Abstract
Background
Ewing’s sarcoma usually presents in paediatric patients with its primary location being bone tissue. Nevertheless, we present such an adult case which arises from the small intestine. We registered thirty one cases of such origin published so far excluding ours.
Case presentation
We report a case of 30 year old female who was admitted due to the persistent anaemia. Whole body computed tomography scan revealed abdominal mass in her left upper abdominal compartment. Surgery on the mass originating from jejunum was performed, although due to extremely complicated postoperative period and rapid dissemination no additional therapy had been performed. The tumour was positive for CD99, ERG, CD56, Synaptophysin, PanCK, Cam5.2.
Conclusion
Extraosseus Ewing’s sarcoma is extremely rare entity, with poor prognosis.
Keywords: Ewing’s sarcoma, Extraosseus sarcoma, Primitive neuroectodermal tumor, Small bowel sarcoma, ERG-FUS translocation
Background
Ewing’s sarcoma was first identified by A.P. Stout in 1918 [1]. Genetically Ewing’s sarcoma is determined by recurrent balanced translocations involving the EWSR1 gene on chromosome 22 and members of the E-twenty six (ETS) family of transcription factor genes [2–4]. It includes extra-osseous (also called extra-skeletal) Ewing’s sarcoma, peripheral neuroepithelioma, Askin’s tumour (tumour of chest wall), and peripheral neuroblastoma [4, 5]. Primitive neuroectodermal tumours (PNET) are also referred as Ewing‘s sarcoma [6]. Histologically they are presented as small round cell tumours which originate from the bone and soft tissue [7]. Nevertheless they can be found in most organs: chest (44%), retroperitoneum and pelvis (26%), extremities (20%), head and neck (6%), kidneys, oesophagus, ovaries, prostate [5–10] and are especially rare in small bowel [7]. To make matters clearer, they are divided into pPNET (peripheral primitive neuroectodermal tumours), CNS primitive neuroectodermal tumours (PNETs) and neuroblastoma [11]. While microscoping pPNET looks almost identical to the tumours originating from the bone [12] which makes them hard to differentiate especially when it originates near the bone. In all cases Ewing’s sarcoma metastasises rapidly disregarding its origin [13]. It usually occurs in young patients, with paediatric patients being a second most common tumour in this age group [5, 12–15]. In older patients survival rate is lower and there are more cases with metastatic spread or extra skeletal tumours [3]. The common sites of Ewing’s sarcoma recurrence are the soft tissue of the lower extremities, paravertebral region, and pelvis [14]. Five year overall survival rate is 44% (ranging 20–60%) [16].
Up to date only 31 cases of extraosseus Ewing’s sarcoma arising in a small intestine are reported in the literature (Table 1).
Table 1.
Clinical characteristics and outcomes of patients with intestinal Ewing sarcoma
| Author, year | Sex | Age, y | Part of small intestine | Treatment | Survival, months | MTS on diagnosis |
|---|---|---|---|---|---|---|
| Horie, 2000 [15] | M | 40 | Mesentery of jejunum | Surgery - > systemic therapy | 5 | N/A |
| Shek, 2001 [9] | F | 9 | Mesentery of the small bowel | Surgery- > systemic therapy - > surgery- > systemic therapy | 25 | pelvis |
| Saranganathan, 2001 [17] | M | 13 | Jejunum | Surgery | 12+ | Absent |
| Balasubramanian, 2002 [16] | F | 53 | Mesentery of ileum | Surgery | N/A | N/A |
| Graham, 2002 [2] | M | 14 | Distal ileum | Surgery- > systemic therapy | 52+ | N/A |
| Boehm, 2003 [18] | M | 18 | Ileum | Surgery- > systemic therapy - > regression - > systemic therapy, autologous cell Tx | + | peritoneum |
| Bala, 2006 [8] | F | 57 | Terminal ileum | Surgery- > systemic therapy | 8+ | N/A |
| Batziou, 2006 [12] | M | 66 | Small intestine | 2x surgery - > 4 systemic therapy | 48+ | N/A |
| Kim, 2007 [14] | M | 63 | Terminal ileum and jejunum | Surgery- > systemic therapy | N/A | Regional l/n |
| Sethi, 2007 | M | 44 | Terminal ileum | Surgery- > 6 courses systemic therapy | 13 | N/A |
| Rodarte-Shade, 2012 [19] | M | 32 | Ileum | Surgery- > systemic therapy | 6+ | Absent |
| Vignali, 2012 [20] | F | 15 | Terminal ileum, mesentery | Surgery- > systemic therapy | N/A | N/A |
| Kim, 2013 [4] | M | 23 | Mesentery of jejunum | Surgery- > systemic therapy - > surgery | N/A | Porta hepatis, l/n |
| Rachan Shetty, 2014 | F | 24 | Ileum | Surgery - > systemic therapy | 15+ | N/A |
| Milione, 2014 [3] | M | 18 | Ileum | Core biopsy | 8 | Liver |
| Milione, 2014 [3] | M | 20 | Ileum | Core biopsy | 28 | Liver |
| Milione, 2014 [3] | M | 42 | Ileum | Surgery - > systemic therapy | 11 | Absent |
| Milione, 2014 [3] | M | 45 | Ileum | Surgery - > systemic therapy | 13 | Absent |
| Milione, 2014 [3] | F | 15 | Ileum | Surgery - > systemic therapy + radiotherapy | 28 | Absent |
| Milione, 2014 [3] | M | 57 | Ileum | Surgery | + | Absent |
| Milione, 2014 [3] | F | 28 | Ileum | Surgery | 204+ | Liver |
| Peng, 2015 [13] | M | 59 | Mesentery of terminal ileum | Surgery - > no adjuvant therapy | N/A | N/A |
| Peng, 2015 [13] | M | 22 | Ileum | Surgery - > no adjuvant therapy | N/A | Liver |
| Peng, 2015 [13] | F | 36 | Mesentery of ileum | Surgery - > 8 cycles systemic therapy | 34 | N/A |
| Padma, 2015 [5] | F | 22 | Distal jejunum | Surgery | N/A | Absent |
| Liu, 2015 | M | 15 | Mesentery of jejunum | Surgery | 7 | N/A |
| Li, 2017 [7] | F | 16 | Ileum | Surgery | N/A | N/A |
| Kim, 2017 [10] | F | 9 | Jejunum | Systemic therapy - > surgery - > adjuvant therapy | N/A | peritoneum |
| Liao, 2018 [21] | F | 25 | Ileum | Surgery | + | N/A |
| Cantu, 2019 [22] | F | 67 | Jejunum | Surgery | 3+ | No |
| Yagnik, 2019 [11] | M | 42 | Jejunum | Surgery - > systemic therapy | + | N/A |
| Our case, 2020 | F | 30 | Jejunum | Surgery | 2 | No |
Tx – Transplant
N/A – Not available
L/n – Lymph nodes
+ − No information of death upon the last follow up
Here we present a case of Ewing’s sarcoma in a small intestine with an extremely rapid dissemination and unfortunate ending.
Case presentation
Here we present a 30 year old female admitted to local hospital complaining of mild general weakness lasting for four months. Full blood count showed severe anaemia of 54 g/l and a mild gastric wall inflammation was seen on gastroscopy. Blood transfusion in therapeutic ward was then performed. Whole body computed tomography (CT) scan discovered 4.7 × 6.2 × 6.5 cm non-homogenic tumour with a cystic component in a left upper abdominal compartment. Tumour had a close contact with an inferior mesenteric vein (IMV) at the long segment, near the entrance to the superior mesenteric vein (SMV) (Type A/B) without overgrowing any another surrounding organ. Gastrointestinal stromal tumour (GIST) was suspected (Figs. 1 and 2). Patient was transferred to our cancer institute and after multidisciplinary team discussion she was elected for a surgery – removal of the GIST of the jejunum. The patient had no previous medical history of other diseases, surgeries or allergies. Her initial blood test showed haemoglobin of 74.6 g/l, so additional blood transfusion was performed.
Fig. 1.
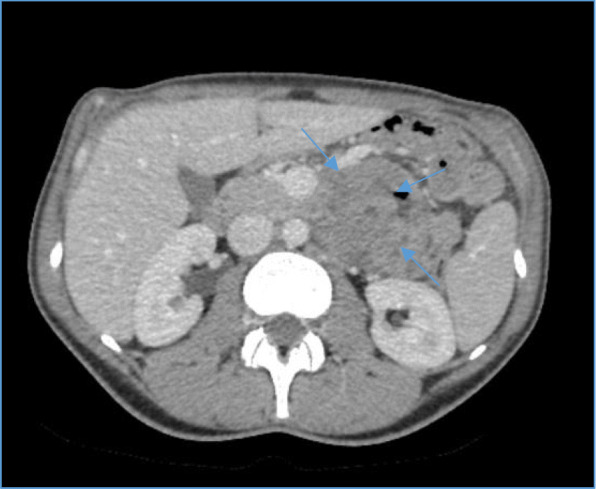
Computed tomography scan of the abdomen. Axial transverse view of 4.7 × 6.2 × 6.5 cm non-homogenic tumour (blue arrows) with a cystic component contacting with an inferior mesenteric vein
Fig. 2.

Computed tomography scan of the abdomen. Coronal view – 4.7 × 6.2 × 6.5 cm non-homogenic tumour with a cystic component contacting with an inferior mesenteric vein (blue arrows)
On laparotomy the tumour involving the first loop of the small intestine (30 cm from the Treitz ligament), a part of uncinated process of the pancreas, IMV and inferior mesenteric artery (IMA) was found. Enlarged small intestine lymph nodes were also seen. Resection of 50 cm of small intestine with the tumour was performed. Two layer end-to-end entero-entero anastomosis was performed and enteral feeding tube was inserted below the anastomosis. Early postoperative course was uneventful. On postoperative day (POD) five the blood appeared through the drains – emergency surgery was initiated. Massive bleeding from superior mesenteric artery (SMA) was found and the arterial defect was sutured. The cyanotic small intestines were noticed and a partial occlusion of SMA was suspected. Aorto-mesenteric shunt using saphenous vein was performed and the small intestine regained its blood supply. Two days later anastomotic leak was suspected – bile from the drain was noticed. Anastomosis was resected and two layer side-to-side duodenojejunal anastomosis was performed. By then, the pathology report revealed a high grade G3 peripheral/primitive neuroectodermal tumour (PNET)/atypical Ewing sarcoma which expansion to the pancreas (Figs. 3, 4, 5, 6, 7 and 8). R1 resection (at the uncinated process of the pancreas) was confirmed (pT4N1, LVI [2]).
Fig. 3.
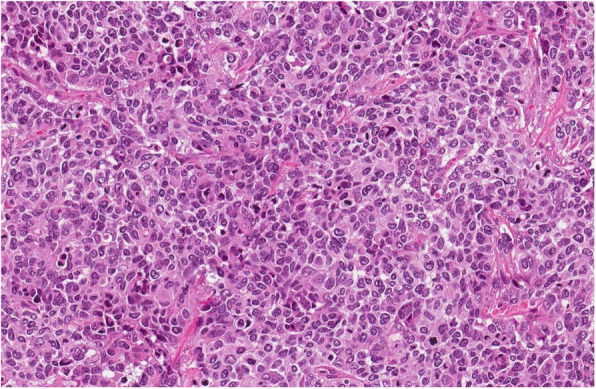
Tumour is composed of sheets of mildly to moderately atypical cells with round or oval nuclei and prominent nucleoli. There were up to 60 mitoses per 10 HPF, HE 20x
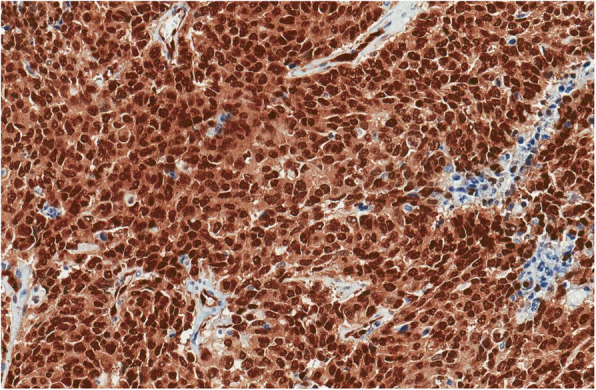
Fig. 4.
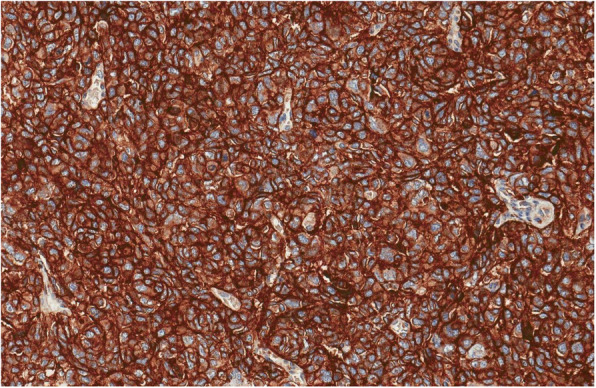
Tumour showed diffuse membranous positivity for CD99
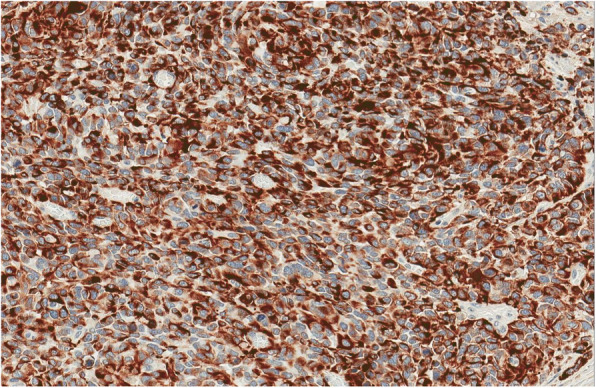
Fig. 5.
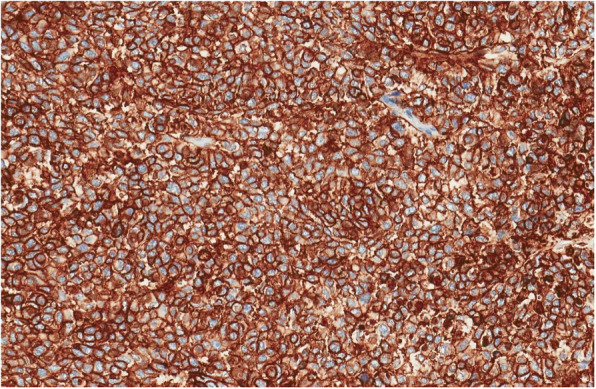
Tumour showed diffuse membranous positivity CD56
Fig. 6.
Diffuse nuclear positivity for ERG
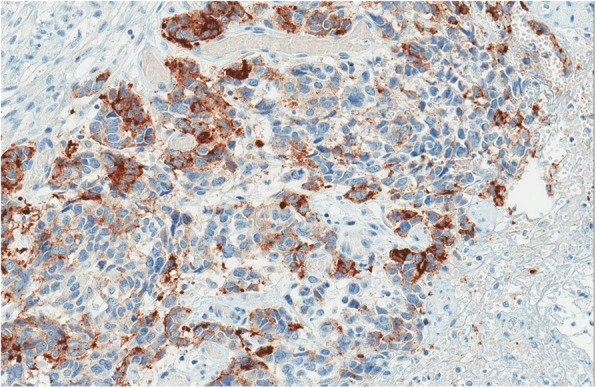
Fig. 7.
Focal immunoreactions for Cam5.2
Fig. 8.
Focal immunoreactions for Synaptophysin
Tumour histology
An ulcerated tumour in small intestine wall was composed of solid sheets of small blue cells with irregular nuclear contours and prominent nucleoli. Differential diagnosis included poorly differentiated adenocarcinoma, neuroendocrine carcinoma, melanoma, lymphoma, gastrointestinal clear cell sarcoma, synovial sarcoma, rhabdomyosarcoma, epithelioid angiosarcoma, epithelioid sarcoma and germ cell tumour. Immunohistochemical tests were performed and tumour demonstrated diffuse positivity for CD99, ERG, CD56 and focal positivity for Synaptophysin, PanCK, Cam5.2. Tumour was consistently negative for LCA, SMA, Desmin, S100, HMB45, TLE1, Chromogranin A, CDX2, TTF1, PAX8, CK7, CK19, CD31, SALL4, Glucagon, Somatostatin, Gastrin and Serotonin. There was no INI1 loss. Diffuse CD99, ERG, CD56, focal PanCK, Cam5.2 and Synaptophysin immune positivity are characteristic for Ewing sarcoma family of tumours. EWSR1 (22q12) break-apart FISH test and PCR test for EWSR1-ERG, EWSR1-ETV1, EWSR1-FLI1, EWSR1-FEV, EWSR1-ETV4 translocations were performed. Unfortunately, there was no evidence of EWRS1 gene rearrangements by both FISH and PCR EWSR1 methods. Despite this fact there was no evidence of any other tumour and final diagnosis was high grade G3 peripheral/primitive neuroectodermal tumour (PNET)/atypical Ewing’s sarcoma, possibly with a rare translocation.
Postoperative period
Eleven days after the third surgery bleeding recurred – bleeding from the aorto-mesenteric shunt was found. It was sutured along its wall and intraoperative ultrasound showed reduced diameter of the shunt, and recanalized SMA. During postoperative period due to progressing bile leakage, bile ducts were catheterized trans-hepatically. Nine days later intraabdominal bleeding recurred. Bleeding from the aorta at the shunt area was found and sutured. Small intestine on the other hand showed total necrosis with multiple perforations. The changes were incompatible with life. Nonetheless 48 h later, patient vital signs improved and the condition stabilized. Therefore, during the next surgery necrotised small intestine was removed while closing both ends of the intestines at the demarcation lines and gastrostomy was made for the drainage of the gastric content. During the next few weeks bleeding recurred and multiple (> 50) liver metastases were found. Bleeding was controlled but the patient died because of rapid dissemination of the disease.
Discussion and Conclusion
Intestinal Ewing’s sarcoma as many other tumours can manifest asymptomatic although there are cases in which it occurs as intussusception [18], perforation [11, 15], intestinal obstruction [14, 23], rupture [4] but usually it presents with abdominal pain or fatigue and weakness caused by mass and/or bleeding as in our case. It can be misdiagnosed as a gynaecologic pathology especially in young females as the literature shows pain can often occur in the lower abdomen [6, 13, 20]. Clinical presentation mainly depends on the affected site of the gastrointestinal tract [19].
Thorough examination should follow CT scan to exclude other acute diseases although there are no specific radiological signs of Ewing’s sarcoma [8]. For this reason Ewing’s sarcoma may initially be treated as GIST [7] as in our case.
To provide proper diagnosis, pathological examination should be carried out. It‘s round cell morphology is similar to neuroblastoma, malignant lymphoma, rhabdomyosarcoma, GIST, and desmoplastic small round cell tumour [14]. While Ewing’s sarcoma shows rosette formation, glycogen deposition, also NSE, S-100 protein, neurosecretory-type granules [12]. In addition CD99 antigen could also be a useful tool [15]. Nowadays molecular testing is a reliable diagnostic method to diagnose ES. The most frequent translocation EWSR1-FLI1 occurs in 85% of cases of ES [2, 22]. Second most common translocation is EWSR1-ERG (5–15%) and in such cases tumour cells are immunohistochemically positive for ERG marker. In our case ERG immunohistochemical reaction was positive, although there was no EWSR1-ERG translocation. However there is a very rare ERG-FUS translocation (< 1%), when tumour cells are also positive for ERG. We suppose that this translocation could occur in our case. It is also mentioned that fusion transcripts should not be the sole criterion of PNET [17].
All Ewing’s sarcoma treatment includes local surgical and/or radiotherapy treatment followed by multidrug systemic chemotherapy [5, 7]. It usually includes vincristine, doxorubicin, cyclophosphamide and dactinomycin [16] although of ifosfamide and etoposide were added. Latter improves outcomes in non-metastatic cases [13].
Prognosis of intestinal Ewing’s sarcoma is not known as there are not enough cases. It could be compared to other sites. Although some authors do not relate tumour size with worse outcomes [13] other find > 5 cm size of the tumour having impact for worse survival [24]. Even in those cases surgical intervention is recommended as it decreases morbidity [21, 25]. Worse survival also may include pelvic site, older patients, poor response to chemotherapy, and metastatic disease at presentation [8] which was in our case. The main two reasons of unfortunate consequence in our case was acute pancreatitis caused by R1 resection at the uncinated process and a very aggressive underlying disease.
To conclude, extraosseus Ewing’s sarcoma is extremely rare entity, with most often poor prognosis.
Acknowledgements
Not applicable.
Abbreviations
- ETS
E-twenty six
- PNET
Primitive neuroectodermal tumours
- pPNET
peripheral primitive neuroectodermal tumour)
- PNETs
CNS primitive neuroectodermal tumours
- CT
computed tomography
- GIST
Gastrointestinal stromal tumour
- IMV
inferior mesenteric vein
- SMV
superior mesenteric vein
- IMA
inferior mesenteric artery
- SMA
superior mesenteric artery
- LVI
lympho vascular invasion
- PCR
polymerase chain reaction
Authors’ contributions
AK analysed and interpreted the patient data regarding the previous cases. AK and AD performed the literature search and manuscript writing. DS and VS performed the histological examination of the tumour, and were part contributors in writing the manuscript. KP, ES performed the surgery. All authors read and approved the final manuscript.
Funding
None.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Ethics approval and consent to participate
The case was approved by the National Cancer Institute Review Board (No 2019.12.00073).
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor of this journal.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Stout A. A tumor of ulnar nerve. Proc NY Pathol Soc. 1918;18:2–12. [Google Scholar]
- 2.Graham DK, Stork LC, Wei Q, Ingram JD, Karrer FM, Mierau GW, et al. Molecular genetic analysis of a small bowel primitive Neuroectodermal tumor. Pediatr Dev Pathol. 2002;5(1):86–90. doi: 10.1007/s10024-001-0192-1. [DOI] [PubMed] [Google Scholar]
- 3.Milione Massimo, Gasparini Patrizia, Sozzi Gabriella, Mazzaferro Vincenzo, Ferrari Andrea, Casali Paolo G, Perrone Federica, Tamborini Elena, Pellegrinelli Alessio, Gherardi Giorgio, Arrigoni Gianluigi, Collini Paola, Testi Adele, De Paoli Elena, Aiello Antonella, Pilotti Silvana, Pelosi Giuseppe. Ewing sarcoma of the small bowel: a study of seven cases, including one with the uncommonly reportedEWSR1-FEVtranslocation. Histopathology. 2014;64(7):1014–1026. doi: 10.1111/his.12350. [DOI] [PubMed] [Google Scholar]
- 4.Kim JM, Chu YC, Choi CH, Kim L, Choi SJ, Park IS, et al. Peripheral primitive neuroectodermal tumor with osseous component of the small bowel mesentery: a case study. Korean J Pathol. 2013;47(1):77. doi: 10.4132/KoreanJPathol.2013.47.1.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Padma M, Lakshmi RR, Kumar CK. Extraskeletal Ewing’s sarcoma of the small bowel. Int J Med Sci Clin Invent. 2015;2:645–647. [Google Scholar]
- 6.Shetty R, Naveen JA, Premalatha CS, Lakshmaiah KC. Peripheral primitive neuroectodermal tumor of small bowel mesentry presenting as intestinal obstruction: a case report. [Internet]. [cited 2019 Oct 6]. Available from: https://www.australasiancancer.org/journal-article-view/peripheral-primitive-neuroectodermal-tumor-of-665.
- 7.Li T, Zhang F, Cao Y, Ning S, Bi Y, Xue W, et al. Primary Ewing’s sarcoma/primitive neuroectodermal tumor of the ileum: case report of a 16-year-old Chinese female and literature review. Diagn Pathol. 2017;12(1):37. doi: 10.1186/s13000-017-0626-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bala M, Maly A, Remo N, Gimmon Z, Almogy G. Peripheral primitive neuroectodermal tumor of bowel mesentery in adults. Isr Med Assoc J. 2006;8(7):515–516. [PubMed] [Google Scholar]
- 9.Shek TWH, Chan GCF, Khong PL, Chung LP, Cheung ANY. Ewing sarcoma of the small intestine. J Pediatr Hematol Oncol. 2001;23(8):530–532. doi: 10.1097/00043426-200111000-00013. [DOI] [PubMed] [Google Scholar]
- 10.Kim YS, Moon HM, Lee KS, Park YS, Kim HY, Kim JY, et al. Pediatric Ewing’s sarcoma/primitive Neuroectodermal tumor (ES/PNET) developed in the small intestine: a case report. Clin Pediatr Hematol Oncol. 2017;24(2):162. doi: 10.15264/cpho.2017.24.2.162. [DOI] [Google Scholar]
- 11.Yagnik VD, Dawka S. Extraskeletal Ewing’s sarcoma/peripheral primitive neuroectodermal tumor of the small bowel presenting with gastrointestinal perforation. Clin Exp Gastroenterol. 2019;12:279–285. doi: 10.2147/CEG.S203697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Batziou C, Stathopoulos GP, Petraki K, Papadimitriou C, Rigatos SK, Kondopodis E, et al. Primitive neurectodermal tumors: a case of extraosseous Ewing’s sarcoma of the small intestine and review of the literature. J BUON. 2006;11(4):519–522. [PubMed] [Google Scholar]
- 13.Peng L, Yang L, Wu N, Wu B. Primary primitive neuroectodermal tumor arising in the mesentery and ileocecum: a report of three cases and review of the literature. Exp Ther Med. 2015;9(4):1299–1303. doi: 10.3892/etm.2015.2242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim D-W, Chang HJ, Jeong JY, Lim S-B, Lee J-S, Hong EK, et al. Ewing’s sarcoma/primitive neuroectodermal tumor (ES/PNET) of the small bowel: a rare cause of intestinal obstruction. Int J Color Dis. 2007;22(9):1137–1138. doi: 10.1007/s00384-006-0142-5. [DOI] [PubMed] [Google Scholar]
- 15.Horie Y, Kato M. Peripheral primitive neuroectodermal tumor of the small bowel mesentery: a case showing perforation at onset. Pathol Int. 2000;50(5):398–403. doi: 10.1046/j.1440-1827.2000.01045.x. [DOI] [PubMed] [Google Scholar]
- 16.Balasubramanian B, Dinakarababu E, Molyneux AJ. Primary primitive neuroectodermal tumour of the small bowel mesentery: case report. Eur J Surg Oncol. 2002;28(2):197–198. doi: 10.1053/ejso.2001.1155. [DOI] [PubMed] [Google Scholar]
- 17.Sarangarajan R, Hill DA, Humphrey PA, Hitchcock MG, Dehner LP, Pfeifer JD. Primitive Neuroectodermal tumors of the biliary and gastrointestinal tracts: Clinicopathologic and molecular diagnostic study of two cases. Pediatr Dev Pathol. 2001;4(2):185–191. doi: 10.1007/s100240010141. [DOI] [PubMed] [Google Scholar]
- 18.Boehm R, Till H, Landes J, Schmid I, Joppich I. Ileoileal intussusception caused by a Ewing sarcoma tumour. An unusual case report. Eur J Pediatr Surg. 2003;13(4):272–275. doi: 10.1055/s-2003-42234. [DOI] [PubMed] [Google Scholar]
- 19.Rodarte-Shade M, Palomo-Hoil R, Vazquez J, Ancer A, Vilches N, Flores-Gutierrez JP, et al. Primitive Neuroectodermal tumor (PNET) of the small bowel in a young adult with lower gastrointestinal bleeding. J Gastrointest Canc. 2012;43(S1):243–245. doi: 10.1007/s12029-012-9409-y. [DOI] [PubMed] [Google Scholar]
- 20.Vignali M, Zacchè MM, Messori P, Natale A, Busacca M. Ewing’s sarcoma of the small intestine misdiagnosed as a voluminous pedunculated uterine leiomyoma. Eur J Obstet Gynecol Reprod Biol. 2012;162(2):234–235. doi: 10.1016/j.ejogrb.2012.02.009. [DOI] [PubMed] [Google Scholar]
- 21.Liao Y-S, Chiang I-H, Gao H-W. A mesenteric primary peripheral Ewing’s sarcoma/primitive neuroectodermal tumor with molecular cytogenetic analysis: report of a rare case and review of literature. Indian J Pathol Microbiol. 2018;61(2):248–251. doi: 10.4103/IJPM.IJPM_546_17. [DOI] [PubMed] [Google Scholar]
- 22.Cantu C, Bressler E, Dermawan J, Paral K. Extraskeletal Ewing sarcoma of the jejunum: a case report. Perm J. 2019;23. [DOI] [PMC free article] [PubMed]
- 23.Sethi B, Smith GT. Primary primitive neuroectodermal tumour arising in the small bowel. Histopathology. 2007;50(5):665–666. doi: 10.1111/j.1365-2559.2007.02631.x. [DOI] [PubMed] [Google Scholar]
- 24.Kushner BH, Hajdu SI, Gulati SC, Erlandson RA, Exelby PR, Lieberman PH. Extracranial primitive neuroectodermal tumors. The Memorial Sloan-Kettering Cancer Center experience. Cancer. 1991;67(7):1825–1829. doi: 10.1002/1097-0142(19910401)67:7<1825::AID-CNCR2820670702>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 25.Liu Z, Xu Y-H, Ge C-L, Long J, Du R-X, Guo K-J. Huge peripheral primitive neuroectodermal tumor of the small bowel mesentery at nonage: a case report and review of the literature. World J Clin Cases. 2016;4(9):306–309. doi: 10.12998/wjcc.v4.i9.306. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.


