Supplemental Digital Content is available in the text
Keywords: mammary gland hyperplasia, Tui Na, Rupixiao
Abstract
To study the effects of Tui Na therapy on patients with mammary gland hyperplasia.
A total of 68 female patients with mammary gland hyperplasia were included in this retrospective study from May 2016 to May 2017 and assigned into control group (N = 34) treated with Rupixiao only (a proprietary Chinese medicine) or Tui Na group (N = 34) treated with Tui Na (Chinese massage) combined with Rupixiao. The pain intensity (visual analogous scale, VAS) and serum levels of luteinizing hormone (LH), estradiol (E2), prolactin (PRL), and progesterone (P) were examined before and after the treatment.
The efficacies were 94.1% (32/34) in the Tui Na group and 76.5% (26/34) in the control group (P = .04). After treatment, VAS in Tui Na groups was significantly lower than that in control group (2.1 ± 1.1 vs 3.1 ± 1.1, P < .05). After follow-up for five months, the recurrence rates were 12.5% (4/32) in the Tui Na group and 23.1% (6/26) in the control group (P = .01). The levels of all 4 hormones in the Tui Na group increased significantly after treatment. In control group, only LH and E2 levels were significantly increased after treatment.
In patients with mammary gland hyperplasia, Tui Na combined with Rupixiao could improve clinical symptoms, regulate sex hormone levels, and decrease the recurrence rate than Rupixiao alone. Our finding suggests that Tui Na can be potentially used for the treatment of mammary gland hyperplasia.
1. Introduction
Mammary gland hyperplasia is a benign disorder, which commonly happens in adult females.[1] The clinical symptoms of mammary gland hyperplasia include breast lump and nipple discharge, worsening during menstrual periods. Mammary gland hyperplasia has an increased risk to develop into breast cancer and cause anxiety and life disturbance in affected patients.[2,3] As a complex disease, mammary gland hyperplasia could be affected by multiple factors, such as age, race, lifestyles, menstrual history, breastfeeding, and obesity.[4] Endocrine dysfunction is the main cause of the disease. Estrogen (E2) can expand and extend the ducts of the breast, promote the use of protein and sugar, and increase the permeability of capillaries. Progesterone (P) can further facilitate the estrogen activity into lobules and reduce the transparency of the capillaries. Prolactin (PRL), a hormone released by the pituitary gland, can promote breast epithelial growth and influence other sex hormones, such as E2 and luteinizing hormone (LH). Therefore, the imbalance among sex hormones and their receptors has a major impact on mammary gland development.[5,6]
To date, there is no consensus or guideline for the treatment of mammary gland hyperplasia. The common management in clinical settings includes hormone therapy and surgical excision.[7] The traditional Chinese herbal medicine has been shown to play an important role in the regulation of sex hormone to relieve symptoms and improve prognosis in patients with mammary gland hyperplasia.[8] For example, Wang et al demonstrated that Huiru Yizeng Yihao, a Chinese herbal medicine can significantly regulate disorder of hyperprolactinemia and eliminate the formation of mammary gland hyperplasia in a rat model.[9] Recently, Zhou et al reported protective and therapeutic effects of Rupixiao on mammary gland hyperplasia in rat model.[10] Tui Na, a Chinese massage therapy, is a fundamental part of traditional Chinese medicine (TCM). In a small human study, Lv et al found that mammary gland hyperplasia could be significantly improved by massage therapy combined with exercises.[11] When combined with herbal medicines, Tui Na can enhance and speed up the effects of Chinese herbal medicines. Furthermore, the combination of Tui Na with Chinese herbs can improve clinical outcomes in patients with various disorders.[12–15] However, whether the combination of Tui Na with Chinese herbal medicine can improve mammary gland hyperplasia has never been reported.
In this study, female patients with mammary gland hyperplasia were divided to 2 groups receiving Rupixiao only (control group) and a combination of Tui Na and Rupixiao (Tui Na group) for 12 weeks. We measured pain intensity and serum levels of sex hormones (i.e., E2, P, PRL, and LH) before and after the treatments in all patients.
2. Materials and method
2.1. Study design and participants
This study was approved by the Ethics Committee of the Traditional Chinese Medicine Hospital of Xinjiang Uyghur Autonomous Region (2015XE0122–1). Inclusion criteria were:
-
1)
diagnosis of mammary gland hyperplasia based on the diagnostic criteria established by Breast Health and Disease Prevention Group from the Women's Health Branch of Chinese Preventive Medicine Association;[16]
-
2)
disease duration more than 2 months;
-
3)
age 18 to 35 years old.
Exclusion criteria were:
-
1)
breast infection or malignant tumor;
-
2)
serious liver or kidney dysfunctions.
A total of 68 female patients with mammary gland hyperplasia who received treatment in the Department of Massage, the Traditional Chinese Medicine Hospital of Xinjiang Uyghur Autonomous Region, between May 2016 and May 2017 were included in our study. Patients were randomly assigned based on the medical record number into control group (n = 34, Rupixiao only) or the Tui Na group (n = 34, a combination of Tui Na and Rupixiao).
2.2. Study protocol
All treatments started 1 week before expected menses. All patients in both groups received the oral Rupixiao capsule (Chinese Food and Drug Administration Approval (FDA) number Z10970115, Guangdong Pharmaceutical Co., Ltd, China), 5 capsules each time, 3 times daily for 12 weeks (as 1 cycle). Patients in Tui Na group received Tui Na in the out-patient department once a day (Monday to Friday) for 12 weeks. Tui Na was held during the menses. Tui Na was performed by a team of experienced professional Chinese massage therapists. Patients were in the supine and relaxing pose. At the level of horizontal nipple line, pressing and rubbing manipulations were applied around edges of breasts to the nipples. Then, acupoint massages with point-pressing techniques were applied to Ashi, Tanzhong, and bilateral Rugen for 3 minutes. The pressing intensity was controlled within the patients’ tolerance without any pain. Afterwards, along the lines for the liver, conception vessel, and flush vessel meridians, kneading technique was applied to the acupoints at Guanyuan, Qihai, and Tianshu for 3 minutes each, with gentle and soft manipulations. Patients were then changed to prone position. Rolling technique was used back and forth along the bladder meridian for 3 to 5 minutes. At the end, pressing and kneading massages were applied to the bilateral Ganyu, Jueyinyu, Yanglingquan, Zusanli, Ligou, Yinlingquan, and Taichong acupoints.
Baseline data were collected from all patients. The visual analogue scale (VAS) was used to assess pain intensity (0–10 with a higher number correlating to higher pain intensity). The serum levels of sex hormones, including E2, P, PLR, and LH were measured by an automatic biochemical analyzer (HITACHI 7020, Japan). VAS and serum levels were measured before (1 week prior to the menses) and after the treatment in all patients.
2.3. Outcome measurements
At the end of 12-week, the primary outcome was evaluated based on the guideline for new Chinese medicine published by FDA.[17] The outcomes were assigned into 3 categories:
-
1)
complete improvement: breast pain was completely relief. Cord-like induration became smaller or disappeared with the breast palpation examination;
-
2)
partial improvement: breast pain was partially relieved. Cord-like induration became smaller with the breast palpation examination;
-
3)
no improvement: patients did not meet above criteria.
The total rate of improvement was calculated as: total rate of improvement = (number of significant improvement + number of partial improvement) / total number of patients × 100%. The secondary outcomes included VAS and serum levels of LH, E2, PRL, and P. Patients were followed up for their disease recurrence 5 months after the completion of the treatments.
2.4. Statistical analysis
Continuous data were presented as mean ± standard deviation, and categorical data were presented as percentage, when appropriately. Student t test was used to compare continuous data and Chi-square analysis was used to compare categorical data, after examining for test assumptions. All statistical tests were performed with SPSS software (version 18.0, IBM, USA). A P < .05 was considered statistically significantly different.
3. Results
There were no statistically significant differences in basic information (including age, disease duration, VAS, and serum levels of sex hormones) between the 2 groups (Table 1). All patients completed treatments and were followed up for five months after the treatments. The patient enrollment flowchart is shown in Figure 1.
Table 1.
Baseline characteristic of patients in Tui Na and control groups (N = 68).
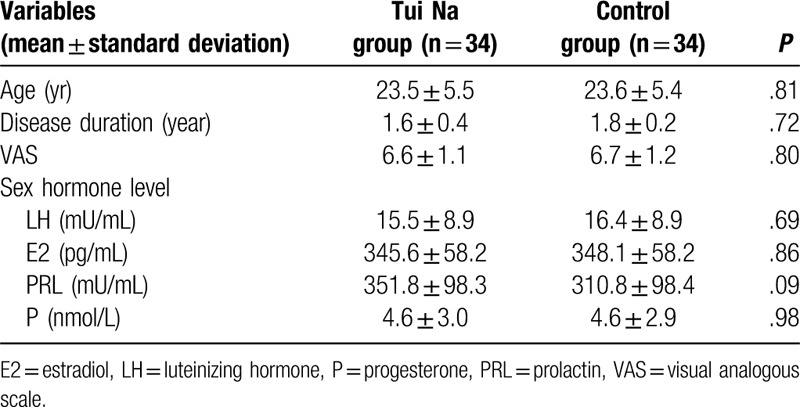
Figure 1.
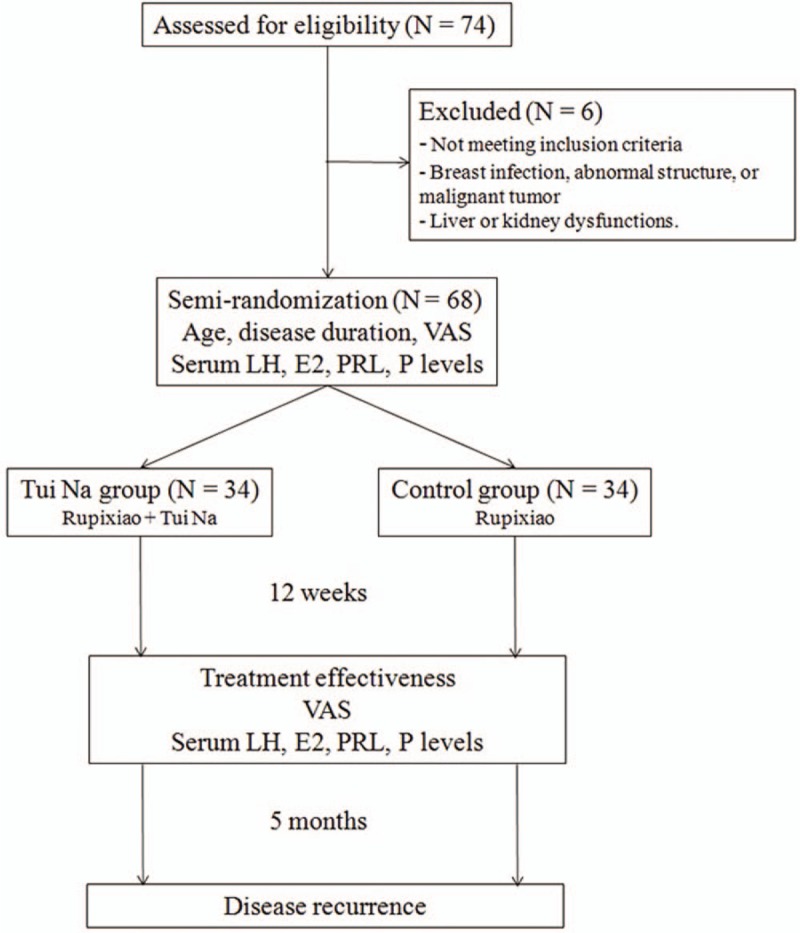
Patient enrollment flowchart (E2 = estradiol, LH = luteinizing hormone, PRL = prolactin, P = progesterone, VAS = visual analogous scale).
Compared with patients in control group, the percentage of patients with symptom improvement was significantly higher in the Tui Na group (76.5% vs 94.1%, P = .04) (Table 2).
Table 2.
Outcome of patients in Tui Na and control groups (N = 68).
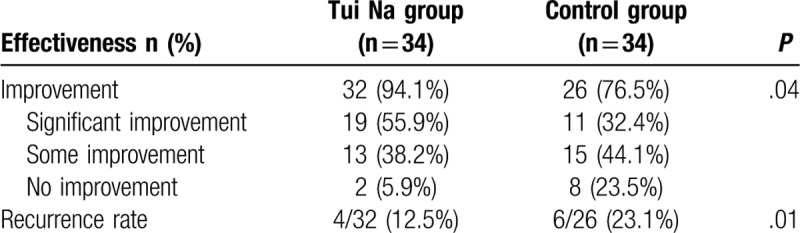
After the treatment, VAS scores were significantly lower in Tui Na group than control group (2.1 ± 1.1 vs 3.1 ± 1.1, P < .01). There were statistically significant increases in the serum levels of LH, E2, PRL, and P (all P < .01) in the Tui Na group. However, we only detected significant increases in serum levels of LH and E2 in the control group (Fig. 2, Supplemental Table 1). At the end of 5-month after the treatment, the recurrence rate was 12.5% (4/32) in the Tui Na group and 23.1% (6/26) in the control group (P = .01, Table 2).
Figure 2.
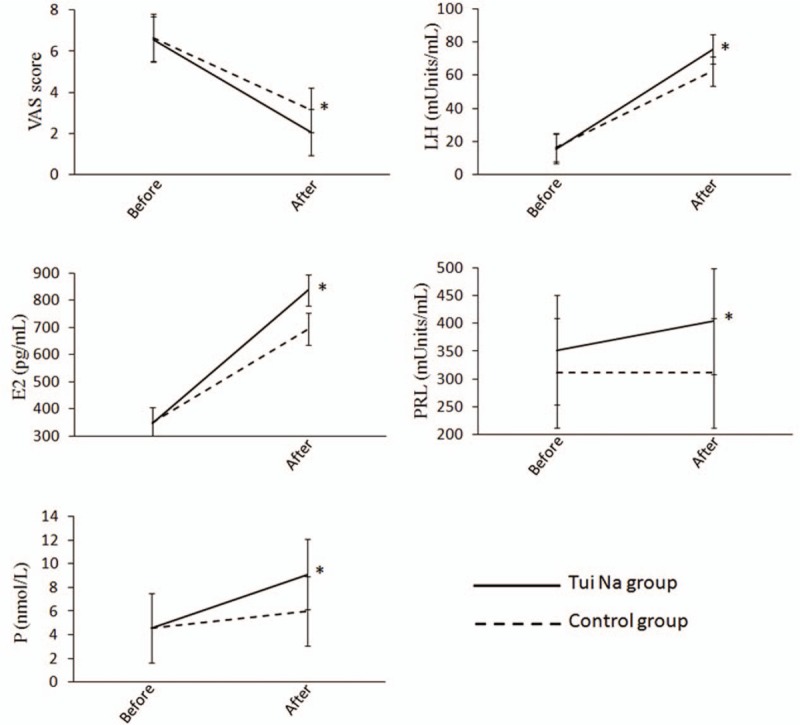
Secondary outcomes in the Tui Na and the control groups (E2 = estradiol, LH = luteinizing hormone, PRL = prolactin, P = progesterone, VAS = visual analogous scale). ∗, P < .01 when comparing the Tui Na group with the control group in the post-treatment period.
4. Discussion
Mammary gland hyperplasia is a common disease in women, and the appropriate management is still under investigation. Traditional treatments include hormone therapy and endocrine therapy by supplementations of steroid, vitamin A, B6, or E to restore the disordered hormone system.[18,19] However, the side effects and complications of those treatments are serious and the curative effect in long-term application is doubtful.[8] Chinese massage, Tui Na, combined with herbs, could be one treatment option for patients with mammary gland hyperplasia.
Based on the Qi and blood balance theory in TCM, the major pathogenesis of mammary gland hyperplasia includes stagnation of Qi and blood circulation, as well as Chong-Ren meridian disorder, which is consistent with the concepts in modern medicine.[8] First, emotional discomforts or sudden mental aggravations could lead to stagnation of Qi and blood circulation, which may eventually result in blockage in the breast collateral and pain. Second, Chong-Ren meridian disorder explains that breast collateral stagnancy, sputum accumulation, and blood stasis could lead to nodule formation. Therefore, in TCM, removal of liver stagnation, regulation of Qi, and coordination of Chong-Ren meridians are critical important in the treatment of mammary gland hyperplasia.
Tui Na stimulates the acupressure points to remove blockage and balance the flow of Qi and blood in the meridians, thereby, alleviating common health problems. Tui Na has been used for thousands of years to help treat muscle pain or stiffness in the body.[12–14] However, whether it can be used to help breast pain in mammary gland hyperplasia has never been reported. In the current study, based on the TCM theory of stagnation of Qi and Chong-Ren meridian disorder, we included local breast acupoints and acupoints in the liver meridian, as well as acupoints to regulate the Chong-Ren meridians in Tui Na. This study shows that Tui Na could reduce the intensity of breast pain and alleviate clinical symptoms. Tui Na could help to improve blood circulation and reduce edema, which could eventually decrease the stimulations to the nerve fibers by mammary gland and relief pain caused by the liver Qi stagnation in patients with mammary gland hyperplasia
Dysregulation of sex hormones plays an important role in the pathogenesis of mammary gland hyperplasia. These sex hormones can interact each other and play a complicated role in the mammary gland development.[5,6] E2, PRL and P can promote the growth of breast ducts and also maintain lactation. P can further facilitate the estrogen activity into lobules and reduce the transparency of the capillaries. PRL can promote breast epithelial growth and influence other sex hormones, such as E2 and LH, whereas LH has inhibitory effects in the lobules of mammary gland. Although limited, increasing evidence has suggested the role of sex hormone regulation by Tui Na. For example, Huang et al found that Tui Na combined with drug therapy can regulate ovulation and secretion of sex hormones to normal levels compared with the those received only drug therapy in patients with polycystic ovarian syndrome.[20] In addition to pain relief, Tui Na is also effective in reducing stress, encouraging relaxation and deepening sleep, which may all contribute to the regulation of hormone imbalance.[21,22] Our finding of increased sex hormone levels in Tui Na group suggest that Tui Na can be potentially used for the prevention and treatment, possibly through regulation serum sexual hormones. The exact role of these sex hormone changes after Tui Na requires more investigations in future studies. More studies using molecular biology techniques are needed to reveal the mechanisms of Tui Na in the treatment of mammary gland hyperplasia, which could shed light on the effective treatment for the disease.
Rupixiao is a commonly used oral herb to treat mammary gland hyperplasia.[23,24] It is a compound preparation, containing multiple components (i.e., antler, dandelion, kelp, loulu seaweed, TCS, millettia, three-seven, red peony root, woody, scrophulariaceae, cortex moutan, prunella vulgaris, forsythia, and safflower) with potential functions in mammary gland hyperplasia.[10] For example, Antler can regulate Chong-Ren meridians and has been used to dissipate blood stasis and reduce edema in breast blood congestion and painful swellings. Dandelion can mediate meridians and has been used treat acute breast painful swellings through detoxification. Kelp and seaweed are commonly combined to soften mass and dispel block. Loulu, forsythia, and prunella vaulgaris are components with detoxification and detumescence effects. In addition, loulu can guide to dredge the breast collateral, and prunella vulgaris can inhibit the proliferation of the connective tissue and slow down the hyperplasia of mammary gland and interstitial matrix. Millettia, three-seven, red peony root, cortex moutan, and safflower can promote blood circulation and remove stagnation. The compound preparation from all components could coordinate to soften mass, dispel block, improve blood circulation, and remove stagnation.[25]
Limitations of the current investigation included single center study, small sample size, and a short follow-up period. Future multi-center studies with larger sample size and longer follow-up are required to better evaluate the efficacy and elucidate the underlying mechanisms of Tui Na in mammary gland hyperplasia.
5. Conclusion
In conclusion, our study results showed that Tui Na combined with oral Rupixiao could improve clinical symptoms and decrease the recurrence rate in patients with mammary gland hyperplasia more effectively than Rupixiao alone.
Author contributions
DL and CW contributed to the study design. DR, JL, NJ, XM, YL, YQ, ZX, and LS collected the data and performed the data analysis. All authors prepared the manuscript.
Supplementary Material
Footnotes
Abbreviations: E2 = estradiol, LH = luteinizing hormone, P = progesterone, PRL = prolactin, TCM = Traditional Chinese Medicine, VAS = visual analogue scale.
How to cite this article: Li D, Wang C, Ruan D, Li J, Ji N, Ma X, Li Y, Qu Y, Xuan Z, Song L. Chinese massage, Tui Na, combined with herbs improves clinical symptoms and regulates sex hormones in patients with mammary gland hyperplasia. Medicine. 2020;99:21(e20300).
DL and CW contributed equally to this work.
Ethical approval was given by the Ethics Committee of Traditional Chinese Medicine Hospital of Xinjiang Uyghur Autonomous Region (2015XE0122-1).
All parents gave their written consent.
The study was supported by the program of Natural Science Foundation of Xinjiang Uygur Autonomous Region, grand No. 2018D01C287.
All the authors declare that they have no conflict of interest.
Supplemental Digital Content is available for this article.
The datasets generated during and/or analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
References
- [1].Thomas ET, Del Mar C, Glasziou P, et al. Prevalence of incidental breast cancer and precursor lesions in autopsy studies: a systematic review and meta-analysis. BMC Cancer 2017;17:808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Yu QC, Verheyen EM, Zeng YA. Mammary development and breast cancer: a Wnt perspective. Cancers (Basel) 2016;8: [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Coradini D, Boracchi P, Oriana S, et al. Epithelial cell identity in hyperplastic precursors of breast cancer. Chin J Cancer 2015;34:121–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Ying J, Shen XY, Ding GH, et al. Study on surface infrared radiation spectrums of danzhong (CV 17) in the patient of hyperplasia of mammary glands. Zhongguo Zhen Jiu 2008;28:499–502. [PubMed] [Google Scholar]
- [5].Brisken C, O’Malley B. Hormone action in the mammary gland. Cold Spring Harb Perspect Biol 2010;2:a003178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Russo IH, Russo J. Role of hormones in mammary cancer initiation and progression. J Mammary Gland Biol Neoplasia 1998;3:49–61. [DOI] [PubMed] [Google Scholar]
- [7].Hartmann LC, Degnim AC, Santen RJ, et al. Atypical hyperplasia of the breast--risk assessment and management options. N Engl J Med 2015;372:78–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Li X, Xin P, Wang C, et al. Mechanisms of traditional chinese medicine in the treatment of mammary gland hyperplasia. Am J Chin Med 2017;45:443–58. [DOI] [PubMed] [Google Scholar]
- [9].Wang X, Chen YG, Ma L, et al. Effect of Chinese medical herbs-Huiru Yizeng Yihao on hyperprolactinemia and hyperplasia of mammary gland in mice. Afr J Tradit Complement Altern Med 2013;10:24–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Zhou D, Wan R, Jia Y, et al. The anti-hyperplasia of mammary gland effect of Chinese Traditional Medicine compound RPXT in Rats. SDRP J Food Sci Technol 2019;4:840–5. [Google Scholar]
- [11].Lv P, Chong Y, Zou H, et al. A study of using massage therapy accompanied with stretching exercise for rehabilitation of mammary gland hyperplasia. Biomed Res Int 2016;2016:9426167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Guo A, Meng Q. Acupuncture combined with spinal tui na for treatment of primary dysmenorrhea in 30 cases. J Tradit Chin Med 2008;28:7–9. [DOI] [PubMed] [Google Scholar]
- [13].Wei X, Wang S, Li L, et al. Clinical evidence of chinese massage therapy (Tui Na) for cervical radiculopathy: a systematic review and meta-analysis. Evid Based Complement Alternat Med 2017;2017:9519285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Lu CN, Friedman M, Lin HC, et al. Alternative therapy for patients with obstructive sleep apnea/hypopnea syndrome: a 1-year, single-blind, randomized trial of Tui Na. Altern Ther Health Med 2017;23:16–24. [PubMed] [Google Scholar]
- [15].Yang M, Feng Y, Pei H, et al. Effectiveness of Chinese massage therapy (Tui Na) for chronic low back pain: study protocol for a randomized controlled trial. Trials 2014;15:418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Association BHaDPGftWsHBoCPM. Experts consensus on diagnosis and treatment of breast hyperplasia. Chin J Pract Surg 2016;36:759–62. [Google Scholar]
- [17].Administration CFaD. Guidelines on clinical investigation of new Chinese medicine. Chin Med Sci Tech 2002;366–8. [Google Scholar]
- [18].Brentnall AR, Cuzick J. Atypical hyperplasia of the breast. N Engl J Med 2015;372:1269–70. [DOI] [PubMed] [Google Scholar]
- [19].Cuzick J, Sestak I, Thorat MA. Impact of preventive therapy on the risk of breast cancer among women with benign breast disease. Breast 2015;24: Suppl 2: S51–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Huang M, Lai H, Lv F, et al. Moxibustion in treating polycystic ovarian syndrome. Massage Methodol 2007;01. [Google Scholar]
- [21].ter Horst JP, de Kloet ER, Schachinger H, et al. Relevance of stress and female sex hormones for emotion and cognition. Cell Mol Neurobiol V 32 2012;725–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Lord C, Sekerovic Z, Carrier J. Sleep regulation and sex hormones exposure in men and women across adulthood. Pathol Biol 2014;62:302–10. [DOI] [PubMed] [Google Scholar]
- [23].Peng Z, Shen H, Gu J. Clinical observation of breast hyperplasia treated with auricular point sticking therapy and Xiaopijian. Zhongguo Zhen Jiu 2015;35:778–80. [PubMed] [Google Scholar]
- [24].Niu BZ, Li YH. Observation on clinical therapeutic effect of point sticking therapy on hyperplasia of mammary glands. Zhongguo Zhen Jiu 2008;28:179–82. [PubMed] [Google Scholar]
- [25].Chinese Pharmacopoeia Commission. Pharmacopoeia of the People's Republic of China, China Medical Science Press: Beijing, China 2015;1:1454–5. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


