All authors completed the ICMJE uniform disclosure form and declare no competing interests.
Data sharing
The de-identified data set and replication files are available from the Harvard Dataverse.
References
- Aboud FE, Singla DR, Nahil MI, & Borisova I (2013). Effectiveness of a parenting program in Bangladesh to address early childhood health, growth and development. Social Science & Medicine, 97, 250–258. [DOI] [PubMed] [Google Scholar]
- Aboud FE, & Yousafzai AK (2015). Global health and development in early childhood. Annual Review of Psychology, 66, 433–457. [DOI] [PubMed] [Google Scholar]
- Aboud FE, & Yousafzai AK (2019). Scaling up child psychosocial stimulation programmes for young children. Lancet Global Health, 7(3), e294–e295. [DOI] [PubMed] [Google Scholar]
- Andrew A, Attanasio O, Fitzsimons E, & Rubio-Codina M (2016). Why is multiple micronutrient powder ineffective at reducing anaemia among 12–24 month olds in Colombia? Evidence from a randomised controlled trial. SSM-population health, 2, 95–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Attanasio O, Cattan S, Fitzsimons E, Meghir C, & Rubio-Codina M (2015). Estimating the production function for human capital: Results from a randomized control trial in Colombia (NBER Working Paper No. w20965). Retrieved from https://www.nber.org/papers/w20965.
- Attanasio O, Fernández C, Fitzsimons E, Grantham-McGregor SM, Meghir C, & Rubio-Codina M (2014). Using the infrastructure of a conditional cash transfer program to deliver a scalable integrated early child development program in Colombia: cluster randomized controlled trial. BMJ, 349, g5785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Attanasio O, Meghir C, & Nix E (2015). Human capital development and parental investment in India (NBER Working Paper No. w21740). Retrieved from https://www.nber.org/papers/w21740.
- Bayley N (2006). Bayley Scales of Infant Development, 3rd edition. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Bentley ME, Wasser HM, & Creed-Kanashiro HM (2011). Responsive feeding and child undernutrition in low- and middle-income countries. Journal of Nutrition, 141, 502–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black MM, Walker SP, Fernald LC, Andersen CT, DiGirolamo AM, Lu C, … & Devercelli AE (2017). Early childhood development coming of age: science through the life course. The Lancet, 389(10064), 77–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Britto PR, Lye SJ, Proulx K, Yousafzai AK, Matthews SG, Vaivada T, … & MacMillan H (2017). Nurturing care: promoting early childhood development. The Lancet, 389(10064): 91–102. [DOI] [PubMed] [Google Scholar]
- Bundy DA, de Silva N, Horton S, Jamison DT, & Patton GC (2018). Optimizing education outcomes: High-return investments in school health for increased participation and learning. Washington, DC: World Bank. [Google Scholar]
- Dewey KG, & Adu-Afarwuah S (2008). Systematic review of the efficacy and effectiveness of complementary feeding interventions in developing countries. Maternal and Child Nutrition, 4, 4–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engle PL, Black MM, Behrman JR, De Mello MC, Gertler PJ, Kapiriri L, … & International Child Development Steering Group. (2007). Strategies to avoid the loss of developmental potential in more than 200 million children in the developing world. The Lancet; 369(9557), 229–242. [DOI] [PubMed] [Google Scholar]
- Fewtrell L, Kaufmann RB, Kay D, Enanoria W, Haller L, & Colford JM Jr. (2005). Water, sanitation, and hygiene interventions to reduce diarrhoea in less developed countries: a systematic review and meta-analysis. The Lancet Infectious Diseases, 5(1), 42–52. [DOI] [PubMed] [Google Scholar]
- Fitzsimons E, Malde B, Mesnard A, & Vera-Hernandez M (2016). Nutrition, information and household behavior: experimental evidence from Malawi. Journal of Development Economics, 122, 113–126. [Google Scholar]
- Gowani S, Yousafzai AK, Armstrong R, & Bhutta ZA (2014). Cost effectiveness of responsive stimulation and nutrition interventions on early child development outcomes in Pakistan. Annals of the New York Academy of Sciences, 1308(1), 149–161. [DOI] [PubMed] [Google Scholar]
- Grantham-McGregor SM, Cheung YB, Cueto S, Glewwe P, Richter L, Strupp B, & International Child Development Steering Group. (2007). Developmental potential in the first 5 years for children in developing countries. The Lancet, 369(9555), 60–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grantham-McGregor SM, Fernald LC, Kagawa R, & Walker S (2014). Effects of integrated child development and nutrition interventions on child development and nutritional status. Annals of the New York Academy of Sciences, 1308(1), 11–32. [DOI] [PubMed] [Google Scholar]
- Hamadani JD, Mehrin SF, Tofail F, Hasan MI, Huda SN, Baker-Henningham H, … & Grantham-McGregor SM (2019). Integrating an early childhood development programme into Bangladeshi primary health-care services: an open-label, cluster-randomised controlled trial. Lancet Global Health, 7(3): e366–e375. [DOI] [PubMed] [Google Scholar]
- Haque MR, Parr N, & Muhidin S (2019). Parents’ healthcare-seeking behavior for their children among the climate-related displaced population of rural Bangladesh. Social Science & Medicine, 226, 9–20. [DOI] [PubMed] [Google Scholar]
- Heckman JJ (2013). Giving kids a fair chance. Cambridge, MA: MIT Press. [Google Scholar]
- Heckman JJ, & Kautz T (2014). Fostering and measuring skills: interventions that improve character and cognition In Heckman JJ (ed.), The GED myth: education, achievement tests, and the role of character in American life (pp. 341–430). Chicago, IL: Univ. Chicago Press. [Google Scholar]
- Hurley KM, Yousafzai AK, & Lopez-Boo F (2016). Early childhood development and nutrition: a review of the benefits and challenges of implementing integrated interventions. Advances in Nutrition, 7(2), 357–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lassi ZS, Zahid GS, Das JK, & Bhutta ZA (2013). Impact of complementary food and education on complementary food on growth and morbidity of children less than 2 years of age in developing countries: a systematic review. BMC Public Health, 13(suppl 3), S13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lei L (2017). The impact of community context on children’s health and nutritional status in China. Social Science & Medicine, 179, 172–181. [DOI] [PubMed] [Google Scholar]
- Luby SP, Rahman M, Arnold BF, Unicomb L, Ashraf S, Winch PJ, … & Leontsini E (2018). Effects of water quality, sanitation, handwashing, and nutritional interventions on diarrhoea and child growth in rural Bangladesh: a cluster randomised controlled trial. The Lancet Global Health, 6(3), e302–e315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo R, Shi Y, Zhou H, Yue A, Zhang L, Sylvia S, … & Rozelle S (2014). Anemia and feeding practices among infants in rural Shaanxi Province in China. Nutrients, 6(12), 5975–5991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo R, Shi Y, Zhou H, Yue A, Zhang L, Sylvia S, … & Rozelle S (2015). Micronutrient deficiencies and developmental delays among infants: evidence from a cross-sectional survey in rural China. BMJ Open, 5(10): e008400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo R, Yue A, Zhou H, Shi Y, Zhang L, Martorell R, … & Sylvia S (2017). The effect of a micronutrient powder home fortification program on anemia and cognitive outcomes among young children in rural China: a cluster randomized trial. BMC Public Health, 17(1), 738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwan PJ (2012). Cost-effectiveness analysis of education and health interventions in developing countries. Journal of Development Effectiveness, 4(2): 189–213. [Google Scholar]
- Mistry KB, Minkovitz CS, Riley AW, Johnson SB, Grason HA, Dubay LC, & Guyer B (2012). A new framework for childhood health promotion: the role of policies and programs in building capacity and foundations of early childhood health. American Journal of Public Health, 102(9), 1688–1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ngure FM, Reid BM, Humphrey JH, Mbuya MN, Pelto G, & Stoltzfus RJ (2014). Water, sanitation, and hygiene (WASH), environmental enteropathy, nutrition, and early child development: making the links. Annals of the New York Academy of Sciences, 1308(1), 118–128. [DOI] [PubMed] [Google Scholar]
- Pérez-Escamilla R, & Moran VH (2017). The role of nutrition in integrated early child development in the 21st century: contribution form the Maternal and Child Nutrition journal. Maternal & Child Nutrition, 13, e12387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao N, Sun J, Wong JMS, Weekes B, Ip P, Shaeffer S, … & Lee D (2014). Early childhood development and cognitive development in developing countries: a rigorous literature review. London: Department for International Development. [Google Scholar]
- Ran T, Chattopadhyay SK, Hahn RA, & Community Preventive Services Task Force. (2016). Economic evaluation of school-based health centers: a Community Guide systematic review. American Journal of Preventive Medicine, 51(1), 129–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richter LM, Daelmans B, Lombardi J, Heymann J, Boo FL, Behrman JR, … & Bhutta ZA (2017). Investing in the foundation of sustainable development: pathways to scale up for early childhood development. Lancet, 389(10064), 103–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubio-Codina M, Araujo MC, Attanasio O, Muñoz P, & Grantham-McGregor S (2016). Concurrent validity and feasibility of short tests currently used to measure early childhood development in large scale studies. PLoS One, 11(8), e0160962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seguin M, & Zarazúa NM (2015). Non-clinical interventions for acute respiratory infections and diarrhoeal diseases among young children in developing countries. Tropical Medicine & International Health, 20(2), 146–169. [DOI] [PubMed] [Google Scholar]
- Soofi S, Cousens S, Iqbal SP, Akhund T, Khan J, Ahmed I, … & Bhutta ZA (2013). Effect of provision of daily zinc and iron with several micronutrients on growth and morbidity among young children in Pakistan: a cluster-randomised trial. Lancet, 382(9886), 29–40. [DOI] [PubMed] [Google Scholar]
- Sylvia S, Shi Y, Xue H, Tian X, Wang H, Liu Q, … & Rozelle S (2015). Survey using incognito standardized patients shows poor quality care in China’s rural clinics. Health Policy and Planning, 30(3), 322–333. [DOI] [PubMed] [Google Scholar]
- Sylvia S, Warrinnier N, Luo R, Attanasio O, Medina A, & Rozelle S (2018). From quantity to quality: delivering a home-based parenting intervention through China’s family planning cadres (LICOS Discussion Paper No. 402). Retrieved from KU Leuven LICOS website: https://feb.kuleuven.be/drc/licos/publications/discussion-papers.
- Tao SY, Cheng YL, Lu Y, Hu YH, & Chen DF (2013). Handwashing behavior among Chinese adults: a cross-sectional study in five provinces. Public Health, 127(7), 620–628. [DOI] [PubMed] [Google Scholar]
- Wang L, Liang W, Zhang S, Jonsson L, Li M, Yu C, … & Luo R (2019). Are infant/toddler developmental delays a problem across rural China? Journal of Comparative Economics, 47(2), 458–469. [Google Scholar]
- Wang L, Sun Y, Liu B, Zheng L, Li M, Bai Y, … & Rozelle S (2018). Is Infant/Toddler Anemia a Problem across Rural China? A Mixed-Methods Analysis. International Journal of Environmental Research and Public Health, 15(9), 1825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yousafzai AK, & Aboud F (2014). Review of implementation processes for integrated nutrition and psychosocial stimulation interventions. Annals of the New York Academy of Sciences, 1308(1), 33–45. [DOI] [PubMed] [Google Scholar]
- Yousafzai AK, Rasheed MA, Rizvi A, Armstrong R, & Bhutta ZA (2014). Effect of integrated responsive stimulation and nutrition interventions in the Lady Health Worker programme in Pakistan on child development, growth, and health outcomes: A cluster-randomised factorial effectiveness trial. The Lancet, 384(9950), 1282–1293. [DOI] [PubMed] [Google Scholar]
- Zelen M (1979). A new design for randomized clinical trials. New England Journal of Medicine, 300(22), 1242–45. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


