Aspirin has been widely used in primary prevention of atherosclerotic cardiovascular disease (ASCVD).[1–4] Aspirin for primary prevention of ASCVD does not significantly reduce all-cause mortality or cardiovascular mortality, and the main benefit of aspirin for primary prevention of ASCVD is a significant reduction in non-fatal ischemic events including myocardial infarction, transient ischemic attack, ischemic stroke, and major cardiovascular events (cardiovascular death, non-fatal myocardial infarction, and non-fatal stroke), whereas the main risk is a significant increase in non-fatal major bleeding events including gastrointestinal bleeding and intracranial hemorrhage.[5–8] Obviously, it makes sense to prescribe aspirin for primary prevention only if the benefits clearly outweigh the risks. In Europe and the United States, the benefit-risk ratio of aspirin for primary prevention has gradually decreased compared to the past due to the wide application of other primary prevention measures such as blood pressure reduction, smoking cessation, and the use of statins. Three recent large-scale clinical trials have shown that aspirin has no net clinical benefit when used in low-risk populations.[9–13] Therefore, aspirin must be used with caution in the primary prevention of ASCVD.
On the contrary, it is not clear yet that aspirin has primary prevention value. First, an up-to-date summary of all primary prevention clinical trial data shows that aspirin can still significantly reduce major cardiovascular events.[6,7] Second, patients who are unable to take other primary prevention measures (such as statins) may need aspirin more often.[14,15] Third, through careful evaluation, it is possible to identify individuals with a relatively reasonable benefit-risk ratio. Primary prevention of aspirin is mainly applicable to adults aged 40 to 69 years who still have high risk of ischemia (≥10% expected risk for 10 years) after taking active intervention, with low risk of bleeding and are willing to take low-dose aspirin for long-term prophylaxis use.[3,15,16]
Based on the latest evidence-based medicine and China's national conditions, we propose the following recommendations of aspirin for primary prevention of ASCVD in Chinese population as follows:
1. For all patients who intend to use aspirin, four measures must be taken before medication (I, C):
-
(a)
Carefully weigh the benefit-bleeding risk ratio, screen and exclude high-risk populations of bleeding, and periodically or dynamically assess the benefit-bleeding risk ratio during usage, solve the problems timely when any found.
-
(b)
According to the relevant medical specialist regulations,[17] take preventive measures to reduce the risk of gastrointestinal bleeding, treat gastrointestinal active pathological changes in advance (including Helicobacter pylori), if necessary, prophylactically apply proton pump inhibitor or H2 receptor antagonists.
-
(c)
Adhere to a healthy lifestyle (smoking cessation, careful drinking, scientific diet and proper exercise) and positively control blood pressure, blood sugar, and blood lipid levels. Aspirin should be considered when hypertensive patients keep their blood pressure at <140/90 mmHg.
-
(d)
Doctors should communicate with patients and obtain their consent prior to prescribing aspirin.
2. The following ASCVD high-risk groups may consider taking low-dose aspirin (75–100 mg/day) for primary prevention (IIb, A):
-
(a)
Adults aged 40 to 69 years, if the 10-year expected risk of ASCVD is ≥10% for their initial risk assessment, and there are still ≥3 major risk factors that remain poorly controlled or difficult to change after active treatment intervention (eg, family history of early onset of cardiovascular disease), aspirin can be considered to reduce the risk of ischemic cardiovascular disease.
-
(b)
ASCVD risk assessment can refer to relevant domestic guidelines.[4,18,19] The main risk factors include: (1) hypertension, (2) diabetes, (3) dyslipidemia (total cholesterol ≥6.2 mmol/L or low-density lipoprotein ≥4.1 mmol/L or high-density lipoprotein <1.0 mmol/L), (4) smoking, (5) family history of early onset of cardiovascular disease (first-degree relatives’ age <50 years), (6) obesity (body mass index ≥28 kg/m2), (7) coronary artery calcification score ≥100[20–23] or non-obstructive coronary artery stenosis (<50%).[24–27] Coronary imaging examination of primary prevention subjects is not recommended routinely.
3. The following populations are not recommended to take aspirin for primary prevention of ASCVD[3,15,19]:
-
(a)
Population aged ≥70 years or <40 years old (III, B): The current evidence is insufficient to make a primary prevention recommendation, and individualized evaluation is needed.
-
(b)
Population at high risk of bleeding (III, C): In use of other drugs that increase the risk of bleeding (including anti-platelet drugs, anti-coagulants drugs, hormones, and non-steroidal anti-inflammatory drugs), gastrointestinal bleeding, peptic ulcer, or history of bleeding in other sites, age ≥70 years, thrombocytopenia, coagulopathy, severe liver disease, chronic kidney disease stage 4 to 5, uneradicated H. pylori infection, uncontrollable hypertension.
-
(c)
Patients whose risk of bleeding was assessed to be greater than the risk of thrombosis (III, C).
4. A brief flow chart of population screening for aspirin in primary prevention [Figure 1].
Figure 1.
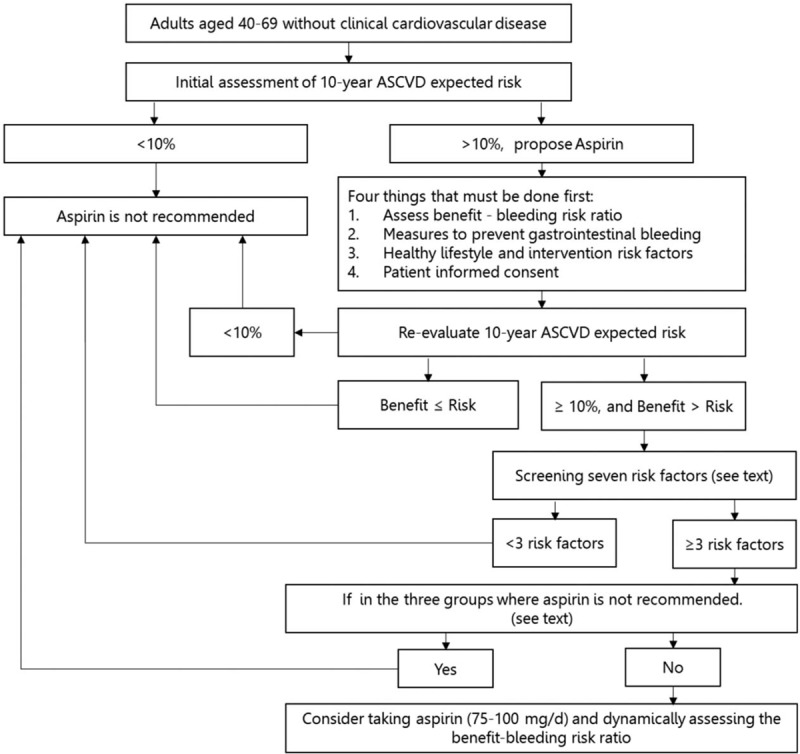
A brief flow chart of population screening for aspirin in primary prevention. ASCVD: Atherosclerotic cardiovascular disease.
List of expert groups (sorted by last name): Xiao-Juan Bai, Lu-Yuan Chen , Jin Fan, Run-Lin Gao, Dong-Feng Gu, Yi-Fang Guo, Ming-Li He, Ying-Long Hou, Qi Hua, Yong Huo, Ai-Ping Jin, Wei Li, Xiao-Ying Li, Yan Li, Li Yong, Liu Chaozhong, Dai-Hong Liu, Jing Liu, Hong-Bin Liu, Mei-Lin Liu, Qiang Liu, Ming Lu, Bin Luo, Shu-Zhen Lu, Ming-Kang Pan, Dan-Tao Peng, Ming-Zhao Qin, Wei-Hong Sha, Pei-Yan Shan, Zhong-Wei Shi, Xu-Bo Shi, Zhi-Qiang Song, Yi-Hong Sun, Xi-cheng Wang, Xiao-Ming Wang, Di Wu, Yang-Feng Wu, Qian Xiao, Hao Xu, Feng Xu, Xiao-Wei Yan, Yun-Mei Yang, Da-Wei Yin, Hai-Tao Yuan, Cun-Tai Zhang, Dong Zhao, Ying-Xin Zhao, and Song-Bai Zheng.
Conflicts of interest
None.
Footnotes
How to cite this article: Li XY, Shi ZW, Zhao D, Yin DW. 2019 Chinese expert consensus statement on aspirin application in primary prevention of cardiovascular disease. Chin Med J 2020;133:1221–1223. doi: 10.1097/CM9.0000000000000762
References
- 1.Pearson TA, Blair SN, Daniels SR, Eckel RH, Fair JM, Fortmann SP, et al. AHA Guidelines for Primary Prevention of Cardiovascular Disease and Stroke: 2002 update: consensus panel guide to comprehensive risk reduction for adult patients without coronary or other atherosclerotic vascular diseases. American Heart Association Science Advisory and Coordinating Committee. Circulation 2002; 106:388–391. doi: 10.1161/01.cir.0000020190.45892.75. [DOI] [PubMed] [Google Scholar]
- 2.Maciosek MV, Coffield AB, Edwards NM, Flottemesch TJ, Goodman MJ, Solberg LI. Priorities among effective clinical preventive services: results of a systematic review and analysis. Am J Prev Med 2006; 31:52–61. doi: 10.1016/j.amepre.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 3.Bibbins-Domingo K. Aspirin use for the primary prevention of cardiovascular disease and colorectal cancer: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med 2016; 164:836–845. doi: 10.7326/M16-0577. [DOI] [PubMed] [Google Scholar]
- 4.Task Force on Chinese Guidelines for the Prevention of Cardiovascular Diseases(2017); Editorial Board of Chinese Journal of Cardiology Chinese guidelines for the prevention of cardiovascular diseases (2017) [in Chinese]. Zhonghua Xin Xue Guan Bing Za Zhi 2018; 46:10–25. doi: 10.3760/cma.j.issn.0253-3758.2018.01.004. [DOI] [PubMed] [Google Scholar]
- 5.Baigent C, Blackwell L, Collins R, Emberson J, Godwin J, Peto R, et al. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet 2009; 373:1849–1860. doi: 10.1016/S0140-6736(09)60503-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zheng SL, Roddick AJ. Association of aspirin use for primary prevention with cardiovascular events and bleeding events: a systematic review and meta-analysis. JAMA 2019; 321:277–287. doi: 10.1001/jama.2018.20578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abdelaziz HK, Saad M, NVK P, Megaly M, Potluri R, Saleh M, et al. Aspirin for primary prevention of cardiovascular events. J Am Coll Cardiol 2019; 73:2915–2929. doi: 10.1016/j.jacc.2019.03.501. [DOI] [PubMed] [Google Scholar]
- 8.Mora S, Manson JE. Aspirin for primary prevention of atherosclerotic cardiovascular disease: advances in diagnosis and treatment. JAMA Intern Med 2016; 176:1195–1204. doi: 10.1001/jamainternmed.2016.2648. [DOI] [PubMed] [Google Scholar]
- 9.Gaziano JM, Brotons C, Coppolecchia R, Cricelli C, Darius H, Gorelick PB, et al. Use of aspirin to reduce risk of initial vascular events in patients at moderate risk of cardiovascular disease (ARRIVE): a randomised, double-blind, placebo-controlled trial. Lancet 2018; 392:1036–1046. doi: 10.1016/S0140-6736(18)31924-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bowman L, Mafham M, Wallendszus K, Stevens W, Buck G, Barton J, et al. Effects of aspirin for primary prevention in persons with diabetes mellitus. N Engl J Med 2018; 379:1529–1539. doi: 10.1056/NEJMoa1804988. [DOI] [PubMed] [Google Scholar]
- 11.McNeil JJ, Woods RL, Nelson MR, Reid CM, Kirpach B, Wolfe R, et al. Effect of aspirin on disability-free survival in the healthy elderly. N Engl J Med 2018; 379:1499–1508. doi: 10.1056/NEJMoa1800722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McNeil JJ, Wolfe R, Woods RL, Tonkin AM, Donnan GA, Nelson MR, et al. Effect of aspirin on cardiovascular events and bleeding in the healthy elderly. N Engl J Med 2018; 379:1509–1518. doi: 10.1056/NEJMoa1805819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McNeil JJ, Nelson MR, Woods RL, Lockery JE, Wolfe R, Reid CM, et al. Effect of aspirin on all-cause mortality in the healthy elderly. N Engl J Med 2018; 379:1519–1528. doi: 10.1056/NEJMoa1803955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gaziano JM. Aspirin for primary prevention: clinical considerations in 2019. JAMA 2019; 321:253–255. doi: 10.1001/jama.2018.20577. [DOI] [PubMed] [Google Scholar]
- 15.Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2019; 74:e177–177e232. doi: 10.1016/j.jacc.2019.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pignone M. What is so hard about aspirin for primary prevention? J Am Coll Cardiol 2019; 73:2930–2931. doi: 10.1016/j.jacc.2019.03.502. [DOI] [PubMed] [Google Scholar]
- 17.Chinese Expert Consensus Group on Prevention and Treatment of Gastrointestinal Injury with Antiplatelet Drugs Chinese Expert Consensus on Prevention and Treatment of Gastrointestinal Injury with Antiplatelet Drugs (2012 updated version). Chin J Intern Med 2013; 52:264–270. doi: 10.3760/cma.j.issn.0578-1426.2013.03.027. [Google Scholar]
- 18.Geriatrics Branch of Chinese Medical Association; Editorial Board of Chinese Journal of Internal Medicine; and Editorial Board of Chinese Journal of Geriatrics Aspirin use in patients with atherosclerotic cardiovascular disease: the 2016 Chinese expert consensus statement [in Chinese]. Zhonghua Nei Ke Za Zhi 2017; 56:68–80. doi: 10.3760/cma.j.issn.0578-1426.2017.01.020. [DOI] [PubMed] [Google Scholar]
- 19.Joint Task Force for Guideline on the Assessment and Management of Cardiovascular Risk in China Guideline on the assessment and management of cardiovascular risk in China [in Chinese]. Zhonghua Yu Fang Yi Xue Za Zhi 2019; 53:13–35. doi: 10.3760/cma.j.issn.0253-9624.2019.01.004. [DOI] [PubMed] [Google Scholar]
- 20.Miedema MD, Duprez DA, Misialek JR, Blaha MJ, Nasir K, Silverman MG, et al. Use of coronary artery calcium testing to guide aspirin utilization for primary prevention: estimates from the multi-ethnic study of atherosclerosis. Circ Cardiovasc Qual Outcomes 2014; 7:453–460. doi: 10.1161/CIRCOUTCOMES.113.000690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mitchell JD, Fergestrom N, Gage BF, Paisley R, Moon P, Novak E, et al. Impact of statins on cardiovascular outcomes following coronary artery calcium scoring. J Am Coll Cardiol 2018; 72:3233–3242. doi: 10.1016/j.jacc.2018.09.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Budoff MJ, Young R, Burke G, Jeffrey CJ, Detrano RC, Folsom AR, et al. Ten-year association of coronary artery calcium with atherosclerotic cardiovascular disease (ASCVD) events: the multi-ethnic study of atherosclerosis (MESA). Eur Heart J 2018; 39:2401–2408. doi: 10.1093/eurheartj/ehy217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2019; 73:e285–e1285. doi: 10.1016/j.jacc.2018.11.003. [DOI] [PubMed] [Google Scholar]
- 24.Hwang IC, Jeon JY, Kim Y, Kim HM, Yoon YE, Lee SP, et al. Association between aspirin therapy and clinical outcomes in patients with non-obstructive coronary artery disease: a cohort study. PLoS One 2015; 10:e0129584.doi: 10.1371/journal.pone.0129584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chow BJ, Small G, Yam Y, Chen L, McPherson R, Achenbach S, et al. Prognostic and therapeutic implications of statin and aspirin therapy in individuals with nonobstructive coronary artery disease: results from the CONFIRM (COronary CT Angiography EvaluatioN For Clinical Outcomes: An InteRnational Multicenter registry) registry. Arterioscler Thromb Vasc Biol 2015; 35:981–989. doi: 10.1161/ATVBAHA.114.304351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Huang FY, Huang BT, Lv WY, Liu W, Peng Y, Xia TL, et al. The prognosis of patients with nonobstructive coronary artery disease versus normal arteries determined by invasive coronary angiography or computed tomography coronary angiography: a systematic review. Medicine (Baltimore) 2016; 95:e3117.doi: 10.1097/MD.0000000000003117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Herscovici R, Sedlak T, Wei J, Pepine CJ, Handberg E, Bairey MCN. Ischemia and no obstructive coronary artery disease (INOCA): what is the risk? J Am Heart Assoc 2018; 7:e008868.doi: 10.1161/JAHA.118.008868. [DOI] [PMC free article] [PubMed] [Google Scholar]


