The coronavirus disease 2019 (COVID-19) pandemic necessitates identifying laboratory markers to assist the clinicians in early recognition of severe disease [1]. Given the unclear association of hypoalbuminemia and severe COVID-19, we conducted a systematic review and meta-analysis to answer this.
An extensive literature search of PubMed/MEDLINE, Embase, Cochrane, and Web of Science was conducted through April 3, 2020, using search strategy created by an experienced librarian (W.L.S). Two independent reviewers (M.A. and R.F.) performed screening and data extraction of articles. Articles were selected if they reported data on COVID-19 patients with respect to hypoalbuminemia. Discrepancy in screening/data collection was resolved through mutual discussion. Random-effects meta-analysis was conducted, and odds ratio (OR) and mean difference (MD) for proportional and continuous variables were computed, respectively. For each outcome, forest plot, 95% confidence interval (CI), p value (< 0.05 considered statistically significant), and I2 statistic (> 50% considered as substantial heterogeneity) was generated using Open Meta Analyst (CEBM, Oxford, UK).
Severe COVID-19 was defined as respiratory distress (with either rate ≥ 30/min, oxygen saturation ≤ 93% at rest, and/or PaO2/FiO2 ≤ 300 mmHg), ICU admission, and/or death [1]. Hypoalbuminemia was reported based on reference laboratory parameters for each study.
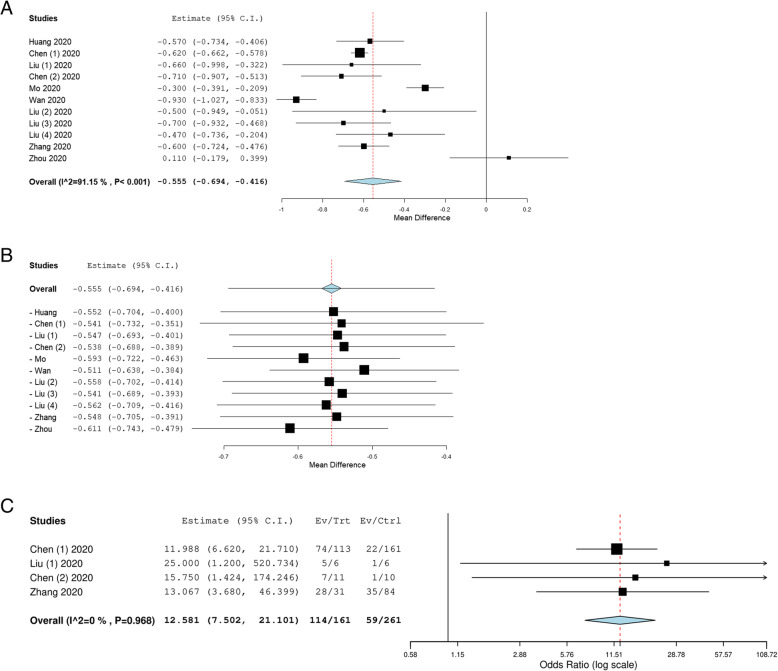
A total of 11 studies (with 910 patients, mean age 47.6 ± 8.2 years and 47.0% females) were included (Table 1). The weighted mean serum albumin on admission was 3.50 g/dL (CI 3.26–3.74 g/dL) and 4.05 g/dL (CI 3.82–4.27 g/dL) in severe and non-severe COVID-19 group, respectively. This was statistically significant (MD:− 0.56 g/dL, CI -0.69 to -0.42 g/dL, p < 0.001, I2 = 91.2%)(Fig. 1a). Leave-one-out meta-analysis was consistent with point estimate (MD) ranging from -0.61 to -0.51 g/dL (Fig. 1b). The results were consistent on subgroup analysis of 8 studies that defined severe COVID-19 based on respiratory distress definition (MD -0.58 g/dL, 95% CI -0.78 to -0.37 g/dL, p < 0.001, I2 = 87.9%). Four studies assessed the hypoalbuminemia status and severe COVID-19 and increased risk was demonstrated (OR 12.6, 95% CI 7.5–21.1, p < 0.001, I2 = 0%) (Fig. 1c).
Table 1.
Study characteristic and demographics of included patients (n no. of patients, NR not reported, SD standard deviation)
| Study, year | Country | Language | Hospital | Study period | Total patients | Mean/median age | Female gender,n (%) | Severe patients#, n (%) | Serum albumin level, mean (SD) g/dL | |
|---|---|---|---|---|---|---|---|---|---|---|
| Severe | Non-severe | |||||||||
| Huang, 2020 [2] | China | English | Jinyintan Hospital | Dec 16 to Jan 2 | 41 | 49 | 11 (26.8%) | 13 (31.7%) | 2.83 (0.24) | 3.4 (0.27) |
| Chen (1), 2020 [3] | China | English | Tongji Hospital | Jan 13 to Feb 28 | 274 | NR | NR | 113 (41.2%) | 3.03 (0.06) | 3.65 (0.26) |
| Liu (1), 2020 [4] | China | English | Shenzhen Third People’s Hospital | Jan 11 to Jan 21 | 12 | 58.9 | 4 (33.3%) | 6 (50.0%) | 3.77 (0.25) | 4.43 (0.34) |
| Chen (2), 2020 [5] | China | English | Tongji Hospital | Dec to Jan 27 | 21 | 56 | 4 (19.0%) | 11 (52.4%) | 3.02 (0.24) | 3.73 (0.22) |
| Mo, 2020 [6] | China | English | Zhongnan Hospital | Jan 1 to Feb 5 | 155 | 54 | 69 (44.5%) | 92 (59.4%) | 3.6 (0.31) | 3.9 (0.27) |
| Wan, 2020 [7] | China | English | Chongqing University Three Gorges Hospital | Jan 23 to Feb 8 | 135 | 47 | 63 (46.7%) | 40 (29.6%) | 3.59 (0.26) | 4.52 (0.27) |
| Liu (2), 2020 [8] | China | Chinese | Multicenter | Jan 23 to Feb 8 | 32 | 38.5 | 12 (37.5%) | 4 (12.5%) | 3.55 (0.44) | 4.05 (0.34) |
| Liu (3), 2020 [9] | China | Chinese | Jianghan University Affiliated Hospital | Jan 10 to Jan 31 | 30 | 35 | 20 (66.7%) | 4 (13.3%) | 3.5 (0.21) | 4.2 (0.28) |
| Liu (4), 2020 [10] | China | English | Multicenter | Dec 30 to Jan 15 | 78 | 38 | 39 (50.0%) | 11 (14.1%) | 3.66 (0.43) | 4.13 (0.33) |
| Zhang, 2020 [11] | China | English | Zhongnan Hospital | Jan 18 to Feb 22 | 115 | 49.52 | 66 (57.4%) | 31 (30.0%) | 3.44 (0.31) | 4.04 (0.28) |
| Zhou, 2020 [12] | China | English | Ninth Hospital of Nanchang | Jan 28 to Feb 6 | 17 | 41.7 | 11 (64.7%) | 5 (29.4%) | 4.6 (0.28) | 4.49 (0.27) |
#Respiratory distress (rate ≥ 30/min, oxygen saturation ≤ 93% at rest and/or PaO2/FiO2 ≤ 300 mmHg), ICU admission and/or death
Fig. 1.
Forest plot demonstrating a meta-analysis comparing mean serum albumin, b leave-one-out meta-analysis comparing mean serum albumin, and c meta-analysis comparing hypoalbuminemia status for patients in severe vs non-severe group (C.I. confidence interval)
Hypoalbuminemia status has been associated with critically ill patients and mortality across numerous clinical settings [13]. The pathophysiology behind hypoalbuminemia in disease state (such as pancreatitis, infection, trauma, burn, and organ dysfunction) is thought to be secondary to increased capillary permeability, decreased protein synthesis, decreased half-life of serum albumin, decreased serum albumin total mass, increased volume of distribution, and increase expression of vascular endothelial growth factor [14]. The hallmark of severe COVID-19 includes the cytokine storm and an interplay of some of the aforementioned mechanisms [1].
Our study had some limitations. There was lack of reporting on temporal association of hypoalbuminemia and severe COVID-19. The serum albumin level was noted on admission; however, it is difficult to make conclusive evidence whether severe COVID-19 caused hypoalbuminemia or vice versa. We were also not able to address if hypoalbuminemia should be corrected or not in the current study and needs further evaluation in future studies. The strength of our study is the reporting of large cohort of patients with consistent results across subgroup and sensitivity analysis.
We demonstrate the association of hypoalbuminemia and severe COVID-19. A low albumin level can potentially lead to early recognition of severe disease and assist clinicians in making informed decision for their patients.
Acknowledgements
None
Abbreviations
- CI
Confidence interval
- COVID-19
Coronavirus disease 2019
- ICU
Intensive care unit
- MD
Mean difference
- n
No. of patients
- OR
odds ratio
- SD
standard deviation
Authors’ contributions
Muhammad Aziz: planning and conducting the study, collecting, interpreting data, statistical analysis, drafting the manuscript. Rawish Fatima: collecting data, drafting the manuscript. Wade lee-smith: created the search strategy and critical revision of manuscript. Ragheb Assaly: study design and conception, critical revision of the manuscript. The authors read and approved the final manuscript
Funding
No funding received for preparing this manuscript.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Not obtained as this is a systematic review and meta-analysis of published studies.
Consent for publication
Consent from patients not obtained due to reason above. All authors approved for the submission of the manuscript.
Competing interests
The authors declare no competing/conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Muhammad Aziz, Email: marajani@hotmail.com.
Rawish Fatima, Email: Rawish.f@gmail.com.
Wade Lee-Smith, Email: Wade.Lee@utoledo.edu.
Ragheb Assaly, Email: ragheb.assaly@utoledo.edu.
References
- 1.Aziz M, Fatima R, Assaly R. Elevated interleukin-6 and severe COVID-19: a meta-analysis. J Med Virol. 2020. 10.1002/jmv.25948. [DOI] [PMC free article] [PubMed]
- 2.Huang Chaolin, Wang Yeming, Li Xingwang, Ren Lili, Zhao Jianping, Hu Yi, Zhang Li, Fan Guohui, Xu Jiuyang, Gu Xiaoying, Cheng Zhenshun, Yu Ting, Xia Jiaan, Wei Yuan, Wu Wenjuan, Xie Xuelei, Yin Wen, Li Hui, Liu Min, Xiao Yan, Gao Hong, Guo Li, Xie Jungang, Wang Guangfa, Jiang Rongmeng, Gao Zhancheng, Jin Qi, Wang Jianwei, Cao Bin. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen T, Wu D, Chen H, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091. 10.1136/bmj.m1091. [DOI] [PMC free article] [PubMed]
- 4.Liu Yingxia, Yang Yang, Zhang Cong, Huang Fengming, Wang Fuxiang, Yuan Jing, Wang Zhaoqin, Li Jinxiu, Li Jianming, Feng Cheng, Zhang Zheng, Wang Lifei, Peng Ling, Chen Li, Qin Yuhao, Zhao Dandan, Tan Shuguang, Yin Lu, Xu Jun, Zhou Congzhao, Jiang Chengyu, Liu Lei. Clinical and biochemical indexes from 2019-nCoV infected patients linked to viral loads and lung injury. Science China Life Sciences. 2020;63(3):364–374. doi: 10.1007/s11427-020-1643-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen Guang, Wu Di, Guo Wei, Cao Yong, Huang Da, Wang Hongwu, Wang Tao, Zhang Xiaoyun, Chen Huilong, Yu Haijing, Zhang Xiaoping, Zhang Minxia, Wu Shiji, Song Jianxin, Chen Tao, Han Meifang, Li Shusheng, Luo Xiaoping, Zhao Jianping, Ning Qin. Clinical and immunological features of severe and moderate coronavirus disease 2019. Journal of Clinical Investigation. 2020;130(5):2620–2629. doi: 10.1172/JCI137244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mo P, Xing Y, Xiao Y, et al. Clinical characteristics of refractory COVID-19 pneumonia in Wuhan, China. Clin Infect Dis. 2020;ciaa270. 10.1093/cid/ciaa270.
- 7.Wan S, Xiang Y, Fang W, et al. Clinical features and treatment of COVID-19 patients in northeast Chongqing. J Med Virol. 2020;10.1002/jmv.25783. . [DOI] [PMC free article] [PubMed]
- 8.Liu C, Jiang ZC, Shao CX, et al. Zhonghua Gan Zang Bing Za Zhi. 2020;28:107–11. 10.3760/cma.j.issn.1007-3418.2020.02.003.
- 9.Liu M, He P, Liu HG, et al. Zhonghua Jie He He Hu Xi Za Zhi. 2020;43:E016. 10.3760/cma.j.issn.1001-0939.2020.0016.
- 10.Liu Wei, Tao Zhao-Wu, Wang Lei, Yuan Ming-Li, Liu Kui, Zhou Ling, Wei Shuang, Deng Yan, Liu Jing, Liu Hui-Guo, Yang Ming, Hu Yi. Analysis of factors associated with disease outcomes in hospitalized patients with 2019 novel coronavirus disease. Chinese Medical Journal. 2020;133(9):1032–1038. doi: 10.1097/CM9.0000000000000775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang Y, Zheng L, Liu L, Zhao M, Xiao J, Zhao Q. Liver impairment in COVID-19 patients: A retrospective analysis of 115 cases from a single centre in Wuhan city, China. Liver Int. 2020;10.1111/liv.14455. 10.1111/liv.14455. [DOI] [PubMed]
- 12.Zhou Yulong, Zhang Zhicheng, Tian Jie, Xiong Shaoyun. Risk factors associated with disease progression in a cohort of patients infected with the 2019 novel coronavirus. Annals of Palliative Medicine. 2020;9(2):428–436. doi: 10.21037/apm.2020.03.26. [DOI] [PubMed] [Google Scholar]
- 13.Akirov Amit, Masri-Iraqi Hiba, Atamna Alaa, Shimon Ilan. Low Albumin Levels Are Associated with Mortality Risk in Hospitalized Patients. The American Journal of Medicine. 2017;130(12):1465.e11-1465.e19. doi: 10.1016/j.amjmed.2017.07.020. [DOI] [PubMed] [Google Scholar]
- 14.Soeters Peter B., Wolfe Robert R., Shenkin Alan. Hypoalbuminemia: Pathogenesis and Clinical Significance. Journal of Parenteral and Enteral Nutrition. 2018;43(2):181–193. doi: 10.1002/jpen.1451. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.