Abstract
Background: Prehabilitation to maximize exercise capacity before lung cancer surgery has the potential to improve operative tolerability and patient outcomes. However, translation of this evidence into clinical practice is limited. Aims: To determine the acceptability and perceived benefit of prehabilitation in lung cancer among thoracic surgeons. Procedure: 198 cardiothoracic surgeons within Australia and New Zealand were surveyed to evaluate their attitudes and perceived benefits of prehabilitation in lung cancer. Results: Response rate was 14%. A moderate proportion of respondents reported that there is a need to refer lung resection patients to preoperative physiotherapy/prehabilitation, particularly high-risk patients or those with borderline fitness for surgery. 91% of surgeons were willing to delay surgery (as indicated by cancer stage/type) to optimize patients via prehabilitation. The main barriers to prehabilitation reported were patient comorbidities and access to allied health professionals, with 33% stating that they were unsure who to refer to for prehabilitation in thoracic surgery. This is despite 60% of the cohort reporting that pulmonary rehabilitation is available as a preoperative resource. 92% of respondents believe that further research into prehabilitation in lung cancer is warranted. Conclusion: The benefits of prehabilitation for the oncology population have been well documented in the literature over recent years and this is reflected in the perceptions surgeons had on the benefits of prehabilitation for their patients. This survey demonstrates an interest among cardiothoracic surgeons in favor of prehabilitation, and therefore further research and demonstration of its benefit is needed in lung cancer to facilitate implementation into practice.
Keywords: lung cancer, exercise, prehabilitation, surgery, exercise capacity, survey
Background
Prehabilitation is described as a
process on the continuum of care that occurs between the time of cancer diagnosis and the beginning of acute treatment, includes physical and psychological assessments that establish a baseline functional level, identifies impairments, and provides targeted interventions that improve a patient’s health to reduce the incidence and severity of current and future impairments (p. 716).1
Prehabilitation programs may include one or more of the following: exercise, smoking cessation, dietary intervention, psychological assessment, and medical optimization; however, the optimal combination of these components in the context of lung cancer remains unknown. In the context of lung cancer, prehabilitation programs usually target patients who are awaiting lung resection and the primary goal of the program is to increase functional exercise capacity. Interventions that aim to maximize functional exercise capacity in the time available before surgery (prehabilitation) have the potential to improve operative tolerability and this is supported by emerging evidence. Systematic reviews demonstrate “proof of principle” supporting the safety and feasibility of prehabilitation in several cancer tumor streams including lung cancer and show that prehabilitation may also be associated with improved functional exercise capacity and patient-reported outcomes.2
Prehabilitation in lung cancer provides an opportunity for physiological assessment of the patient and multidisciplinary workup prior to surgery. It is known that individuals with lung cancer experience a high symptom burden and present with reduced levels of physical activity prior to surgery.3 This poses a significant risk for patients with operable lung cancer, as it is recognized that low cardiorespiratory fitness prior to lung surgery is predictive of poor postoperative outcomes.4,5 This presents a strong case for prehabilitation, as improved fitness prior to lung cancer surgery is shown to halve the rate of postoperative complications and reduce hospital length of stay.2,6,7 Despite this evidence, and current randomized controlled trials (6 international studies registered on Clinical trials.gov) attempting to determine the ideal mode, optimal timing, and patient selection for prehabilitation in lung cancer, translation into practice remains stagnant.
Barriers to the implementation of robust prehabilitation programs for patients with lung cancer include the traditional hurdles of funding, clinician knowledge, and acceptability, as well as healthcare system–related factors such as access to programs.8,9 Another factor to consider is the referral basis for prehabilitation, with thoracic surgeons acting as the main “gatekeepers” to this service. Since the inception of prehabilitation, little research has been dedicated to uncovering the perceptions or attitudes to prehabilitation among these gatekeepers. Only one article to date examined the perceptions of both anesthetists and colorectal surgeons to prehabilitation in the colorectal cancer patient population.10 The results of this research demonstrate clear recognition of the association between functional capacity and postoperative outcomes among both anesthetists and surgeons. This cross-sectional survey concluded that there is a “window of opportunity” for prehabilitation within the colorectal cancer cohort of 2 to 4 weeks after cancer diagnosis and recommended that further multicenter or implementation studies are required.
Purpose
This study aimed to determine the acceptability and perceived benefit of prehabilitation in lung cancer among thoracic surgeons throughout Australia and New Zealand. It was postulated that responses from the survey could be used to gain further insight into the referral pathways and reasons why surgeons choose or do not choose to utilize prehabilitation for patients with lung cancer prior to surgery. The survey also aimed to gather data on the perceived interest in prehabilitation among these gatekeepers to establish if, along with the evidence currently being generated, implementation of prehabilitation into standard care was a common goal within the thoracic surgical oncology field.
Procedure
Ethical approval was obtained from the University of Melbourne (Ethics ID: 1646932).
The survey was conducted as an online survey, with paper versions of the survey also being available (see Supplemental file available online). A 24-item survey was specifically designed for this investigation and was piloted on 2 thoracic surgeons prior to distribution among the larger target population. An email invitation with the link to the survey was sent to 198 fellows of the Royal Australasian College of Cardiothoracic Surgeons; as thoracic surgery is not a stand-alone specialty in Australia, it was not possible to target pure thoracic surgeons. After the initial invitation, 2 further email invitations were distributed via college newsletters and digital press. The survey invitation was sent with a cover letter briefly outlining the purpose of the survey along with instructions and intended use of the survey results. The survey was also distributed in printed format at the Australian and New Zealand Society of Cardiothoracic Surgery Annual Scientific Meeting. Consent was implied by participation in the survey. Following completion of the survey, demographic data and responses to the survey were collated on the online portal Survey Monkey (www.surveymonkey.com; Palo Alto, CA). Data were analyzed descriptively.
Results
Twenty-eight surgeons responded to the survey; the response rate was 14%. The highest response rate was received from surgeons in the state of Victoria 61% (n = 16). Respondents to the survey included cardiothoracic surgeons working in tertiary public and private hospitals throughout Australia and New Zealand. The mean age of the surgeons was 46 years (range = 32-56 years), with a mean level of experience in cardiothoracic surgery of 12.5 years. Most of the surgeons completed an average of 3.4 thoracic cases per week (range = 1-8; Table 1).
Table 1.
Participant Demographics.
| Characteristic | Mean (SD) |
|---|---|
| Age (years) | 46 (12.3) |
| Experience (years) | 12.5 (8.6) |
| Volume of thoracic surgery (cases/week) | 3.4 (1.9) |
| Number of hospitals operating | 2.6 (0.9) |
Abbreviation: SD, standard deviation.
Only 23% of respondents practiced thoracic surgery exclusively (most surgeons performed a mix of cardiac and thoracic cases) (Table 2). The most common waiting period between diagnosis and surgery reported was reported to be 20 days by 38% of the sample, and the most common postoperative length of stay was reported as 6 to 7 days (55% of respondents). All surgeons reported that respiratory physiotherapy was delivered as part of the standard postoperative care, and 63% reported that a thoracic surgery pathway was utilized in their hospital unit. Only 18% of those surveyed reported that they refer lung cancer patients post lung resection for outpatient pulmonary rehabilitation as part of their ongoing care (Table 3).
Table 2.
Work Characteristics of Respondents.
| Thoracic Surgeons, N = 28 | n (%) |
|---|---|
| State of practice | |
| Victoria | 16 (61.5%) |
| New South Wales | 2 (7.7%) |
| South Australia | 0 (0%) |
| Western Australia | 2 (7.7%) |
| Queensland | 2 (7.7%) |
| Northern Territory | 0 (0%) |
| Tasmania | 1 (3.9%) |
| Australian Capital Territory | 0 (0%) |
| New Zealand | 0 (0%) |
| Clinical caseload | |
| Cardiac + thoracic | 20 (76.9%) |
| Thoracic only | 6 (23%) |
| Public versus private | |
| Public | 11 (42.3%) |
| Private | 1 (3.9%) |
| Combination | 14 (53.9%) |
| Dedicated thoracic unit | |
| Yes | 10 (40%) |
| No | 15 (60%) |
| Average waiting period (diagnosis to surgery) | |
| 10 days | 5 (19.2%) |
| 20 days | 10 (38.5%) |
| 30 days | 6 (23%) |
| 40 days | 3 (11.5%) |
| 50 days | 1 (3.9%) |
Table 3.
Pre- and Postoperative Referral for Lung Cancer Patients Undergoing Surgery.
| Pre- and Postoperative Care | n (%) |
|---|---|
| Preoperative referral to physiotherapy | |
| Yes | 8 (32%) |
| Sometimes | 4 (12%) |
| No | 13 (52%) |
| What preoperative resources are available for lung cancer patients? | |
| Pulmonary prehabilitation | 12 (60%) |
| Physiotherapy outpatient appointment | 6 (30%) |
| Private exercise class/clinic | 5 (25%) |
| Home-based intervention | 2 (10%) |
| Other | 6 (30%) |
| Standard postoperative care of thoracic patients | |
| Respiratory physiotherapy as inpatient | 22 (100%) |
| Thoracic surgery pathway as inpatient | 14 (63.6%) |
| Outpatient pulmonary rehabilitation following hospital discharge | 4 (18%) |
| Outpatient clinic follow up | 21 (95.5%) |
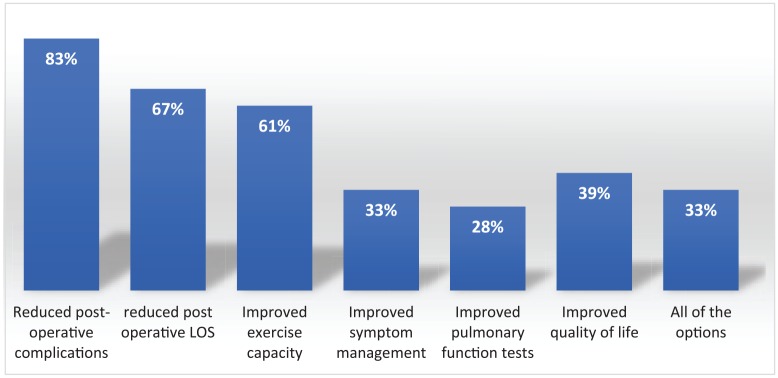
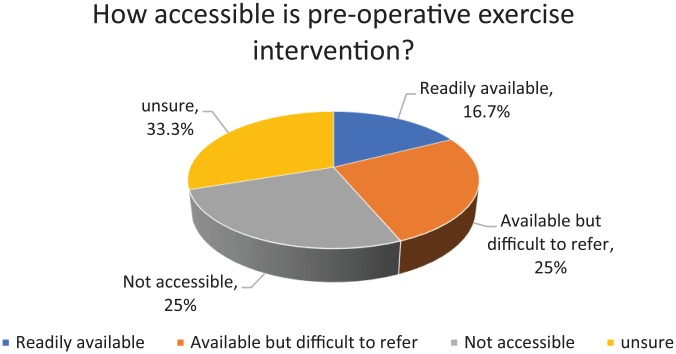
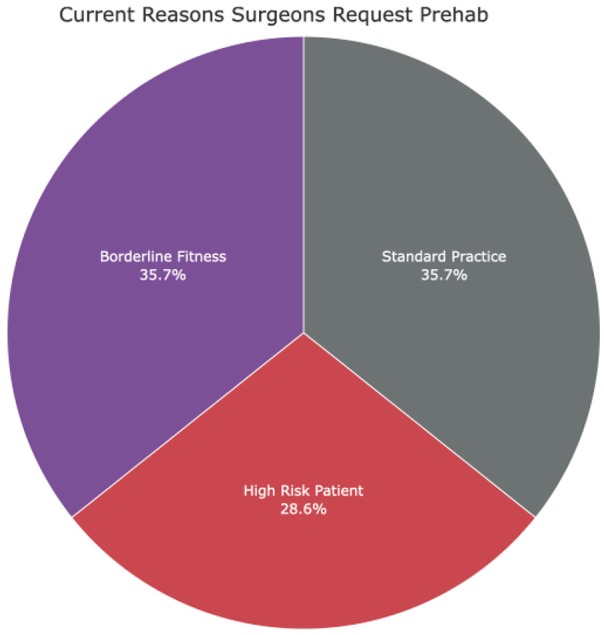
The majority of respondents reported that there is a perceived need to refer lung resection patients to preoperative physiotherapy or prehabilitation, particularly high-risk patients or those with borderline fitness for surgery (Figure 1). In fact, 91% of surgeons were willing to delay surgery (as indicated by cancer stage/type) to optimize patients via prehabilitation. The main perceived benefits of prehabilitation (% of respondents that reported the variable) included the following: reduced postoperative complications (86%), reduced postoperative length of stay (76%), improved exercise capacity (67%), improved quality of life (57%), and improved symptom management (52%; Figure 2). The respondents reported that prehabilitation programs were either not accessible, or available and difficult to refer to (Figure 3). The main barriers to prehabilitation recorded were access to allied health professionals (57%), patient comorbidities (57%), transport or access issues (52%), time (48%), and costs/financial constraints (33%). Despite these difficulties, the perceived benefits of prehabilitation were clear and 92% of respondents believed that further research into prehabilitation in lung cancer is warranted.
Figure 1.
Reasons why surgeons request prehabilitation. Data reported in percentage of responders.
Figure 2.
Surgeon’s perceived benefits of prehabilitation. Data reported in percentage of responders. Responders could choose more than one option. LOS, length of stay.
Figure 3.
Accessibility of preoperative exercise interventions. Data reported in percentage of responders.
Discussion
This was the first study in the Australian setting examining the attitudes and perceptions of thoracic surgeons to prehabilitation in lung cancer. The results of this study are consistent with those of a recent survey performed with colorectal surgeons and anesthetists, which concluded that surgeons recognize the clear association between functional capacity and postoperative outcomes, robust evidence for prehabilitation is currently lacking and that surgeons would be willing to delay surgery (up to 2 weeks) in order to optimize their patients.10
We surveyed 198 cardiothoracic surgeons; however, the response rate was poor with only 28 responses (of a potential 198), yielding a response rate of 14%. A recent online survey of thoracic surgeons in the United States examining the preoperative management of thoracic surgery patients who were smokers reported a similar low response rate of 13% with this population.11 Within the medical profession, in particular surgery, time to participate in additional nonclinical tasks, such as a survey, is limited and may explain some of the inadequate capture of the wider target population despite multiple methods and modes to increase response rate. Another limitation that must be considered is the language and motivations of the survey and how they align with those of the surgeons. Surgeons are often driven by results and invest in strategies that will improve the outcomes for their patients. Unless prehabilitation can demonstrate clear benefits for their patients through robust evidence, it is unlikely to become part of their standard referral practices. Of the surgeons interviewed, a large proportion were from the state of Victoria. This state has a strong bias toward surgeons who practice thoracic surgery as its own specialty, in comparison to cardiothoracic surgeons who perform both cardiac and thoracic surgery and may therefore be more representative of the attitudes and opinions, which are most relevant for prehabilitation prior to lung cancer surgery.
Despite the results of the survey demonstrating that the majority of cardiothoracic surgeons practice minimally invasive techniques (video-assisted thoracoscopic surgery), postoperative morbidity remains a concern for many surgeons. The incidence of postoperative pulmonary complications such as pneumonia, atelectasis, acute respiratory distress syndrome, pulmonary edema, and respiratory failure after lung resection ranges from 4.8% to 55%.12 The response to the survey question, “Out of the patients that you refer preoperatively, can you describe why these patients are referred to Physiotherapy?” further highlights this concern; as 2 of the 3 reasons for referral were related to factors that are associated with higher postoperative morbidity (high-risk patients or patients with borderline fitness for surgery; Figure 1). The main reason cited for not referring to preoperative physiotherapy (exercise intervention) was urgent need for surgery or short waiting period. The literature to date supports the use of prehabilitation in lung cancer in reducing this postoperative morbidity with a recent systematic review concluding that preoperative exercise intervention halves the rate of postoperative complications (risk ratio = 0.52, 95% confidence interval = 0.36 to 0.74) and reduces hospital length of stay (MD = −2.86 days, 95% confidence interval = −5.4 to −0.33) in patients undergoing lung resection.7 Clearly the evidence is emerging; however, promotion of the role that physiotherapists can play in modifying patient risk factors and providing interventions that may help reduce postoperative morbidity needs further attention.
Achieving greater awareness of the role physiotherapists and prehabilitation can play in reducing postoperative morbidity would be assisted by further studies looking specifically at the cost-benefit of providing prehabilitation to patients with lung cancer. Many of the studies to date have examined the effect of prehabilitation on postoperative outcomes; however, these endpoints may not be “speaking the same language” as the surgeons. In terms of surgical practice, the top priorities for surgeons include morbidity, mortality, and practicing in a way that adds value to their service. If we can provide evidence that prehabilitation demonstrates clear cost saving advantages for both the patient and health care system, as well as more data on postoperative morbidity rather than simply the incidence of complications, perhaps there would be more acceptance and integration of prehabilitation into current thoracic surgery care pathways. This has been well researched in a larger study of general surgery patients having preoperative physiotherapy education to reduce postoperative complications.13 The fact that the surgeons surveyed in our study were able to identify the key benefits of preoperative exercise and that nearly all believe further research into prehabilitation is warranted provides evidence to undertake more research in this patient population.
The strongest message this survey uncovered was the overwhelming support for prehabilitation among surgeons in order to optimize their “high-risk” patients (those with multiple comorbidities, advanced age, positive smoking status/respiratory disease, and/or obesity) preoperatively. Over 90% of cardiothoracic surgeons surveyed would be willing to delay surgery for prehabilitation (depending on the stage/operability of the tumor) indicating that there is potential for prehabilitation to fill a current gap in the lung cancer care pathway, particularly in patients with borderline fitness for surgery (as defined by measures of cardiopulmonary function VO2max and pulmonary function tests). This is corroborated by Li et al’s survey of colorectal surgeons who also reported that surgeons would be willing to delay surgery for 2 to 4 weeks for prehabilitation.10 These results clearly demonstrate the recognition that surgeons have of the association between functional capacity and postoperative outcomes, and point toward the acute need for allied health professionals to work to integrate prehabilitation services into current routine practice. Further randomized controlled trial research is required to determine the efficacy of delaying surgery for high-risk patients, as at present data do not support delaying surgery for patients already deemed fit for surgery,2 but rather prehabilitation is timed opportunistically in the waiting period of these patients prior to their surgery.
Finally, it is important to explore alternate means of delivering prehabilitation for patients with lung cancer, such as via telehealth with virtual/online exercise platforms, which could allow delivery of programs to patients in their home setting. A home-based model would be appealing, particularly for patients who are unable to access the traditional center-based programs who often report barriers such as living too far away from the center or lack of transport.9 The trials testing preoperative exercise programs in lung cancer to date predominately use supervised, center-based exercise programs and these may offer advantages to patients in terms of their ability to enhance patient motivation and adherence.2 However, there are emerging data to suggest that home-based exercise is also effective in this population, with a recent trial demonstrating a 2-week home-based multimodal prehabilitation program, supported with telephone calls, improved functional exercise capacity in patients before lung resection.14 Further research is needed to compare the effectiveness of home-based programs compared with center-based programs in lung cancer,2 as well as the optimal home-based exercise models and how these could be supported with technology,15 which has been relatively underresearched in this field to date.
The Future
This survey of cardiothoracic surgeons within Australia and New Zealand is the first to explore the perceptions and attitudes of these gatekeepers to prehabilitation within lung cancer. Results demonstrate a keen interest in prehabilitation within the thoracic oncology population, with 91% of survey respondents willing to delay surgery for prehabilitation. The poor response rate of 14% is a limitation to this study; however, as the majority of responses were from surgeons practicing thoracic surgery exclusively, the attitudes and perceptions reported closely represent current thoracic surgery practice. The attitudes and perceptions of the 86% of “non-responders” remains unknown and may demonstrate a lack of receptiveness to prehabilitation in lung cancer. Further evidence is required to provide a convincing argument for prehabilitation and to target the “non-responders” who may not, due to low thoracic caseload mix or lack of exposure, had the benefit of experience with such preoperative programs and therefore be willing to incorporate prehabilitation into routine care within lung cancer surgery. The challenges for prehabilitation that must be overcome include enhancing its promotion (through education and research), establishing strong referral pathways, developing good relationships with the surgeon gatekeepers, and being able to provide best evidence prehabilitation services in order to provide optimal care to patients most debilitated by lung cancer.
Supplemental Material
Supplemental material, Supplementary_file_1 for Attitudes and Perceptions to Prehabilitation in Lung Cancer by Anna Shukla, Catherine L. Granger, Gavin M. Wright, Lara Edbrooke and Linda Denehy in Integrative Cancer Therapies
Acknowledgments
The authors wish to thank the administrative staff at The Thoracic Society and the Chief Operating Officer at The Australian & New Zealand Society of Cardiac and Thoracic Surgeons (ANZSCTS) for distribution of the online survey via e-newsletters and email correspondence. We would also like to thank the Chair of the Science and Education committee for ANZSCTS for assistance with promotion and distribution of the survey at the 2018 ANZSCTS Annual Scientific Meeting.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Funding was contributed by The Lung Foundation Grant-in-Aid of Lung Cancer Research.
ORCID iD: Catherine L. Granger  https://orcid.org/0000-0001-6169-370X
https://orcid.org/0000-0001-6169-370X
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Silver JK, Baima J. Cancer prehabilitation: an opportunity to decrease treatment related morbidity, increase cancer treatment options and improve physical and psychological health outcomes. Am J Phys Med Rehabil. 2014;92:715-727. [DOI] [PubMed] [Google Scholar]
- 2. Cavalheri V, Granger CL. Preoperative exercise training for patients with non-small cell lung cancer. Cochrane Database Syst Rev. 2017;(6):CD012020. doi: 10.1002/14651858.CD012020.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Granger CL, McDonald CF, Irving L, et al. Low physical activity levels and functional decline in individuals with lung cancer. Lung Cancer. 2014;83:292-299. [DOI] [PubMed] [Google Scholar]
- 4. Santa Mina D, Clarke H, Ritvo P, et al. Effect of total body prehabilitation on postoperative outcomes: a systematic review and meta-analysis. Physiotherapy. 2014;100:196-207. [DOI] [PubMed] [Google Scholar]
- 5. Myers JN, Fonda H. The impact of fitness on surgical outcomes: the case for prehabilitation. Curr Sports Med Rep. 2016;15:282-289. [DOI] [PubMed] [Google Scholar]
- 6. Garcia RS, Brage MIY, Moolhuyzen EG, Granger CL, Denehy L. Functional and postoperative outcomes after preoperative exercise training in patients with lung cancer: a systematic review and meta-analysis. Interact Cardiovasc Thorac Surg. 2016;23:486-497. [DOI] [PubMed] [Google Scholar]
- 7. Steffens D, Beckenkamp PR, Hancock M, Solomon M, Young J. Preoperative exercise halves the postoperative complication rate in patients with lung cancer: a systematic review of the effect of exercise on complications, length of stay and quality of life in patients with cancer. Br J Sports Med. 2018;52:344. [DOI] [PubMed] [Google Scholar]
- 8. Granger CL, Denehy L, Remedios L, et al. Barriers to translation of physical activity into the lung cancer model of care: a qualitative study of clinicians’ perspectives. Ann Am Thorac Soc. 2016;13:2215-2222. [DOI] [PubMed] [Google Scholar]
- 9. Granger CL, Connolly B, Denehy L, et al. Understanding factors influencing physical activity and exercise in lung cancer: a systematic review. Support Care Cancer. 2017;25:983-999. [DOI] [PubMed] [Google Scholar]
- 10. Li MHG, Bolshinsky V, Ismail H, et al. Cross-sectional survey of Australian anesthetists and surgeons’ perceptions of preoperative risk stratification and prehabilitation. Can J Anesth. 2019;66:388-405. [DOI] [PubMed] [Google Scholar]
- 11. Marino KA, Little MA, Bursac Z, Sullivan JL, Klesges R, Weksler B. Operating on patients who smoke: a survey of thoracic surgeons in the United States. Ann Thorac Surg. 2016;102:911-916. [DOI] [PubMed] [Google Scholar]
- 12. Jing R, He S, Dai H, et al. Incidence and risk factors of postoperative pulmonary complications after thoracic surgery for early non-small cell cancer. Int J Clin Exp Med. 2018;11:285-294. [Google Scholar]
- 13. Boden I, Skinner EH, Browning L, et al. Preoperative physiotherapy for the prevention of respiratory complications after upper abdominal surgery: pragmatic, double-blinded, multicenter randomized controlled trial. BMJ. 2018;360:j5916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Liu ZT, Qiu L, Pei Y, et al. Two-week multimodal prehabilitation program improves perioperative functional capability in patients undergoing thoracoscopic lobectomy for lung cancer: a randomized controlled trial [published online July 23, 2019]. Anesth Analg. doi: 10.1213/ANE.0000000000004342 [DOI] [PubMed] [Google Scholar]
- 15. Cox A, Lucas G, Marcu A, et al. Cancer survivors’ experience with telehealth: a systematic review and thematic analysis. J Med Internet Res. 2017;19;e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplementary_file_1 for Attitudes and Perceptions to Prehabilitation in Lung Cancer by Anna Shukla, Catherine L. Granger, Gavin M. Wright, Lara Edbrooke and Linda Denehy in Integrative Cancer Therapies