Highlights
-
•
Covid-19 lesions manifested as bilateral and subpleural lung opacities (reticular and alveolar).
-
•
Lung abnormalities typically involved less than 50 % of lung parenchyma.
-
•
Chest X ray sensitivity was higher after 5 days of symptoms.
Abbreviations: CRP, C-Reactive Protein; CT, Computed Tomography; MERS, Middle East Respiratory Syndrome; PACS, Picture archiving and communication system; PLT, Platelets; SARS, Severe Acute Respiratory Syndrome; SARS-CoV-2, Severe Acute Respiratory Syndrome Corona-Virus 2; RT-PCR, Reverse Transcriptase-Polymerase Chain Reaction; WBC, White Blood Cell
Keywords: Infections, Coronavirus, Radiography, Tomography, X-ray computed
Abstract
Purpose
To evaluate the diagnostic accuracy and the imaging features of routine admission chest X-ray in patients suspected for novel Coronavirus 2019 (SARS-CoV-2) infection.
Method
We retrospectively evaluated clinical and X-ray features in all patients referred to the emergency department for suspected SARS-CoV-2 infection between March 1st and March 13th. A single radiologist with more than 15 years of experience in chest-imaging evaluated the presence and extent of alveolar opacities, reticulations, and/or pleural effusion. The percentage of lung involvement (range <25 % to 75–100 %) was also calculated. We stratified patients in groups according to the time interval between symptoms onset and X-ray imaging (≤ 5 and > 5 days) and according to age (≤ 50 and > 50 years old).
Results
A total of 518 patients were enrolled. Overall 314 patients had negative and 204 had positive RT-PCR results. Lung lesions in patients with SARS-Cov2 pneumonia primarily manifested as alveolar and interstitial opacities and were mainly bilateral (60.8 %). Lung abnormalities were more frequent and more severe by symptom duration and by increasing age. The sensitivity and specificity of chest X-ray at admission in the overall cohort were 57 % (95 % CI = 47–67) and 89 % (83–94), respectively. Sensitivity was higher for patients with symptom onset > 5 days compared to ≤ 5 days (76 % [62–87] vs 37 % [24–52]) and in patients > 50 years old compared to ≤ 50 years (59 % [48–69] vs 47 % [23–72]), at the expense of a slightly lower specificity (68 % [45–86] and 82 % [73–89], respectively).
Conclusions
Overall chest X-ray sensitivity for SARS-CoV-2 pneumonia was 57 %. Sensitivity was higher when symptoms had started more than 5 days before, at the expense of lesser specificity, while slightly higher in older patients in comparison to younger ones.
1. Introduction
Since February 21st, 2020, several cases of pneumonia due to a novel coronavirus, named SARS-CoV-2 by the World Health Organization (WHO) [1], have been found in Lombardy, an Italian region. As of March 14th, 2020, there are more than 21,000 confirmed cases and more than 1400 deaths in Italy. The SARS-CoV-2 is considered a relative of the deadly Severe Acute Respiratory Syndrome (SARS) and the Middle East respiratory syndrome (MERS) coronaviruses [[2], [3], [4]].
Recent studies revealed that SARS-CoV-2 could spread from human to human, mainly through respiratory droplets, and also through contact [5]. The incubation period is generally 3–7 days, the longest not more than 14 days. Fever, fatigue, and dry cough are the main symptoms [6]. In severe cases, dyspnea occurs more than a week later and ARDS, septic shock, difficult to correct metabolic acidosis, and coagulation dysfunction rapidly develop [7]. SARS-CoV-2 founded cases are frequently diagnosed in emergency settings. The disease mainly occurs in elderly and fragile patients, especially with one or more comorbidities, who often leads to life-threatening conditions with a mortality rate estimated in Italy of about 4%. Countries all over the world adopted molecular assay to find out the presence of the virus in humans, according to WHO guidelines [8]. All major decisions regarding SARS-CoV-2 management, including diagnostic and treatment issues, rely on the initial assessment.
Because suspected SARS-CoV-2 patients often are seen in the emergency department, developing strategies that improve early management is essential. The parenchymal lung disease involvement, required to make the diagnosis of pneumonia, is based on the evidence or absence of parenchymal infiltrates.
Early radiologic investigations consistently reported that the typical computed tomography (CT) findings of SARS-CoV-2 pneumonia were bilateral ground-glass opacities (GGOs) and consolidation with a peripheral and posterior lung distribution [9].
Usually, the routine chest X-rays is the most widely available radiological procedure during hospital admissions, in particular, to complete differential diagnosis of respiratory symptoms, such as cough and dyspnea. A chest radiograph can establish the presence of pneumonia, define its extension and location, and can also diagnose complications like pleural effusion or abscess formation, while the CT may detect abnormalities that are not detectable with chest radiograph, due to its higher sensitivity.
To the best of our knowledge, there are no studies on X-ray imaging of SARS-CoV-2 pneumonia. This study aims to explore the impact of systematic early review of chest X-ray radiograph in patients admitted to the emergency department suspected for SARS-CoV-2, measuring the probability of making the diagnosis of SARS-CoV-2, as estimated by the attending emergency radiologist.
2. Materials and methods
Local Ethical Committee's review of the protocol deemed that formal approval was not required owing to the retrospective, observational, and anonymous nature of this study.
2.1. Patient population
All patients admitted to the emergency department (Hospital San Gerardo, Lombardy, Italy) a tertiary referral hospital Center, with cough, dyspnea, and fever, during the period March 1st to March 13th were enrolled in the study. Patients with a clinical suspicion of SARS-CoV-2 infection, based on referring physician’s judgment, underwent the RT-PCR test. Patients without clinical suspicion of SARS-CoV-2 infection were managed as appropriate.
Patients were eligible for study inclusion if they 1) underwent RT-PCR test for SARS-CoV-2, 2) had at least one bedside chest X-ray. For each patient, the following demographic, clinical and imaging data were recorder: 1) age, 2) sex, 3) fever, 4) cough, 5) dyspnea, 6) white blood cell count (WBC), 7) neutrophil count, 8) lymphocyte count, 9) platelets (PLT); 10) C-reactive protein (CRP) value, and 11) onset of symptoms.
2.2. Imaging technique and analysis
A standard chest X-ray was performed in anteroposterior projection only, obtained in patients at the bedside. A senior attending radiologist (with 15 years of experience in chest imaging) reviewed the chest radiographs in picture archiving and communication systems (PACS, Enterprise Imaging, AGFA Healthcare, Belgium).
X-ray images were assessed for the presence and distribution of parenchymal abnormalities including 1) alveolar opacities, defined as a hazy increase in lung attenuation with no obscuration of the underlying vessels, 2) reticular opacities, defined as fine or coarse linear shadows and, 3) pleural effusion.
The locations of the lesions were specified as superior, middle, and inferior, dividing each lung into three portions. Moreover, the lesions were defined as isolated, when focal lesions involved only one segment, multiple when multiple segments are involved, unilateral or bilateral.
Finally, for each chest X-ray we evaluated the extent of pathological findings according to the percentage of lung involvement: <25 %, from 25 % to 50 %, from 50 % to 75 %, and >75 %.
Chest X-ray was considered positive for SARS-CoV-2 infection if reticulations or alveolar opacities or both of them were found.
2.3. Statistical analysis
Patients were classified according to SARS-CoV-2 positive or negative infection based on the result of the RT-PCR test. Continuous variables are expressed as mean and SD, after assessing for normal distribution using Kolmogorov-Smirnov test, and compared using Student's t-test. Categorical variables are expressed as number and percentage. Patients positive for SARS-CoV-2 infection were also classified according to the time interval between symptoms onset and chest X-ray (≤ 5 days and > 5 days) and according to age (≤ 50 years old and > 50 years old). Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and total accuracy of chest X-ray were estimated. For each parameter 95 % confidence intervals (95 % CI) were computed. A p-value < 0.05 was considered statistically significant. All the statistical analyses were performed using SPSS statistical package (SPSS 21.0 Incorporated, Chicago, Illinois, USA).
3. Results
3.1. Demographic, clinical and laboratory data of the entire cohort
A total of 518 patients were enrolled. The majority of patients were male (290; 56.0 %) with a mean age of 59 years (±18.4). The most common symptom was fever (450; 86.9 %), followed by cough (290; 56.0 %) and dyspnea (208; 40.1 %). Only 18 patients had gastrointestinal symptoms. Overall 314 patients were negative and 204 positive for SARS-CoV-2 infection. The comparison of demographic, clinical, and laboratory data showed a higher mean age in patients with confirmed SARS-CoV-2 infection who had a significantly lower value of white blood cells, neutrophils, lymphocytes, and platelets counts and higher PCR value (Table 1 ). More often they had fever and dyspnea (Table 1). Patients with symptoms onset more than 5 days from X-ray more frequently had dyspnea with lower WBC count, monocytes, and higher PCR value (Table 2 ). Older patients (> 50 years old) mainly presented fever and dyspnea and had lower lymphocytes and PLT values and higher CRP (Table 2).
Table 1.
Clinical and demographic data of patients admitted to the Emergency Department suspect for SARS-CoV-2 infection. Fever and cough are the most common symptoms; a statistical difference was found with fever and dyspnea. WBC, PLT count, and CRP are statistically associated with nCoV-2019 infection. WBC, neutrophils, lymphocytes, monocytes, PLT are expressed as n° x 103/mm3. CRP is expressed in mg/l.
| All (n = 518) | SARS-CoV-2 neg (n = 314) | SARS-CoV-2 pos (n = 204) | p-value | |
|---|---|---|---|---|
| Age (yo ± SD) | 59 ± 18.4 | 57.2 ± 20.6 | 62.6 ± 14.1 | 0.025 |
| Sex: male (n; %) | 290 (56.0) | 164 (52.2) | 126 (61.8) | 0.159 |
| Symptoms (n; %) | ||||
| Fever | 450 (86.9) | 256 (81.5) | 184 (90.2) | 0.003 |
| Cough | 290 (56.0) | 172 (54.8) | 118 (57.8) | 0.213 |
| Dyspnea | 208 (40.1) | 106 (33.7) | 102 (50.0) | 0.048 |
| GI symptoms | 18 (3.5) | 11 (3.5) | 7 (3.4) | 0.479 |
| Labs | ||||
| WBC (x 103/mm3) | 8.1 ± 4.8 | 9.4 ± 5.4 | 6.1 ± 2.6 | <0.0001 |
| Neutrophils (x 103/mm3) | 7.1 ± 9.6 | 8.9 ± 9.8 | 5.5 ± 9.3 | 0.046 |
| Lymphocytes (x 103/mm3) | 1.9 ± 4.0 | 2.4 ± 5.0 | 1.1 ± 1.0 | 0.013 |
| Monocytes (x 103/mm3) | 0.7 ± 0.4 | 0.7 ± 0.3 | 0.4 ± 0.4 | 0.051 |
| PLT (x 103/mm3) | 218.9 ± 87.1 | 236.4 ± 90.5 | 189.8 ± 71.4 | <0.0001 |
| CRP (mg/l) | 5.8 ± 7.2 | 4.9 ± 6.8 | 7.3 ± 7.9 | 0.009 |
P-values in bold denote statistical significance.
Table 2.
Association between demographic and laboratory data according to symptoms onset and age. According to symptom ones, statistical differences were found for dyspnea, WBC, monocytes, and CRP. According to patients’ age (≤ 50 and > 50 years old), statistical differences were found for fever, dyspnea, and PLT count.
| All (n = 518) | Symptoms onset ≤ 5 days (n = 372) | Symptoms onset > 5 days (n = 146) | p-value | Age > 50 (n = 362) | Age ≤ 50 (n = 156) | p-value | |
|---|---|---|---|---|---|---|---|
| Age (yo ± SD) | 59.0 ± 18.5 | 58.2 ± 19.9 | 61.1 ± 14.3 | 0.226 | 68.7 ± 11.3 | 36.1 ± 10.2 | <0.0001 |
| Sex: male (n;%) | 290 (56.0) | 197 (52.9) | 93 (63.7) | 0.098 | 108 (59.7) | 37 (47.4) | 0.077 |
| Symptoms (n;%) | |||||||
| Fever | 450 (86.9) | 320 (86.0) | 130 (89.0) | 0.372 | 204 (56.3) | 146 (93.6) | 0.003 |
| Cough | 291 (56.0) | 201 (54.0) | 90 (61.6) | 0.167 | 188 (51.9) | 92 (59.0) | 0.088 |
| Dyspnea | 208 (40.1) | 130 (34.9) | 78 (53.4) | 0.005 | 172 (47.5) | 36 (23.1) | <0.0001 |
| GI | 18 (3.5) | 10 (2.7) | 8 (5.5) | 0.234 | 12 (3.3) | 6 (3.8) | 0.552 |
| Lab | |||||||
| WBC (x 103/mm3) | 8.1 ± 4.8 | 8.7 ± 5.2 | 6.7 ± 3.0 | 0.002 | 8.0 ± 5.0 | 8.4 ± 4.1 | 0.595 |
| Neutrophils (x 103/mm3) | 7.1 ± 9.6 | 7.3 ± 8.5 | 6.7 ± 11.8 | 0.687 | 7.1 ± 9.8 | 7.2 ± 9.2 | 0.962 |
| Lymphocytes(x 103/mm3) | 1.9 ± 4.0 | 1.9 ± 3.8 | 1.9 ± 4.3 | 0.988 | 1.6 ± 3.3 | 2.8 ± 5.2 | 0.029 |
| Monocytes (x 103/mm3) | 0.7 ± 0.4 | 0.8 ± 0.3 | 0.4 ± 0.3 | 0.004 | 0.6 ± 0.4 | 0.7 ± 0.4 | 0.499 |
| PLT (x 103/mm3) | 218.9 ± 87.1 | 222.9 ± 87.4 | 208.8 ± 86.0 | 0.243 | 202.4 ± 83.6 | 258.4 ± 82.8 | <0.0001 |
| CRP (mg/l) | 5.8 ± 7.2 | 5.2 ± 6.9 | 7.3 ± 7.9 | 0.039 | 6.8 ± 7.5 | 3.5 ± 6.1 | <0.0001 |
P-values in bold denote statistical significance.
3.2. X-ray features
All bedside chest X-ray showed good diagnostic quality, without significant artifacts.
In patients positive for SARS-CoV-2 infection, in comparison with non-infected patients, lung lesions primarily manifested as reticular [154 (75.5) vs 116 (36.9), p < 0.0001] (Fig. 1 ), and alveolar opacities [134 (65.7) vs 104 (33.1), p < 0.0001]. Imaging findings were mainly bilateral, peripheral ad involved more than one lung portion (Table 3 , Fig. 2 ). Pleural effusion was less frequent in comparison to SARS-CoV-2 non-infected patients [33 (16.2) vs 79 (25.1); p = 0.042].
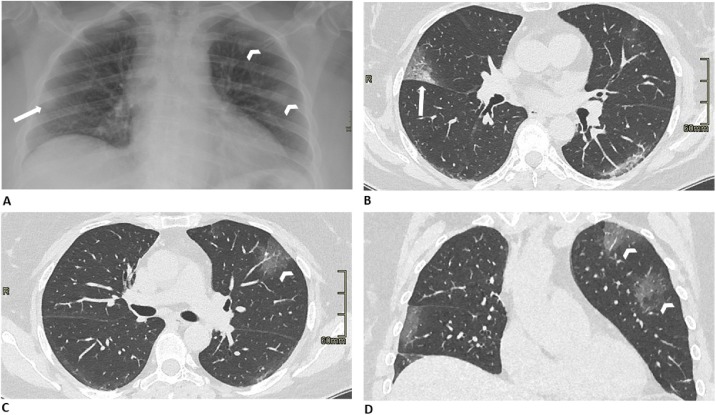
Fig. 1.
Representative chest radiographic (A) and CT images (B, C, and D) of SARS-CoV-2 pneumonia manifesting as confluent pure alveolar or ground-glass opacities. A. Anteroposterior chest radiograph shows tiny and hazy alveolar opacities in the right middle left upper and middle lung, located in peripheral zones (arrow and arrowheads). B, C, and D. Axial and coronal chest CT images show focal pure ground-glass opacities involving both lungs, in the left upper lobe (arrowheads), and the posterior segment of the right upper lobe (arrow). No pleural effusion or consolidative lesions are evident.
Table 3.
Type and distribution of the lesions according to positivity or negativity to SARS-CoV-2 infection. The interstitial pattern is the more frequent imaging finding in SARS-CoV-2 patients. The distribution is typically bilateral, subpleural, and diffuse. No statistically significant difference was found between SARS-CoV-2 positive and negative patients.
| All (n = 518) | SARS-CoV-2 neg (n = 314) | SARS-CoV-2 pos (n = 204) | p-value | |
|---|---|---|---|---|
| Reticulations (n; %) | 270 (52.1) | 116 (36.9) | 154 (75.5) | <0.0001 |
| Alveolar opacities (n; %) | 238 (45.9) | 104 (33.1) | 134 (65.7) | <0.0001 |
| Pleural effusion (n; %) | 112 (21.6) | 79 (25.1) | 33 (16.2) | 0.042 |
| Distribution (n; %) | ||||
| Bilateral | 208 (40.1) | 84 (26.7) | 124 (60.8) | <0.0001 |
| Subpleural | 160 (30.9) | 39 (12.a) | 121 (59.3) | <0.0001 |
| >1 lung portion | 198 (38.2) | 67 (21.3) | 131 (64.2) | <0.0001 |
P-values in bold denote statistical significance.
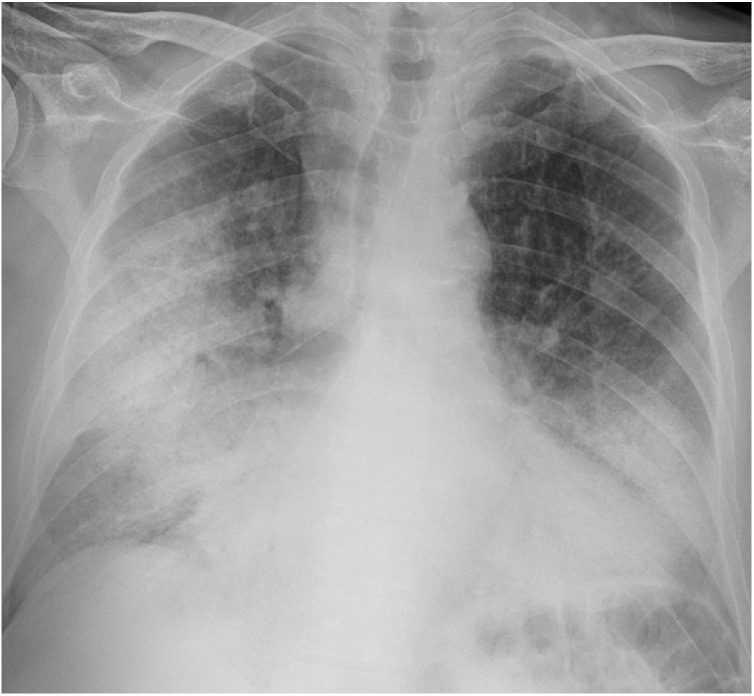
Fig. 2.
Representative chest radiograph of SARS-CoV-2 pneumonia in a 67-year-old man, manifesting as an interstitial pattern or alveolar opacities. The anteroposterior chest radiograph shows multiple bilateral and symmetric linear reticular and diffuse alveolar opacities involving all the parts of both lungs (lung involvement 50-75 %), mainly in peripheral zones.
SARS-CoV-2 patients with symptoms lasting more than 5 days showed a higher number of reticular and alveolar opacities compared to patients with symptoms onset less than 5 days [90 (88.2) vs 64 (62.7) and 88 (86.3) vs 46 (45.1) p = 0.005 and p < 0.0001 respectively] (Table 4 ). Similarly, alveolar and reticular opacities were more frequently detected in older patients [120 (70.6) vs 14 (41.2) and 148 (81.2) vs 16 (47.6)] in comparison to younger (p = 0.009 and p = 0.005, respectively) (Table 4).
Table 4.
Type and distribution of the lesions in patients SARS-CoV-2 positive according to symptoms onset and age. Reticulations and alveolar opacities are statistically associated with infection. Pleural effusion is not associated with SARS-CoV-2 positivity. Pleural effusion is typical only in patients over the age of 50. Radiological findings are typically bilateral, subpleural, and involving more than one lung portion.
| All (n = 204) | Symptoms > 5 days (n = 102) | Symptoms ≤ 5 days (n = 102) | p-value | Age >50 (n = 170) | Age ≤ 50 (n = 34) | p-value | |
|---|---|---|---|---|---|---|---|
| Reticulations (n; %) | 154 (75.5) | 90 (88.2) | 64 (62.7) | 0.005 | 148 (81.2) | 16 (47.0) | 0.005 |
| Alveolar opacities (n; %) | 134 (65.7) | 88 (86.3) | 46 (45.1) | <0.0001 | 120 (70.6) | 14 (41.2) | 0.009 |
| Pleural effusion (n; %) | 32 (15.7) | 14 (13.7) | 18 (17.6) | 0.786 | 32 (18.8) | 0 | 0.041 |
| Distribution (n; %) | |||||||
| Bilateral | 124 (60.8) | 80 (78.4) | 44 (43.1) | <0.0001 | 110 (64.7) | 14 (41.2) | 0.035 |
| Subpleural | 122 (59.8) | 84 (82.3) | 38 (37.2) | <0.0001 | 108 (63.5) | 14 (41.2) | 0.043 |
| >1 lung portion | 132 (64.7) | 84 (82.3) | 48 (47.0) | <0.0001 | 116 (68.2) | 16 (47.0) | 0.046 |
P-values in bold denote statistical significance.
Considering the entire study population, the extent of lung abnormalities was ≤ 25 % in 92 (45.5 %) patients, 25 %–50 % in 84 (41.6 %) and 50 %–75 % in 26 (12.9 %) (Fig. 3, Fig. 4, Fig. 5 ). None of the patients has an extension greater than 75 % of lung parenchyma.
Fig. 3.
Representative chest radiographs of SARS-CoV-2 pneumonia in a 71-year-old man manifesting as diffuse alveolar opacities. The anteroposterior chest radiograph reveals an extensive alveolar involvement in the peripheral zone of both lungs, more evident in the middle and inferior part or right lung, and the inferior part of the left lung (lung involvement 50-75 %). Pleural effusion can be appreciated on the left side.
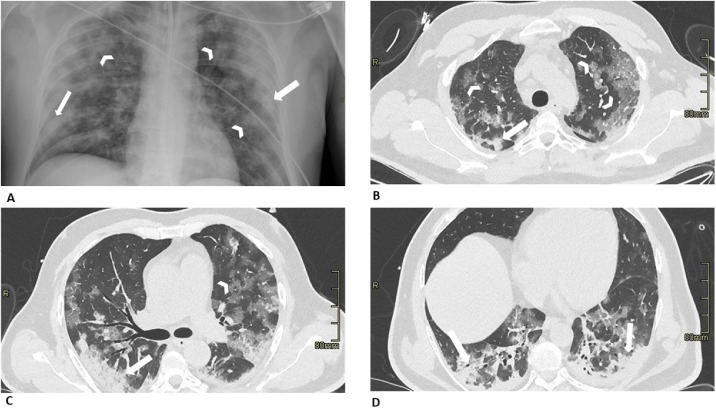
Fig. 4.
Representative chest radiographic (A) and CT images (B, C, and D) of SARS-CoV-2 pneumonia manifesting as confluent mixed alveolar or ground-glass opacities and consolidation. A. Anteroposterior chest radiograph shows multifocal alveolar opacities (arrowheads) and patchy peripheral consolidations in both lungs (arrows) B, C and D. Axial chest CT images show mixed ground-glass opacities (arrowheads) and consolidative lesions (arrows) bilaterally in peripheral zones. The confluent lesions are mainly distributed in peripheral areas and some of them contain air-bronchograms.
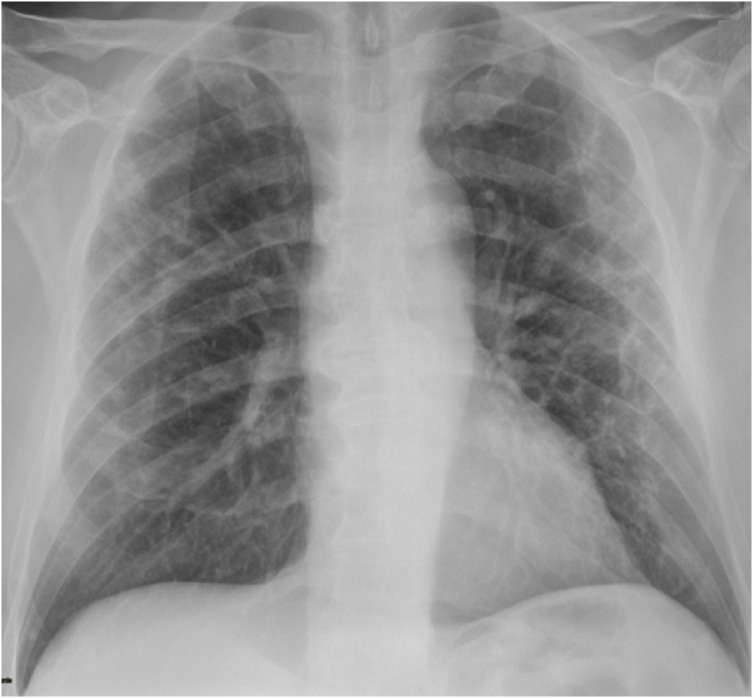
Fig. 5.
Representative chest radiograph of SARS-CoV-2 pneumonia in a 61-year-old man, manifesting mainly as reticular opacities. The anteroposterior chest radiograph shows a few focal linear reticular opacities in the middle part of both lungs located in the central and peripheral areas.
Interestingly patients with an interval ≤ 5 days between symptoms onset and ED admission more frequently had a lung disease extension ≤ 25 % in comparison to those with an interval > 5 days [58 (56.7 %) vs 34 (34 %), p = 0.028]. Similarly, younger patients more frequently had a lesser degree of lung involvement (≤ 25 %) in comparison to older ones [26 (76.5 %) vs 66 (39.3 %), p = 0.007].
3.3. X-ray diagnostic performance
Overall sensitivity, specificity, PPV, NPV and accuracy of chest X-ray in the diagnosis of SARS-CoV-2 related pneumonia were 57 % (95 % CI = 47–67) 89 % (95 %CI = 83–94), 77 % (95 %CI = 68–85), 76 % (95 %CI = 72–80) and 76 % (95 %CI = 71–81) respectively.
Sensitivity and PPV of chest X-ray were lower when symptoms had appeared ≤ 5 days before performing imaging technique while specificity, NPV and accuracy were higher [37 % (95 % CI = 24–52), 93 (95 % CI = 87–96), 65 % (95 % CI = 62–87), 80 % (95 % CI = 76–83) and 77 % (95 % CI = 71–83)]. On the contrary sensitivity and PPV in detecting SARS-CoV-2 pneumonia were higher when symptom had appeared more than 5 days before the X-ray [76 % (95 % CI = 47–67) and 85 % (95 % CI = 75–91)], while specificity, NPV and accuracy were lower [68 % (95 % CI = 45–86), 56 % (95 % CI = 41–69) and 74 (95 % CI = 62–83)].
In patients ≤ 50 years chest X-ray had a lower sensitivity [47 % (95 % CI = 23–72)], and an excellent specificity, PPV, NPV and accuracy [100 % ((95 % CI = 94–100), 100 % (95 % CI = 90–100), 87 % (95 % CI = 81–91) and 88 % (95 % CI = 79–94)]. Sensitivity of chest X-ray was slightly higher in older patients [59 % (95 % CI = 48–69)], at the expense of lesser specificity, PPV, NPV and accuracy [82 % (95 % CI = 73–89), 75 % (95 % CI = 65–82), 70 % (95 % CI = 64–75) and 71 % (95 % CI = 64–78)].
4. Discussion
Our study showed that all SARS-CoV-2 patients have a similar X-ray lung appearance, characterized by reticular and alveolar opacities with bilateral and peripheral lung involvement, whereas there is no typical pattern in those patients affected by common seasonal pneumonia: this may allow us to discriminate the origin of each pneumonia we are in front of. The majority of pulmonary lesions involved both lungs and multiple lung lobes, predominantly the middle ad inferior portions, and mainly distributed peripherally, in the sub-pleural area.
The imaging manifestations of the new SARS-CoV-2 related pneumonia are similar to common viral pneumonia but have also its imaging characteristics, such as the presence of diffuse interstitial opacities and alveolar opacities as we have observed in our sample, in line with other published studies [[9], [10], [11]].
By analyzing international literature the proportion of patients with abnormal initial radiographic findings was 78.3–82.4 % in SARS [3], 83.6 % in MERS [4], while only in 33 % of cases in Korean SARS-CoV-2 related pneumonia [10], and in 60 % of Chinese patients [8]. In our series, investigating Italian patients, the percentage of infected people increased up to 80 %, considering our Country one of the most affected all over the World.
In this study, patients were stratified into two groups: the first group with an interval of less or equal to 5 days between symptom onset and chest X-ray examination, and the second group with an interval greater than 5 days between symptom onset and the chest radiograph. When patients' conditions get worst or in case of a longer course of the disease, the lungs showed diffuse lesions, and the density of both lungs increased widely, demonstrating multiple diffuse alveolar and reticular opacities. In fact, we found out that chest X-ray sensitivity decreased when symptoms appeared ≤ 5 days before performing imaging technique with a value of only 37 %, a specificity of 65 % and overall diagnostic accuracy of 77 %, while in case of a longer course of the disease the sensitivity increased up to 76 % maintaining a good specificity (68 %) with an overall suitable diagnostic accuracy (74 %).
Moreover the subdivision of SARS-CoV-2 patients according to age (≤ and > 50 years) allows to establish that alveolar opacities with coarse linear shadows are more frequent in older patients in comparison to younger ones. On the other hand the diagnostic performance changes: in younger patients chest X-ray showed an excellent specificity (100 %) and accuracy (88 %), but a low sensitivity (47 %), instead sensitivity slightly increased in older patients till about 60 %, while specificity and accuracy barely decreased (82 % and 71 %, respectively), maybe due to the presence of others lung comorbidities.
In recent literature, few studies focused on chest X-ray, mainly evaluating the role of CT as a routine imaging modality for screening or diagnosis [[11], [12], [13]]. The Radiology Scientific Expert Panel suggests that, after CT imaging, the room downtime is typically between 30 min to 1 h for room decontamination [14], suggesting that chest X-ray may be considered to minimize the risk of cross-infection.
Following the aforementioned statement, we assumed that chest X-ray can achieve the potential role of a screening test in medical settings with high disease prevalence, according to its sensitivity. In fact, in the emergency setting, the bedside chest X-ray is a key component of the diagnostic work-up and should be considered as a useful diagnostic tool also to minimize the risk of cross-infection, because the surface of portable unit can be easily cleaned. In these patients, the use of CT means a huge burden for the radiology departments and a big challenge for continuous infection control.
The results in our series support the idea that the conventional radiographs can be considered an important diagnostic resource in patients suspected for SARS-CoV-2, thus being a useful diagnostic approach, especially in Countries where the access to CT is lacking
Our study had some limitations. First of all, most of our patients did not undergo a CT scan examination of the lung, therefore some early radiological lung features may not be demonstrated. It is well known that patients without infiltration observed on radiograph and with unsure diagnosis greatly benefited from CT scan, however, we weighed this consideration against the importance of urgent reporting. Furthermore, chest radiograph results not only induced diagnosis probability changes but also led to the immediate adjustment of patients’ care. Finally, a single radiologist evaluated all images, and consequently, it was not possible to evaluate the agreement.
Implications derived from our results are that the use of chest radiograph may help in determining both diagnosis and treatment, and deciding the best management in patients with suspected SARS-CoV-2-related pneumonia in the emergency setting. Therefore, we believe that a strategy that promotes chest radiograph as imaging technique in targeted patients in the ED would decrease time to diagnosis and may even, sooner, reduce global radiation dose exposure by limiting particular CT examinations.
In conclusion, our observation is that the X-ray manifestations of SARS-CoV-2 infection are quite typical, with an acceptable overall sensitivity of 57 % for SARS-CoV-2-related pneumonia. Sensitivity can be even higher when symptoms had started more than 5 days before, at the expense of lesser specificity, and slightly higher in older patients in comparison to younger ones.
CRediT authorship contribution statement
Davide Ippolito: Conceptualization, Writing - original draft, Writing - review & editing, Supervision, Project administration. Anna Pecorelli: Formal analysis, Writing - original draft, Writing - review & editing, Project administration. Cesare Maino: Writing - original draft, Writing - review & editing, Project administration. Carlo Capodaglio: Investigation, Resources, Data curation. Ilaria Mariani: Software, Investigation, Resources, Data curation. Teresa Giandola: Investigation, Data curation, Project administration. Davide Gandola: Investigation, Data curation. Ilaria Bianco: Investigation. Maria Ragusi: Investigation, Data curation, Project administration. Cammillo Talei Franzesi: Methodology, Project administration. Rocco Corso: Validation. Sandro Sironi: Visualization, Supervision.
Declaration of Competing Interest
All authors declare no conflicts-of-interest related to this article.
Acknowledgments
We would like to thank all the radiographers that have dedicated their time and efforts to perform the several radiological SARS-CoV-2 examinations in the isolation wards during this time and the radiologist staff of hospitals to support that work.
References
- 1.https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200221-sitrep-32-covid-19.pdf?sfvrsn=4802d089_2.
- 2.de Wit E., van Doremalen N., Falzarano D., Munster V.J. SARS, and MERS: recent insights into emerging coronaviruses. Nat. Rev. Microbiol. 2016;14:523–534. doi: 10.1038/nrmicro.2016.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wong K.T., Antonio G.E., Hui D.S., Lee N., Yuen E.H., Wu A., Leung C.B., Rainer T.H., Cameron P., Chung S.S., Sung J.J., Ahuja A.T. Severe acute respiratory syndrome: radiographic appearances and pattern of progression in 138 patients. Radiology. 2003;228(August 2):401–406. doi: 10.1148/radiol.2282030593. [DOI] [PubMed] [Google Scholar]
- 4.Das K.M., Lee E.Y., Langer R.D., Larsson S.G. Middle east respiratory syndrome coronavirus: what does a radiologist need to know? AJR Am. J. Roentgenol. 2016;206(June 6):1193–1201. doi: 10.2214/AJR.15.15363. [DOI] [PubMed] [Google Scholar]
- 5.Chan J.F., Yuan S., Kok K.H. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(February 10223):514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jin X., Lian J.-S., Hu J.-H. Epidemiological, clinical and virological characteristics of 74 cases of coronavirus-infected disease 2019 (COVID-19) with gastrointestinal symptoms. Gut. 2020;69:1002–1009. doi: 10.1136/gutjnl-2020-320926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rodriguez-Morales A.J., Cardona-Ospina J.A., Gutiérrez-Ocampo E. Clinical, laboratory and imaging features of COVID-19: a systematic review and meta-analysis. Travel Med. Infect. Dis. 2020:101623. doi: 10.1016/j.tmaid.2020.101623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/laboratory-guidance.
- 9.Pan Y., Guan H., Zhou S., Wang Y., Li Q., Zhu T., Hu Q., Xia L. Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (SARS-CoV-2): a study of 63 patients in Wuhan, China. Eur. Radiol. 2020;(February 13) doi: 10.1007/s00330-020-06731-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yoon S.H., Lee K.H., Kim J.Y., Lee Y.K., Ko H., Kim K.H., Park C.M., Korean Kim Y.H. Chest radiographic and CT findings of the 2019 novel coronavirus disease (COVID-19): analysis of nine patients treated in Korea. J. Radiol. 2020;(February 26) doi: 10.3348/kjr.2020.0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xu Xi. «Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2». Eur. J. Nucl. Med. Mol. Imaging. 2020;47(5):1275–1280. doi: 10.1007/s00259-020-04735-9. May. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shi Heshui. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect. Dis. 2020;20(4):425–434. doi: 10.1016/S1473-3099(20)30086-4. April. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ng M.Y., Lee EYP Yang J., Yang F., Li X., Wang H. Imaging profile of the COVID-19 infection: radiologic findings and literature review. Radiol.: Cardiothoracic Imaging. 2020;2:e200034. doi: 10.1148/ryct.2020200034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mossa-Basha M., Meltzer C.C., Kim D.C. Radiology department preparedness for COVID-19: radiology scientific expert panel. Radiology. 2020 doi: 10.1148/radiol.2020200988. [DOI] [PMC free article] [PubMed] [Google Scholar]