Abstract
Introduction
We investigated associations between exposure to tobacco outlets within activity spaces and daily tobacco use, and whether exposure to adults or peers using tobacco mediate these relationships.
Methods
We used Geographic Ecological Momentary Assessment data over 14 days from 85 youth aged 16–20 years in eight mid-sized California city areas. Tobacco outlet addresses and global positioning systems locations were geocoded and activity spaces were constructed by joining sequential points. We assessed daily number of tobacco outlets within 50 or 100 m of activity space polylines and number of minutes participants were within 50 or 100 m of tobacco outlets each day; daily use of tobacco; and whether participants saw (1) adults and (2) people their age (peers) using tobacco each day.
Results
Controlling for demographics, results of multilevel structural equation models showed no association between number of tobacco outlets within 50 m of polylines and tobacco use (probit regression coefficient: 0.01, p = .82). However, we found evidence of an indirect effect (p = .001) through daily exposure to peers using tobacco. Specifically, greater number of tobacco outlets within 50 m of polylines was positively associated with seeing peers use tobacco (probit regression coefficient: 0.10, p < .001). In turn, seeing peers use tobacco was positively associated with tobacco use on that day (probit regression coefficient: 2.23, p < .001). Similar results were found for number of tobacco outlets within 100 m of polylines.
Conclusions
Exposure to tobacco outlets within activity spaces affects youth tobacco use through daily exposure to peers who use tobacco.
Implications
Using real-time-ordered data, this article examines whether exposure to adults and peers using tobacco mediate associations between exposure to tobacco outlets within activity spaces and daily tobacco use among youth. Results suggest that exposure to tobacco outlets within activity spaces affects daily tobacco use through exposure to peers who use tobacco. These findings provide additional significant support for policy makers who are considering regulating the number and density of tobacco retailers and point to the importance of interventions focused on peer tobacco use and youths’ daily environments to reduce tobacco use.
Introduction
Tobacco use is the leading cause of preventable death in the United States.1 Because most tobacco use starts during adolescence,1,2 prevention efforts need to focus on youth. One important determinant of youth tobacco use is exposure to tobacco retail outlets. A growing number of studies have found associations between density of tobacco outlets near homes and schools and cigarette smoking.3–9
Recent research has also begun to explore how to best measure exposure to tobacco outlets and its associations with youth tobacco use. For instance, results of an exploratory study in California suggest that focusing only on exposure to tobacco retail outlets around homes and schools may underestimate the extent to which youth are exposed to tobacco outlets in their daily lives and that exposure to tobacco outlets was more accurately measured by considering activity spaces.10 Activity spaces refer to locations that people commonly frequent as part of their daily routines. Activity spaces can be defined a priori as places in the community (eg, parks, malls, urban centers, and schools) or based on routes an individual frequents based on his or her travel patterns. Research shows that individuals engage in many daily activities outside of their home or residential environment.11,12 Few other studies have examined exposure to tobacco outlets considering activity spaces;13–15 however, research on its use and applications are growing.16
Also, questions remain about how exposure to tobacco outlets affects youth tobacco use. Exposure to tobacco outlets may increase tobacco use through perceptions of others’ tobacco use. That is, daily exposure to tobacco outlets may increase exposure to adults or peers who use tobacco, who are likely to be seen around tobacco outlets, which in turn may influence tobacco use. Though the social cognitive theory17,18 and previous research2,19,20 also suggest that perceptions of others’ tobacco use are strong determinants of youth tobacco use, no research, to the best of our knowledge, has examined whether perceptions of tobacco use mediate associations between exposure to tobacco outlets and tobacco use.
To address these research gaps, this study examined whether daily exposure to tobacco outlets within activity spaces is associated with daily tobacco use among youth and whether perceptions of daily tobacco use by adults or peers mediate this relationship. We hypothesized that youth who were exposed to more tobacco outlets and spent more time around tobacco outlets in their daily activity spaces would report seeing more peers and adults use tobacco and in turn, seeing more peers and adults use tobacco would be associated with daily tobacco use.
Methods
Study Cities and Participants
We collected Geographic Ecological Momentary Assessment (GEMA) data from youth aged 16–20 years (n = 101 participants) in eight mid-sized California city areas. GEMA data combine ecological momentary assessment data with global positioning systems (GPS) and geographic information systems and allow researchers to collect real-time data on participants’ behaviors and environments.21 Cities were selected from an existing geographically diverse sample of 50 noncontiguous California cities (population range: 50 000–500 000).22,23 To select the eight cities, we considered cities within a 50-mile radius of the city of Oakland, where our research center was located at the time of the study. Of the 50 cities, 11 cities met this criterion. To maximize variation in youth exposure to tobacco outlets in their living environments, we first stratified these cities based on measures of socioeconomic status (ie, a measure derived from: median household income, percentage of population with a college education, and percentage of population unemployed) and tobacco outlet density (ie, number of licensed tobacco outlets per 10 000 persons) and then randomly selected eight cities representing low versus high socioeconomic status and low versus high tobacco outlet density. We recruited participants who lived in these eight cities or in cities that were within a 10-mile buffer of the eight cities.
At the time of data collection (February 2017–May 2018), California had raised the minimum tobacco sales age to 21, which applied to all cities in the study. Also, in all eight cities, there were no local policies restricting point of sale tobacco promotions at the time of the study. Self-service displays of tobacco products were prohibited by state law though there are some exceptions (eg, pipe tobacco and snuff).24 Of the study cities, four implemented one or more local tobacco sales policies, including stronger tobacco retailer licensing, tobacco retailer location restrictions, licensing ordinances that include emerging products (eg, electronic cigarettes [e-cigarettes]), prohibitions on sales of flavored tobacco products, or prohibitions on sales of single cigars.25
We used a multitiered approach to recruit youth participants (50% past month tobacco users). We recruited participants through internet and social media advertisements, including Craigslist, Facebook, Twitter, and Myspace. Also, participants were recruited through flyers distributed to youth organizations in the study cities and by referral. Potential participants were screened for eligibility (ie, age, city of residence, speak English, and tobacco use). Researchers obtained parental consent for participation for those younger than 18 years. All participants provided signed consent or assent to participate in the research. The Pacific Institute for Research and Evaluation Institutional Review Board (Federal-wide Assurance #FWA00003078) approved the study before implementation.
Procedures
At the beginning of the study, participants completed an online initial survey (30 minutes), which included questions about demographic characteristics, personal risk factors, and tobacco use and beliefs. Using GPS-enabled smartphones with a survey application, participants then responded to brief daily surveys and location coordinates (latitude and longitude) were obtained at 1-minute intervals for 14 days. Research team members provided GPS-enabled phones to participants and briefed them about study procedures. Participants completed the daily surveys using a phone survey application programed to send reminders to complete the survey each evening at 8 pm. Youth had a 3-hour window to respond to the survey each day.
As compensation for their participation, participants received $10 for completing the initial survey, $5 for each daily survey, and a $20 bonus if they completed all surveys. In addition, they received $40 for return of the phone at the end of the study and $10 for return of the charger. Participants could use the phones with unlimited voice and text during the study. All participants received a resource card on completion of the study.
Analytical Sample
We excluded geocoded data for days in which participants were tracked for less than 360 minutes (n = 76). Overall, of the 1483 days, 363 days were missing on observed exogenous variables (ie, control variables and daily neighborhood exposures) and 170 days missing on the endogenous variable (ie, daily tobacco use) and excluded. The final analytic sample therefore included 950 days, which were clustered within 85 participants. After excluding days with missing data, each participant in the study had, on average, 11.12 days of data (SD: 2.52).
Measures
Daily Tobacco Use
Our main outcome of interest was tobacco use, which was measured daily. Participants were asked, “Since this time yesterday, did you…”
1. smoke at least one cigarette?
2. smoke any cigar, cigarillo, or little cigar?
3. use chewing tobacco snuff or dip, such as Redman, Levi Garrett, Beechnut, Skoal, Skoal Bandits, or Copenhagen?
4. use an e-cigarette or vape device, including e-pen, vape pen, cigalikes, e-hookah, personal vaporizers, or mods to get nicotine?
5. smoke part or all of a cigar, cigarillo, or little cigar with marijuana in it (a blunt)?
We included blunt use in our measure because (1) blunts contain nicotine even if all of the tobacco filler is removed from the cigar26 and (2) cigars, cigarillos, or little cigars used to make blunts are sold in tobacco outlets. For each question, participants could respond yes (coded as 1) or no (coded as 0). If a participant reported the use of any of those products on a specific day, they were coded as having used tobacco on that day.
Daily Exposure to Peers and Adults Who Use Tobacco
To determine whether participants were exposed to peers who used tobacco each day, we asked, “Since this time yesterday, did you see people your age who were smoking cigarettes, vaping e-cigarettes, or using any other tobacco or nicotine product?” To determine whether participants were exposed to adults who used tobacco, we asked “Since this time yesterday, did you see adults (other than your parents/guardians) smoking cigarettes, vaping e-cigarettes, or using any other tobacco or nicotine products?” For both questions, participants could respond yes (coded as 1) or no (coded as 0).
Exposure to Tobacco Outlets
Using the Dun & Bradstreet, INC commercial list, the North American Industry Classification System (NAICS) codes were used to identify probable tobacco outlets in the eight cities and within 10-mile buffer of city boundaries. Specifically, probable tobacco outlets were searched using the NAICS codes of the top 10 retail industries that sell tobacco products including supermarkets and other grocery (except convenience) stores (445110), convenience stores (445120), tobacco stores (453991), gasoline station with convenience stores (447110), warehouse clubs and supercenters (452910), news dealers and newsstands (451212), beer, wine, and liquor stores (445310), pharmacies and drug stores (446110), discount department stores (452112), and other gasoline stations (447190). These codes are industries that represent approximately 98% of all tobacco sales and were used in a study that validated the use of commercial lists to identify tobacco outlets in states that do not have a comprehensive list of tobacco outlet addresses.27 Given that none of the selected cities prohibited sales of tobacco products in pharmacies, the NAICS codes for pharmacies and drug stores were included for all cities. Next, chains with policies restricting the sale of tobacco (e.g., Target and CVS Pharmacy) were excluded from the list. To ensure our study included places that sell alternative nicotine delivery systems but do not sell other tobacco products (eg, hookah bars), we conducted an online search of places that sell hookahs and e-cigarettes in each city. All identified tobacco outlets were contacted by telephone to verify business status, sales of tobacco products, address, and hours of operation. Next, these outlets were visited by observers to record outlet GPS point locations (ie, latitude and longitude) and obtain data about tobacco products and marketing (not reported in this study).
Tobacco outlet addresses and participants’ GPS locations were geocoded and activity spaces were constructed by joining sequential GPS points into a polyline, which was then buffered and overlaid with tobacco outlet locations. An example of a participant’s activity space can be seen in Supplementary Figure A. Exposure measures included the number of tobacco outlets within (1) 50 m or (2) 100 m of these polylines each day, as well as the number of minutes participants were within (3) 50 m or (4) 100 m of tobacco outlet each day. The downloaded GPS data had a field of accuracy of each point. The average accuracy was 20 m. To minimize potential errors, we used 50- and 100-m buffers. All four exposure measures were weighted by the time participants were within the study area. We ran separate models for each of these exposures because number of tobacco outlets within 50 m or 100 m of polylines were highly correlated with one another (r = .96, p < .001), as were time spent within 50 m or 100 m of tobacco outlets (r = .73, p < .001).
Control Variables
Control variables included sex assigned at birth (male, female, or intersex), race (white or non-white), ethnicity (Latino or non-Latino), age group (less than 18 or 18+), and perceived socioeconomic status with the item, “Compared with other people in America, how rich or poor do you consider yourself?” Respondents could answer on a Likert scale (1 = rich to 7 = poor). Researchers have found that perceived socioeconomic status is associated with health behaviors and health outcomes.28 All control variables were assessed at baseline.
Data Analysis
We first examined means, SDs, or frequencies of all variables using SAS, version 9.4 (SAS Inc., Cary, NC). We then used multilevel structural equation modeling (MSEM) with Mplus, version 7 for the mediation analysis. As the data were cross-sectional and not able to provide temporal relationships for cause and effect, we have used the term “potentially mediate” throughout the article. We used MSEM for the following three reasons: (1) We had longitudinal data in which days over time were clustered within individuals and MSEM models may decrease bias of effects compared with traditional multilevel mediation approaches;29 (2) our potential mediators and outcomes were binary, which many traditional multilevel mediation approaches cannot easily accommodate;29 and (3) we were interested in examining two potential mediators simultaneously, which is relatively easy with MSEM.30
Because our outcome and potential mediators were binary, we analyzed data using the probit link, which is used to transform outcome probabilities to the standard normal variable.31 The probit regression coefficients give the change in the z-score or probit index for a one unit change in the predictor.32 Because the MSEM included binary outcomes, no model fit data were reported by Mplus. For all analyses, we set critical α = .05 and used two-tailed statistical tests.
Results
Sample Characteristics
Of the 85 participants, more than half identified as white (n = 48, 56.47%) and one-fifth identified as Hispanic or Latino (n = 19, 22.35%). A slight majority of the sample was female (n = 53, 62.35%) and younger than 18 (n = 52, 61.18%; Table 1).
Table 1.
Participant Characteristics, n = 85 Participants and 950 d
| N | % | Mean | SD | Range | |
|---|---|---|---|---|---|
| Individual-level (n = 85) | |||||
| Race | |||||
| White | 48 | 56.47 | — | — | — |
| Non-white | 37 | 43.53 | — | — | — |
| Ethnicity | — | — | — | ||
| Hispanic or Latino | 19 | 22.35 | — | — | — |
| Not Hispanic or Latino | 66 | 77.65 | — | — | — |
| Sex at birth | — | — | — | ||
| Male | 32 | 34.43 | — | — | — |
| Female | 53 | 65.57 | — | — | — |
| Age | — | — | — | ||
| Younger than 18 | 52 | 61.18 | — | — | — |
| 18 or older | 33 | 38.82 | — | — | — |
| Perceived socioeconomic status | 85 | — | 4.22 | 1.46 | 1–7 (higher values = more poor) |
| Mean number of days participants used tobacco over the study period | 85 | — | 2.99 | 4.26 | 0–13 |
| Mean number of days participants were exposed to peers who use tobacco over the study period | 85 | — | 4.21 | 4.16 | 0–13 |
| Mean number of days participants were exposed to adults who use tobacco over the study period | 85 | — | 5.45 | 4.05 | 0–14 |
| Mean tobacco outlets within 50 m of activity space polylines per day | 85 | — | 2.80 | 1.99 | 0–9 |
| Mean number of tobacco outlet within 100 m of activity space polylines per day | 85 | — | 4.22 | 2.86 | 0–14 |
| Mean amount of time spent within 50 m of tobacco outlets per day (in minutes) | 85 | — | 7.12 | 10.27 | 0–74 |
| Mean amount of time spent within 100 m of tobacco outlets per day (min) | 85 | — | 16.48 | 31.38 | 0–273 |
| Day-level (n = 950) | |||||
| Daily tobacco use | |||||
| Days in which participants did not use tobacco | 716 d | 75.37 | — | — | — |
| Days in which participants did use tobacco | 234 d | 24.63 | — | — | — |
| Daily exposure to peers who use tobacco | |||||
| Days in which participants were not exposed to peers who use tobacco | 614 d | 64.70 | — | — | — |
| Days in which participants were exposed to peers who use tobacco | 335 d | 35.30 | — | — | — |
| Daily exposure to adults who use tobacco | |||||
| Days in which participants were not exposed to adults who use tobacco | 520 d | 54.91 | |||
| Days in which participants were exposed to adults who use tobacco | 427 d | 45.09 | — | — | — |
| Mean number of tobacco outlets within 50 m of activity space polylines per day | 950 d | — | 2.95 | 3.65 | 0–21 (higher values = increasing exposure) |
| Mean number of tobacco outlets within 100 m of activity space polylines per day | 950 d | — | 4.40 | 5.03 | 0–27 (higher values = increasing exposure) |
| Mean amount of time spent within 50 m of tobacco outlets per day (min) | 950 d | — | 7.55 | 19.95 | 0–339 (higher values = increasing exposure) |
| Mean amount of time spent within 100 m of tobacco outlets per day (min) | 950 d | — | 17.41 | 48.61 | 0–573 (higher values = increasing exposure) |
Of the 950 study days, participants reported using a tobacco product on 24.63% of days (n = 234 days), seeing a peer use tobacco on 35.30% of days (n = 335 days), and seeing an adult use tobacco on 45.09% of days (n = 427 days). In addition, on average participants were exposed to 2.95 tobacco outlets within 50 m of polylines (SD: 3.65) and 4.40 tobacco outlets within 100 m of polylines (SD: 5.03) per day. Finally, participants spent, on average, 7.55 minutes within 50 m of tobacco outlets (SD: 19.95) and 17.41 minutes within 100 m of tobacco outlets (SD: 48.61) per day (Table 1).
Descriptive Associations
Of the 234 days in which participants reported using a tobacco product, most days (72.65%) participants also reported seeing a peer use tobacco (Table 2). Participants were therefore more likely to report using tobacco on days in which they saw a peer tobacco user (p < .001) than on days in which they did not see a peer tobacco user. Similar results were found for exposure to adult tobacco users. In addition, we found that number of tobacco outlets within 50 m and 100 m of activity space polylines was significantly associated with exposure to peer and adult tobacco users (see Supplementary Table A for these results).
Table 2.
Descriptive Associations Among Daily Exposure to Peer Tobacco Product Users, Daily Exposure to Adult Tobacco Product Users, and Daily Tobacco Use, n = 950 d
| Variable | Days in which participants did not use tobacco n/column n (%) | Days in which participants used tobacco n/column n (%) | p Valueb |
|---|---|---|---|
| Daily exposure to peer tobacco usersa | |||
| Days in which participants were not exposed to peers who use tobacco | 550/715 d (76.92) | 64/234 d (27.35) | <.001 |
| Days in which participants were exposed to peers who use tobacco | 165/715 d (23.08) | 170/234 d (72.65) | |
| Daily exposure to adult tobacco usersa | |||
| Days in which participants were not exposed to adults who use tobacco | 435/714 d (60.92) | 85/233 d (36.48) | <.001 |
| Days in which participants were exposed to adults who use tobacco | 279/714 d (39.08) | 148/233 d (63.52) |
aColumn percentages are provided in parentheses.
b p Values were calculated using chi-square tests.
Mediation
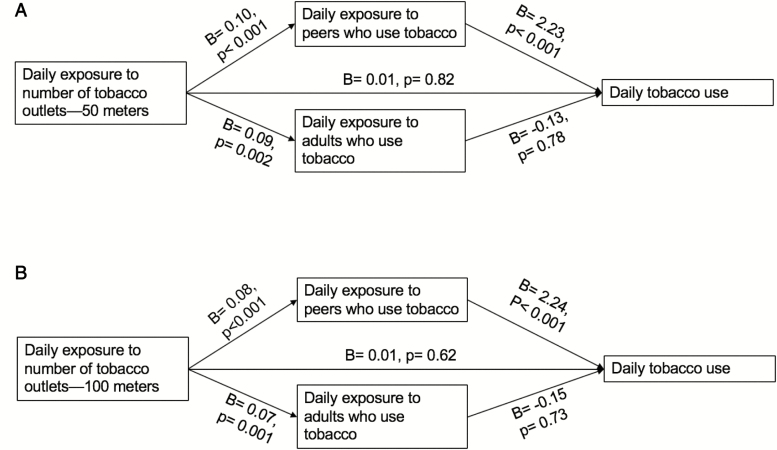
As seen in Figure 1a and b, our structural equation modeling contains two main pathways: (1) the pathway from tobacco retail outlet exposure to the potential mediators and (2) the pathway from the potential mediators to tobacco use.
Figure 1.
Mediation results from models in which daily exposure to number tobacco outlets within 50 m of polylines was modeled as the exposure (a) and daily exposure to number of tobacco outlets within 100 m of polylines was modeled as the exposure (b). In panel a, the Akaike information criterion value was 2358.47 and the Bayesian information criterion value was 2484.73. The indirect effect through exposure to peers who use tobacco was significant at p = .001. The indirect effect through exposure to adults who use tobacco was not significant at p = .78. In panel b, the Akaike information criterion value was 2356.07 and the Bayesian information criterion value was 2482.34. Indirect effect through exposure to peers who use tobacco was significant at p = .001. The indirect effect through exposure to adults who use tobacco was not significant at p = .73.
Exposure to Number of Tobacco Outlets Within 50 m and 100 m of Activity Space Polylines
Controlling for demographics, we found no association between daily tobacco use and number of tobacco outlets within 50 m (probit regression coefficient: 0.01, p = .82, Figure 1a) and 100 m (probit regression coefficient: 0.01, p = .62; Figure 1b) of activity space polylines. However, we found evidence of an indirect effect (p = .001 for both the 50 m and 100 m models) through daily exposure to peers who use tobacco. Specifically, greater daily exposure to tobacco outlets within 50 m and 100 m of activity polylines was positively associated with seeing peers use tobacco on a given day (probit regression coefficient: 0.10, p < .001; probit regression coefficient: 0.08, p < .001, respectively). In turn, seeing peers use tobacco on a given day was positively associated with tobacco use on that day in both the 50 m and 100 m models (probit regression coefficient: 2.23, p < .001; probit regression coefficient: 2.24, p < .001, respectively).
Although increased daily exposure to tobacco outlets within 50 m and 100 m of activity space polylines was also positively associated with daily exposure to adults who use tobacco (probit regression coefficient: 0.09, p = .002; probit regression coefficient: 0.07, p = .001, respectively), there was no association between daily exposure to adults who use tobacco and tobacco use on that day in the 50 m and 100 m models (probit regression coefficient: –0.13, p = .78; probit regression coefficient: –0.15, p = .73). There was, therefore, no indirect effect through daily exposure to adults who use tobacco (p = .78 and p = .73 for the 50 m and 100 m models, respectively).
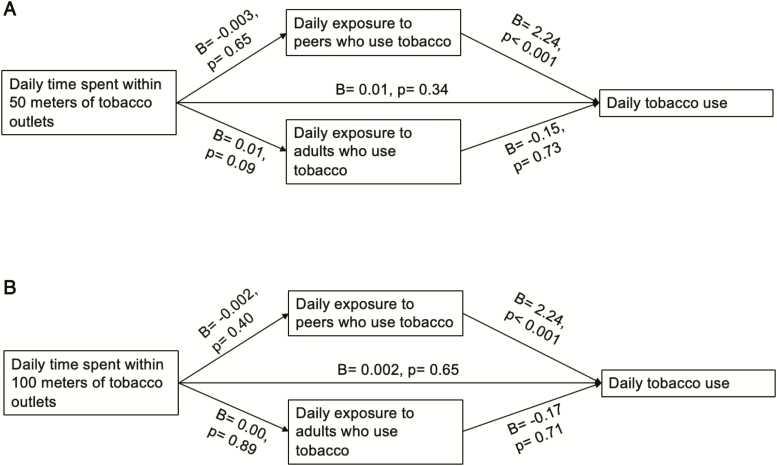
Time Spent Within 50 m and 100 m of Tobacco Outlets
Controlling for demographics, we found no association between daily tobacco use and daily number of minutes participants were within 50 m of tobacco outlets (probit regression coefficient: 0.01, p = .34; Figure 2a) and daily number of minutes participants were within 100 m of tobacco outlets (probit regression coefficient: 0.002, p = .65; Figure 2b), nor evidence of an indirect effect (p = .66, p = .41, respectively) through daily exposures to peers who use tobacco. Specifically, increased number of minutes participants were within 50 m and 100 m of tobacco outlets was not associated with seeing peers use tobacco on a given day (probit regression coefficient: –0.003, p = .65; probit regression coefficient: –0.002, p = .40). However, seeing peers use tobacco on a given day was positively associated with tobacco use on that day in both the 50 m and 100 m models (probit regression coefficient: 2.24, p < .001; probit regression coefficient: 2.24, p < .001).
Figure 2.
Mediation results from models in which daily time spent within 50 m of tobacco outlet was modeled as the exposure (a) and daily time spent within 100 m of tobacco outlet polylines was modeled as the exposure (b). In panel a, the Akaike information criterion value was 2393.64 and the Bayesian information criterion value was 2520.24. The indirect effect through exposure to peers who use tobacco was not significant at p = .66. The indirect effect through exposure to adults who use tobacco was not significant at p = .74. In panel b, the Akaike information criterion value was 2382.69 and the Bayesian information criterion value was 2508.96. The indirect effect through exposure to peers who use tobacco was not significant at p = .41. The indirect effect through exposure to adults who use tobacco was not significant at p = .90.
Similarly, greater time participants spent within 50 m and 100 m of tobacco outlet was not associated with daily exposure to adults who use tobacco (probit regression coefficient: 0.01, p = .09; probit regression coefficient: 0.00, p = .89, respectively) and there was no association between daily exposure to adults who use tobacco and tobacco use on that day (probit regression coefficient: –0.15, p = .73; probit regression coefficient: –0.17, p = .71, respectively). There was, therefore, no indirect effect through daily exposure to adults who use tobacco (p = .74 and p = .90 for the 50 m and 100 m models, respectively).
Discussion
Extending previous findings,3–8 this study is one of the first to examine what factors may mediate the association between exposure to tobacco outlets and tobacco use and also one of the first to use time-ordered data. We found that daily exposure to tobacco outlets within activity spaces affects youth tobacco use through exposure to peers who use tobacco, but not adults. Implications for research, practice, and policy are discussed subsequently.
In contrast to at least one previous exploratory study that used a similar population and activity space measures,10 we found no direct effect of exposure to tobacco outlets on daily tobacco use. It is possible that exposure to tobacco outlets promotes youth tobacco use in a more long-term cumulative manner, such as by increasing receptivity to tobacco products via advertising and promotion and increasing perceptions of the prevalence and acceptability of tobacco use in the general population. It is also likely that the mechanism through which exposure to tobacco outlets influences tobacco use depends on the population (eg, smokers or nonsmokers) and behaviors (eg, tobacco use initiation and cessation) being examined. For instance, in studies of smokers and attempting quitters, researchers found that exposure to tobacco outlets can trigger lapses in quitting, increase impulse tobacco purchases, and reduce self-efficacy to quit smoking.33–35 Our study included both current and never tobacco users. It is therefore possible that exposure to tobacco outlets would therefore not have had an immediate or direct effect on daily tobacco use.
Interestingly, we found that exposure to peers who use tobacco, but not adults, was associated with daily tobacco use. Social cognitive theory suggests that adolescents learn about tobacco use by observing peers and are reinforced to use tobacco if they gain acceptance from peers or establish a particular social identity.2,17,18,36 A large body of research has established that peers’ tobacco use is an important determinant of youth and young adult tobacco use.1,20,37–39 Research also suggests that adolescents often obtain tobacco products from peers40—therefore affording another mechanism through which peer tobacco use influences youth tobacco use. Finally, during adolescence and young adulthood, there is an increasing desire to fit in with peers, which can increase the influence of peers’ substance use.38,41 It is important to note that our measure of “exposure to peers who use tobacco” could have been a proxy for tobacco use norms.42 It is also possible that our measure of exposure to peers who use tobacco could have acted as a cue to use tobacco or that youth were going to tobacco outlets to acquire tobacco with their friends, because many youth use tobacco socially.43 Regardless, it appears that exposure to peers who use tobacco is an important determinant of youth tobacco use and future research could be conducted to disentangle what this measure is capturing.
Contrary to previous research suggesting the importance of adult tobacco use as a determinant of youth tobacco use,19,44 we found no associations between exposure to adult tobacco users and daily tobacco use. It is possible that youth exposure to peer tobacco users increases opportunities to obtain and use tobacco with peers, whereas exposure to adult tobacco users in the community has more overall but not daily effects on youth tobacco use. Peer tobacco use would therefore be related to participants’ momentary tobacco use, as we examined in this study, whereas adult tobacco use would be more distally related to use.
We also found that exposure to number of tobacco outlets was associated with daily exposure to both peer and adult tobacco users. From previous research, we know that the prevalence of cigarette smoking is higher in neighborhoods with tobacco outlets than in neighborhoods without any tobacco outlets.3 Moreover, another study found that teens perceive more adults to be smoking if they live in a neighborhood with more tobacco outlets.45 This is the first study, to the best of our knowledge, that directly examines the link between exposure to tobacco outlets and exposure to tobacco users, particularly by using GEMA data. Interestingly, we found no association between time spent near tobacco outlets and exposure to peer and adult tobacco users, suggesting that exposure effects are because of increased opportunities to see or obtain tobacco from peers rather than the time of exposure.
Results suggest that policies to reduce exposure to tobacco outlets and interventions to address social influences of tobacco use could be used to reduce youth tobacco use. Importantly, our analysis allowed us to investigate exposure to tobacco outlets, exposure to peer and adult users, and tobacco use in a time-ordered design that suggests that these may be causal effects. Communities in the United States have already begun to regulate density and number of tobacco retailers using various strategies (e.g., prohibiting sales in certain venues like pharmacies, prohibiting sales near youth populated areas, such as schools).46 Our findings provide additional significant support for policy makers considering these options. In addition, interventions focusing on peer tobacco use as a determinant of youth tobacco use will continue to be important and should consider how youths’ daily environment increases opportunities for such social influences. For example, a telephone application could send a comic strip with an anti-tobacco message from peers when youth are near tobacco outlets. To this point, some researchers have begun using “just-in-time adaptive interventions”47—to reduce tobacco use and smoking cravings.48
Limitations
We acknowledge a number of limitations. First, we relied on self-reported measures of tobacco use and exposure to peers and adults who use tobacco. Second, we cannot establish that exposure to tobacco outlets came before exposure to people who use tobacco or that exposure to people who use tobacco came before daily tobacco use; although using real-time-ordered data helps lessen this concern. Third, we only examined two possible mediators—exposure to peers and adults using tobacco. There are other plausible mechanisms through which exposure to tobacco outlets influences youth tobacco use. Fourth, we did not control for other factors that may have influenced youth tobacco use, for example, family history of tobacco use, stress. Fifth, it is possible that local policies in some of the cities influenced daily tobacco use. However, the intraclass correlation for daily tobacco use by city was 0.0436 and the between-city variance in daily tobacco use was not significant, which suggests that participants’ cities had small effects on daily tobacco use. Finally, data came from a convenience sample of youth in California and results may not generalize to other populations or locations.
Conclusions
Results of the current study suggest that exposure to tobacco outlets within activity spaces affects youth tobacco use through exposure to peers who use tobacco. Building on these findings, future research could examine other mechanisms through which tobacco retail outlets influence tobacco use. Policies and interventions to regulate both tobacco retail outlet density and social influences of tobacco use may be helpful in preventing and reducing youth tobacco use.
Funding
This research and preparation of this article were supported by grant 25IR-0029 from the California Tobacco-Related Disease Research Program (TRDRP) and grant P60-AA006282 from the National Institute on Alcohol Abuse and Alcoholism (NIAAA) of the National Institutes of Health (NIH). The content is solely the responsibility of the authors and does not necessarily represent the official views of the TRDRP, NIAAA, or NIH.
Conflicts of Interest
None declared.
Supplementary Material
References
- 1. U.S. Department of Health and Human Services. The Health Consequences of Smoking--50 Years of Progress: A Report of the Surgeon General. Rockville, MD: 2014. Available at: https://www.ncbi.nlm.nih.gov/books/NBK179276/pdf/Bookshelf_NBK179276.pdf Accessed January 4, 2016. [Google Scholar]
- 2. U.S. Department of Health and Human Services. Preventing Tobacco Use Among Youth and Young Adults: A Report Of The Surgeon General. Rockville, MD: 2012. Available at: https://www.surgeongeneral.gov/library/reports/preventing-youth-tobacco-use/index.html. Accessed December 13, 2018. [Google Scholar]
- 3. Henriksen L, Feighery EC, Schleicher NC, Cowling DW, Kline RS, Fortmann SP. Is adolescent smoking related to the density and proximity of tobacco outlets and retail cigarette advertising near schools? Prev Med. 2008;47(2):210–214. [DOI] [PubMed] [Google Scholar]
- 4. Henriksen L, Feighery EC, Wang Y, Fortmann SP. Association of retail tobacco marketing with adolescent smoking. Am J Public Health. 2004;94(12):2081–2083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Henriksen L, Schleicher NC, Feighery EC, Fortmann SP. A longitudinal study of exposure to retail cigarette advertising and smoking initiation. Pediatrics. 2010;126(2):232–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Loomis BR, Kim AE, Busey AH, Farrelly MC, Willett JG, Juster HR. The density of tobacco retailers and its association with attitudes toward smoking, exposure to point-of-sale tobacco advertising, cigarette purchasing, and smoking among New York youth. Prev Med. 2012;55(5):468–474. [DOI] [PubMed] [Google Scholar]
- 7. Shortt NK, Tisch C, Pearce J, Richardson EA, Mitchell R. The density of tobacco retailers in home and school environments and relationship with adolescent smoking behaviours in Scotland. Tob Control. 2016;25(1):75–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Paynter J, Edwards R, Schluter PJ, McDuff I. Point of sale tobacco displays and smoking among 14-15 year olds in New Zealand: a cross-sectional study. Tob Control. 2009;18(4):268–274. [DOI] [PubMed] [Google Scholar]
- 9. Finan LJ, Lipperman-Kreda S, Abadi M, et al. Tobacco outlet density and adolescents’ cigarette smoking: a meta-analysis. Tob Control. 2019;28(1):27–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lipperman-Kreda S, Morrison C, Grube JW, Gaidus A. Youth activity spaces and daily exposure to tobacco outlets. Health Place. 2015;34:30–33. [DOI] [PubMed] [Google Scholar]
- 11. Zenk SN, Schulz AJ, Matthews SA, et al. Activity space environment and dietary and physical activity behaviors: a pilot study. Health Place. 2011;17(5):1150–1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rainham DG, Bates CJ, Blanchard CM, Dummer TJ, Kirk SF, Shearer CL. Spatial classification of youth physical activity patterns. Am J Prev Med. 2012;42(5):e87–e96. [DOI] [PubMed] [Google Scholar]
- 13. Shareck M, Kestens Y, Vallée J, Datta G, Frohlich KL. The added value of accounting for activity space when examining the association between tobacco retailer availability and smoking among young adults. Tob Control. 2016;25(4):406–412. [DOI] [PubMed] [Google Scholar]
- 14. Mason MJ, Mennis J, Zaharakis NM, Way T. The dynamic role of urban neighborhood effects in a text-messaging adolescent smoking intervention. Nicotine Tob Res. 2016;18(5):1039–1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mason M, Mennis J, Way T, et al. Young adolescents’ perceived activity space risk, peer networks, and substance use. Health Place. 2015;34:143–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Duncan DT, Kawachi I. Chapter 1: Neighborhoods and health. In: Duncan DT, Kawachi I, eds. Neighborhoods and Health. New York, NY: Oxford University Press; 2018. [Google Scholar]
- 17. Bandura A. Social Foundations of Thought And Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- 18. Fishbein M, Ajzen I.. Predicting and Changing Behavior: The Reasoned Action Approach. New York, NY: Psychology Press, Taylor & Francis; 2010. [Google Scholar]
- 19. Thrul J, Lipperman-Kreda S, Grube JW, Friend KB. Community-level adult daily smoking prevalence moderates the association between adolescents’ cigarette smoking and perceived smoking by friends. J Youth Adolesc. 2014;43(9):1527–1535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Villanti A, Boulay M, Juon HS. Peer, parent and media influences on adolescent smoking by developmental stage. Addict Behav. 2011;36(1–2):133–136. [DOI] [PubMed] [Google Scholar]
- 21. Mennis J, Mason M, Ambrus A, Way T, Henry K. The spatial accuracy of geographic ecological momentary assessment (GEMA): error and bias due to subject and environmental characteristics. Drug Alcohol Depend. 2017;178:188–193. [DOI] [PubMed] [Google Scholar]
- 22. Lipperman-Kreda S, Mair C, Grube JW, Friend KB, Jackson P, Watson D. Density and proximity of tobacco outlets to homes and schools: relations with youth cigarette smoking. Prev Sci. 2014;15(5):738–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lipperman-Kreda S, Grube JW, Friend KB, Mair C. Tobacco outlet density, retailer cigarette sales without ID checks and enforcement of underage tobacco laws: associations with youths’ cigarette smoking and beliefs. Addiction. 2016;111(3):525–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. ChangeLab Solutions. Tobacco Laws Affecting California 2018. Available at: https://www.changelabsolutions.org/sites/default/files/2018_CA_Law_Booklet_FINAL_20180627.pdf. Accessed March 13, 2019.
- 25. American Lung Association in California. State of Tobacco Control 2018: California Local Grades 2018. Available at: https://www.lung.org/local-content/california/documents/state-of-tobacco-control/2018/2018-sotc-california-full.pdf. Accessed March 13, 2019.
- 26. Peters EN, Schauer GL, Rosenberry ZR, Pickworth WB. Does marijuana “blunt” smoking contribute to nicotine exposure?: Preliminary product testing of nicotine content in wrappers of cigars commonly used for blunt smoking. Drug Alcohol Depend. 2016;168:119–122. [DOI] [PubMed] [Google Scholar]
- 27. D’Angelo H, Fleischhacker S, Rose SW, Ribisl KM. Field validation of secondary data sources for enumerating retail tobacco outlets in a state without tobacco outlet licensing. Health Place. 2014;28:38–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Goodman E, Adler NE, Kawachi I, Frazier AL, Huang B, Colditz GA. Adolescents’ perceptions of social status: development and evaluation of a new indicator. Pediatrics. 2001;108(2):E31. [DOI] [PubMed] [Google Scholar]
- 29. Preacher KJ, Zhang Z, Zyphur MJ. Alternative methods for assessing mediation in multilevel data: the advantages of multilevel SEM. Struct Eq Model. 2011;18(2):161–182. [Google Scholar]
- 30. Tofighi D, Thoemmes F. Single-level and multilevel mediation analysis. J Early Adolesc. 2014;34(1):93–119. [Google Scholar]
- 31. Gunzler D, Chen T, Wu P, Zhang H. Introduction to mediation analysis with structural equation modeling. Shanghai Arch Psychiatry. 2013;25(6):390–394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. UCLA Institute for Digital Research and Education. Probit Regression—MPlus Data Analysis Available at: https://stats.idre.ucla.edu/mplus/dae/probit-regression/. Accessed October 5, 2018.
- 33. Burton S, Spanjaard D, Hoek J. An investigation of tobacco retail outlets as a cue for smoking. Austr Mark J. 2013;21(4):234–239. [Google Scholar]
- 34. Kirchner TR, Cantrell J, Anesetti-Rothermel A, Ganz O, Vallone DM, Abrams DB. Geospatial exposure to point-of-sale tobacco: real-time craving and smoking-cessation outcomes. Am J Prev Med. 2013;45(4):379–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Mennis J, Mason M. Tobacco outlet density and attitudes towards smoking among urban adolescent smokers. Subst Abus. 2016;37(4):521–525. [DOI] [PubMed] [Google Scholar]
- 36. Bandura A. Social Learning Theory. Englewood Cliffs, NJ: Prentice Hall; 1977. [Google Scholar]
- 37. Liu J, Zhao S, Chen X, Falk E, Albarracín D. The influence of peer behavior as a function of social and cultural closeness: a meta-analysis of normative influence on adolescent smoking initiation and continuation. Psychol Bull. 2017;143(10):1082–1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Van Ryzin MJ, Fosco GM, Dishion TJ. Family and peer predictors of substance use from early adolescence to early adulthood: an 11-year prospective analysis. Addict Behav. 2012;37(12):1314–1324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Powell LM, Tauras JA, Ross H. The importance of peer effects, cigarette prices and tobacco control policies for youth smoking behavior. J Health Econ. 2005;24(5):950–968. [DOI] [PubMed] [Google Scholar]
- 40. Meyers MJ, Delucchi K, Halpern-Felsher B. Access to tobacco among California high school students: the role of family members, peers, and retail venues. J Adolesc Health. 2017;61(3):385–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Spear LP. The adolescent brain and age-related behavioral manifestations. Neurosci Biobehav Rev. 2000;24(4):417–463. [DOI] [PubMed] [Google Scholar]
- 42. Eisenberg ME, Forster JL. Adolescent smoking behavior: measures of social norms. Am J Prev Med. 2003;25(2):122–128. [DOI] [PubMed] [Google Scholar]
- 43. Pepper JK, Coats EM, Nonnemaker JM, Loomis BR. How do adolescents get their e-cigarettes and other electronic vaping devices? Am J Health Promot. 2019;33(3):420–429. [DOI] [PubMed] [Google Scholar]
- 44. Richardson A, Williams V, Rath J, Villanti AC, Vallone D. The next generation of users: Prevalence and longitudinal patterns of tobacco use among US young adults. Am J Public Health. 2014;104(8): 1429–1436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Schleicher NC, Johnson TO, Fortmann SP, Henriksen L. Tobacco outlet density near home and school: associations with smoking and norms among US teens. Prev Med. 2016;91:287–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Ackerman A, Etow A, Bartel S, Ribisl KM. Reducing the density and number of tobacco retailers: policy solutions and legal issues. Nicotine Tob Res. 2017;19(2):133–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Nahum-Shani I, Smith SN, Spring BJ, et al. Just-in-Time Adaptive Interventions (JITAIs) in mobile health: key components and design principles for ongoing health behavior support. Ann Behav Med. 2018;52(6):446–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Cerrada CJ, Dzubur E, Blackman KCA, Mays V, Shoptaw S, Huh J. Development of a just-in-time adaptive intervention for smoking cessation among Korean American emerging adults. Int J Behav Med. 2017;24(5):665–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.