Abstract
The need to improve access to palliative care across multiple settings and disease groups has been identified. This requires equipping health care professionals from many different professions, including physicians and nurses, among others, with basic palliative care competencies to provide a palliative care approach. Pallium Canada's Curriculum Development Framework supports the development, deployment, and dissemination, on a large scale, of multiple courses targeting health care professionals across multiple settings of care and disease groups. The Framework is made up of eight phases: (1) Concept, (2) Decision, (3) Curriculum Planning, (4) Prototype Development, (5) Piloting, (6) Dissemination, (7) Language and Cultural Adaptation, and (8) Ongoing Maintenance and Updates. Several of these phases include iterative cyclical activities. The framework allows multiple courses to be developed simultaneously, staggered in a production line with each phase and their corresponding activities requiring different levels of resources and stakeholder engagement. The framework has allowed Pallium Canada to develop, launch, and maintain numerous versions of its Learning Essential Approaches to Palliative Care (LEAP) courses concurrently. It leverages existing LEAP courses and curriculum materials to produce new LEAP courses, allowing significant efficiencies and maximizing output. This article describes the framework and its various activities, which we believe could be very useful for other jurisdictions undertaking the work of developing education programs to spread the palliative care approach across multiple settings, specialties, and disease groups.
Keywords: continuing professional development, curriculum development, education, palliative care, palliative care approach
Introduction
A large body of evidence points to a lack of access to palliative care for patients with progressive life-limiting illnesses.1–3 This need exists across many disease groups, including cancer care and advanced heart,4,5 lung,6,7 kidney,8 and neurological disease9 among others. The need has also been described across many different settings of care where patients with palliative care needs find themselves. These are community and home care,10 hospitals,11,12 intensive care units,13,14 emergency departments (EDs),15 surgical services,16 pediatric services,17 and long-term care nursing homes.18,19
Given the large scope of needs, the provision of palliative care cannot be the sole responsibility of specialist palliative care clinicians and teams.20 Equipping health care professionals who work in these various settings and disease groups with essential skills to initiate and provide a palliative care approach is therefore paramount.21,22 This primary- or generalist-level palliative care, delivered by health care professionals who are not palliative care specialists, is referred to as the “palliative care approach.”23 It includes identifying patients with palliative care needs early in the illness trajectory, engaging in timely advance care planning and goals of care discussions, screening for physical, psychological, social, and spiritual needs, and beginning to address these. They consult or refer to palliative care specialist-level services when complex situations arise or when additional assistance is needed.
Pallium Canada (www.pallium.ca) is a nonprofit organization founded in 2000 to build primary-level palliative care capacity across Canada by spreading the palliative care approach.24 A need had been expressed by palliative care programs in several Canadian jurisdictions to collaborate on developing palliative care courses for health care professionals so as to reduce duplication of efforts, harness expertise across the country, and provide materials to educators who would otherwise not have the means to develop and distribute the courseware themselves. The collaborative effort has resulted in the Learning Essential Approaches to Palliative Care (LEAP) courseware. Various versions of the course target different care settings and disease groups.
The LEAP courses are intentionally designed to be interprofessional—specifically targeting physicians, nurses, pharmacists, and social workers—and range from one to two days in length. They are developed by content experts from across the country and are extensively peer-reviewed. The modules cover topics such as identifying patients with palliative care needs early in the illness trajectory, decision making, pain and symptom management, communication skills such as initiating a palliative care approach early and undertaking goals of care and advance care planning discussions, and addressing psychosocial and spiritual needs of patients and families.
Although most courses are designed for classroom delivery, some include online components (flipped or hybrid courses) and one version is entirely online. The classroom versions are one- or two-day courses, and class sizes are limited to about 30 participants to ensure a high degree of interactivity. Small-group, case-based learning methods are used. The courseware is available for use by undergraduate and postgraduate education programs. Some programs choose to use one entire course, whereas others select specific modules from the various LEAP courses to address their curriculum requirements.
The number of courses developed, and the number of sessions delivered has increased over the years; there are currently 20 different course versions developed or underdevelopment, each targeting different disease groups or settings of care (Table 1). In 2019 alone, 430 LEAP courses were delivered across Canada to more than 7000 health care professionals, mainly doctors, nurses, pharmacists, and social workers. This number has been increasing by 20% annually since 2014.
Table 1.
List of Learning Essential Approaches to Palliative Care Courseware (Developed and Underdevelopment as of September 2019)
| LEAP course | Targeted professionsaand settings | Description |
|---|---|---|
| LEAP Core | Family physicians, nurses, pharmacists, and social workers. Community settings (e.g., family medicine clinics, home care agencies). |
Total of 13.5 hours (two days) Classroom. E and F |
| LEAP Mini | Same as LEAP Core (see line above). | Condensed version of LEAP Core. Total of 8.5 hours (one day). Classroom. E and F |
| LEAP Long Term Care (LTC) | Family physicians, nurses, pharmacists, social workers, and PSWs/nursing aides. Long-term care facilities and nursing homes. |
Total of 13.5 hours (two days) Classroom. E |
| LEAP Renal | Physicians (e.g., nephrologists, internists), nurses, social workers, and pharmacists who care for patients with advanced kidney diseases (e.g., dialysis units). | Total of 8.5 hours (one day) Classroom. E and F |
| LEAP Oncology | Physicians (oncologists, hospitalists, family physicians, others), nurses, social workers, and pharmacists who care for patients with cancer in outpatient and inpatient cancer care settings. | Total of 8.5 hours (one day) Classroom. E |
| LEAP Paramedics | Paramedics and other emergency service (including primary, advanced care, and specialized paramedics). | Total 9 hours. E and F Flipped learning with online modules followed by classroom group learning. |
| LEAP Health Sciences | Students enrolled in undergraduate health science degree programs (excluding medical or nursing students). These students undertake further degrees in health-related professions, research, and administration. | Total of 8.5 hours (one day) Classroom. E |
| LEAP Undergraduate and Postgraduate | Medical students (undergraduate) and residents/registrars (postgraduate specialization). Students in nursing, pharmacy, social work, and other health professions. | Educators select from the many modules across the different LEAP courses and learning materials (e.g., videos) E and F |
| LEAP Facilitator Training | Palliative care physicians, nurses, social workers, and pharmacists with clinical and teaching roles who wish to facilitate LEAP courses. | Hybrid course with independent online self-learning (about 4 hours) and 7 hours hands-on classroom learning E and F |
| LEAP Taking Ownership | All health care professionals, administrators, students. Introduces palliative care approach. Also open to the public. | 40-minute online module. E and F |
| LEAP Hospital | Physicians, nurses, pharmacists, and social workers working in hospital settings (inpatient and outpatient). | Total of 8.5 hours (one day) Classroom. E |
| LEAP Emergency Department (ED) | Physicians, nurses, pharmacists, and social workers. Emergency departments. |
Total of 8.5 hours (one day) Classroom. E |
| LEAP Online | Health care professionals from different professions and PSWs. A total of 11 online modules. | Designed to support independent, flipped, or hybrid online-classroom. E |
| Under development | ||
| LEAP Liver | Physicians (internists, gastroenterologists, generalists), nurses, pharmacists, and social workers caring for patients with advanced liver diseases. One-day classroom-based course. E | |
| LEAP Pediatrics | Health care professionals caring for pediatric populations with palliative care needs. Hybrid delivery: online self-learning (about 5 hours) and classroom learning (about 8 hours). E | |
| LEAP Heart | Physicians (internists, cardiologists, generalists), nurses, pharmacists, and social workers caring for patients with advanced heart diseases. One-day classroom-based course. E | |
| LEAP Surgery | Surgeons (from different surgical fields), nurses, and social workers working in surgery programs. | |
| LEAP Lung | Physicians (internists, pulmonologists, generalists), nurses, pharmacists, and social workers caring for patients with advanced lung diseases. | |
| LEAP Leaders | Health care leaders and administrators. | |
| LEAP Paramedics online | Paramedics and other emergency service (including primary, advanced care, and specialized paramedics). | |
| LEAP In-Depth | Designed for health care professionals who are not palliative care specialists but serve as local palliative care resource persons in the services they work in and can help palliative care specialists to facilitate LEAP courses in regions where there is a shortage of palliative care specialist physicians and nurses. Completing a LEAP Core or LEAP LTC is a prerequisite. | |
| Under consideration: LEAP Carers, LEAP Forward, LEAP Intensive Care Units (ICU), LEAP Equity (inner city, vulnerable populations) | ||
E = English, F = French (The goal is to have all courses in both English and French versions).
”Nurses” includes registered nurses, nurse practitioners, licensed practical nurses, and registered practical nurses.
LEAP, Learning Essential Approaches to Palliative Care; PSWs, personal support workers.
The goal of this article is to describe Pallium Canada's Curriculum Development Framework. The framework supports large-scale development and deployment, at a national level, of palliative care-related continuous professional development (CPD) education. The framework and the LEAP courses could be useful for other countries facing the challenge of building primary-level palliative care capacity. Further details on Pallium Canada (referred as PalliumCAN in this article), the instructional designs of the LEAP courses, and their impact are presented elsewhere.
Pallium Canada's Curriculum Development Framework
In 2001, PalliumCAN adopted Kern et al.'s Johns Hopkins University curriculum development approach to develop its initial LEAP course, which targeted community-based primary care providers.25 The editions of the model were used thereafter. The approach includes six steps that start with identifying the need, followed by a needs assessment of learners, establishing the goals and learning objectives of the curriculum, and selecting the educational strategies and learning methods. Once those steps are completed, the curriculum is implemented. The final step involves evaluating the curriculum program and getting feedback from, among others, the learners. Informed by the evaluation, the cycle starts again. The important feature of the approach is its flexibility. Although the steps are sequential, one may jump between different steps if needed.
In 2012, PalliumCAN, in response to growing national demand, decided to start developing new LEAP course versions to target other settings and noncancer disease groups. No approach was found that could guide the concurrent development of deployment of multiple course versions with limited resources. As the new courses started rolling out (LEAP LTC [long-term care] in 2014, LEAP Mini in early 2015, LEAP Paramedics in late 2015, and LEAP Renal in early 2016), our efforts to maximize limited resources started evolving into the framework described in this article. It has therefore evolved organically, driven by needs, opportunities, and trial and error.
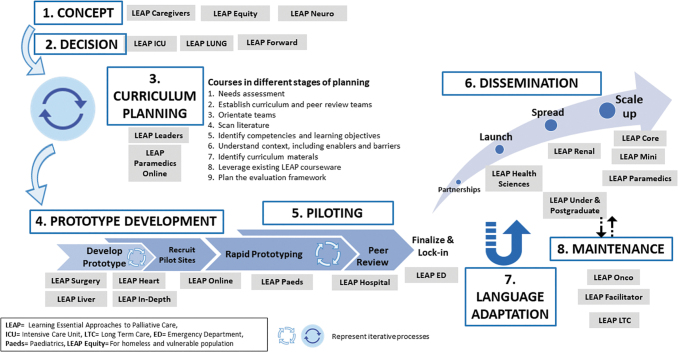
PalliumCAN's framework is made up of eight phases and incorporates the activities described in the Johns Hopkins model (Fig. 1).25 Different LEAP courses are found at different phases of production and deployment. The Kern et al.'s approach is incorporated largely into Phase 3 of the model, but activities such “Implementation” and “Evaluation and feedback” are also used in Phase 4 (Prototype Development). The framework is influenced by assembly-line methods that maximize efficiencies and allow products to be developed in stages, and air-traffic control approaches that ensure adequate time gaps (“spacing”) between products so that resources are not overwhelmed and a relatively small team is able to undertake all the work.
FIG. 1.
PalliumCAN's Curriculum Development Framework (the different LEAP courses are indicated in small gray boxes, as of December 2019). Color image is available online.
Phase 1: Concept
Ideas for new LEAP courseware continually present themselves. These are registered and triaged; ideas that most align with PalliumCAN's mission and vision are prioritized and actioned.
Phase 2: Decision
The decision to move an idea into the planning phase is influenced by several factors. These include the potential impact of the course on access to palliative care, resource requirements, funding availability, production-line capacity, and urgency of the need. Agility is needed to respond to high-impact opportunities that arise, without overwhelming PalliumCAN's resources. The LEAP Paramedics course, which targets ambulance first responders, illustrates this.26 A decision was made in 2015 to prioritize the development of that course because the provincial governments of two provinces, Nova Scotia and Princess Edward Island, identified paramedic palliative care training as a priority and allocated additional resources to support it. A similar situation arose when the Ontario Renal Network (ORN), which oversees kidney care across the province of Ontario, including dialysis services, identified palliative care as a provincial priority, resulting in the development and deployment of LEAP Renal.
PalliumCAN uses a Priority, Action, Consider, Eliminate (PACE) matrix to decide which courses to include and activate. This matrix is based on ease of implementation and anticipated impact and benefits. Courses that are relatively easy to implement and accompanied by the potential for high impact on a health care sector or disease group are slotted into the “Priority” quadrant. The entry of new courses into the planning phase is staggered so as to not overwhelm resources.
Phase 3: Curriculum Planning
Several key activities are undertaken during this phase, including a general and learner-targeted needs assessment, environmental and literature scans for relevant materials, establishing a course curriculum team and identifying the competencies and learning objectives to be addressed. The environmental scan provides an additional opportunity to decide on continuing or discontinuing course development.
Curriculum teams
Subject matter experts (SMEs) from across Canada and from different targeted professions who are considered thought leaders in the setting or disease group being targeted by the LEAP course are recruited. Representatives of the different targeted professions are included. Physician members with certification in the College of Family Physicians of Canada (CFPC) or the Royal College of Physicians and Surgeons of Canada (Royal College) are also included to ensure CPD accreditation requirements are met. An interprofessional curriculum team of four to five members is formed. This curriculum team collaborates with PalliumCAN's scientific and courseware management team to develop the course. The small team size maximizes efficiency; broader input will follow during the peer review process. The curriculum team undergoes an orientation, including the goals of the course and learning approaches to consider. The team is also given access to existing LEAP courses to facilitate the process and to increase efficiencies, as well as to ensure common messaging and design across the courses.
Environmental scan, needs assessment, and understanding the context
The team, supported by PalliumCAN's office, undertakes an environmental scan and competency development process. This includes identifying seminal publications germane to the setting or disease group, and insights from experts, stakeholders, and targeted learners. The scan also includes identifying resources and material that can be adopted, adapted, or that need to be developed de novo. In most cases, interprofessional focus groups of targeted learners are held to explore and understand the setting or disease group being targeted. These focus groups also help identify factors that can support or challenge the integration of the palliative care approach in the respective sectors and they contribute to elaborating the competencies for that setting.
Competency mapping and establishing learning objectives
PalliumCAN has used different approaches to identify the competencies for different professions in the LEAP courses, including the Developing a Curriculum (DACUM) method.27 This method uses a focus group approach that includes experienced professionals who know the role well. The competencies are reviewed periodically such as when a course undergoes a major revision. Previous sets of competencies serve as a starting point to identify the competencies and learning objectives for targeted professions in the new course. Literature scans further inform this work.
Evaluation framework
Work on the course evaluation plan and framework begins during this phase. Previous LEAP courses' instruments and methods can be leveraged, thereby streamlining the process.
Phase 4: Prototype Development
With the competencies and learning objectives delineated, the targeted sector or disease group better understood, the curriculum team sets out to develop a course prototype. This includes designing the course, selecting the appropriate learning methods, and incorporating the relevant content. Consistent with PalliumCAN's role as a Knowledge-to-Action (KTA) agent, the process includes identifying, analyzing, and synthesizing pertinent research and best practices to incorporate into the course content.28
Existing LEAP courses are used as templates for new ones. For example, LEAP Core served as a template for two-day classroom-based courses such as LEAP LTC. LEAP Mini has been a useful template for intensive one-day courses such as LEAP Hospital and LEAP ED, whereas LEAP LTC provides a template for courses that need to include breakout sessions that specifically meet the learning needs and scopes of practices of professions (e.g., personal support workers) that are generally not targeted by LEAP courses. LEAP Renal, in turn, is a useful starting point for LEAP Heart and other disease-specific course types. LEAP Facilitator training, which uses a flipped classroom approach with independent online learning followed by a one-day classroom experience, served as a template for LEAP Paramedics.
Adaptations to existing LEAP courses and materials include using learning methods that better address new competencies or setting realities, inserting evidence and studies as well as cases that are more relevant to the domain, modifying facilitator notes accordingly and, in some cases, replacing or inserting new modules. Where possible, existing material such as videos is adopted, adapted, or repackaged for the new course. In some cases, new material needs to be created de novo during this phase.
Prototype Development also includes developing the pre- and post-course quizzes and surveys, most of which are adapted from existing LEAP courses, and creating complementary materials such as facilitator and learner manuals.
While Prototype Development is underway, PalliumCAN begins to identify and recruit pilot sites and participants for the piloting phase that will follow. A purposive sampling approach is undertaken. Local palliative care teams are approached to help recruit the site and course participants. Recruitment to the pilot sessions can be challenging as prototypes generally do not yet have CPD credits; the nominal course registration fee is therefore waived.
Phase 5: Piloting
The Piloting phase consists of two critical processes: rapid prototyping and peer review. Pilot sessions are usually facilitated by curriculum team members with the assistance of other LEAP facilitators.
Rapid prototyping
The rapid prototyping approach is borrowed from industry. Desrosier has argued that it can be leveraged to meet marketplace needs while also ensuring quality standards.29 It involves iterative plan-do-study-act cycles that are used in quality improvement. Modifications are made after each pilot session, based on the input from learners and course facilitators. In our experience, between three and six pilot sessions and peer review are required to bring a prototype to a point where it is ready for launch.
Peer review
Peer review strengthens the quality, accuracy, and relevancy of the courseware and minimizes bias. It is undertaken using two methods: the first occurs concurrently with the rapid prototyping process and the second after prototyping. Course facilitators who present a prototype and who were not part of the curriculum team provide one layer of peer review. During and after piloting, the courseware is also sent to an interprofessional team of 6 to 10 reviewers who are recognized as SMEs in the field. This component of peer reviewing is blinded; neither PalliumCAN's Scientific Officer nor the curriculum team can link a comment with a specific peer reviewer.
Once final adjustments are made based on the peer review feedback, the course is “locked-in” and readied for launch. This process includes proofreading, copy-editing, and formatting of all the courseware, including the slides and course manuals. The courseware is then submitted to the CFPC and/or the Royal College for CPD accreditation. With the current resources and development processes and logistics in place, it now takes a course about 10 to 12 months to reach this stage. The length of time can vary, however, and is largely influenced by the availability of content experts (SMEs, the scientific officer, and scientific consultants), who generally have other work commitments.
Phase 6: Dissemination
PalliumCAN uses a multipronged approach to facilitate spread of the courses to the targeted learner groups and settings, and across Canadian jurisdictions. This consists of a decentralized course organization and delivery model, development of strategic partnerships, a train-the-trainer model, and an online learning management system (LMS).
With few exceptions, PalliumCAN does not organize and deliver courses itself. Rather, it relies largely on local, regional, or provincial partners to do this. Local and regional partners include regional palliative care programs, primary care clinic networks, hospital groups, home care nursing agencies, and medical and nursing schools who use the material in their CPD offerings or undergraduate and postgraduate education. Provincial partners include provincial hospice and palliative care associations, provincial and territorial health ministries or ministry programs (such as provincial cancer or renal care programs), and provincial professional bodies such as physician or nursing associations. In Ontario, Cancer Care Ontario, which oversees cancer care across the province, has promoted the LEAP Core and LEAP Oncology courses in its palliative care integration initiative. ORN, which oversees dialysis services across the province, includes LEAP Renal training as part of its initiative to integrate palliative care in the management of advanced kidney disease. The Network helps organize LEAP Renal courses across the province and subsidizes course registration. In Nova Scotia and Prince Edward Island, the provincial government emergency services programs supported the development and spread of LEAP Paramedics training to all its paramedic ambulance emergency providers. Federal organizations such as the Canadian Partnership Against Cancer and Canadian Foundation for Healthcare Improvement have helped disseminate it across other provinces.
The regional, provincial, and federal partners, which vary from province to province, promote the courses to their staff and members and usually organize several course offerings a year. Some partners organize “open” courses, which are open to registration by any health care professional in the jurisdiction. Others offer “closed” courses where registration is limited to only their staff or members as part of their CPD education. Some regional nursing home care agencies, for example, have made palliative care training of their staff obligatory. In all cases, organizers draw upon the local pool of certified LEAP facilitators to teach the various course offerings.
The large train-the-trainer program consists of more than 900 certified LEAP facilitators across the country. They are mainly palliative physicians and nurses and also include some social workers and pharmacists who work in palliative care services. The criteria for being a facilitator and the training program they undertake are described elsewhere. They download the teaching materials from the online LMS, as do registered learners. The LMS is also used to register all courses and learners, manage course registration fees, and facilitate the completion of pre- and post-course questionnaires and surveys.
The accreditation by professional organizations such as the two physician colleges of Canada serves as an additional incentive for health care professionals to register. In Canada, for example, physicians must meet annual quotas of CPD accredited activities to maintain their professional certification.
Phase 7: Language and Cultural Adaptation
Once a course is developed in English, it undergoes adaptation to French. Adaptation includes incorporating cultural sensitivities and language nuances. The process begins with the course being translated and adapted by an independent professional translation team. Once translated and adapted, it undergoes further revisions by a lead team of two or three Francophone SMEs. The course is then further reviewed by Francophone facilitators who are involved in the piloting of the French courses. Two to three pilots usually suffice. The LEAP Mini course has also been adapted to the Inuktitut language and culture to educate Inuit support workers in Canada's far north.
The experience we have gained from undertaking these adaptations in Canada and from some limited testing of course content and design in Spain (University of Navarra), Portugal, and Barbados suggests that the framework can be used in other international jurisdictions to develop new courseware de novo or to adapt the LEAP courseware to local realities and context. Some new materials such as communication videos would need to be developed. Activities in Phase 3 can be used to understand the local context, a curriculum team could be established to make the modifications in Phase 4, and the prototype can be piloted in Phase 5. These would replace the need for Phase 7 (Language and Cultural Adaptation).
Phase 8: Update and Maintenance
Each course undergoes an annual update, and a major revision every three years. These are informed by the evaluations received from learners and feedback from facilitators. Curriculum teams are re-established for the major revisions. They consist of some original curriculum team members and additional new ones to encourage further innovation and increase objectivity. If the modifications are considerable, the courses may be re-piloted and re-submitted to peer-review. Course changes also require resubmission for CPD credits to the CFPC and Royal College.
A triage process is in place to manage corrections or modifications that need to be made to the courseware. Suggestions for changes are usually brought to PalliumCAN's attention by its scientific team and scientific advisors, LEAP facilitators, or learners. Suggestions for changes are triaged into one of three categories, “Emergent,” “Urgent,” or “Minor.” Changes that are deemed “Emergent” are errors or new information that may place patients at risk. These changes are made immediately, and notices are sent to all LEAP facilitators to bring these to their attention. Examples include medication warnings or withdrawals issued by Health Canada, or new legislation. “Urgent” changes are made during the annual updates. These include information that does not place patients at risk, such as changes in medication coverage by Canadian provincial insurers. “Minor” changes, such as spelling errors, are scheduled for course revisions every three years.
Preconditions and Factors for Success
The multiple activities described in the framework, including the infrastructure, resources, and logistics that support them, require funding. The main source of funding has been federal government grants and provincial ministry initiatives have supported some of the work. However, government funding is not guaranteed and sometimes insufficient. From 2008 to 2012, for example, PalliumCAN received no government grants, prompting it in 2014 to adopt a social enterprise model in which revenues received from course registration fees help support the work and ensure program sustainability. This model has been refined in the last two years and now supports a large part of the framework's infrastructure and some of PalliumCAN's other activities, including its Compassionate Communities work. The funding that PalliumCAN receives and its revenues from course fees is able to support activities only within Canada. PalliumCAN continues to seek funding to support international collaborations.
PalliumCAN currently has a staff of 18 full- or part-time persons, of which approximately eight have roles that exclusively or mostly relate to courseware development, deployment, and spread. Honoraria are offered to the core curriculum team members of the various LEAP courses, peer reviewers, and scientific consultants.
Earlier LEAP courses serve as templates for new courses, creating considerable efficiencies and economies-of-scale that facilitate the development of multiple LEAP courses. Many of the modules can be adopted or adapted for new LEAP course versions.
The large community of committed SMEs who participate in the various LEAP curriculum and peer review teams represents a major asset and factor for success, as does the large pool of LEAP facilitators. The latter are remunerated by the local organizers, usually through course registration fees or other subsidies.
Strategic partnerships with regional, provincial, territorial, and federal entities play a critical role in the spread and scale up of courses within and across Canadian jurisdictions. This continues to be a major driver of success, and significant efforts are invested into nurturing and supporting established partnerships and securing new ones. PalliumCAN has, for example, employed business development staff to support this work.
Challenges and Limitations
A major challenge, which occasionally results in curriculum delays, relates to the heavy workloads and multiple responsibilities that many SMEs and scientific consultants already carry in their regular work roles. The support offered by the PalliumCAN courseware team mitigates some of this. This support includes assistance with setting up the teams and coordinating team meetings, literature searches, recruiting and organizing pilot sites, coordinating peer review processes, collating feedback, and copy-editing slides and facilitator notes.
Curriculum development work was previously limited by funding limitations. The adoption of a social enterprise funding model has reduced this limitation, providing more flexibility on which courses to develop and update.
Finally, it is important to note that the framework depicts the curriculum development phases and their associated activities as a sequenced process. The work is, however, often nonlinear and iterative. Circular symbols in Figure 1 highlight the phases that are iterative and sometimes nonlinear activities. Situations also arise that require backtracking or revisiting a previously completed phase.
Conclusions
PalliumCAN's Curriculum Development Framework provides an approach that helps address the pressing need of developing palliative care education programs for multiple settings and disease groups. It supports the concurrent development and deployment of several courses by leveraging existing courses, materials and experiences, and maximizing efficiencies. Content and message alignment across courses are made possible by using some of the existing courses as “templates” for the development of new ones. Each course reflects the context and realities of the targeted setting or disease group.
The framework can be used to develop multiple courses de novo in other international jurisdictions. In our experience, the work of developing, deploying, spreading, and maintaining education programs across multiple settings and on a large scale requires sustained funding and resources. The use of pre-existing courseware such as the LEAP courses as a starting point would create significant efficiencies.
Acknowledgments
We wish to thank the entire PalliumCAN community who have contributed to building PalliumCAN, the LEAP courses, and this framework, particularly all the colleagues who over the years have participated in the LEAP course curriculum and peer review teams. We also wish to thank the LEAP course facilitators whose contributions are a key success factor of PalliumCAN.
Funding Information
The work described in this article has been largely funded by grants from Health Canada, the Canadian Federal Health Ministry (2001 to current). Some of the work undertaken between 2012 and 2015 was aided by a generous grant from a private benefactor (the estate of Mr. Patrick Gillin). Some key operations are currently funded by revenues generated from course registration fees.
Author Disclosure Statement
Some of the authors are current employees of PalliumCAN (JP, JM, JF, DV, BR, TT, and LN). SC is a board member of PalliumCAN's Foundation (unpaid).
References
- 1. Traue DC, Ross JR: Palliative care in non-malignant diseases. J R Soc Med 2005;98:503–506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Murray SA, Boyd K, Kendall M, et al. : Dying of lung cancer or cardiac failure: Prospective qualitative interview study of patients and their carers in the community. BMJ 2002;325:929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Solano JP, Gomes B, Higginson IJ: A comparison of symptom prevalence in far advanced cancer, AIDS, heart disease, chronic obstructive pulmonary disease and renal disease. J Pain Symptom Manage 2006;31:58–69 [DOI] [PubMed] [Google Scholar]
- 4. Goodlin S: Palliative care in congestive heart failure. J Am Coll Cardiol 2009;54:386–396 [DOI] [PubMed] [Google Scholar]
- 5. McIlvennan CK, Allen LA: Palliative care in patients with heart failure. BMJ 2016;53:i1010. [DOI] [PubMed] [Google Scholar]
- 6. Hardin KA, Meyers F, Louie S: Integrating palliative care in severe chronic obstructive lung disease. COPD 2008;5:207–220 [DOI] [PubMed] [Google Scholar]
- 7. Rocker GM, Sinuff T, Horton R, Hernandez P: Advanced chronic obstructive pulmonary disease: Innovative approaches to palliation. J Palliat Med 2007;10:783–797 [DOI] [PubMed] [Google Scholar]
- 8. Davison SN: End-of-life care preferences and needs: Perceptions of patients with chronic kidney disease. Clin J Am Soc Nephrol 2010;5:195–204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gofton TE, Jog MS, Schulz V: A palliative approach to neurological care: A literature review. Can J Neurol Sci 2009;36:296–302 [DOI] [PubMed] [Google Scholar]
- 10. Thomas K, Noble B: Improving the delivery of palliative care in general practice: An evaluation of the first phase of the Gold Standards Framework. Palliat Med 2007;21:49–53 [DOI] [PubMed] [Google Scholar]
- 11. Gott M, Ingleton C, Bennett MI, Gardiner C: Transitions to palliative care in acute hospitals in England: Qualitative study. BMJ 2011;342:d1773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Edmonds P, Karlsen S, Addington-Hall J: Palliative care needs of hospital inpatients. Palliat Med 2000;14:227–228 [DOI] [PubMed] [Google Scholar]
- 13. Aslakson RA, Curtis JR, Nelson JE: The changing role of palliative care in the ICU. Crit Care Med 2014;42:2418–2428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mosenthal AC, Weissman DE, Curtis JR, et al. : Integrating palliative care in the surgical and trauma intensive care unit: A report from the Improving Palliative Care in the Intensive Care Unit (IPAL-ICU) Project Advisory Board and the Center to Advance Palliative Care. Crit Care Med 2012;40:1199–1206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Smith AK, Fisher J, Schonberg MA, et al. : Am I doing the right thing? Provider perspectives on improving palliative care in the emergency department. Ann Emerg Med 2009;54:86–93, 93.e1. [DOI] [PubMed] [Google Scholar]
- 16. Hahne P, Lundström S, Leveälahti H, et al. : Changes in professionals' beliefs x2following a palliative care implementation programme at a surgical department: A qualitative evaluation. BMC Palliat Care 2017;16:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Baughcum AE, Gerhardt CA, Young-Saleme T, et al. : Evaluation of a pediatric palliative care educational workshop for oncology fellows. Pediatr Blood Cancer 2007;49:154–159 [DOI] [PubMed] [Google Scholar]
- 18. Kristjanson LJ, Walton J, Toye C: End-of-life challenges in residential aged care facilities: A case for a palliative approach to care. Int J Palliat Nurs 2005;11:127–129 [PubMed] [Google Scholar]
- 19. Brazil K, Bédard M, Krueger P, et al. : Barriers to providing palliative care in long-term care facilities. Can Fam Physician 2006;52:472–473 [PMC free article] [PubMed] [Google Scholar]
- 20. Quill TE, Abernethy AP: Generalist plus specialist palliative care—Creating a more sustainable model. N Engl J Med 2013;368:1173–1175 [DOI] [PubMed] [Google Scholar]
- 21. Osborn R, Moulds D, Schneider EC, et al. : Primary care physicians in ten countries report challenges caring for patients with complex health needs. Health Aff (Millwood) 2015;34:2104–2112 [DOI] [PubMed] [Google Scholar]
- 22. Stajduhar KI, Tayler C: Taking an “upstream” approach in the care of dying cancer patients: The case for a palliative approach. Can Oncol Nurs J 2014;24:144–153 [PubMed] [Google Scholar]
- 23. Sawatzky R, Porterfield P, Lee J, et al. : Conceptual foundations of a palliative approach: A knowledge synthesis. BMC Palliat Care 2016;15:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Aherne M, Pereira JL: Learning and development dimensions of a pan-Canadian primary health care capacity-building project. Leadersh Heal Serv 2008;21:229–266 [Google Scholar]
- 25. Thomas PA, Kern DE, Hughes MT, Chen BY (eds): Curriculum Development for Medical Education: A Six-Step Approach, 3rd ed. Baltimore, MD: Johns Hopkins University Press, 2015 [Google Scholar]
- 26. Carter AJE, Arab M, Harrison M, et al. : Paramedics providing palliative care at home: A mixed-methods exploration of patient and family satisfaction and paramedic comfort and confidence. CJEM 2019;21:513–522 [DOI] [PubMed] [Google Scholar]
- 27. Cooper D, Aherne M, Pereira J; Pallium Spiritual Care Providers DACUM Group: The competencies required by professional hospice palliative care spiritual care providers. J Palliat Med 2010;13:869–875 [DOI] [PubMed] [Google Scholar]
- 28. Straus SE, Tetroe J, Graham I: Defining knowledge translation. CMAJ 2009;181:165–168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Desrosier J: Rapid prototyping reconsidered. J Contin High Educ 2011;59:135–145 [Google Scholar]