Abstract
Objective
To assess the efficacy of manual acupuncture as prophylactic treatment for acupuncture naive patients with episodic migraine without aura.
Design
Multicentre, randomised, controlled clinical trial with blinded participants, outcome assessment, and statistician.
Setting
Seven hospitals in China, 5 June 2016 to 15 November 2018.
Participants
150 acupuncture naive patients with episodic migraine without aura.
Interventions
20 sessions of manual acupuncture at true acupuncture points plus usual care, 20 sessions of non-penetrating sham acupuncture at heterosegmental non-acupuncture points plus usual care, or usual care alone over 8 weeks.
Main outcome measures
Change in migraine days and migraine attacks per four weeks during weeks 1-20 after randomisation compared with baseline (four weeks before randomisation).
Results
Among 150 randomised patients (mean age 36.5 (SD 11.4) years; 123 (82%) women), 147 were included in the full analysis set. Compared with sham acupuncture, manual acupuncture resulted in a significantly greater reduction in migraine days at weeks 13 to 20 and a significantly greater reduction in migraine attacks at weeks 17 to 20. The reduction in mean number of migraine days was 3.5 (SD 2.5) for manual versus 2.4 (3.4) for sham (adjusted difference −1.4, 95% confidence interval −2.4 to −0.3; P=0.005) at weeks 13 to 16 and 3.9 (3.0) for manual versus 2.2 (3.2) for sham (adjusted difference −2.1, −2.9 to −1.2; P<0.001) at weeks 17 to 20. At weeks 17 to 20, the reduction in mean number of attacks was 2.3 (1.7) for manual versus 1.6 (2.5) for sham (adjusted difference −1.0, −1.5 to −0.5; P<0.001). No severe adverse events were reported. No significant difference was seen in the proportion of patients perceiving needle penetration between manual acupuncture and sham acupuncture (79% v 75%; P=0.891).
Conclusions
Twenty sessions of manual acupuncture was superior to sham acupuncture and usual care for the prophylaxis of episodic migraine without aura. These results support the use of manual acupuncture in patients who are reluctant to use prophylactic drugs or when prophylactic drugs are ineffective, and it should be considered in future guidelines.
Trial registration
Clinicaltrials.gov NCT02765581.
Introduction
The latest Global Burden of Disease Study showed that 1.25 billion people had migraine in 2017.1 Migraine was responsible for 45.1 million years of life lived with disability.2 In the 15-49 year age group, migraine was the top cause of life lived with disability.3 Although some authors have suggested that prophylactic drugs should be recommended for migraineurs who have at least four headache days per month, only 13% of patients reported current use of preventive drugs.4 Ineffectiveness of and/or contraindications to migraine medication affect 10-15% of people with migraine.5 Hence, a need exists to investigate non-drug interventions.
Acupuncture has emerged as a prophylactic treatment for migraine because of its potential efficacy.6 7 8 Clinically, two acupuncture interventions are widely used: manual acupuncture and electrical acupuncture. Manual acupuncture is commonly used by traditional acupuncturists and is highly effective for pain relief.9 Besides insertion of penetrating needles into specific acupuncture points, manual manipulation (that is, intermittent rotation as well as lift and thrust) of the needle may enhance its clinical benefit.10 11 However, clinical evidence for the benefit of manual acupuncture for migraine prophylaxis remains scarce. Several randomised clinical trials found no differences between manual and sham acupuncture.12 13 14 15 16 These negative results might be ascribed to inappropriate placebo control settings.
Blinding is challenging in trials of non-drug treatments. An appropriate placebo acupuncture design should be both physiologically inert and indistinguishable from true acupuncture. So far, only one randomised clinical trial of acupuncture in migraine has reported successful blinding.15 Furthermore, some authors have suggested that sham acupuncture interventions were not totally inert, often being associated with moderately large non-specific effects.17 18 19 This could make detection of additional specific effects of manual acupuncture difficult. In particular, sham acupuncture involving penetrating needles should be avoided in clinical trials.20 However, penetrating sham acupuncture has been commonly used in previous randomised clinical trials in migraine.12 13 14 15 16
Therefore, we designed a randomised clinical trial among patients with migraine who were naive to acupuncture, using non-penetrating sham control and assessment of blinding to determine the efficacy of manual acupuncture and quantify the true placebo response in the prophylaxis of episodic migraine without aura.
Methods
Study design
This randomised, single blind, three arm clinical trial was conducted in seven centres in China between 5 June 2016 and 15 November 2018. The protocol and the statistical analysis plan are available in appendix 1. The total trial period was 24 weeks, including four weeks of baseline assessment, eight weeks of treatment after randomisation, and 12 weeks of follow-up. We obtained written informed consent from each patient before randomisation.
Participants
A neurologist made the diagnosis of episodic migraine without aura on the basis of the International Classification of Headache Disorders, 3rd edition β version (ICHD-3β).21 Other inclusion criteria were age between 15 and 65 years, history of migraine without aura for more than 12 months, initial onset of migraine before the age of 50 years, between two and eight migraine attacks during the baseline phase, naivety to acupuncture, and ability to give informed consent. Exclusion criteria included all other types of primary and secondary headaches, history of a clinically significant disorder (for example, severe mental illness), pregnancy or breast feeding, and non-adherence to the baseline diary. In addition, all patients were instructed not to take any other analgesics and to avoid starting other interventions.
Randomisation and masking
After the baseline assessment, an independent investigator randomised eligible patients in a 2:2:1 ratio to receive manual acupuncture, sham acupuncture, or usual care. We used the 2:2:1 ratio to facilitate recruitment and increase patients’ adherence. Treatments were allocated in a centralised manner via an interactive web response system with stratification by centre and a block size of five. To maintain blinding in patients, outcome assessors, and statisticians, the allocation sequence was concealed until the end of the study.
Study interventions
Fourteen licensed acupuncturists delivered treatments. They each had more than five years of clinical experience and attended centralised training before recruitment. All patients received 20 sessions of 30 minute acupuncture treatments or usual care over eight weeks. They were treated every other day to fulfil a 10 session treatment course and received another 10 session course after a nine day break. In both the manual and sham acupuncture group, acupuncture treatment began after randomisation. In the usual care group, patients received acupuncture for free after waiting 24 weeks. Details of acupuncture (location of acupuncture points/non-acupuncture points, depth of insertion) are shown in tables 1 and 2 of appendix 1.
Acupuncturists applied manual acupuncture at 10 obligatory acupoints, included bilateral L14, LR3, EX-HN5, GB20, and GB8. Additional acupoints were selected on the basis of meridian diagnosis and the patient’s symptoms: bilateral ST8 for Yangming meridian headache, BL10 for Taiyang meridian headache, and DU20 for Jueying meridian headache. Streitberger acupuncture needles (0.30 mm in diameter and 30 mm in length) were used. After sterilisation, the sharp needles were inserted into the deep tissue layers of acupoints. Acupuncturists then tried to elicit acupuncture de-qi sensation by the manual manipulation of needles. Over a 30 minute period, manual manipulation for each acupoint lasted 10 seconds and was repeated four times with intervals of 10 minutes.
Non-penetrating sham acupuncture was performed at four bilateral non-acupuncture points, which were all located on the back and in different segments from the headache area. After sterilisation, Streitberger placebo needles with blunt tip were used.22 When they were fixed on the skin through plastic rings, patients felt a pricking sensation, simulating a puncture of the skin. However, instead of penetrating the skin, the needles retracted up into the shaft when they were pressed against the skin. We formulated and followed standardised step-by-step instructions and operations to use the same rituals in the manual acupuncture and sham acupuncture groups as far as possible (appendix 2).
In accordance with the migraine guidelines developed by the Canadian Headache Society Prophylactic Guidelines Development Group in 2012,23 we provided usual care to all three groups in terms of lifestyle changes and migraine self-management. We taught patients about lifestyle factors that may contribute to an increased frequency of migraine, identifying migraine triggers or precipitants through the keeping of a detailed headache diary, pacing, pain communication, sleep hygiene, and regular exercise. In case of severe pain (visual analogue score >8), diclofenac sodium enteric coated tablets (25 mg/tablet; maximal tolerated dose 200 mg/day) were allowed as a rescue medication.
Outcome measures
Independent research assistants supervised patients to complete their headache diaries in paper and pencil format from baseline to week 20 and evaluated their outcomes. The primary outcomes were change in the mean number of migraine days and migraine attacks per four week cycle during weeks one to 20 after randomisation compared with baseline (the four weeks before randomisation). Secondary outcomes included the proportion of patients achieving at least a 50% reduction in the mean number of migraine days or migraine attacks during weeks 17 to 20 and changes in the severity of migraine as measured by a visual analogue scale, the Migraine-Specific Quality-of-Life Questionnaire (MSQ),24 the Pittsburgh Sleep Quality Index (PSQI),25 the Migraine Disability Assessment Score (MIDAS),26 the Beck Anxiety Inventory (BAI) scale,27 the Beck Depression Inventory II (BDI-II) scale,28 and the mean dose of used rescue medication from baseline to week 20. We also measured patients’ expectations of of positive outcomes from acupuncture by using the Acupuncture Expectancy Scale.29 At the end of the study, we determined the maintenance of blinding of patients by asking them whether they thought the needles had penetrated the skin. Patients recorded adverse events after each treatment, including bleeding, subcutaneous haemorrhage, serious pain, palpitation, fainting, and local infection.
Statistical analyses
On the basis of a pilot study, we anticipated a mean difference of 1.8 (SD 2.8) days and 1.2 (1.8) attacks for manual versus sham acupuncture and a difference of 2.2 (2.8) days and 1.5 (1.8) attacks for manual acupuncture versus usual care. To drive all the primary hypothesis tests, we used PROC POWER in SAS to calculate that a sample of 135 evaluable patients (54 in manual acupuncture, 54 in sham acupuncture, and 27 in usual care) would be needed to provide 90% power at a two sided significance level of 5%. Therefore, we planned to recruit 150 patients into this study, with an anticipated 10% dropout rate.
We did efficacy analyses in the full analysis set, which included all randomised patients who received at least one session of treatment and had at least one efficacy measure. We imputed missing data by using the last observation carried forward method.30 We did sensitivity analyses in the per protocol set, which included all randomised patients who had no major protocol deviation. We did safety analyses in the safety set, which included all randomised patients who received at least one session of acupuncture.
We assessed the poolability of treatment effects across centres by including an interaction term of treatment group by centre in the model for the primary analysis. If P values associated with the interaction term of both primary endpoints were greater than 0.15,31 the treatment effect was homogenous across centres.
We presented continuous variables as the mean with standard deviation or median and interquartile range. For tests across groups, we used analysis of variance or the Kruskal-Wallis test when relevant. We described categorical variables as numbers and percentages and used the χ2 test or Fisher’s exact test. For comparisons of the primary endpoints across the groups, we used analysis of covariance with the baseline migraine days or migraine attacks adjusted. Superiority of manual acupuncture over sham acupuncture or usual care could be claimed only when both co-primary endpoints were statistically significant. We used a fixed sequence procedure for multiple comparisons among groups, which would not inflate the type I error, and comparisons were made with an α value of 0.05. We also evaluated multivariate adjusted treatment effects across the groups on the basis of a linear mixed effects model. For the secondary endpoints, we made pairwise multiple comparisons on the basis of Bonferroni adjusted P values and confidence intervals, if a significant difference was noted across the groups.
An independent statistician used SAS statistical software for all statistical analyses. For both continuous and categorical variables, 95% confidence intervals were calculated as appropriate. All the statistical comparisons were two sided with P<0.05 considered as significant.
Patient and public involvement
No patients were involved in the design or conduct of the study, in setting the research question, or in determining the outcome measures of this study, nor did they have any input on data analysis, interpretation, or writing up of results. Results of the trial will be shared with all participants by web or email.
Results
Study participants
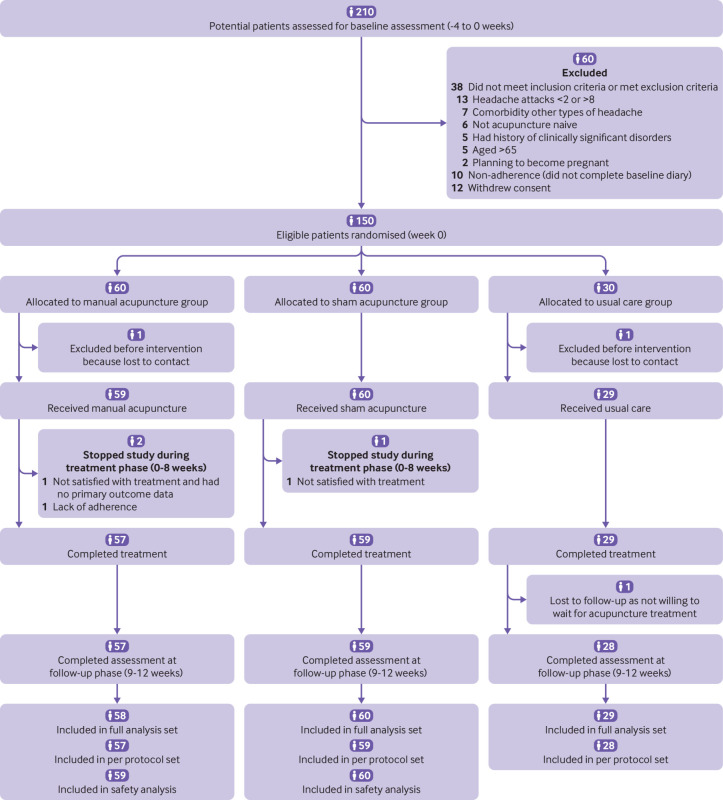
Between 5 June 2016 and 15 November 2018, we screened 210 patients, of whom 150 were randomised (fig 1). The main reason for exclusion was not meeting the inclusion criterion of between two and eight migraine attacks during the baseline phase (table A in appendix 3). The baseline characteristics of all randomised patients were well balanced among the three groups (table 1). Similar baseline characteristics were observed in the full analysis set population (table B in appendix 3).
Fig 1.
Flowchart showing trial group assignments, loss to follow-up, treatment completion, and protocol deviations
Table 1.
Baseline characteristics of randomised population. Values are mean (SD) unless stated otherwise
| Characteristics | Manual acupuncture (n=60) | Sham acupuncture (n=60) | Usual care (n=30) |
|---|---|---|---|
| Age, years | 36.6 (12.0) | 36.0 (10.9) | 37.3 (11.7) |
| No (%) women | 47 (78) | 50 (83) | 26 (87) |
| Median (IQR) body mass index | 20.4 (19.5-23.1) | 22.0 (20.3-23.4) | 20.8 (19.5-22.4) |
| Median (IQR) disease duration, years, | 10.0 (5.0-19.5) | 10.0 (6.0-14.0) | 16.5 (7.8-23.0) |
| Accompanying symptoms: | |||
| No (%) nausea or vomiting | 53 (88) | 51 (85) | 25 (83) |
| No (%) photophobia or phonophobia | 52 (87) | 52 (87) | 23 (77) |
| Patient personality: | |||
| Neuroticism | 31.8 (7.1) | 31.9 (6.6) | 31.3 (7.1) |
| Extraversion | 37.4 (7.0) | 38.0 (6.6) | 37.0 (6.4) |
| Openness | 37.6 (4.9) | 37.4 (4.8) | 35.9 (2.8) |
| Agreeableness | 43.2 (4.6) | 43.1 (4.9) | 43.6 (5.2) |
| Conscientiousness | 41.2 (5.6) | 41.8 (6.2) | 41.5 (5.5) |
| No (%) chronic migraine | 1 (2) | 2 (3) | 0 (0) |
| Acupuncture Expectancy Scale score | 10.9 (3.7) | 11.1 (3.5) | NA |
| Days with migraine | 5.8 (2.6) | 6.3 (3.8) | 5.8 (3.0) |
| No of migraine attacks | 3.8 (1.4) | 4.1 (2.6) | 3.9 (1.7) |
| Mean VAS score | 5.1 (1.3) | 5.3 (1.3) | 5.2 (1.8) |
| Migraine-Specific Quality-of-Life Questionnaire: | |||
| Role restrictive subscale | 55.2 (17.6) | 54.4 (15.5) | 56.0 (15.0) |
| Role preventive subscale | 60.6 (23.3) | 59.9 (19.5) | 64.0 (19.0) |
| Emotional subscale | 61.6 (23.3) | 65.3 (20.3) | 62.9 (21.6) |
| Pittsburgh Sleep Quality Index | 5.7 (2.7) | 5.6 (2.7) | 5.3 (3.5) |
| Median (IQR) Migraine Disability Assessment Score | 27.5 (12.0-49.8) | 33.5 (15.3-57.3) | 27.5 (13.8-44.8) |
| Median (IQR) doses of rescue medication | 0.0 (0.0-1.8) | 0.0 (0.0-3.5) | 0.0 (0.0-2.0) |
| Median (IQR) Beck Depression Inventory II | 6.5 (3.0-13.0) | 7.0 (2.3-14.0) | 7.0 (1.0-13.0) |
| Median (IQR) Beck Anxiety Inventory | 10.0 (4.0-15.0) | 7.5 (4.0-14.0) | 7.0 (3.8-9.5) |
IQR=interquartile range; NA=not applicable; VAS=visual analogue scale.
After randomisation, six (4%) patients were lost to follow-up (three in the manual acupuncture group, one in the sham acupuncture group, and two in the usual care group; P=0.3025, χ2 test). Of these patients, three were lost without one primary outcome measure and another three did not complete all the visits. Therefore, 147 patients were included in the full analysis set and 144 in the per protocol set.
Primary outcomes
Table 2 and figure 2 show the primary analyses. The reduction of migraine days and migraine attacks per four weeks from baseline was significantly greater in the manual acupuncture group than in the usual care group during weeks 1 to 20. Compared with sham acupuncture, manual acupuncture resulted in a significantly greater reduction in migraine days during weeks 13 to 20, with a group difference of −1.4 (95% confidence interval −2.4 to −0.3; P=0.005) days at weeks 13 to 16 and −2.1 (−2.9 to −1.2; P<0.001) days at weeks 17 to 20, and a significantly greater reduction in migraine attacks at weeks 17 to 20, with a group difference of −1.0 (−1.5 to −0.5; P<0.001) attacks. Sham acupuncture also resulted in a significantly greater reduction in migraine attacks during weeks 5 to 20 compared with usual care. We observed similar results in the per protocol analysis population (table C in appendix 3). In addition, we developed mixed effects models including participants, centres, acupuncturists, baseline, study visits, treatment groups, and the interaction term of treatment groups by study visits, the results of which were consistent with those of the primary analyses (table D in appendix 3). The poolability of both primary efficacy endpoints across centres was verified (P values for the interaction effects were >0.15).
Table 2.
Primary outcome measurements of full analysis set population. Values are mean (SD) unless stated otherwise
| Time point | Manual acupuncture (n=58) | Sham acupuncture (n=60) | Usual care (n=29) | P value* | Pairwise comparisons—mean (95% CI) | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Manual v sham | P value* | Manual v usual care | P value* | Sham v usual care | P value* | |||||
| Change from baseline in mean number of days with migraine | ||||||||||
| Weeks 1-4 | −2.2 (2.0) | −1.6 (3.0) | −0.7 (2.9) | 0.003 | −0.9 (−1.8 to 0.0) | 0.052 | −1.5 (−2.5 to −0.4) | 0.004 | −0.6 (−1.7 to 0.5) | 0.589 |
| Weeks 5-8 | −3.1 (2.6) | −2.7 (3.6) | −1.3 (2.5) | 0.002 | −0.7 (−1.6 to 0.2) | 0.198 | −1.7 (−2.8 to −0.5) | 0.001 | −1.0 (−2.1 to 0.2) | 0.119 |
| Weeks 9-12 | −3.5 (2.6) | −2.9 (3.8) | −1.3 (2.7) | <0.001 | −1.0 (−2.0 to 0.1) | 0.077 | −2.1 (−3.4 to −0.8) | <0.001 | −1.1 (−2.4 to 0.1) | 0.100 |
| Weeks 13-16 | −3.5 (2.5) | −2.4 (3.4) | −1.0 (2.4) | <0.001 | −1.4 (−2.4 to −0.3) | 0.005 | −2.4 (−3.7 to −1.2) | <0.001 | −1.1 (−2.3 to 0.2) | 0.136 |
| Weeks 17-20 | −3.9 (3.0) | −2.2 (3.2) | −1.4 (2.7) | <0.001 | −2.1 (−2.9 to −1.2) | <0.001 | −2.4 (−3.5 to −1.4) | <0.001 | −0.4 (−1.4 to 0.7) | 0.495 |
| Change from baseline in mean number of migraine attacks | ||||||||||
| Weeks 1-4 | −1.1 (1.3) | −1.0 (2.5) | −0.2 (1.5) | 0.032 | −0.3 (−0.9 to 0.3) | 0.643 | −0.8 (−1.6 to −0.1) | 0.026 | −0.5 (−1.3 to 0.2) | 0.305 |
| Weeks 5-8 | −1.8 (1.4) | −1.7 (2.5) | −0.7 (1.3) | 0.002 | −0.3 (−0.9 to 0.2) | 0.526 | −1.0 (−1.7 to −0.4) | <0.001 | −0.7 (−1.4 to 0.0) | 0.032 |
| Weeks 9-12 | −1.9 (1.3) | −1.8 (2.7) | −0.4 (1.3) | <0.001 | −0.4 (−1.0 to 0.2) | 0.410 | −1.5 (−2.3 to −0.8) | <0.001 | −1.1 (−1.9 to −0.4) | 0.001 |
| Weeks 13-16 | −2.1 (1.5) | −1.8 (2.7) | −0.7 (1.3) | <0.001 | −0.6 (−1.2 to 0.1) | 0.092 | −1.3 (−2.1 to −0.6) | <0.001 | −0.8 (−1.5 to 0.0) | 0.043 |
| Weeks 17-20 | −2.3 (1.7) | −1.6 (2.5) | −0.4 (1.3) | <0.001 | −1.0 (−1.5 to −0.5) | <0.001 | −1.8 (−2.4 to −1.2) | <0.001 | −0.8 (−1.4 to −0.2) | 0.008 |
P values, differences, and confidence intervals were based on analysis of covariance adjusted for days with migraine (or number of migraine attacks) at baseline. According to fixed sequence procedure planned for primary analyses, pairwise comparisons at weeks 17-20 were made at nominal α level without further adjustment. For visits other than weeks 17-20, multiple pairwise comparisons were adjusted by Bonferroni approach.
Fig 2.
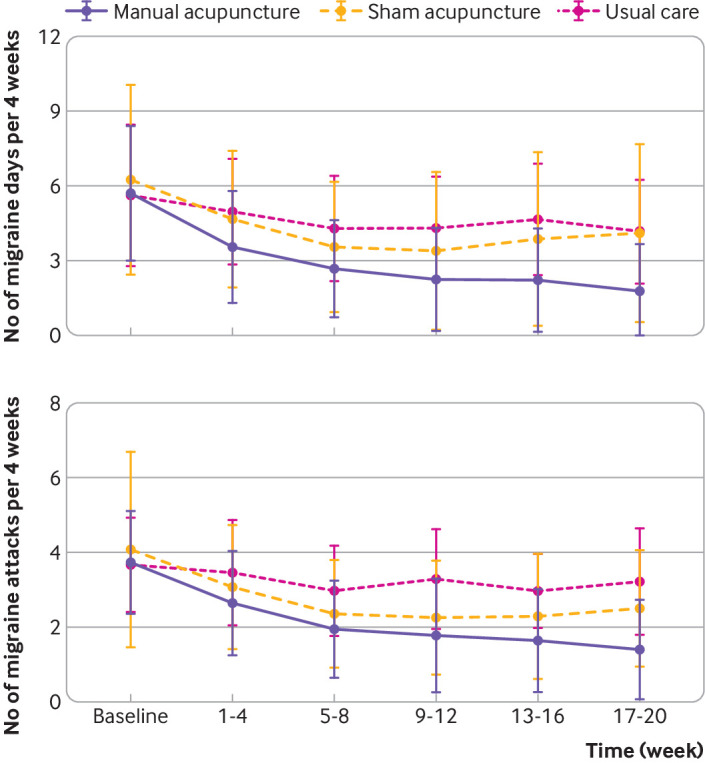
Primary outcomes throughout trial. Top: number of migraine days per 4 weeks through study period. Bottom: frequency of migraine attacks per 4 weeks through study period
Secondary outcomes
Table 3 summarises the secondary analyses. Overall, the responder rates in the manual acupuncture group were significantly higher than in the two control groups during weeks 17 to 20. All subscales of the Migraine-Specific Quality-of-Life Questionnaire were improved significantly more in the manual acupuncture group than in the two control groups at weeks 20. The visual analogue scale showed a greater reduction in score for the manual acupuncture group than for the two control groups at weeks 20.
Table 3.
Secondary outcome measurements of full analysis set population
| Time point | Manual acupuncture (n=58) | Sham acupuncture (n=60) | Usual care (n=29) | P value* | Pairwise comparison | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Manual v sham | P value* | Manual v usual care | P value* | Sham v usual care | P value* | |||||||
| Proportion of participants with ≥50% reduction in number of migraine days (%) | ||||||||||||
| Weeks 17-20 | 82.5 | 45.8 | 17.9 | <0.001 | 36.7 (17.0 to 56.4) | <0.001 | 64.6 (43.5 to 85.7) | <0.001 | 27.9 (4.6 to 51.2) | 0.012 | ||
| Proportion of participants with ≥50% reduction in number of migraine attacks (%) | ||||||||||||
| Weeks 17-20 | 78.9 | 44.1 | 14.3 | <0.001 | 34.9 (14.7 to 55.0) | <0.001 | 64.7 (44.2 to 85.1) | <0.001 | 29.8 (7.6 to 51.9) | 0.004 | ||
| Mean (SD) change from baseline in visual analogue scale | ||||||||||||
| Weeks 20 | −2.2 (2.5) | −0.9 (1.9) | −0.0 (1.4) | <0.001 | −1.3 (−2.2 to −0.3) | 0.005 | −2.1 (−3.3 to −1.0) | <0.001 | −0.9 (−2.0 to 0.3) | 0.224 | ||
| Mean (SD) change from baseline in MSQ, role restrictive subscale | ||||||||||||
| Weeks 20 | 24.4 (21.4) | 12.8 (16.0) | 5.8 (14.2) | <0.001 | 11.6 (3.5 to 19.8) | 0.002 | 18.6 (8.5 to 28.7) | <0.001 | 7.0 (−3.1 to 17.0) | 0.285 | ||
| Mean (SD) change from baseline in MSQ, role preventive subscale | ||||||||||||
| Weeks 20 | 22.5 (25.1) | 10.1 (14.1) | 4.5 (15.5) | <0.001 | 12.5 (3.7 to 21.2) | 0.002 | 18.1 (7.2 to 29.0) | <0.001 | 5.6 (−5.2 to 16.4) | 0.630 | ||
| Mean (SD) change from baseline in MSQ, emotional subscale | ||||||||||||
| Weeks 20 | 19.5 (26.8) | 8.4 (19.0) | 8.8 (20.9) | 0.020 | 11.2 (0.9 to 21.4) | 0.027 | 10.7 (−2.0 to 23.4) | 0.129 | −0.4 (−13.1 to 12.2) | >0.999 | ||
| Mean (SD) change from baseline in global score of PSQI | ||||||||||||
| Weeks 20 | −1.8 (2.3) | −0.7 (2.5) | −0.1 (2.6) | 0.007 | −1.1 (−2.2 to 0.0) | 0.058 | −1.7 (−3.0 to −0.3) | 0.011 | −0.6 (−2.0 to 0.8) | 0.894 | ||
| Median (IQR) change from baseline in score of MIDAS | ||||||||||||
| Weeks 20 | −15.0 (−36.0-−5.0) | −6.0 (−30.0-2.0) | −0.5 (−16.0-6.5) | 0.007 | −8.0 (−17.0 to 2.0) | 0.139 | −14.0 (−28.0 to −3.0) | 0.006 | −6.0 (−22.0 to 4.0) | 0.523 | ||
| Median (IQR) change from baseline in doses of rescue medication | ||||||||||||
| Weeks 17-20 | 0.0 (−1.0-0.0) | 0.0 (−1.0-0.0) | 0.0 (−1.5-0.0) | 0.745 | NA | NA | NA | NA | NA | NA | ||
| Median (IQR) change from baseline in BDI- II | ||||||||||||
| Weeks 20 | −2.0 (−6.0-0.0) | −1.0 (−5.0-1.0) | 0.0 (−2.5-1.0) | 0.081 | NA | NA | NA | NA | NA | NA | ||
| Median (IQR) change from baseline in BAI | ||||||||||||
| Weeks 20 | −4.0 (−8.0-0.0) | −1.0 (−5.0-1.0) | 0.0 (−3.5-1.5) | 0.005 | −2.0 (−5.0 to 0.0) | 0.051 | −4.0 (−7.0 to −1.0) | 0.007 | −1.0 (−4.0 to 1.0) | 0.980 | ||
BAI=Beck Anxiety Inventory; BDI-II=Beck Depression Inventory II; IQR=interquartile range; MIDAS=Migraine Disability Assessment Scores; MSQ=Migraine-Specific Quality-of-Life Questionnaire; NA=not applicable; PSQI=Pittsburgh Sleep Quality Index.
Pairwise comparison include differences in means, medians, and proportions and corresponding confidence intervals. For continuous variables, analysis of variance or Kruskal-Wallis test was used for comparisons among treatment groups. If Kruskal-Wallis test was significant, pairwise comparisons were made using Wilcoxon rank sum test. Difference in median is estimated on basis of Hodges-Lehmann estimator of location shift. Asymptotic (Moses) confidence intervals are provided. For categorical variables, linear probability model was used for comparisons among treatment groups. For all pairwise comparisons, P values and confidence intervals were adjusted by Bonferroni approach.
The total scores on the Pittsburgh Sleep Quality Index and Migraine Disability Assessment Score were significantly lower in the manual acupuncture group than in the usual care group at week 20. However, we found no significant difference in these scores between manual acupuncture and sham acupuncture. We also found no significant difference in the mean dose of rescue medication or in Beck Anxiety Inventory and Beck Depression Inventory II scores among the three groups at week 20.
At the end of the study, we assessed the credibility of blinding of treatment. We found no significant difference between the manual acupuncture and sham acupuncture groups for patients’ ability to correctly guess their allocation status (P=0.891) (table E in appendix 3).
Adverse events
In the manual acupuncture group, five (8%) patients reported at least one acupuncture related adverse event compared with no patients in the sham acupuncture group. One patient withdrew from the study because of an adverse event. No patients in either the manual or sham acupuncture group had severe adverse events (table F in appendix 3).
Discussion
In this study in acupuncture naive patients with episodic migraine without aura, 20 sessions of manual acupuncture produced a relatively long lasting reduction in migraine days and migraine attacks compared with sham acupuncture and usual care. We found that, compared with the usual care group, both the reductions in migraine days and migraine attacks per four week period from baseline in the manual acupuncture group were significantly larger from the first four week period after the start of treatment, and the significant reductions lasted until the last four week period of follow-up (weeks 17-20), with an apparent increasing trend. Compared with the usual care group, only in migraine attacks per four week period from baseline did the sham acupuncture group show significant reductions from the second four week period after treatment to the last four week period of follow-up. In the last four week period, that reduction fell a little. In comparisons between the manual acupuncture group and the sham acupuncture group, reductions in migraine days were significantly larger in the manual group at weeks 13-16 and 17-20, and reductions in migraine attacks were significantly larger in the manual group at weeks 17-20. Overall, the therapeutic effects in the manual acupuncture group occurred earlier, were larger, and might last longer.
Comparison with other studies
The latest Cochrane meta-analysis,32 published in 2016, found that up to both eight weeks/two months and three to four months after randomisation, acupuncture was associated with a small but statistically significant reduction in migraine attacks compared with sham. The effect size was −0.35 (95% confidence interval −0.57 to −0.13) at up to eight weeks/two months after randomisation and −0.32 (−0.53 to −0.10) at up to three to four months after randomisation. Since then, results have been published for only one randomised clinical trial.30 It found that electrical acupuncture resulted in a long term reduction in migraine attacks. At week 16 after randomisation, a greater reduction was observed in the true electrical acupuncture group than in the sham acupuncture group (difference of 1.1 (0.4 to 1.9) attacks; P=0.002) and in the true electrical acupuncture group than the no acupuncture group (difference of 1.8 (1.1 to 2.5) attacks; P<0.001). The effect size for manual acupuncture over sham acupuncture observed in our study was similar to the effect size seen with electrical acupuncture,30 but larger than the effect size seen in the latest Cochrane meta-analysis.32 We also updated the meta-analysis to include our results (appendix 4). Additionally, the effect size for manual acupuncture was larger than the effect size seen with prophylactic drugs, such as monthly subcutaneous injections of fremanezumab (225 mg or 675 mg) or galcanezumab (120 mg or 300 mg).33 34
However, our findings are not completely consistent with those of several randomised clinical trials,12 13 14 15 16 which found no significant differences between true acupuncture and sham acupuncture in reducing migraine headaches. The inconsistency might be driven predominantly by differences in treatments received by the control group.
Comparison between manual and electrical acupuncture
In acupuncture practice, manual acupuncture and electrical acupuncture are the two most common interventions for the treatment of pain conditions. Manual acupuncture emphasises the occurrence of “de-qi” feelings, which can be induced by proper and effective manual manipulation of the needle. The intensity of de-qi feelings plays a key role in the analgesic effects of manual acupuncture.35 The importance of manipulation of the needle is no less than that of the selection of the appropriate acupoint.36 The effects of electrical acupuncture depend on current parameters (frequency, intensity, and duration of pulses). Different manual manipulations or different electrical parameters may produce different therapeutic effects. The peripheral and central mechanisms for pain relief produced by manual acupuncture and electrical acupuncture are homologous, but some differences exist. The effects of manual acupuncture may be mediated by all types of afferents, whereas the effects of electrical acupuncture might be preferentially mediated by Aβ and parts of Aδ type afferents.9 In addition, subtle differences exist between the areas of the brain activated by manual and electrical acupuncture.37
So far, only a few small trials for several conditions have directly compared the effects of manual and electrical acupuncture.38 39 40 41 42 The findings of these studies were inconsistent and inconclusive. The choice of different manual manipulations or different electrical parameters may need to be based on a specific disease or condition and should be guided by more high quality randomised controlled trials.
Strengths and limitations of study
An advantage of this trial is the design of a reasonable sham comparator. Previous acupuncture research has often used penetrating sham acupuncture, involving needling non-acupuncture points, needling irrelevant acupuncture points, or superficial needling.43 44 However, whether the needle is inserted into an acupuncture point or a non-acupuncture point, it could produce a physiological effect.44 This is in part due to the activation of the pain inhibiting system in the spinal cord and diffuse noxious inhibitory controls.45 46 47 In addition, sham acupuncture applied at points beside the real acupoints might be an active control, because the area of the acupoint could be enlarged by increased expression of nociceptive substances during various pain conditions.48 In this study, we applied non-penetrating sham acupuncture at heterosegmental non-acupuncture points, thereby avoiding segmental analgesia and minimising any physiological effect in the sham acupuncture group.
Another strength of this trial is the successful blinding. Previous trials lacked assessment of blinding or had ineffective blinding,12 13 14 16 so comparisons between true acupuncture and sham acupuncture might be biased by unsuccessful blinding. Ideal blinding should be psychologically credible yet physiologically inert. To ensure successful blinding, we recruited acupuncture naive patients, used non-penetrating needles as the control, and designed the same procedures to perform the same rituals as far as possible in the manual and sham acupuncture groups. These factors made the sham acupuncture as close to a real placebo as possible. At the end of the study, we asked patients to guess whether they thought the needles penetrated the skin. Satisfyingly, we found no significant difference between the two treatment groups in patients’ ability to correctly guess their allocation status. Successful blinding showed the reliability of the difference between manual acupuncture and sham acupuncture, as well as between sham acupuncture and usual care. Furthermore, successful blinding increased the adherence of patients, especially those allocated to the sham acupuncture group. Only one patient in the sham acupuncture group was lost to follow-up.
The study does, however, have limitations. Firstly, the lack of baseline prophylaxis is not typical, but the latest meta-analysis indicated that acupuncture reduced the frequency of migraine significantly more than did drug prophylaxis and was less likely to lead to dropout due to adverse effects and to reporting of adverse effects.32 In addition, we should respect the opinions of patients who are reluctant to use drug treatment; the decision to treat with drugs and the choice of a prophylactic drug should be made together with the patient.49 Secondly, the timeframe of this study may be not have been long enough to see a long lasting effect, although we observed that the treatment effects of manual acupuncture could persist for 12 weeks after treatment. In the future, trials with longer follow-up periods are needed to assess how long the effects of manual and sham acupuncture last.
Clinical relevance
A considerable number of patients do not respond well to drug treatment, cannot tolerate the adverse effects of drugs, or have contraindications, which can lead to low adherence, chronification of headache, and acute drug overuse.50 Our results show that acupuncture can be recommended as an effective alternative treatment. Although sham acupuncture produced a minor benefit in reducing migraine attacks, the differences between manual acupuncture and sham acupuncture support the specific effects of manual acupuncture. On the basis of our results, clinical acupuncturists should pay careful attention to the specific components of acupuncture, including acupuncture points, needle manipulation, and acupuncture sensations, and the non-specific effects of acupuncture (acupuncture ritual or expectation for efficacy51 52) should also not be neglected in clinical practice. In randomised controlled trials of acupuncture, the sham acupuncture group should not use penetrating needles.
Conclusion and policy implications
Among acupuncture naive patients with episodic migraine without aura, treatment with manual acupuncture, compared with sham acupuncture or usual care, resulted in a significantly greater reduction in the frequency of migraine days and migraine attacks. Acupuncture can be recommended as a prophylactic treatment when updating the guidelines and insurance coverage for migraine and its related substance misuse. When discussing prophylactic treatment strategies with patients, clinicians should provide them with information about acupuncture as an option.
What is already known on this topic
Clinical evidence for the benefit of manual acupuncture in migraine prophylaxis remains scarce
Several recent clinical trials found that manual acupuncture was superior to no acupuncture
Comparisons between manual acupuncture and sham acupuncture found only minor or even no differences
What this study adds
Manual acupuncture was more effective than sham acupuncture and usual care in reducing migraine headaches
Acknowledgments
We thank Fengcai Zhu and Jingxin Li of the Jiangsu Provincial Center for Disease Control and Prevention, for guidance of the statistical analyses. We also thank the research assistants, acupuncturists, supporters of this study, and all of the patients who participated in this study.
Web extra.
Extra material supplied by authors
Appendix 1: protocol
Appendix 2: acupuncture ritual
Appendix 3: supplementary tables
Appendix 4: meta-analysis
Contributors: SX, LY, and XL contributed equally to the study. SX, LY, XL, HW, and WW conceived and designed the study. SX, LY, XL, HW, and WW had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. SX, LY, and XL drafted the manuscript. SX, LY, XL, MW, GC, QZ, ZZ, JS, HJ, HW, and WW contributed to the acquisition, analysis, and interpretation of data. All authors contributed to the critical revision of the manuscript for important intellectual content and gave final approval of the version to be published. WL did the statistical analysis. HW and WW obtained funding. GC, ZZ, JS, HJ, GH, FL, HW, and WW provided administrative, technical, or material support. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. HW and WW supervised the study and are the guarantors.
Funding: This study was supported by a grant from the National Natural Science Foundation of China (61327902), and a project grant from Hubei University of Chinese Medicine/Hubei Provincial Collaborative Innovation Center of Preventive Treatment by Acupuncture and Moxibustion. Study sponsors were not involved in study design, data interpretation, writing the article, or the decision to submit the article for publication.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: funding for the submitted work as described above; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: This study was approved by the Clinical Trial Ethics Committee of Tongji Medical College, Huazhong University of Science and Technology (2016S009), the Medical Ethics Committee of Wuhan No.1 Hospital (WuWeiYiYuanLunShen[2016]14), the Ethics Committee of Hubei Province Hospital of Traditional Chinese Medicine (HBZY2016-C25-01), the Ethics Committee of Xiangyang No.1 Hospital (YN20171220), the Ethics Committee of The Second Hospital of Huangshi (HEYLWJY1701), and the Ethics Committee of Hubei University of Chinese Medicine ([2018] IEC No. 2). The trial was overseen by an independent trial steering committee and data monitoring and ethics committee. All patients gave written informed consent.
Data sharing: The raw trial data after de-identification can be shared on individual request to the corresponding author at wwang@vip.126.com.
Transparency: The lead author affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Dissemination to participants and related patient and public communities: Participants will be informed of the results of the study by telephone. Dissemination to the public will be achieved through media outreach.
References
- 1. GBD 2017 Disease and Injury Incidence and Prevalence Collaborators Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392:1789-858. 10.1016/S0140-6736(18)32279-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. GBD 2016 Headache Collaborators Global, regional, and national burden of migraine and tension-type headache, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 2018;17:954-76. 10.1016/S1474-4422(18)30322-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Steiner TJ, Stovner LJ, Vos T, Jensen R, Katsarava Z. Migraine is first cause of disability in under 50s: will health politicians now take notice? J Headache Pain 2018;19:17. 10.1186/s10194-018-0846-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lipton RB, Bigal ME, Diamond M, Freitag F, Reed ML, Stewart WF, AMPP Advisory Group Migraine prevalence, disease burden, and the need for preventive therapy. Neurology 2007;68:343-9. 10.1212/01.wnl.0000252808.97649.21 [DOI] [PubMed] [Google Scholar]
- 5. Schulte LH, May A. Headache research in 2014: Advancing migraine therapy. Lancet Neurol 2015;14:6-7. 10.1016/S1474-4422(14)70295-9 [DOI] [PubMed] [Google Scholar]
- 6. Facco E, Liguori A, Petti F, et al. Traditional acupuncture in migraine: a controlled, randomized study. Headache 2008;48:398-407. 10.1111/j.1526-4610.2007.00916.x [DOI] [PubMed] [Google Scholar]
- 7. Allais G, De Lorenzo C, Quirico PE, et al. Acupuncture in the prophylactic treatment of migraine without aura: a comparison with flunarizine. Headache 2002;42:855-61. 10.1046/j.1526-4610.2002.02203.x [DOI] [PubMed] [Google Scholar]
- 8. Wang LP, Zhang XZ, Guo J, et al. Efficacy of acupuncture for migraine prophylaxis: a single-blinded, double-dummy, randomized controlled trial. Pain 2011;152:1864-71. 10.1016/j.pain.2011.04.006 [DOI] [PubMed] [Google Scholar]
- 9. Zhao ZQ. Neural mechanism underlying acupuncture analgesia. Prog Neurobiol 2008;85:355-75. 10.1016/j.pneurobio.2008.05.004 [DOI] [PubMed] [Google Scholar]
- 10. Kim SK, Moon HJ, Na HS, et al. The analgesic effects of automatically controlled rotating acupuncture in rats: mediation by endogenous opioid system. J Physiol Sci 2006;56:259-62. 10.2170/physiolsci.SC002706 [DOI] [PubMed] [Google Scholar]
- 11. Goldman N, Chen M, Fujita T, et al. Adenosine A1 receptors mediate local anti-nociceptive effects of acupuncture. Nat Neurosci 2010;13:883-8. 10.1038/nn.2562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Li Y, Zheng H, Witt CM, et al. Acupuncture for migraine prophylaxis: a randomized controlled trial. CMAJ 2012;184:401-10. 10.1503/cmaj.110551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Linde K, Streng A, Jürgens S, et al. Acupuncture for patients with migraine: a randomized controlled trial. JAMA 2005;293:2118-25. 10.1001/jama.293.17.2118 [DOI] [PubMed] [Google Scholar]
- 14. Diener HC, Kronfeld K, Boewing G, et al. GERAC Migraine Study Group Efficacy of acupuncture for the prophylaxis of migraine: a multicentre randomised controlled clinical trial. Lancet Neurol 2006;5:310-6. 10.1016/S1474-4422(06)70382-9 [DOI] [PubMed] [Google Scholar]
- 15. Wang Y, Xue CC, Helme R, Da Costa C, Zheng Z. Acupuncture for frequent migraine: a randomized, patient/assessor blinded, controlled trial with one-year follow-up. Evid Based Complement Alternat Med 2015;2015:920353. 10.1155/2015/920353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wallasch TM, Weinschuetz T, Mueller B, Kropp P. Cerebrovascular response in migraineurs during prophylactic treatment with acupuncture: a randomized controlled trial. J Altern Complement Med 2012;18:777-83. 10.1089/acm.2011.0308 [DOI] [PubMed] [Google Scholar]
- 17. Linde K, Niemann K, Schneider A, Meissner K. How large are the nonspecific effects of acupuncture? A meta-analysis of randomized controlled trials. BMC Med 2010;8:75. 10.1186/1741-7015-8-75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Birch S. A review and analysis of placebo treatments, placebo effects, and placebo controls in trials of medical procedures when sham is not inert. J Altern Complement Med 2006;12:303-10. 10.1089/acm.2006.12.303 [DOI] [PubMed] [Google Scholar]
- 19. Lund I, Lundeberg T. Are minimal, superficial or sham acupuncture procedures acceptable as inert placebo controls? Acupunct Med 2006;24:13-5. 10.1136/aim.24.1.13 [DOI] [PubMed] [Google Scholar]
- 20. MacPherson H, Vertosick E, Lewith G, et al. Acupuncture Trialists’ Collaboration Influence of control group on effect size in trials of acupuncture for chronic pain: a secondary analysis of an individual patient data meta-analysis. PLoS One 2014;9:e93739. 10.1371/journal.pone.0093739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia 2013;33:629-808. 10.1177/0333102413485658 [DOI] [PubMed] [Google Scholar]
- 22. Streitberger K, Kleinhenz J. Introducing a placebo needle into acupuncture research. Lancet 1998;352:364-5. 10.1016/S0140-6736(97)10471-8 [DOI] [PubMed] [Google Scholar]
- 23. Pringsheim T, Davenport W, Mackie G, et al. Canadian Headache Society Prophylactic Guidelines Development Group Canadian Headache Society guideline for migraine prophylaxis. Can J Neurol Sci 2012;39(Suppl 2):S1-59. [PubMed] [Google Scholar]
- 24. Cole JC, Lin P, Rupnow MF. Validation of the Migraine-Specific Quality of Life Questionnaire version 2.1 (MSQ v. 2.1) for patients undergoing prophylactic migraine treatment. Qual Life Res 2007;16:1231-7. 10.1007/s11136-007-9217-1 [DOI] [PubMed] [Google Scholar]
- 25. Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 1989;28:193-213. 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- 26. Santoro A, Fontana A, Miscio AM, Zarrelli MM, Copetti M, Leone MA. Quarterly repeat cycles of onabotulinumtoxinA in chronic migraine patients: the benefits of the prolonged treatment on the continuous responders and quality-of-life conversion rate in a real-life setting. Neurol Sci 2017;38:1779-89. 10.1007/s10072-017-3054-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Leyfer OT, Ruberg JL, Woodruff-Borden J. Examination of the utility of the Beck Anxiety Inventory and its factors as a screener for anxiety disorders. J Anxiety Disord 2006;20:444-58. 10.1016/j.janxdis.2005.05.004 [DOI] [PubMed] [Google Scholar]
- 28. Geisser ME, Roth RS, Robinson ME. Assessing depression among persons with chronic pain using the Center for Epidemiological Studies-Depression Scale and the Beck Depression Inventory: a comparative analysis. Clin J Pain 1997;13:163-70. 10.1097/00002508-199706000-00011 [DOI] [PubMed] [Google Scholar]
- 29. Mao JJ, Armstrong K, Farrar JT, Bowman MA. Acupuncture expectancy scale: development and preliminary validation in China. Explore (NY) 2007;3:372-7. 10.1016/j.explore.2006.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Zhao L, Chen J, Li Y, et al. The long-term effect of acupuncture for migraine prophylaxis: a randomized clinical trial. JAMA Intern Med 2017;177:508-15. 10.1001/jamainternmed.2016.9378 [DOI] [PubMed] [Google Scholar]
- 31. Thiese MS, Ronna B, Ott U. P value interpretations and considerations. J Thorac Dis 2016;8:E928-31. 10.21037/jtd.2016.08.16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Linde K, Allais G, Brinkhaus B, et al. Acupuncture for the prevention of episodic migraine. Cochrane Database Syst Rev 2016;(6):CD001218. 10.1002/14651858.CD001218.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Dodick DW, Silberstein SD, Bigal ME, et al. Effect of fremanezumab compared with placebo for prevention of episodic migraine: a randomized clinical trial. JAMA 2018;319:1999-2008. 10.1001/jama.2018.4853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Skljarevski V, Oakes TM, Zhang Q, et al. Effect of Different Doses of Galcanezumab vs Placebo for Episodic Migraine Prevention: A Randomized Clinical Trial. JAMA Neurol 2018;75:187-93. 10.1001/jamaneurol.2017.3859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Spaeth RB, Camhi S, Hashmi JA, et al. A longitudinal study of the reliability of acupuncture deqi sensations in knee osteoarthritis. Evid Based Complement Alternat Med 2013;2013:204259. 10.1155/2013/204259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Han JS. Acupuncture analgesia: areas of consensus and controversy. Pain 2011;152(Suppl):S41-8. 10.1016/j.pain.2010.10.012 [DOI] [PubMed] [Google Scholar]
- 37. Napadow V, Makris N, Liu J, Kettner NW, Kwong KK, Hui KK. Effects of electroacupuncture versus manual acupuncture on the human brain as measured by fMRI. Hum Brain Mapp 2005;24:193-205. 10.1002/hbm.20081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Tsui P, Leung MC. Comparison of the effectiveness between manual acupuncture and electro-acupuncture on patients with tennis elbow. Acupunct Electrother Res 2002;27:107-17. 10.3727/036012902816026040 [DOI] [PubMed] [Google Scholar]
- 39. Plaster R, Vieira WB, Alencar FA, Nakano EY, Liebano RE. Immediate effects of electroacupuncture and manual acupuncture on pain, mobility and muscle strength in patients with knee osteoarthritis: a randomised controlled trial. Acupunct Med 2014;32:236-41. 10.1136/acupmed-2013-010489 [DOI] [PubMed] [Google Scholar]
- 40. Kim BH, Kim K, Nam HJ. A comparative study on the effects of systemic manual acupuncture, periauricular electroacupuncture, and digital electroacupuncture to treat tinnitus: A randomized, paralleled, open-labeled exploratory trial. BMC Complement Altern Med 2017;17:85. 10.1186/s12906-017-1589-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Schliessbach J, van der Klift E, Arendt-Nielsen L, Curatolo M, Streitberger K. The effect of brief electrical and manual acupuncture stimulation on mechanical experimental pain. Pain Med 2011;12:268-75. 10.1111/j.1526-4637.2010.01051.x [DOI] [PubMed] [Google Scholar]
- 42. Wang K, Bugge J, Bugge S. A randomised, placebo-controlled trial of manual and electrical acupuncture for the treatment of tinnitus. Complement Ther Med 2010;18:249-55. 10.1016/j.ctim.2010.09.005 [DOI] [PubMed] [Google Scholar]
- 43. Lundeberg T, Lund I. Are reviews based on sham acupuncture procedures in fibromyalgia syndrome (FMS) valid? Acupunct Med 2007;25:100-6. 10.1136/aim.25.3.100 [DOI] [PubMed] [Google Scholar]
- 44. Moffet HH. Sham acupuncture may be as efficacious as true acupuncture: a systematic review of clinical trials. J Altern Complement Med 2009;15:213-6. 10.1089/acm.2008.0356 [DOI] [PubMed] [Google Scholar]
- 45. Le Bars D, Villanueva L, Bouhassira D, Willer JC. Diffuse noxious inhibitory controls (DNIC) in animals and in man. Patol Fiziol Eksp Ter 1992;(4):55-65. [PubMed] [Google Scholar]
- 46. Cadden SW, Villanueva L, Chitour D, Le Bars D. Depression of activities of dorsal horn convergent neurones by propriospinal mechanisms triggered by noxious inputs; comparison with diffuse noxious inhibitory controls (DNIC). Brain Res 1983;275:1-11. 10.1016/0006-8993(83)90412-2 [DOI] [PubMed] [Google Scholar]
- 47. Liu X, Zhu B, Zhang SX. Relationship between electroacupuncture analgesia and descending pain inhibitory mechanism of nucleus raphe magnus. Pain 1986;24:383-96. 10.1016/0304-3959(86)90124-7 [DOI] [PubMed] [Google Scholar]
- 48. He W, Wang XY, Shi H, et al. Cutaneous neurogenic inflammation in the sensitized acupoints induced by gastric mucosal injury in rats. BMC Complement Altern Med 2017;17:141-9. 10.1186/s12906-017-1580-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Massiou H, Bousser MG. [Prophylactic drug treatment of migraine]. Rev Neurol (Paris) 2005;161:681-4. 10.1016/S0035-3787(05)85116-1 [DOI] [PubMed] [Google Scholar]
- 50. Puledda F, Shields K. Non-Pharmacological Approaches for Migraine. Neurotherapeutics 2018;15:336-45. 10.1007/s13311-018-0623-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Kaptchuk TJ. Placebo studies and ritual theory: a comparative analysis of Navajo, acupuncture and biomedical healing. Philos Trans R Soc Lond B Biol Sci 2011;366:1849-58. 10.1098/rstb.2010.0385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Makary MM, Lee J, Lee E, et al. Phantom acupuncture induces placebo credibility and vicarious sensations: a parallel fMRI study of low back pain patients. Sci Rep 2018;8:930. 10.1038/s41598-017-18870-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix 1: protocol
Appendix 2: acupuncture ritual
Appendix 3: supplementary tables
Appendix 4: meta-analysis