Abstract
The coronavirus disease-2019 (COVID-19) pandemic has put healthcare services all over the world into a challenging situation. The contagious nature of the disease and the respiratory failure necessitating ventilatory care of these patients have put extra burden on intensive care unit (ICU) services. India has been no exception; by March 2020, the number of COVID-19 patients started increasing in India. This article describes the measures taken and challenges faced in creating ample ICU bed capacity to cater to the anticipated load of patients in the state of Delhi, India, as a result of the COVID-19 pandemic. The main challenges faced, among others, were estimating the number of ICU beds to be created; deciding on dedicated hospitals to treat COVID-19 patients; procuring ventilators, personal protective equipment, and other related material; mobilizing human resources and providing their training; and providing isolated in-house accommodations to the staff on duty. The authors acknowledge and agree that the methodology proposed in this article is but one way of approaching this difficult scenario and that there could be other, perhaps better, methods of dealing with such a problem.
Key Words: COVID-19 outbreak, Coronavirus disease-2019, COVID-19, Intensive care, Challenges
IN DECEMBER 2019, many healthcare facilities in Wuhan, China, reported patients with symptoms of severe acute respiratory failure, similar to those observed in 2002 with severe acute respiratory syndrome. On January 7, 2020, a novel strain of coronavirus, severe acute respiratory syndrome coronaviurs-2, was isolated, and this confirmed the circulation of a new disease with respiratory illness, coronavirus disease-2019 (COVID-19).1 The virus spread rapidly to several other countries, and at the time of writing this article (April 12, 2020), the disease had been reported to have spread to 210 countries, with a total number of reported cases of 1,826,245 and deaths of 112,371.2
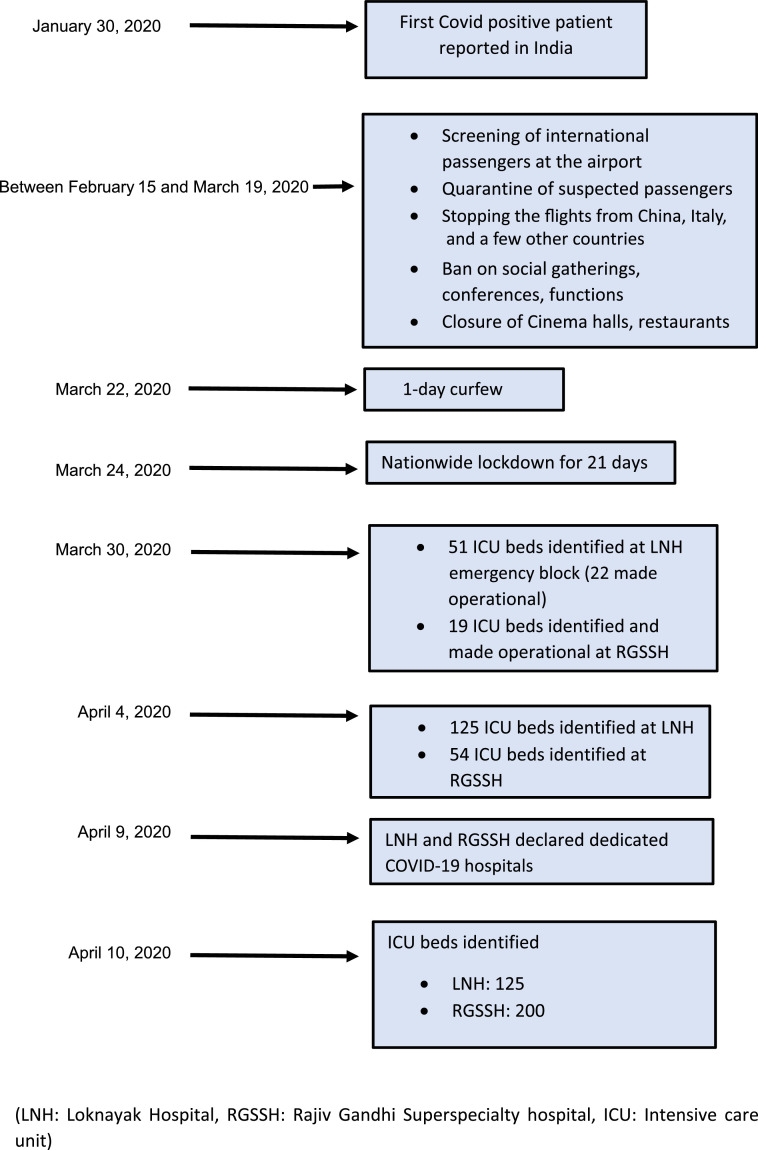
In India, the first case of COVID-19 was reported in the state of Kerala on January 30, 2020, and the number increased to 3. All three were students who had returned from Wuhan, China..3 , 4 The government of India initiated several precautionary measures, such as screening international travelers at the airport and quarantining travelers suspected of being infected with COVID-19. Later, flights from China, Italy, and a few other countries were not allowed to land in the country. In addition, India imposed bans on social gatherings, movies, restaurants, functions, and conferences, among others.
The prime minister of India, Narendra Modi, imposed a 1-day curfew on March 22, 2020, and on March 24, Modi announced a nationwide lockdown for 21 days. These steps initiated by the central government forewarned citizens of the impending danger and set the ball rolling for all the state governments and other agencies to start preparing on a war footing to deal with the pandemic. As of April 12, 2020, there were 7,409 confirmed cases of COVID-19 in India.5 This article is an account of the measures taken and challenges faced in creating ICU bed capacity to cater to the anticipated load of patients needing ICU care during the COVID-19 pandemic.
Basic Groundwork and Planning
On March 24, the chief minister of Delhi formulated a task force committee, with Dr S.K. Sarin as its chairman and authors D.K.T. and G.C.K. as 2 of its other members, with the responsibility to review the current status of preparedness and to recommend urgent measures for the preparedness of Delhi for the COVID-19 pandemic. At that time, there were 31 COVID-19–positive patients in Delhi. In the absence of any published data to suggest how many who were exposed became infected (ie, test positive for COVID-19), the committee took into account World Health Organization estimates and the existing published literature to arrive at a worst-case scenario in Delhi. Accordingly, it was estimated that about 15% of Delhi's population of about 20 million might be exposed during the coming months (ie, around 3 million people may be exposed to COVID-19). It was not known how many might become infected or how many infections would be symptomatic. However, it was known that of those who test positive for COVID-19, about 14% experience severe disease; 5% become critically ill, necessitating ICU admission; 2.3% require mechanical ventilation; and 1.4% die.6
It was a challenging task to estimate the numbers, and after deliberating on various aspects, it was proposed that for Delhi to be prepared, at least 3,000 ICU beds with ventilation available were needed. However, it should be noted that 3,000 ICU beds would not be needed all at one time but that preparedness for 1,000 ICU beds with ventilation available should be considered. In addition, ICU bed capacity would need to be reviewed from time to time. Another aspect that was taken into account was the presence of a dual health-care system in Delhi. Being the capital city, Delhi also has large hospitals run by the central government, which would share the burden of these patients. Even so, the committee decided to persist with these numbers and preferred to err on the safer side.
With these factors in mind, a comprehensive plan to ensure that all aspects needed to provide care to COVID-19 patients, including infrastructure, equipment, disposables, medicines, and human resources, was designed. D.K.T. agreed to be the responsible officer for training and to supervise the ICU services at Delhi state government hospitals.
In Delhi, there is a perpetual shortage of ICU beds; therefore, the biggest challenge was to create sufficient ICU bed capacity for an anticipated surge of COVID-19 patients during the next few weeks. Initially, specialists and residents from all Delhi government hospitals from the departments of anesthesiology, pulmonary medicine, and other specialties, because of their experience in working in the ICUs, would be recruited for managing the ICUs. To meet this challenge, the following fundamental steps were suggested:
-
1.
One or 2 major hospitals should be designated as exclusive COVID-19 hospitals.
-
2.
It was appreciated that best/recommended care may not be possible if there were an excessive load of patients, and in that case, the plan would be to provide optimum care in the existing circumstances.
-
3.
Suspension of elective procedures after initial curtailment in hospitals designated to cater to COVID-19 patients.
-
4.
Arrangements to transfer existing ICU patients initially to other ICUs of the given hospital to make immediate availability of some ICU beds for COVID-19 patients and later transfer to other government non-COVID-19 hospitals.
-
5.
Include all ICUs, such as general ICU, respiratory ICU, coronary care units, medical ICU, surgical ICU, postoperative wards, and any others.
-
6.
Conversion of as many non-ICU beds that have a centralized oxygen source into makeshift ICU beds by providing a ventilator and a monitor.
-
7.
Conversion of nearly all operating rooms into ICUs to be used for COVID-19 patients, if necessary.
-
8.
Urgent purchase of vital equipment, such as ventilators and disposables, to meet the demands of ICU beds created in the aforementioned manner.
-
9.
The aforementioned arrangements should be made in a phased manner because it was realized that all converted ICU beds could not be made available all at once.
-
10.
In case the patient load is increased further, private hospitals may have to be involved in providing ICU care to COVID-19 patients.
Execution
Identifying ICU Beds
Early in the pandemic (March 25, 2020), Lok Nayak Hospital (LNH), an 1,800-bed tertiary care, teaching hospital, and Rajiv Gandhi Super Specialty Hospital (RGSSH), a 450-bed, recently commissioned hospital, were designated for caring for COVID-19 patients. However, they were not declared as exclusive COVID-19 hospitals, but a part (block[s]) of each hospital was to be used for COVID-19 patients.
On March 30, the status at LNH was reviewed, and 51 beds located on different floors of the emergency block were identified as being able to be converted into COVID-19 ICU beds. Some of these were non-ICU beds and were without a ventilator and some were occupied by patients on a ventilator, so a decision was made to transfer those patients to other areas and mobilize ventilators from other areas for use in the COVID-19 ICU.
In this manner, by the evening of March, 30, 2020, a total of 22 ICU beds were placed in the emergency block; and ventilators were being arranged for some of these beds. In the meantime, nearly 80 patients suspected of being infected with COVID-19 were admitted to LNH, 3 of whom were having breathing difficulty and were moved to the newly created COVID-19 ICU for the administration of high-flow oxygen therapy. Thus, the efforts to create a dedicated COVID-19 ICU were put into place. Likewise, the situation was reviewed at RGSSH, and a 19-bed ICU on a single floor was identified and reserved for COVID-19 patients. RGSSH also received about 100 suspected COVID-19 patients, but none of them had breathing difficulty and did not require ICU admission.
There was a sudden surge of patients during the first week of April. In anticipation of an additional surge in numbers, the government decided to convert 3 hospitals into exclusive COVID-19 hospitals; these were LNH, RGSSH, and GB Pant Institute of Postgraduate Medical Education and Research (GIPMER). The other hospitals in Delhi would remain as non-COVID-19 hospitals.
On the morning of April 4, 2020, the status at the 3 designated COVID-19 hospitals was reviewed in relation to the availability of ICU beds. The total number of ICU beds identified were as follows: LNH, 125 beds; GIPMER, 180 beds; and RGSSH, 54 beds (total of 359 beds).
On the morning of April 9, 2020, it was appreciated that because GIPMER is the major super specialty hospital of the Delhi government and converting it into an exclusive COVID-19 hospital could affect the care provided to patients experiencing cardiovascular, neurologic, and gastrointestinal ailments, the decision to declare GIPMER as an exclusive COVID-19 hospital was reversed. Subsequently, the decision was made to add more ICU beds in RGSSH (total of 200) because the 450-bed hospital has oxygen points on almost all its beds. This change would be done in 2 phases of 100 beds each.
Thus, on the morning of April 10, 2020, LNH had 125 ICU beds and RGSSH 200 ICU beds (total of 325 beds). Admission to the ICU would be determined by the severity of disease as defined by the government of India on April 7, 2020. Only patients with severe symptoms (respiratory rate >30/min, arterial oxygen saturation [SpO2] <90% on room air) would be admitted to a COVID-19 ICU; patients with moderate symptoms (respiratory rate 15-30/min, SpO2 90%-94%) would be admitted to dedicated COVID-19 health centers for oxygenation and monitoring.7 The timeline of various important events is depicted in Fig 1 .
Fig 1.
Timeline of important events. COVID-19, coronavirus disease-2019; ICU, intensive care unit; LNH, Lok Nayak Hospital; RGSSH, Rajiv Gandhi Super Specialty Hospital.
Equipment
In this crisis situation, in order to commission as many ICU beds as possible, the minimum amount of equipment required to make a bed functional as an ICU bed was identified. This entailed judicious distribution of available resources and minimizing the requirement of urgent procurement of additional equipment (which were available with difficulty because of shortages) to overcome the deficit of equipment. With these factors in mind, the decision was made that each ICU bed would have the following:
-
1.
ICU ventilator
-
2.
Multiparameter monitor with minimum of electrocardiography, noninvasive blood pressure, and SpO2 monitoring
-
3.
Syringe pump (2 per bed)
-
4.
Ripple bed/air mattress
This allowed for the creation of a maximum number of ICU beds at a given time. The other necessary equipment, including ICU ventilators, deep vein thrombosis pump with garments, portable ultrasound machines, and video laryngoscopes, were added to a list of urgent purchases to be made and submitted to the authorities (Table 1 ), and this would be beneficial to properly equip each ICU bed in the coming days.
Table 1.
List of Equipment, Disposables, Consumables, and Other Items for Urgent Procurement for COVID-19 ICUs
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Abbreviations: ABG, arterial blood gas; AED, automated external defibrillator; COVID-19, coronavirus disease-2019; CVP, central venous pressure; ICU, intensive care unit; NIBP, noninvasive blood pressure.
Ventilators and Multiparameter Monitors
COVID-19 patients likely will experience acute respiratory distress syndrome. It was considered, as a first preference, to use ICU ventilators with the standard modes of ventilation inclusive of airway pressure release ventilation. However, in view of the shortage of ventilators in the market, it was suggested to consider even lower-end ICU ventilators, including even the transport ventilators, which would be used as a backup in situations in which a standard ventilator was not available. In addition, it was recommended that patients in the operating room should be ventilated with anesthesia ventilators installed on the work station/anesthesia machines. In extreme circumstances, a bed without an oxygen source would be used as an ICU bed with the addition of a turbine-based transport ventilator that can ventilate with air. Bi-level positive- pressure ventilation and high-flow oxygen therapy also would be a consideration as well as split ventilation, but the latter would be used only in exceptional, pressing situations with the consent from the patient/relative. As a general principle, it was considered that patients whose condition was deemed salvageable should receive a better ventilator compared with those whose condition was considered difficult to salvage; however, the final decision would be left to the concerned consultant of a particular ICU.
Some agencies came forward with offers to donate ventilators from their resources, which would be helpful to compensate for the deficiency in part. As of April 12, 2020, the additional requirement of ICU ventilators was estimated to be approximately 150 to activate the proposed 325 ICU beds. An equal number of multiparameter monitors also was proposed to be purchased.
Disposables/Medicines
An inventory of various disposables/small equipment that is required to run the ICU was prepared (Table 2 ). The list of medicines required to run the various ICUs also was prepared (Table 3 ). In addition, the readiness of blood banks to fulfill the demand of blood and blood products was considered. A core committee consisting of 5 senior doctors was formed for each hospital to look into the aforementioned requirements and to submit their requests to the appropriate authorities for urgent procurement.
Table 2.
List of Equipment/Disposables Required for Recurrent Use in COVID-19 ICUs
| Equipment |
|---|
| Electric suction machine |
| Crash cart |
| PPE dedicated for COVID-19 |
| N95 mask |
| Alcohol-based sanitizer |
| Disposable endotracheal tube with subglottic suction |
| Laryngoscope with disposable blades (adult sizes 3 and 4 [disposable, plastic]) |
| Video laryngoscope with Macintosh type disposable blades (adult size) |
| Tracheostomy tubes |
| Airway exchange catheter (adult size) |
| Intubation stylet, disposable (adult size) |
| Anesthesia transparent face mask for bag mask ventilation |
| Oropharyngeal airways |
| Nasopharyngeal airways |
| LMA supreme |
| Full body transparent plastic sheet |
| Closed suction catheters |
| Disposable suction containers |
| HME bacterial / viral filters |
| Magill forceps (adult size) |
| HEPA filters |
| Disposable Ambu bags (adult size) |
| Triple-lumen CVP lines (18 F) |
| Ryles tubes (sizes 12/14/16) |
| Syringe infusion pumps |
| High-pressure tubing |
| 3-way stopcock |
| Simple face mask for O2 therapy |
| Ventimask for O2 therapy |
| Nasal prongs for O2 therapy |
| Noninvasive ventilation masks |
| Patient interface/nasal prongs for high-flow nasal oxygen |
| Nonrebreathing face mask with reservoir bag |
| T piece for O2 therapy |
| Disposable tubing for ventilator circuits |
| Deep vein thrombosis pumps and garments |
| Air mattress |
| Consumable items for monitors (eg, SpO2 probes, CO2 sampling lines, NIBP cuff) |
| General equipment as per requirements (eg, gloves, cannulae, syringes, needles) |
| Sodium hypochlorite solution |
| Resealable plastic bags large for samples to be sealed |
| Arterial blood gas and electrolyte analyzer for point-of-care testing |
| Plastic sheet |
Abbreviations: CO2, carbon dioxide; COVID-19, coronavirus disease-2019; CVP, central venous pressure; HEPA, high-efficiency particulate air; HME, heat and moisture exchanger; ICU, intensive care unit; LMA, laryngeal mask airway; NIBP, noninvasive blood pressure; O2, oxygen; PPE, personal protective equipment; SpO2, arterial oxygen saturation.
Table 3.
Drugs and Fluids Required for COVID-19 ICUs
| Drugs and Fluids |
|---|
| Epinephrine |
| Atropine |
| Dopamine |
| Dobutamine |
| Vasopressin |
| Noradrenaline |
| Propofol vial |
| Thiopentone, 500 mg vial |
| Ketamine vial |
| Etomidate ampoule |
| Xylocard vial |
| Amiodarone ampoule |
| Adenosine |
| Succinylcholine vial |
| Rocuronium vial |
| Vecuronium ampoule |
| Morphine ampule, 15 mg |
| Fentanyl, 2 mL ampoule |
| Fentanyl, 10 mL ampoule |
| Midazolam vial |
| Paracetamol/perfalgan, 1 g |
| Perinorm ampoules (Metoclopramide) |
| Ondansetron ampoule |
| Sodium bicarbonate 7.5% ampoule, 10 mL |
| Lasix |
| Calcium gluconate, 10 mL |
| Parenteral nutrition bags, 1 L |
| Syrup potassium chloride |
| Magnesium sulfate ampoules |
| Hydrocortisone |
| Nebulization solutions |
| Asthalin |
| Duolin |
| N-acetyl cysteine |
| Intravenous fluids |
| Dextrose normal saline |
| 5% Dextrose |
| Normal saline |
| Ringer's lactate |
| Tablet hydroxychloroquine, 400 mg |
| Tablet hydroxychloroquine, 200 mg |
| Tablet azithromycin, 500 mg |
| Tablet oseltamivir, 75 mg |
| Heparin vials |
| Low-molecular–weight heparin |
Abbreviations: COVID-19, coronavirus disease-2019; ICU, intensive care unit.
Human Resources
It was recognized by the committee that ICU staff would become fatigued quickly while working with the bulky personal protective equipment (PPE). Hence, it was planned to schedule staff in 6-hour shifts (some countries have preferred to use 4-hour shifts). It was proposed to form a team of staff to manage patients in a 12- to 15-bed ICU. Each team would work for a period of 1 week. The team would be divided into 4 sub-teams to work in 4 shifts of 8 am to 2 pm, 2 pm to 8 pm, 8 pm to 2 am, or 2 am to 8 am. After 1 week, the team would be replaced by another team. The first team would be quarantined for a period of 2 weeks before it could return to work, if necessary. Thus, each team would work for a period of 1 week and then have a rest period of 2 weeks.8 In the beginning, 3 teams were to be assigned to each 10- to 15-bed ICU so that arrangements would be made for the initial 3 weeks. The constitution of each team and the requirement of staff for a period of 3 weeks for 100 ICU patients are shown in Table 4 . The testing protocol for healthcare professionals (HCPs) would be symptom- driven, except before termination of the quarantine period, when it would be mandatory.
Table 4.
Staff Requirement for COVID-19 ICU Services
| Constitution of 1 Team of Staff to Manage a 10- to 15-Bed ICU | Requirement of Staff for 3 Weeks if 100 Patients Are Admitted to ICU (7 ICUs with 15 Beds Each) |
|---|---|
|
|
|
21 |
|
126 |
|
126 |
|
504 |
|
126 |
|
252 |
|
105 |
| Total: 60 | 1260 |
NOTE: Sub-teams would work 1 of the following 4 shifts: 8 am to 2 pm, 2 pm to 8 pm, 8 pm to 2 am, or 2 am to 8 am. Each team would work 6 hour-shifts for 1 week then be quarantined for 2 weeks while a second team would replace the first team at the end of the first week.
Abbreviations: COVID-19, coronavirus disease-2019; ICU, intensive care unit.
Safety of HCPs
It was emphasized that the safety of HCPs was paramount and therefore good-quality PPE must be provided to each HCP. In addition, N95 face masks and sufficient hand scrub antiseptic solution should be readily available to all staff members. A full complement of PPE, inclusive of goggles, face shield, mask, gloves, coverall/gowns (with or without apron), head cover, and shoe cover, as defined by the government of India should be used by the staff working in the ICU.9
Staff Accommodations
It also was understood that all HCPs would be required to go into isolation after finishing their shift duty. Hence, adequate accommodations for HCPs were arranged on the hospital premises. For LNH staff, accommodations were arranged at the adjacent GIPMER by vacating 3 floors of a special ward that has separate rooms with an attached bathroom. In addition, rooms were arranged in a nearby hotel. For RGSSH staff, the newly constructed resident doctor's hostel was proposed to be used for staff accommodations. Adequate arrangements for serving food to these staff members also were determined.
Challenges and Lessons
Considering March 24 as day zero, on day 7 (ie, April 1), 41 ICU beds were created for COVID-19 patients in the 2 hospitals. Although some of them still needed to be equipped to fully function as ICU beds, all of them were available for providing oxygen therapy, and 5 patients needing oxygen therapy were admitted to these beds on day 7 (total number of COVID-19–positive patients in Delhi on this day was 152). The daily COVID-19–positive patients requiring ICU admissions is shown in Table 5 . The daily availability of ICU beds that could be created along with the number of COVID-19–positive patients on that particular day are shown in Table 6 . On day 19 (ie, April 12), the total number of ICU beds that could be created in the 2 hospitals was 105, with another 154 beds that were awaiting availability of ventilators, which was short of the total number (325) of beds that the committee hoped to make fully functional. Fortunately, at that time, the ICUs were sufficient to meet the requirements, with 13 patients admitted to ICUs. The various challenges faced in accomplishing sufficient ICU capacity are shown in Table 7 , and some of the more important challenges are discussed in the following.
Table 5.
Date-Wise COVID-19–Positive Patients in the State of Delhi
| Date | Yesterday | Today | Cumulative | Admissions LNH (Cumulative) ICU/O2/Vent | Admissions RGSSH (Cumulative) ICU/O2/Vent | Private Hospitals (Cumulative) ICU/O2/Vent | Cumulative Deaths |
|---|---|---|---|---|---|---|---|
| Mar 29 | 72 | ||||||
| Mar 31 | 23 | 120 | |||||
| April 1 | 32 | 152 | |||||
| April 2 | 141 | 293 | |||||
| April 3 | 293 | 93 | 386 | 04/04/0 | 0/01/0 | ||
| April 4 | 386 | 59 | 445 | 04/04/0 | 0/01/0 | ||
| April 5 | 445 | 58 | 503 | 04/04/0 | 0/02/0 | ||
| April 6 | 525 | 04/07/0 | 04/04/0 | 11/01/06 | 7 | ||
| April 7 | 525 | 51 | 576 | 06/12/0 | 04/0/0 | 19/12/06 | 9 |
| April 8 | 576 | 93 | 669 | 05/0/0 | 05/05/0 | 12/08/04 | 9 |
| April 9 | 669 | 51 | 720 | 05/05/0 | 05/05/0 | 22/10/07 | 12 |
| April 10 | 720 | 183 | 903 | 07/07/0 | 07/0/0 | 24/11/06 | 14 |
| April 11 | 903 | 166 | 1,069 | 07/07/0 | 07/02/01 | 22/08/4 | 19 |
| April 12 | 1,069 | 85 | 1,154 | 05/6/0 | 07/0/01 | 21/08/04 | 24 |
NOTE. Data were obtained from the Delhi Health Bulletin, which is released daily by the Health Department. Data from central government and private hospitals are not included for indoor patients (blank columns indicate data are not available).
Abbreviations: COVID-19, coronavirus disease-2019; ICU, intensive care unit; LNH, Lok Nayak Hospital; O2, oxygen; RGSSH, Rajiv Gandhi Super Specialty Hospital; vent, on ventilator.
Table 6.
Date-Wise Availability of ICU Beds and Number of COVID-19–Positive Patients
| Date | COVID-19–Positive Patients (Cumulative) | Admitted to ICU (Cumulative) | ICU Beds Available at LNH | ICU Beds Available at RGSSH |
|---|---|---|---|---|
| March 19 | 14 | 0 | 0 | 0 |
| March 24 | 30 | 0 | 0 | 0 |
| March 30 | 97 | 4 | 22 | 19 |
| April 1 | 152 | 5 | 22 | 19 |
| April 4 | 445 | 5 | 51 + 74 more being readied | 19 + 26 more being readied |
| April 5 | 503 | 6 | ||
| April 6 | 525 | 11 | ||
| April 7 | 576 | 16 | ||
| April 8 | 669 | 10 | ||
| April 9 | 720 | 10 | ||
| April 10 | 903 | 14 | Number to be enhanced to 200 | |
| April 11 | 1,069 | 14 | ||
| April 12 | 1,154 | 13 | 70, with 15 more if ventilator is arranged | 35, with 139 more if ventilator is arranged |
NOTE. Data related to COVID-19–positive patients and intensive care unit admissions were obtained from the Delhi Health Bulletin, which is released daily by the Health Department.
Abbreviations: COVID-19, coronavirus disease-2019; ICU, intensive care unit; LNH, Lok Nayak Hospital; RGSSH, Rajiv Gandhi Super Specialty Hospital.
Table 7.
Challenges Faced to Create Additional ICU Facilities at Various Hospitals
|
|
|
|
|
|
|
|
|
|
|
|
Abbreviations: COVID-19, coronavirus disease-2019; ICU, intensive care unit; PPE, personal protective equipment.
Estimating the Number of ICU Beds to Be Created
In the absence of any definite data and not knowing how effective the complete lockdown would be, it was very difficult to estimate even the probable number of ICU beds that likely would be required during the next 4- to- 8 weeks. The authors believed that it would be safer to assume the worst scenario and err on the safer (higher patient census) side for this purpose. The committee projected to create 1,000 ICU beds; but in the first phase, was able to identify only 325 beds that could be converted into ICU beds. One hundred more beds could be created at RGSSH in the next phase, and for additional increase in ICU beds, the ICUs of the private hospitals would need to be included. Because the situation was dynamic, evaluation was necessary at regular intervals.
Dedicated COVID-19 Hospitals
It is crucial to identify dedicated COVID-19 hospitals exclusively for the care of COVID-19 patients. In the initial phase, when the number of cases is small, it may be possible to manage COVID-19 patients in an isolated area of a hospital that also treats non-COVID-19 patients. However, as the number of cases increases, it is most appropriate to designate a particular hospital exclusively for the care of COVID-19 patients. However, this is easier said than done because vacating a hospital that is occupied with non-COVID-19 patients is a challenging task. In this respect, it is important to identify such hospitals that can be vacated relatively easily. The committee believes that there was an error of judgment by identifying GIPMER for this purpose. That initial decision was made on the basis that GIPMER is a super specialty hospital and therefore would be well-equipped to provide ICU care. However, it was soon realized ( in time) that it would be difficult to vacate GIPMER completely and rapidly because it housed many sick patients. Furthermore, suspending super specialty services provided at GIPMER might seriously hamper the care of non-COVID-19 patients. Therefore, the more appropriate choice would have been to dedicate additional ICU capacity for the care of COVID-19 patients at RGSSH, which is another super specialty hospital that is relatively less busy. This decision was corrected in a few days, and services at GIPMER were resumed for non-COVID-19 patients. GIPMER, however, contributed by providing a special ward (housed in a separate block) for the accommodation of staff providing care to COVID-19 patients at the adjacent LNH. Thus, there are a few logistic issues that should be taken into account to decide when and which facilities are to be dedicated as COVID-19 hospital. These logistics, of course, will vary from place to place, and individualization will be necessary.
Procurement of Ventilators, PPE, Masks, and Other Related Material
Because of a sudden increase in the demand of equipment and other disposable materials for managing COVID-19 patients all around the world, and because of the stoppage of import and export materials, there was an acute shortage of critical equipment in India. The government wanted to make bulk purchases of these items, but there were not enough supplies to meet the demands. However, efforts on war footing are ongoing, and sufficient supplies are expected soon. On April 19, a 3-ply surgical mask–making machine that had a capability to produce 100,000 masks per day was set up by the Delhi government. Likewise, the domestic manufacturing of PPE and medical equipment was ramped up to meet the increasing demand. The Defense Research and Development Organization has taken a lead in this matter.10 In addition, substantial material and equipment supplies are expected from the central government and will be shared among all the states of India. These will be used to equip each of the ICU beds dedicated to COVID-19 care in the 2 hospitals.
Human Resources
Because of the sudden increase in the number of ICU beds, the 6-hour duty roster, and a mandatory break of 2 weeks (quarantine period), acute shortage of trained staff should be anticipated. Hence, deployment of additional staff who can work in an ICU from other hospitals will be necessary. It was suggested that a pool of staff should be created as soon as possible so that as and when the situation worsens, the identified staff is readily available for providing necessary care.
Training of Staff
It was decided to arrange for the provision of training to all levels of staff on various aspects related to the management of COVID-19 patients. In particular, the measures and precautions to be taken to avoid contact and spread of the disease were taken into account. Other training measures provided included collection of samples for confirmation of COVID-19, donning and doffing of PPE, basic ventilatory management of a patient in the ICU, general care of a patient in the ICU, and precautions and methods of performing safe endotracheal intubation. The trainers for this purpose were identified, and training programs for doctors, nurses, and other HCPs were started. Doctors and nurses also were advised to attend various webinars organized by the professional bodies and the health department. The trainers were from the departments of anesthesiology; microbiology; and otolaryngology. Mannequins, audiovisual aids, and video clips were used for training purposes. Later, individual departments took on the responsibility of imparting training to staff within their respective departments.
Other Challenges
Other challenges included creating facilities to meet the logistical requirements, which included signage and partitioning; arranging in-house accommodations for staff; encouraging and motivating staff to keep up morale; and arranging for the transport of patients to and from COVID-19 hospitals, among others.
Conclusion
The COVID-19 pandemic has posed many challenges. In essence, it is a fight against a common enemy with an unknown transmission pattern with no treatment or vaccine available. Healthcare facilities are not geared to manage a large influx of patients who necessitate ICU care and at the same time pose a risk of infecting HCPs. Many decisions depend on new scientific information that evolves each day. Good team working and communication are essential for planning and implementing the decisions made to fulfill the healthcare needs of patients. Despite all the efforts, the number of beds and the facilities may not prove sufficient if a large influx of patients is received. It also is necessary to review the decisions repeatedly and make necessary amendments as per new requirements or circumstances. So far, the progress of the disease in Delhi has been relatively slow compared with that in other nations.11 The authors hope that the strict measures taken and implemented by the government by way of social (physical) distancing and the complete lockdown will have positive results and the preparations will not actually be put to the test; however, if they are, it is expected that they will fulfill the requirements. The authors acknowledge and agree that the model proposed in this article is but one method of approaching such a difficulty and there could be other, perhaps better, methods of dealing with the problem. In addition, local circumstances and existing facilities will vary from place to place and must be taken into account before such plans are prepared elsewhere.
Acknowledgments
The authors acknowledge the support provided by the political leaders, administrators, doctors, and other staff members in formulating the plan to be executed by the concerned hospital authorities. Special thanks to the honorable Chief Minister, Shri Arvind Kejriwal; honorable Health Minister, Shri Satyendra Jain; and the Health Secretary, Padmini Singla, who posed a variety of questions to the committee chairman, Dr Sarin, that made us think, discuss, deliberate, and search for answers related to this little-known disease that helped in appropriate planning to face this challenging situation. The authors also thank Dr Sarin for his valuable inputs.
Conflict of Interest
DKT is on the Editorial Board of JCVA.
References
- 1.Li Q, Guan X, Wu P. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Worldometer. COVID-19 coronavirus pandemic. Available at: https://www.worldometers.info/coronavirus. Accessed April 12, 2020.
- 3.CNBC. India confirms its first coronavirus case. Available at: https://www.cnbc.com/2020/01/30/india-confirms-first-case-of-the-coronavirus.html. Accessed April 12, 2020.
- 4.The Weather Channel. India news. Kerala defeats coronavirus; India's 3 COVID-19 patients successfully recover. Available at: https://weather.com/en-IN/india/news/news/2020-02-14-kerala-defeats-coronavirus-indias-three-covid-19-patients-successfully. Accessed April 12, 2020.
- 5.Government of India. COVID-19 statewide status. Available at: https://www.mygov.in/covid-19. Accessed April 12, 2020.
- 6.Guan W, Ni Z, Hu Y. Clinical characteristics of coronavirus disease 2019 in China. New Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Government of India Ministry of Health and Family Welfare. Guidance document on appropriate management of suspect/confirmed cases of COVID-19. Available at: https://www.mohfw.gov.in/pdf/FinalGuidanceonMangaementofCovidcasesversion2.pdf. Accessed April 12, 2020.
- 8.Liew MF, Siow WT, MacLaren G. Preparing for COVID-19: Early experience from an intensive care unit in Singapore. Crit Care. 2020;24:83. doi: 10.1186/s13054-020-2814-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Government of India Ministry of Health and Family Welfare. Novel coronavirus disease 2019 (COVID-19): Guidelines on rational use of personal protective equipment. Available at: https://www.mohfw.gov.in/pdf/GuidelinesonrationaluseofPersonalProtectiveEquipment.pdf. Accessed April 12, 2020.
- 10.livemint. Covid-19: India ramps up manufacture of personal protection kits, devices. Available at: https://www.livemint.com/news/india/covid-19-india-ramps-up-domestic-manufacturing-of-ppes-masks-ventilators-11585580452636.html. Accessed April 12, 2020.
- 11.The Economic Times. Covid-19 cases: Decline in progression of 5 days. Available at: https://economictimes.indiatimes.com/news/politics-and-nation/covid-19-cases-decline-in-progression-after-five-days/articleshow/74959332.cms. Accessed April 12, 2020.