Abstract
Background:
Ineffective referral networks in low- and middle-income countries hinders access to evidence-based therapies by hypertensive patients, leading to high cardiovascular mortality and morbidity. The STRENGTHS (Strengthening Referral Networks for Management of Hypertension Across Health Systems) study evaluates strategies to improve referral processes utilizing the International Association of Public Participation framework to engage stakeholders.
Objectives:
This study sought to identify and engage key stakeholders involved in referral of patients in the Ministry of Health, western Kenya.
Methods:
Key stakeholders involved in policy formulation, provision, or consumption of public health care service were mapped out and contacted by phone, letters, and emissaries to schedule meetings, explain research objectives, and obtain feedback.
Results:
Key stakeholders identified were the Ministry of Health, the Academic Model Providing Access to Healthcare, health professionals, communities and their leadership, and patients. Engaging them resulted in permission to contact research in their areas of jurisdiction and enabled collaboration in updating care protocols with emphasis on timely and appropriate referrals.
Conclusions:
Early stakeholder identification and engagement using the International Association of Public Participation model eased explanation of research objectives, building consensus, and shaping the interventions to improve the referral process.
Hypertension is the leading risk factor for cardiovascular disease and the number 1 cause of mortality globally. The bulk (80%) of deaths occur in low- and middle-income countries (LMIC), including Kenya [1]. In LMIC, hypertension affected 1 in 5 adults in 2013 [2], and this is projected to increase to 3 in 4 adults by 2025 [3,4]. Unfortunately, the level of hypertension control in LMIC is poor, with rates ranging from <1% to 36% [5,6]. Inability to achieve target blood pressure at lower tiers of health care and management of hypertension-related complications require patient referral up the health care system to access services and medications unavailable at the lower level [6]. Referral completion rates for nonacute illness in LMIC are low, ranging from 41% to 45% due to a number of failures in the health referral system, which include poor relationships and linkages between referring and receiving facilities, lack of communication and feedback mechanism, and lack of referral monitoring [7–9]. To improve referral compliance, engaging all stakeholders at all tiers of health care is paramount for sustainability of workable, mutually acceptable solutions.
Stakeholder engagement is a bidirectional process whereby an organization or a research team involves relevant stakeholders—the Ministry of Health (MOH), Academic Model Providing Access to Healthcare (AMPATH), health care providers affiliated with the MOH and AMPATH, patients, and communities—to achieve a prescribed outcome—referral completion, blood pressure control, and reduction in cardiovascular risk [10]. The NCD (Noncommunicable Diseases) Global Action Plan 2013 to 2020 realizes that early stakeholder identification and engagement may help bridge the challenges faced by governments in implementing policies aimed at reducing the NCD burden in the LMIC [11]. They cite successes achieved in tackling the human immunodeficiency virus (HIV) scourge in sub-Saharan Africa in the areas of early diagnosis, prevention, and treatment as being a result of a combination of government policies, structures, and multisectorial actions of stakeholders [12]. A similar multisectorial action by stakeholders was used in addressing tobacco use, another risk factor for NCD, with tremendous success in legislations and taxation policies aimed at reducing its consumption [12,13]. Stakeholder engagement to strengthen referral of appropriate cases is crucial to realign health care research with the needs of clinicians, patients, and policy makers by improving relevance of research questions and accelerating translation of evidence into practice [14,15]. However, scanty information exists on engagement of stakeholder in referral of patients with uncontrolled hypertension or hypertension-related complications in sub-Saharan.
The MOH has an elaborate policy document on referral strategies for patients that was developed in 2014 (Kenya Health Sector Referral Strategy, 2014 to 2018), but its implementation has lagged behind due to financial constraints, a reason cited by many LIMC [11,16]. The document cites the “lack of effective referral system monitoring with standardized referral tools to communicate referrals and capture referral data” as a challenge in implementing the referral strategy. It further cites “inadequate financing for operations and maintenance of referral services” as a serious challenge in ensuring proper functioning of the referral system that has made it difficult for the country to achieve universal social health protection coverage, defined as effective access to affordable health care services of adequate quality and financial protection in case of sickness [16]. The existence of the MOH referral policy and structures (NCD office) provides an avenue of partnering with the government and a platform of identifying and engaging multiple stakeholders to experiment with innovative and cost-effective solutions to facilitate the hypertension referral process.
The main objective of the STRENGTHS (Strengthening Referral Networks for Management of Hypertension Across the Health System) study is to conduct transdisciplinary, translational implementation research focused on strengthening referral networks for hypertension control in western Kenya, using a mixed research methodology. The study team has mapped out and engaged key stakeholders involved in referral of patients with hypertension in western Kenya to identify perceived gaps in the referral process for improvement at sites affiliated with the AMPATH program. AMPATH is an academic partnership among Moi Teaching and Referral Hospital, Moi University College of Health Sciences, and a consortium of North American universities led by Indiana University [15]. AMPATH has established an HIV care program that treats >200,000 patients across a catchment population of ~4.5 million [16]. This HIV infrastructure has been used as the foundation to improve the overall health system, specifically including the creation of a chronic disease management (CDM) program in partnership with the MOH. Through this partnership, AMPATH has been able to implement comprehensive task-shifted care at all levels of the health care system. This infrastructure has also been used to create a robust research program in cardiovascular and pulmonary disease, which has been designated as a National Heart, Lung, and Blood Institute Center of Excellence [17,18]. The MOH-NCD office and the AMPATH-CDM partnership provided a platform for other stakeholder identification and engagement. The identification and engagement process needs to start early to build trust and align research objectives with those of the key stakeholder. The identification and engagement of the multiple stakeholders is challenging, complex, and iterative and requires a flexible framework that allows engagement dose variation during the entire life of the research project. We used the International Association of Public Participation (IAP2) framework to identify and effectively engage stakeholders involved in the referral process due to its simplicity and flexibility in varying the dosing of the engagement.
CONCEPTUAL FRAMEWORK
The IAP2 framework clarifies the roles of stakeholders (public or community) in planning and decision making and how much influence the stakeholders have over the planning or decision-making processes. The level of stakeholder engagement varies between research and projects and depends on the degree of controversy and complexity of a project. It identifies 5 levels of stakeholder engagement: inform; consult; involve; collaborate; and empower [19]. Each level articulates the engagement goal and promise to the stakeholders from the vantage point of the research team. At the “inform” level of engagement, the researcher’s goal is to provide the stakeholders with honest, balanced, and objective information to assist them in understanding the problem the research is to address, the research objectives, and alternative opportunities and/or solutions available for the stated problem. Success at this level is characterized by stakeholders who are adequately informed to reach their own conclusions as to appropriateness of the research and the adequacy of the decisions and solutions brought forward by the research team. This level is unidirectional, with information flowing from the research team to the stakeholders and happens across the entire spectrum of the framework. Some writers have argued that it should not exist as a separate level but be placed across the entire spectrum to demonstrate that “effective engagement with stakeholders at all levels on the Spectrum requires a strategic flow of information” [18].
At the “consult” level, the goal of engagement is to obtain stakeholder feedback on analysis, alternatives, and/or decisions touching on the intended research or intervention. The research team listens to and acknowledges the concerns of stakeholders, their aspirations, and may incorporate the stakeholder feedback into the planned research.
The “involve” level entails direct engagement with the stakeholders by the research team during the entire project period to ensure their concerns and aspirations are consistently understood and considered. The “collaborate” level is about partnership and sharing between the research team and the stakeholders. The stakeholders highly participate in each aspect of the decision process, including the development of alternatives and the identification of the preferred solution. The “empower” level places the final decision making in the hands of the stakeholder, through processes that may require varying degrees of engagement; for example, little engagement is required in holding a public referendum on an issue affecting a community. As such, the empower level is not necessarily the purview of stakeholder engagement because a stakeholder can make a decision without engaging a researcher or they may be empowered by a law or directive to make certain choices unilaterally. Our research aims to empower both patients and clinicians to aptly complete referral decisions, with the help of technology that is user-friendly and acceptable to them. The IAP2 models applies to our research in many aspects in that the STRENGTHS study uses a participatory research methodology, which solicits views from the public before designing the interventions to facilitate referral completion at the various health care levels. The 5 IAP2 levels are summarized in the IAP2 framework in Figure 1.
FIGURE 1.
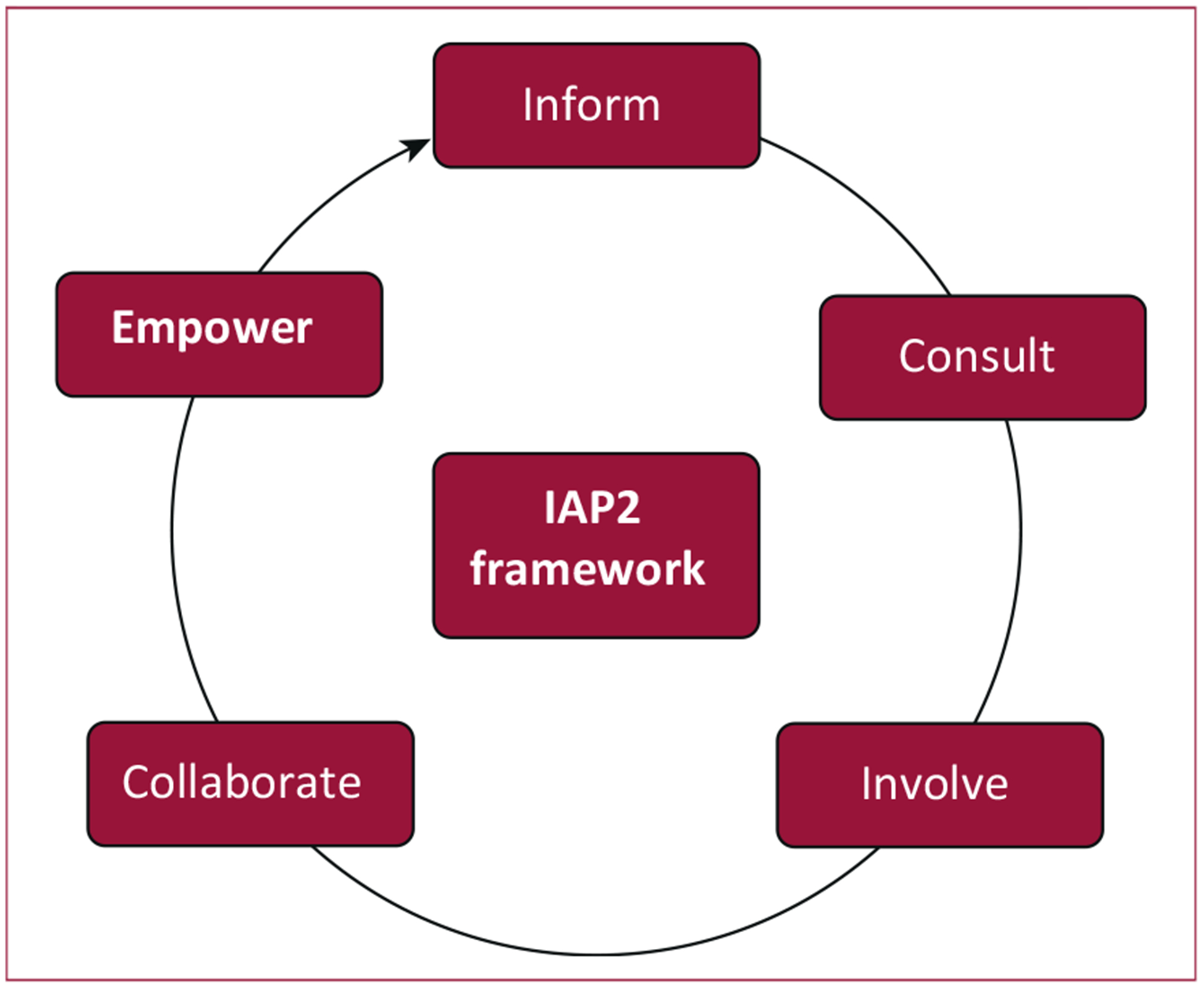
Graphic presentation of the International Association of Public Participation (IAP2) framework for stakeholder engagement.
METHODS
Setting
There are 6 levels of care in the Kenyan public sector health system: community; dispensary; health center; subcounty hospital; county hospital; and national referral hospital [16]. Functionally, these coalesce into the 3 traditional health system levels: primary (dispensary and health center); secondary (subcounty hospital and county hospital); and tertiary (national teaching and referral hospital). The AMPATH-CDM Program has enrolled >15,000 patients with hypertension at 69 facilities spanning the 3 levels of the health system. We are conducting the STRENGTHS project within the AMPATH catchment area across 6 geographically separate referral networks, each centered around a secondary-level health facility staffed by medical officers (physicians who are general practitioners) and clinical officers (analogous to physician assistants). Each of these serves as the link between the tertiary-level center, staffed by specialists and subspecialists, and several primary-level health facilities staffed by clinical officers and nurses.
Participants
We identified stakeholders as persons, groups, or organizations with vested interest in the referral of patients with hypertension from the community through the various levels of the MOH health care system. The key stakeholders were deemed to have significant influence on the referral process policy and their perspectives would be very important for the research success and subsequent uptake of the research results for implementation. Those fitting the above-mentioned criteria and participating in the engagement included the Kenya MOH, AMPATH, health professionals, patients, communities, and their administrators.
Procedure
We gathered data from the public using a participatory research methodology design. The researchers convened community assemblies, locally referred to as “Mabaraza,” where the public and their leadership were informed of the research protocol and deliberated on how to improve referral completions for hypertensive patients. The qualitative data collection occurred over a 6-month period from July 2017 to January 2018 at various participating sites. Their views, concerns, and suggestions have influenced the intervention design and will affect the research products. The researchers’ engagement with the public largely re-flected the IAP2 framework of inform, consult, involve, collaborate, and empower, and they will continue using the model at different stages of the research.
Measures
The meetings to obtain different measures were both informal and formal. We obtained advice and informal verbal assurance from the head of the MOH department of NCD to support implementation of a strategy that would strengthen the referral of hypertension patients prior to preparing the overall research proposal, through a telephone call, and later digitally through e-mail, before writing a formal letter after successful grant application. We held formal meetings with health care administrators and health care providers at the county, subcounty, and community levels after obtaining approval from the Institutional Research and Ethics Committee approval, National Commission for Science and Technology, and AMPATH research office. During the meetings with health professionals, we gave public presentations on our research project and sought understanding and feedback on the same.
RESULTS
A total of 5 key stakeholders involved in the referral process of patients at the different levels of the health care system were identified and mapped out as shown in Figure 2.
FIGURE 2. STRENGTHS (Strengthening Referral Networks for Management of Hypertension Across Health Systems) study stakeholder map.
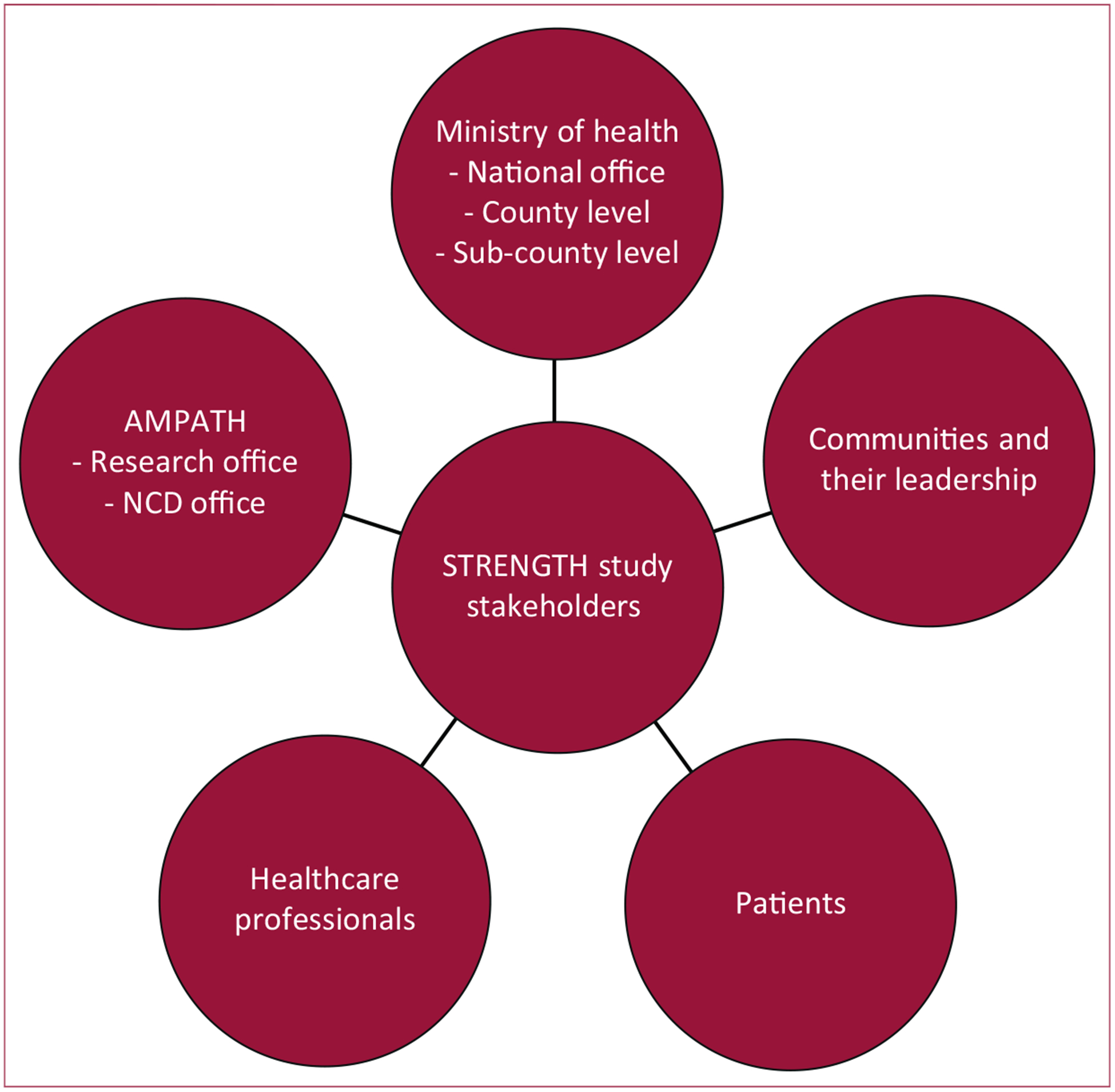
AMPATH, Academic Model Providing Access to Healthcare; NCD, noncommunicable disease.
The MOH houses the national leadership that is the overall policy maker and coordinates countrywide health care activities. It has established the NCD office in accordance with WHO requirements, which oversees and coordinates policy and activities related to NCD. We engaged the head of the NCD office digitally via e-mail, by telephone, and by writing to obtain written clearance to carry out research in the county and subcounty hospitals. The county and subcounty institutions directly fall under the MOH umbrella, but they are currently independent administrative-wise following decentralization of health care to the local (county) government. The county minister of health heads them while the medical officers of health head the subcounty hospitals. We consulted them through writing to gain written permission to hold public meetings with their staff and patients within their facilities.
The AMPATH program has partnered with the MOH to provide clinical care to patients with HIV and now cardiovascular diseases through its NCD office. The AMPATH research office provides permission to carry out research in its areas of operation and helps facilitate community entry through its community entry network. The MOH and AMPATH Center of Excellence have health professionals, mainly physicians, physician assistants (analogous to clinical officers), nurses, nutritionists, public health officers, and health records personnel who play key roles in the referral network of patients. We engaged them during the public presentation of the research protocol and obtained valuable feedback from them that has helped modify our research tools. We held multiple meetings with the AMPATH NCD team of physicians and physician assistants to update clinical care algorithms with emphasis on when to appropriately refer patients with hypertension in tandem with the MOH guidelines. The AMPATH NCD team has been screening community members for HIV, diabetes, and hypertension for over 5 years now, and many of those diagnosed with hypertension require referral to the health facilities to start care.
We held a single interview with key area informants and a focused group discussion with patients at each health facilities to brief them on the study and obtain their perspective on referral of patients with hypertension. The results of our interactions with the multiple stakeholders utilizing the IAP2 model are summarized in Table 1.
TABLE 1.
Summary of stakeholders identified, purpose, and methods of engagement
| IAP2 Domain | Stakeholders Identified | Purpose of Engagement | Methods of Achieving Engagement and Dose | Outcomes and Benefits |
|---|---|---|---|---|
| Inform | MOH | Explain the objectives of STRENGTHS study | Telephone, digitally via e-mail, and formal letters | Written permission to conduct research in MOH and AMPATH areas of operation |
| AMPATH: Leadership and research office | ||||
| Obtain permission to carry out research in their area of jurisdiction | Meeting forums with administrators, health care providers | |||
| Health professionals | Acceptance by patients, health professionals, and the community | |||
| Communities | ||||
| Patients | Ethical approval to carry out research | Presented research protocol for approval | ||
| IREC | Build trust | |||
| Ethical approvals | ||||
| Consult | MOH | Clarify objectives of the study | Group forums with administrators and health care personnel | Gain a different perspective and modify protocol |
| AMPATH | Get feedback on the study | |||
| Community Members, patients, and their leadership | Consider alternative solutions from the stakeholders | Enhance ownership | ||
| Letters | Synchronize goals | |||
| Focused group discussions | ||||
| Involve | MOH | Develop care protocols that highlight referral signals | Group forums with health care personnel and administrators | Enhance ownership and adoption of research findings |
| AMPATH | ||||
| Community members and their leadership | Facilitate access to the community | E-mails | ||
| Collaborate | MOH | Align the STRENGTHS study objectives with those of the MOH and AMPATH | Group forums with health care personnel and administrators | Incorporate the research findings into care |
| AMPATH | ||||
| Community | Enhance sustainability | |||
| Contextualize the referral intervention | ||||
| Empower | MOH | To own the referral strategy for sustainability | Group forums with the leadership and health care personnel (Ongoing) | Enhance sustainability |
AMPATH, Academic Model Providing Access to Healthcare; IAP2, International Association of Public Participation; IREC, Institutional Research and Ethics Committee; MOH, Ministry of Health; STRENGTHS, Strengthening Referral Networks for Management of Hypertension Across Health Systems.
DISCUSSION
Effective stakeholder engagement to strengthen referral systems across health care networks requires involvement of multiple players at different levels of the health delivery network. It is an iterative bidirectional process that begins at conception of the research idea and continuous during the implementation of the research project to increase stakeholder buy-in to ensure sustainability. Identifying stakeholders whose common goal resonates with the key research objectives while maintaining relevance, quality of care, and financial sustainability is key to successful engagement, especially in the LMIC setup [20], due to the double burden of communicable and noncommunicable diseases, financial constraints, and low health care capacity [13,16,20–22]. An effective referral strategy has a potential to improve patient access to the nearest best possible health care that is cost-effective to both the patient and the health system, thus reducing unnecessary referrals (including self-referrals) to secondary facilities [23]. Indeed in our setup, the MOH has an excellent referral process policy that has not been implemented fully due to budgetary constraints. Due to its complexity, the referral system has a multiplicity of stakeholders who must be enjoined in implementation of strategies aimed at improving the referral process, without increasing cost of care, to incorporate their perspective and eventual ownership of the referral process. The IAP2 model is best suited to adopt in engaging these multiple stakeholders due to its simplicity and iterative nature at different stages of the protocol development. The IAP2 framework has been used in populations of Australia, Canada, and United States of America, but this is the first time the model is being used in an LMIC country to engage stakeholders.
The MOH is a key stakeholder in the referral process. It is the entry point of patients into clinical care and provides the physical structures, employs health care workers, and makes the policy on referral of patients with hypertension within the primary, secondary, and tertiary facilities. The success and sustainability of any referral strategy must gain the MOH acceptance and adoption; that is, the strategy must be aligned with Kenyan Health Sector Referral Strategy. By engaging the MOH-NCD leadership in advance and informing them of the intentions to study the current referral strategy for hypertension to identify gaps and opportunities for improvement in writing, we made subsequent collaborations with county and subcounty easier. Public presentation of the research project to health care providers at the county and subcounty elicited a lot of enthusiasm and provided useful feedback that helped design research tools for aim-1 research activities of our study.
The health care workers pointed out frustrations the patients face when referred to secondary or tertiary facilities and that poor communication between the different health care systems compound the issue. The counties have county health committees, with whom we held consultative meetings to further explain the objectives of the research and strictly align it to the county referral goals. They expressed the desire to have their county health information systems and records personnel involved in the design and development of the referral module to ensure that it will communicate with their health information systems. They also requested to be administered quarterly reports on the progress of the study through writing or formal meetings. The facility administrators were key in facilitating the meetings with clinicians and health committees. They work directly with the community strategy officers who in turn facilitate meetings with the community.
AMPATH serves as a key collaborator in providing access to the CDM program. Engaging their county and subcounty coordinators yielded smooth entry into the respective areas of operations due to their familiarity with the local leadership and extensive involvement in community research. The engagements of the CDM physicians and their assistants were pivotal in updating the clinical care protocols for hypertension, with emphasis on appropriate referrals based on guidelines. They own the protocols and are embarking on updating the clinicians at the county and subcounty levels on the changes made. Their coordinators work with MOH community strategy officers to coordinate the linkage of patients from the community to the health facilities.
The county health management teams in collaboration with the area chiefs, grass root–selevel administrators, community gatekeepers, and opinion leaders coordinated access to the local communities. The community gate-keepers are key in mobilizing the community members to participate in activities such as interviews and focused group discussions. The community units are organized under the community health workers and community health extension workers and headed by the public health officers. They provided insights into contextualizing our interventions in line with local culture and beliefs. The engagement process is iterative and ongoing as the research unfolds. The IAP2 framework provides flexibility of multiple encounters with each stakeholder, providing an avenue for clarifying issues and obtains feedback on the study. During the engagement process, we have encountered a number of challenges and barriers, which we tried to address in the context of our set up, as shown in Table 2.
TABLE 2.
Challenges, barriers, facilitators, and solutions to stakeholders’ engagement across the IAP2 framework
| Challenges for Stakeholder Engagement | Overcoming Challenges for Stakeholder Engagement |
|---|---|
| Identifying relevant stakeholders and key personnel to engage | Identifying stakeholders and key personnel to engage: we used the existing AMPATH outreach team and the CEC to identify the key people who needed to be advised on the referral process |
| Communicating with stakeholders (indirect links with the county leadership) | |
| Communication with county leadership: we wrote letters, made phone calls. and in some instances sent emissaries to deliver messages | |
| Scheduling meetings with stakeholders (conflicting meetings, meetings cancellation without prior warning) | |
| Scheduling meetings: we approached the alternative representatives of the local leadership, observing the laid out protocols, whenever the designated person had other engagements | |
| Competing health care priorities and a limited budget | |
| Limited budget: we supplied assurance that we will use existing personnel and structures | |
| Structural Barriers | Overcoming Structural Barriers with Facilitators |
| Lack of communication between tiers of health care along the referral cascade | Interfacility communication barriers: we send letters and made phone calls to designated personnel |
| Lack of person or office dedicated to referral of patients across primary, secondary, and tertiary health care facilities | Absence of referral office or personnel: discussed need to develop better communication and reporting protocols, both manual and electronic |
| Geographic barriers: development of care algorithms to minimize referral, determine availability of medications at lower facilities, and task shift care | |
| Great distances between the community and health care facilities, compounded by poor road networks and lack of transport |
CEC, county executive committee; other abbreviations as in Table 1.
Through our engagement with the national health leadership, we learned that the current referral health strategy as laid out in the Kenya Health Sector Referral Strategy (2014 to 2018) is well articulated but has not yet succeeded in improving the health care delivery and referral process. The reasons may be multifactorial, but the gap between the policy intentions and practice is glaring and we hope the STRENGTHS project will highlight some of the gaps and opportunities to help successfully implement the referral strategy. At the regional level, in consultation with the stakeholders, we learned of the need for evidence-based contextualized solutions that would be adopted to improve referral of patients with hypertension and that study findings should be shared at regular intervals to help inform referral strategies.
CONCLUSIONS
We identified and engaged 5 key stakeholders involved in the referral of hypertension patients in western Kenya, namely the MOH, AMPATH, health providers, patients, and communities, using the IAP2 framework. The early engagement enabled us to explain the research objectives and obtained useful feedback that helped shape the final research protocol, which led to smooth endorsement of the protocol by key stakeholders. The IAP2 framework provided the flexibility of engaging the different stakeholders at varying degrees and repeatedly. Stakeholder acceptance of solutions generated is important in guaranteeing sustainability and can be bolstered by aligning research goals with their objectives before research development and implementation.
Acknowledgments
This work is funded by the National Heart, Lung, and Blood Institute (NHLBI) of the National Institutes of Health (NIH), award number 1U01HL138636 under the Hypertension Outcomes for T4 Research within Lower Middle-Income Countries (Hy-TREC) Program.
Footnotes
The authors report no relationships that could be construed as a conflict of interest.
REFERENCES
- 1.World Health Organization. World Health Report: Global Status Report on Noncommunicable Diseases. World Health Organization Report. 2014. Available at: http://www.who.int/nmh/publications/ncd-status-report-2014/en/. Accessed July 31, 2017.
- 2.van de Vijver S, Akinyi H, Oti S, et al. Status report on hypertension in Africa: consultative review for the 6th Session of the African Union Conference of Ministers of Health on NCD’s. Pan Afr Med J 2014;16:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Seedat YK. Hypertension in developing nations in sub-Saharan Africa. J Hum Hypertens 2000;14:739–47. [DOI] [PubMed] [Google Scholar]
- 4.Opie LH, Seedat YK. Hypertension in sub-Saharan African populations. Circulation 2005;112:3562–8. [DOI] [PubMed] [Google Scholar]
- 5.Edwards R, Unwin N, Mugusi F, et al. Hypertension prevalence and care in an urban and rural area of Tanzania. J Hypertens 2000;18:145–52. [DOI] [PubMed] [Google Scholar]
- 6.Steyn K, Gaziano TA, Bradshaw D, Laubscher R, Fourie J. Hypertension in South African adults: results from the Demographic and Health Survey, 1998. J Hypertens 2001;19:1717–25. [DOI] [PubMed] [Google Scholar]
- 7.Uwemedimo OT, Arpadi SM, Chhagan MK, et al. Compliance with referrals for non-acute child health conditions: evidence from the longitudinal ASENZE study in KwaZulu Natal, South Africa. BMC Health Serv Res 2014;14:242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ilboudo TP, Chou YJ, Huang N. Compliance with referral for curative care in rural Burkina Faso. Health Policy Plan 2011;27:256–64. [DOI] [PubMed] [Google Scholar]
- 9.Ministry of Health, Kenya. The State of the Health Referral System in Kenya: Results from a Baseline Study on the Functionality of the Health Referral System in Eight Counties. 2013. Available at: https://www.measureevaluation.org/pima/baseline-assessments/07rssbaselineassessment_rev.pdf. Accessed July 10, 2019.
- 10.Merai R, Siegel C, Rakotz M, et al. CDC Grand Rounds: a public health approach to detect and control hypertension. MMWR Morb Mortal Wkly Rep 2016;65:1261–4. [DOI] [PubMed] [Google Scholar]
- 11.Juma PA, Mohamed SF, Matanje Mwagomba BL, et al. Noncommunicable disease prevention policy process in five African countries. BMC Public Health 2018;18(Suppl 1):961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lo YR, Chu C, Ananworanich J, Excler JL, Tucker JD. Stakeholder engagement in HIV cure research: lessons learned from other HIV interventions and the way forward. AIDS Patient Care STDS 2015;29: 389–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Juma PA, Mapa-Tassou C, Mohamed SF, et al. Multi-sectoral action in non-communicable disease prevention policy development in five African countries. BMC Public Health 2018;18(Suppl 1):953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Antonakoudis G, Poulimenos I, Kifnidis K, Zouras C, Antonakoudis H. Blood pressure control and cardiovascular risk reduction. Hippokratia 2007;11:114–9. [PMC free article] [PubMed] [Google Scholar]
- 15.WHO; UNAIDS; UNICEF. Towards Universal Access: Scaling Up Priority HIV/AIDS Interventions in the Health Sector. Progress report. 2009. Available at: https://www.who.int/hiv/pub/2009progressreport/en/. Accessed July 10, 2019.
- 16.Ministry of Health, Kenya. Kenya health sector referral strategy (2014–2018). Available at: http://guidelines.health.go.ke:8000/media/Ministry-of-Health-Referral-Strategy1.pdf. Accessed July 10, 2019.
- 17.US Department of Health and Human Services. Federal Coordinating Council for Comparative Effectiveness Research Report to the President and Congress. Washington, DC: US Department of Health and Human Services; 2009. [Google Scholar]
- 18.Binanay CA, Akwanalo CO, Aruasa W, et al. Building sustainable capacity for cardiovascular care at a public hospital in western Kenya. J Am Coll Cardiol 2015;66:2550–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.International Association for Public Participation. IAP2 Spectrum. Available at: https://iap2canada.ca/Resources/Documents/0702-Foundations-Spectrum-MW-rev2%20(1).pdf. Accessed July 10, 2019.
- 20.WHO. WHO Noncommunicable Diseases Progress Monitor 2015. Geneva, Switzerland: World Health Organization; 2015. [Google Scholar]
- 21.European Commission. Tools and Methodologies for Assessing the Performance of Primary Care: Report of the Expert Panel on effective ways of investing in Health (EXPH). Available at: https://ec.europa.eu/health/expert_panel/sites/expertpanel/files/docsdir/opinion_primarycare_performance_en.pdf. Accessed July 10, 2019.
- 22.Nyaaba GN, Stronks K, de-Graft Aikins A, Kengne AP, Agyemang C. Tracing Africa’s progress towards implementing the Non-Communicable Diseases Global action plan 2013–2020: A synthesis of WHO country profile reports. BMC Public Health 2017;17:297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Binanay CA, Akwanalo CO, Aruasa W, et al. Building sustainable capacity for cardiovascular care at a public hospital in western Kenya. J Am Coll Cardiol 2015;66:2550–60. [DOI] [PMC free article] [PubMed] [Google Scholar]


