Abstract
Background: Patient navigation is increasingly being used by pediatric health care delivery systems to address patients’ unmet social needs. However, it is not known whether navigators working remotely can be as effective at linking families to community resources as on-site navigators. The aim of this study was to assess whether a patient navigator located on-site versus remotely is more likely to receive referrals from clinicians, successfully follow-up with patients, and assist families with enrollment in social needs resources. Methods: A patient navigator worked on-site and remotely as she divided her time between 4 federally qualified health centers (FQHCs) from May 2015 to June 2019. We conducted a 1-sample test of proportion comparing the proportion of on-site referrals made with the proportion of the week spent in each FQHC. To assess the impact of on-site versus remote referrals on number of contacts with a family, we conducted a 2-sample t test. We used chi-square testing to assess the effect of on-site versus remote status on resource enrollment. Results: Of the referrals (N = 414) made to the patient navigator, the majority were made through the electronic health record (83%) versus in person (17%) (P < .0001). When the navigator was on-site, significantly more referrals were made than expected (45% vs 29%, P < .0001). Between remote and on-site referral groups, there was no significant difference in number of contact points (1.0 vs 1.1 points, P = .32) or in the proportion of families who received a resource (4.6% vs 5.1%, P = .31). Conclusion: Our results indicate that clinicians were significantly more likely to refer families to patient navigation if the navigator was on-site. The likelihood of having contact with the navigator and enrolling in a resource, however, did not differ between families referred when the patient navigator was on-site compared with remote.
Keywords: pediatrics, primary care, community health centers, social determinants of health, unmet needs, patient navigator
Background
Children are the poorest segment of the US population. Childhood exposure to social adversities such as food and housing insecurity is linked to negative health outcomes such as obesity, cardiovascular disease, diabetes, and asthma as well as earlier mortality.1-6 These social adversities disproportionately affect low-income and racial minority populations.6 In 2016, the American Academy of Pediatrics recommended screening for social determinants of health at pediatric visits, thus sparking increased adoption of social needs interventions by pediatric clinical practices. Many of these interventions are innovatively using a patient navigator to help families with unmet social needs receive community-based resources and public benefits.
Patient navigators have been widely implemented in cancer care programs to address the complex medical and social needs of patients. In these settings, the use of patient navigators has produced increased rates of cancer screening, adherence to treatment, and patient satisfaction while decreasing patient anxiety.7-9 Regarding the use of patient navigation for addressing families’ social needs, the evidence base is still scant. One study found that compared with patients who receive only written materials on community services, patients who receive on-site patient navigation services report reductions in unmet social needs and improvements in parent-reported child health outcomes,10 while another similar study found no difference between the 2 groups.11
As patient navigation interventions have expanded into pediatric health care delivery systems, issues have arisen regarding implementation barriers and utilization of these interventions.12 Unfortunately, while in-person patient navigation is preferred by patients and physicians, it is often not feasible due to lack of financial resources and space.12,13 As a result, patient navigators may need to work remotely. Previous studies have also found that face-to-face meetings with patients are a key element to complex care coordination,13-15 and this is often cited as an argument for having on-site patient navigators.12 However, it is currently unclear whether patient navigators working remotely are as effective at linking families to resources for addressing unmet social needs as on-site navigators.
The goals for this study were to assess whether a patient navigator located on-site versus remotely is more likely to receive referrals from clinicians, successfully follow-up with patients, and assist families with enrollment in social needs resources.
Methods
A patient navigator was embedded at 4 federally qualified health centers (FQHCs) as part of a cluster randomized control trial (RCT) testing the effectiveness and implementation of a social needs screening and referral care model (WE CARE [Well-child care, Evaluation, Community resources, Advocacy, Referral, Education]) in pediatric primary care from May 2015 to June 2019. Efficacy of WE CARE on increasing parental receipt of community resources was previously demonstrated in an RCT in 8 urban community health centers.16 The navigator’s primary task during this study was to connect parents with unmet social needs to community-based health and social services. The patient navigator typically worked with parents of children aged 0 to 2 years due to the RCT’s primary focus, but accepted parents of older children with social needs on a case-by-case basis. Because most adults working with the patient navigator were parents, we use the term parents to include all caregivers (parents and other legal guardians including foster parents). The patient navigator worked both on-site and remotely as she divided her time between the FQHCs and spent an average of 29% of the week at each location, equaling approximately 1.5 weekdays per week per FQHC.
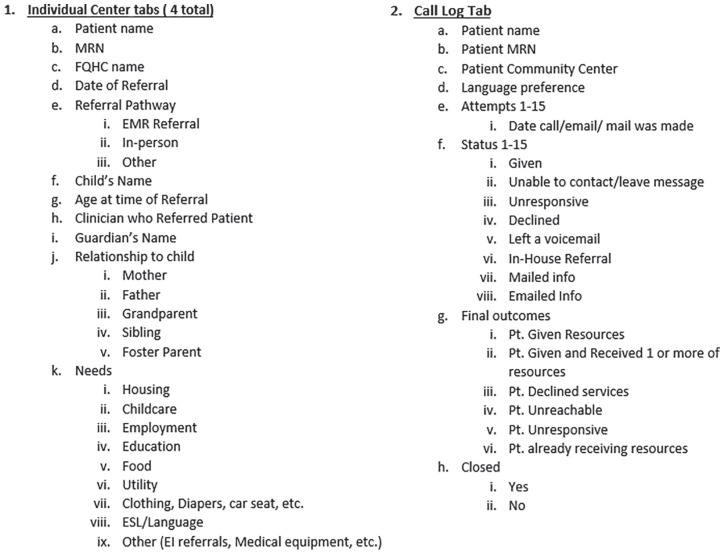
During the study period, clinicians would assess families’ unmet social needs with the help of the WE CARE paper self-assessment tool given to parents of pediatric patients at well-child care visits. If a clinician determined a family had unmet social needs, they were instructed to print a resource information sheet directly from the patient’s electronic health record (EHR) using smart phrases specific for each need. For instance, if a clinician used the smart phrase “.WECAREHousing” in the After Visit Summary (AVS) section of the visit note, housing resource information would populate into the AVS which was provided to parents at the end of each visit. Additionally, clinicians were instructed to make a referral to the patient navigator through the EHR, or, if the patient navigator was on-site and space was available, she could be called into the room to meet with the family face-to-face. The patient navigator kept records of each referral in a Microsoft Excel patient database (Figure 1). The Boston University Medical Campus Institutional Review Board approved this study (H-33061), and provided a waiver of consent because the research did not present more than minimal risk of harm to subjects and did not involve procedures for which written consent is normally required outside of the research context.
Figure 1.
Microsoft Excel patient database outline.
Data Analysis
We coded each clinician referral to the patient navigator as “on-site” or “remote” depending on whether the patient navigator was present at the FQHC the day the referral was made. We then reviewed the navigator’s database which recorded the number of successful contacts with each family (ie, instances where the patient navigator and family spoke in person or over the phone, not including voicemail) and documented whether the family received and/or enrolled in a resource. We conducted a 1-sample test of proportion comparing the proportion of on-site referrals made with the proportion of the week the patient navigator spent in each FQHC. To assess the impact of on-site versus remote navigation on the number of contacts with a family, we conducted a 2-sample t test. We used chi-square testing to assess the effect of on-site versus remote status on enrollment in a resource. A total of 30 families were already enrolled in the resource the patient navigator was offering and were not included in final calculations for enrollment in resources.
Results
A total of 414 parents were referred to the patient navigator during the study period. Overall, the majority of parents were Black or African American (63.8%), not Hispanic or Latino (69.3%), English speaking (75%), and publicly insured (90.8%) (Table 1). The average age of referred patients was 1.7 years (SD, 4.6 years; range, 0-42 years of age). The most common unmet needs requiring assistance were childcare (42% of families), housing (29% of families), and utilities (21% of families) (Table 2).
Table 1.
Sociodemographics of Children Referred to Patient Navigator, Stratified by Referral Type, Number of Patient Navigator Contacts, and Enrollment in Resources.
| Overall |
Remote |
On-site |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Total | Contacts | Enrolled | Total | Contacts | Enrolled | ||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | |
| Sex | 414 | 229 | 55.3 | 233 | 53.2 | 17 | 7.4 | 185 | 44.7 | 205 | 46.8 | 18 | 10.4 | |
| Female | 199 | 48.1 | 106 | 46.3 | 110 | 47.2 | 7 | 41.2 | 93 | 50.3 | 106 | 51.7 | 10 | 55.6 |
| Male | 215 | 51.9 | 123 | 53.7 | 123 | 52.8 | 10 | 58.8 | 92 | 49.7 | 99 | 48.3 | 8 | 44.4 |
| Race | ||||||||||||||
| American Indian/Alaska Native | 1 | 0.2 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0.5 | 0 | 0 | 0 | 0 |
| Asian | 21 | 5.1 | 12 | 5.2 | 14 | 6.0 | 2 | 11.8 | 9 | 4.9 | 9 | 4.4 | 0 | 0 |
| Black or African American | 264 | 63.8 | 149 | 65.1 | 149 | 63.9 | 9 | 52.9 | 115 | 62.2 | 124 | 60.5 | 12 | 66.7 |
| Native Hawaiian or Other Pacific Islander | 5 | 1.2 | 3 | 1.3 | 3 | 1.3 | 1 | 5.9 | 2 | 1.1 | 0 | 0 | 0 | 0 |
| White | 29 | 7 | 14 | 6.1 | 16 | 6.9 | 1 | 5.9 | 15 | 8.1 | 21 | 10.2 | 3 | 16.7 |
| Unreported/unknown | 94 | 22.7 | 51 | 22.3 | 51 | 21.9 | 4 | 23.5 | 43 | 23.2 | 51 | 24.9 | 3 | 16.7 |
| Ethnicity | ||||||||||||||
| Hispanic or Latino | 82 | 19.8 | 43 | 18.8 | 40 | 17.2 | 3 | 17.6 | 39 | 21.1 | 39 | 19 | 5 | 27.8 |
| Not Hispanic or Latino | 287 | 69.3 | 160 | 69.9 | 164 | 70.4 | 11 | 64.7 | 127 | 68.7 | 135 | 65.9 | 10 | 55.6 |
| Unreported/unknown | 45 | 10.9 | 26 | 11.4 | 29 | 12.4 | 3 | 17.6 | 19 | 10.3 | 31 | 15.1 | 3 | 16.7 |
| Language | ||||||||||||||
| Cape Verdean Creole | 26 | 6.3 | 14 | 6.1 | 19 | 8.2 | 1 | 5.9 | 12 | 6.5 | 14 | 6.9 | 0 | 0 |
| English | 310 | 75 | 171 | 74.7 | 163 | 70.0 | 12 | 70.6 | 139 | 75.5 | 148 | 72.2 | 17 | 94.4 |
| French Creole | 5 | 1.2 | 2 | 0.9 | 1 | 0.4 | 0 | 0 | 3 | 1.6 | 4 | 2 | 0 | 0 |
| Haitian Creole | 10 | 2.4 | 8 | 3.5 | 11 | 4.7 | 0 | 0 | 2 | 1.1 | 6 | 2.9 | 0 | 0 |
| Spanish | 38 | 9.2 | 18 | 7.9 | 21 | 9.0 | 2 | 11.8 | 20 | 10.9 | 22 | 10.7 | 1 | 5.6 |
| Vietnamese | 14 | 3.4 | 8 | 3.5 | 11 | 4.7 | 1 | 5.9 | 6 | 3.3 | 8 | 3.9 | 0 | 0 |
| Other | 8 | 1.9 | 7 | 3.1 | 6 | 2.6 | 1 | 5.9 | 1 | 0.5 | 1 | 0.5 | 0 | 0 |
| Unreported/unknown | 3 | 0.7 | 1 | 0.4 | 1 | 0.4 | 0 | 0 | 1 | 0.5 | 2 | 1 | 0 | 0 |
| Insurance | ||||||||||||||
| Private | 21 | 5.1 | 11 | 4.8 | 15 | 6.4 | 1 | 5.9 | 10 | 5.4 | 12 | 5.9 | 0 | 0 |
| Public | 376 | 90.8 | 207 | 90.4 | 208 | 89.3 | 14 | 82.4 | 169 | 91.4 | 190 | 92.7 | 17 | 94.4 |
| No insurance listed | 17 | 4.1 | 11 | 4.8 | 10 | 4.3 | 2 | 11.8 | 6 | 3.2 | 3 | 1.5 | 1 | 5.6 |
Table 2.
Unmet Needs of Families Referred to Patient Navigator.
| Unmet need | Total |
On-site |
Remote |
|||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Childcare | 173 | 41.8 | 79 | 42.9 | 94 | 41.2 |
| Clothing, diapers, baby supplies | 56 | 13.5 | 25 | 13.6 | 31 | 13.6 |
| Employment | 78 | 18.8 | 33 | 17.9 | 45 | 19.7 |
| Food | 70 | 16.9 | 34 | 18.5 | 36 | 15.8 |
| Housing | 120 | 29.0 | 50 | 27.2 | 70 | 30.7 |
| Language/ESL | 37 | 8.9 | 16 | 8.7 | 21 | 9.3 |
| Parental education | 39 | 9.4 | 21 | 11.4 | 18 | 7.9 |
| Utilities | 85 | 20.5 | 39 | 21.2 | 46 | 20.3 |
| Other (early intervention, medical devices, etc) | 50 | 12.1 | 28 | 15.2 | 22 | 23.4 |
Abbreviation: ESL, English as second language.
The referrals ranged from 55 to 135 per FQHC. The majority of clinician referrals were made through the EHR (83%) versus in person (16%) (P < .0001). When the patient navigator was on-site, the majority of referrals (67%) were still placed through the EHR rather than in person (32%). However, when the patient navigator was on-site, significantly more referrals were made than expected (45% vs 29%, P < .0001). The number of referrals by type (on-site vs remote) differed significantly between study sites (P < .0001). A total of 298 (72%) families were successfully contacted. Between remote and on-site referral groups, there was no significant difference in the number of successful contacts with families (1.0 vs 1.1 points, P = .32) or in the proportion of families who enrolled in a resource (10.4% vs 8.1%, P = .43).
Discussion
In this study, we found that the benefits of an on-site navigator rather than a remote navigator were seen only with regard to the number of referrals made to the navigator. Once patients were referred to the patient navigator, there was no significant difference between the 2 groups in terms of successful contacts with families or enrollment of families in resources. These findings provide practical implications for pediatric practices seeking guidance on how to best utilize patient navigators despite limited space and financial resources.
Referral of Families With Unmet Needs
While on-site patient navigation did not result in more successful contacts with families or increase the percentage of families who enrolled in a resource, it did produce a higher percentage of referrals. A previous study in urban pediatric practices found that fewer than half of families with unmet needs received referrals from their providers, even though their providers had access to information on resources to make such referrals.17 Our study results indicate that an on-site patient navigator may help providers identify families with unmet social needs which likely would have been missed if the navigator had been working remotely. These results may be explained by the fact that when the patient navigator was on-site, she did not have a designated office space. Instead, she typically was seated somewhere in the FQHC’s pediatric department where she greeted providers. It is possible that seeing and briefly interacting with the patient navigator in the office primed clinicians to refer patients to her for assistance.
Contact With Families and Enrollment in Resources
Since we did not find a significant benefit of on-site patient navigation over remote navigation in regard to number of contacts with families and enrollment of families in resources, our results suggest that a remote patient navigator may be just as effective as an on-site patient navigator once families are referred to them. However, these findings differed from the findings of previous studies that found in-person care coordination services to be more effective than remote services.14,15 A possible explanation for this difference is while in these previous studies, the successful in-person care coordinators had frequent face-to-face communication with their patients and the remote coordinators used phone calls and email, the patient navigator in our study used similar methods to maintain contact with patients in both referral groups. While 32% of patients in the on-site referral group were able to initially meet with the patient navigator in person, follow-up contacts in both groups were usually completed remotely using email or phone calls. As previous studies have found, relatively frequent in-person contact with families may be required to establish the patient navigator as a trusted member of families’ care networks.12,14,15
Strengths and Limitations
To our knowledge, this is the first study to quantitatively assess the impact of an on-site versus remote patient navigator. This study is limited because it only focuses on one individual working in a small number of practices. Additionally, we were only able to access data on patients once they were referred to the patient navigator. Because we were not able to access practice-level data such as total number of patients seen and total number of patients with unmet needs, we must assume that the number of families with unmet needs seen at each FQHC was equal each day of the week. Additionally, more information such as total patient volume is needed to assess why the sites differed in terms of referral type.
While we refer to the patient navigator as “remote” throughout this article, it is important to remember that she spent an average of 1.5 days per week on-site at each FQHC. This factor potentially allowed the patient navigator to more easily create and maintain working relationships with providers and staff at each site. Conversely, the fact that the navigator was dividing her time between 4 locations may have negatively impacted these working relationships as well. Previous research involving a single patient navigator shared between multiple practices found that this factor made fully integrating the navigator into the practice challenging and may have impacted the navigator’s ability to reach patients.12 Therefore, caution should be taken when applying these results to full-time on-site or remote navigators.
Conclusion
Patient navigation can offer valuable services for families with unmet social needs. Yet, while these services are available, many families with needs may not be appropriately referred. Our results indicate that clinicians were significantly more likely to refer families to patient navigation if the navigator was on-site compared with working remotely. We hypothesize that this difference is the result of brief interactions between the patient navigator and the referring clinicians. The likelihood of having contact with the navigator and enrolling in a resource, however, did not differ between families referred when the patient navigator was on-site compared to remote. Further mixed-methods studies are needed to understand how best to optimize the integration of patient navigators into primary care to address patients’ and families’ unmet social needs.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The authors were supported an R01 grant from the NIH National Institute on Minority Health and Health Disparities (R01MD007793).
ORCID iD: Emily Messmer  https://orcid.org/0000-0003-2430-1257
https://orcid.org/0000-0003-2430-1257
References
- 1. Fieldston ES, Zaniletti I, Hall M, et al. Community household income and resource utilization for common inpatient pediatric conditions. Pediatrics. 2013;132:e1592-e1601. doi: 10.1542/peds.2013-0619 [DOI] [PubMed] [Google Scholar]
- 2. Shonkoff JP, Garner AS; Committee on Psychosocial Aspects of Child and Family Health; Committee on Early Childhood, Adoption, and Dependent Care; Section on Developmental and Behavioral Pediatrics. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129:e232-e246. doi: 10.1542/peds.2011-2663 [DOI] [PubMed] [Google Scholar]
- 3. National Scientific Council on the Developing Child; National Forum on Early Childhood Policy and Preograms. The foundations of lifelong health are built in early childhood. Accessed April 20, 2020 https://developingchild.harvard.edu/resources/the-foundations-of-lifelong-health-are-built-in-early-childhood/
- 4. Bauman LJ, Silver EJ, Stein REK. Cumulative social disadvantage and child health. Pediatrics. 2006;117:1321-1328. doi: 10.1542/peds.2005-1647 [DOI] [PubMed] [Google Scholar]
- 5. Alaimo K, Olson CM, Frongillo EA., Jr. Food insufficiency and American school-aged children’s cognitive, academic, and psychosocial development. Pediatrics. 2001;108:44-53. [PubMed] [Google Scholar]
- 6. Braveman P, Barclay C. Health disparities beginning in childhood: a life-course perspective. Pediatrics. 2009;124(suppl 3):S163-S175. doi: 10.1542/peds.2009-1100D [DOI] [PubMed] [Google Scholar]
- 7. Wells KJ, Battaglia TA, Dudley DJ, et al. ; Patient Navigation Research Program. Patient navigation: state of the art or is it science? Cancer. 2008;113:1999-2010. doi: 10.1002/cncr.23815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Freund KM, Battaglia TA, Calhoun E, et al. Impact of patient navigation on timely cancer care: The patient navigation research program. J Natl Cancer Inst. 2014;106:dju115. doi: 10.1093/jnci/dju115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Battaglia TA, Darnell JS, Ko N, et al. The impact of patient navigation on the delivery of diagnostic breast cancer care in the National Patient Navigation Research Program: a prospective meta-analysis. Breast Cancer Res Treat. 2016;158:523-534. doi: 10.1007/s10549-016-3887-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gottlieb LM, Hessler D, Long D, et al. Effects of social needs screening and in-person service navigation on child health: a randomized clinical trial. JAMA Pediatr. 2016;170:e162521. doi: 10.1001/jamapediatrics.2016.2521 [DOI] [PubMed] [Google Scholar]
- 11. Gottlieb LM, Adler NE, Wing H, et al. Effects of in-person assistance vs personalized written resources about social services on household social risks and child and caregiver health: a randomized clinical trial. JAMA Netw Open. 2020;3:e200701. doi: 10.1001/jamanetworkopen.2020.0701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ferrante JM, Cohen DJ, Crosson JC. Translating the patient navigator approach to meet the needs of primary care. J Am Board Fam Med. 2010;23:736-744. doi: 10.3122/jabfm.2010.06.100085 [DOI] [PubMed] [Google Scholar]
- 13. Wood D, Winterbauer N, Sloyer P, et al. A longitudinal study of a pediatric practice-based versus an agency-based model of care coordination for children and youth with special health care needs. Matern Child Health J. 2009;13:667-676. doi: 10.1007/s10995-008-0406-5 [DOI] [PubMed] [Google Scholar]
- 14. McAllister JW, Presler E, Cooley WC. Practice-based care coordination: a medical home essential. Pediatrics. 2007;120:e723-e733. doi: 10.1542/peds.2006-1684 [DOI] [PubMed] [Google Scholar]
- 15. Peikes D, Chen A, Schore J, Brown R. Effects of care coordination on hospitalization, quality of care, and health care expenditures among Medicare beneficiaries 15 randomized trials. JAMA. 2009;301:603-618. doi: 10.1001/jama.2009.126 [DOI] [PubMed] [Google Scholar]
- 16. Garg A, Toy S, Tripodis Y, Silverstein M, Freeman E. Addressing social determinants of health at well child care visits: a cluster RCT. Pediatrics. 2015;135:e296-e304. doi: 10.1542/peds.2014-2888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Fleegler EW, Lieu TA, Wise PH, Muret-Wagstaff S. Families’ health-related social problems and missed referral opportunities. Pediatrics. 2007;119:e1332-e1341. doi: 10.1542/peds.2006-1505 [DOI] [PubMed] [Google Scholar]