Highlights
-
•
We used microsimulation model to project the impact of coronavirus disease-2019 on childhood obesity.
-
•
Physical education cancelation and stay-at-home order cause physical activity decline and weight gain.
-
•
U.S. childhood obesity rate may increase by 2.4% if school closures continue to December 2020.
-
•
Impact of coronavirus disease-2019 may be modestly larger in boys, non-Hispanic blacks, and Hispanics.
-
•
Health interventions are urgently called to promote physical activity under coronavirus disease-2019.
Keywords: Childhood obesity, Coronavirus, COVID-19, Microsimulation, Physical activity
Abstract
Purpose
The coronavirus disease-2019 (COVID-19) pandemic in the United States led to nationwide stay-at-home orders and school closures. Declines in energy expenditure resulting from canceled physical education classes and reduced physical activity may elevate childhood obesity risk. This study estimated the impact of COVID-19 on childhood obesity.
Methods
A microsimulation model simulated the trajectory of a nationally representative kindergarten cohort's body mass index z-scores and childhood obesity prevalence from April 2020 to March 2021 under the control scenario without COVID-19 and under the 4 alternative scenarios with COVID-19—Scenario 1: 2-month nationwide school closure in April and May 2020; Scenario 2: Scenario 1 followed by a 10% reduction in daily physical activity in the summer from June to August; Scenario 3: Scenario 2 followed by 2-month school closure in September and October; and Scenario 4: Scenario 3 followed by an additional 2-month school closure in November and December.
Results
Relative to the control scenario without COVID-19, Scenarios 1, 2, 3, and 4 were associated with an increase in the mean body mass index z-scores by 0.056 (95% confidence interval (95%CI): 0.055–0.056), 0.084 (95%CI: 0.084–0.085), 0.141 (95%CI: 0.140–0.142), and 0.198 (95%CI: 0.197–0.199), respectively, and an increase in childhood obesity prevalence by 0.640 (95%CI: 0.515–0.765), 0.972 (95%CI: 0.819–1.126), 1.676 (95%CI: 1.475–1.877), and 2.373 (95%CI: 2.135–2.612) percentage points, respectively. Compared to girls and non-Hispanic whites and Asians, the impact of COVID-19 on childhood obesity was modestly larger among boys and non-Hispanic blacks and Hispanics, respectively.
Conclusion
Public health interventions are urgently called to promote an active lifestyle and engagement in physical activity among children to mitigate the adverse impact of COVID-19 on unhealthy weight gains and childhood obesity.
Graphical abstract
1. Introduction
The coronavirus disease-2019 (COVID-19) pandemic has been reported in more than 200 countries, claiming massive illnesses, hospitalizations, and death tolls.1,2 Following the declaration of a national emergency in the United States in response to COVID-19,3 42 states and Washington, DC, issued stay-at-home orders from March 19 to April 7.4 These orders covered approximately 95% of the U.S. population.4 Closely related to the stay-at-home orders are various non-pharmaceutical interventions that aim to promote social distancing.5,6 One of the most widely adopted policy interventions across the states is school closures.7,8 The U.S. Centers for Disease Control and Prevention recommended school closures in response to community transmission of COVID-19.9 All 50 states and Washington, DC, have issued executive orders on school closures, and most states issued these orders during March 13–23.7,8 To date, no state has lifted school closure orders, and it is likely for the school closures in most places to continue for the rest of the 2019–2020 academic year.10,11 It remains unclear whether and on what scale schools will reopen after the summer break, as such decisions by states are primarily contingent upon how the COVID-19 pandemic evolves in the coming months.12,13
The COVID-19 pandemic may expose children to an increased risk of childhood obesity.14,15 Childhood obesity is associated with various immediate and long-term illnesses such as sleep apnea, hypertension, type 2 diabetes, heart disease, stroke, osteoarthritis, and certain types of cancer.16,17 In the United States, childhood obesity prevalence has increased by 3-fold over the past few decades.18,19 In 2017–2018, approximately 18.5% of children aged 2–19 years (13.7 million) had obesity.20 Non-Hispanic blacks and Hispanics have higher childhood obesity prevalence than non-Hispanic whites and Asians.20 Physical inactivity among children is one of the major behavioral risk factors for childhood obesity.21 The Physical Activity Guidelines for Americans (2nd edition) recommends 60 min or more of moderate-to-vigorous physical activity (MVPA) daily among children.22 However, more than 3-quarters (76%) of children in the United States do not meet the daily PA level recommended in the guidelines,23 and nearly one-half (47%) of U.S. children exceed 2 h per day in sedentary behavior.24 Physical education (PE) is a mandated part of the school curricula in most states.25 PE contributes to children's daily accumulation of PA and is of particular importance for those who have obesity or lack access to PA opportunities in their home environment.26 Because schools have been closed nationwide, children in the United States have missed their opportunity to participate in PE classes and other school-based PA (e.g., recess, after-school sports programs).27 They are also less likely to make up for it under the stay-at-home orders, as parks and outdoor recreation areas across the states are closed, thus limiting PA opportunities outside.27,28 In sum, the COVID-19 pandemic has reinforced the obesogenic environment conducive to physical inactivity and sedentary behavior.29 Children living under such conditions are likely to be exposed to an elevated risk for energy imbalance and unhealthy weight gain.29,30
Given the looming influence of COVID-19 on PA and the deep uncertainties about how the pandemic may evolve in the future,29,30 it is critical to assess the impact of COVID-19 on childhood obesity and project its trajectory in response to the pandemic. Such information will be valuable to policymakers at federal, state, and local levels, as well as to various stakeholders (e.g., schools, communities, and families), in designing and implementing countermeasures to minimize the detrimental impact of COVID-19 on PA and prevent children from obesity onset. This study aimed to build a microsimulation model to project the impact of COVID-19 on childhood obesity in the United States.
2. Methods
2.1. Study sample
The study sample of the microsimulation model was retrieved from the Early Childhood Longitudinal Study, Kindergarten Class of 2010–2011 (ECLS-K:2011). The ECLS-K:2011 is a longitudinal study sponsored by the U.S. Department of Education.31 The same children (n = 15,631) were followed from kindergarten through 5th grade.31 Most children were 5–6 years old when they first entered the study. Information was collected in the fall and spring of kindergarten (2010–2011), fall and spring of 1st grade (2011–2012), fall and spring of 2nd grade (2012–2013), spring of 3rd grade (2014), spring of 4th grade (2015), and spring of 5th grade (2016).31 The children in the ECLS-K:2011 comprise a nationally representative sample drawn from both public and private schools, with participants attending both full-day and part-day kindergarten in 2010–2011.31 A total of 15,631 children with diverse socioeconomic and racial/ethnic backgrounds participated in the ECLS-K:2011 and were followed up in 9 waves from kindergarten through 5th grade.31
2.2. Overview of microsimulation model
A microsimulation model was built to project the impact of COVID-19 on body mass index z-scores (BMIz) and childhood obesity in the United States. In particular, the model used data from the ECLS-K:2011 kindergarten cohort (the data were first collected in 2010–2011) to simulate changes in BMIz and obesity prevalence from April 2020 to March 2021. The study sample's trajectory of BMIz and childhood obesity prevalence was compared between the control scenario without the COVID-19 pandemic and 4 alternative scenarios with COVID-19. Scenario 1 assumed a 2-month nationwide school closure due to COVID-19 in April and May 2020. Scenario 2 assumed that Scenario 1 would be followed by a 10% reduction in daily PA in the summer from June to August. Scenario 3 assumed that Scenario 2 would be followed by a 2-month school closure in September and October. Scenario 4 assumed that Scenario 3 would be followed by an additional 2-month school closure in November and December 2020. For each of the 4 alternative scenarios, a full resumption of routine life and social operations immediately following the event, and until the end of the study period, i.e., March 2021, was assumed. Under the 4 alternative scenarios, the COVID-19 pandemic is expected to positively impact kindergarteners’ body weight (and consequently BMIz and childhood obesity prevalence) through reduced energy expenditure (EE) resulting from canceled PE classes during the academic months and decreased PA during the summer break.
Five technical details regarding model specifications are noted. First, the model runs by an increment of a month, but a 2-month time interval during the spring and fall academic terms was adopted to simplify the reporting and illustration of modeling results. Second, states and school districts follow different academic calendars, so that the exact start and end dates for academic terms and the summer break differ. However, such geographical and school information was unavailable in the ECLS-K:2011; thus, we were unable to model child-specific school schedules. Nevertheless, it should have little influence on the model estimates because the comparisons in BMIz and childhood obesity prevalence between the control and 4 alternative scenarios were made in March 2021, 3 months after the end of the assumed impact of COVID-19. Therefore, as long as the overall impact duration of COVID-19 remains the same for all children, the variations in academic calendars across schools should not impact the estimated differences in the accumulated impact of COVID-19 on BMIz and childhood obesity prevalence. Third, a 10% reduction in PA during the summer break was assumed based on a study of adult Fitbit users in the United States (i.e., a 12% reduction in PA due to COVID-19).32 In the sensitivity analyses, an 8% and 12% reduction in PA during the summer break were used to assess their respective influence on model estimates. Fourth, the model assumed that all children would take PE classes if offered. However, in reality, some children may be absent from PE due to health or other reasons. In such a case, the forgone PE classes would serve as a proxy for other missed PA opportunities due to school closures (e.g., recess, before-, and after-school sports programs). Finally, the ECLS-K:2011 followed study participants for 6 years from their kindergarten entrance in 2010–2011 to 5th grade in 2016. It would not be appropriate to extrapolate their BMIz and childhood obesity to 2020–2021. Instead, the microsimulation model assumed that the ECLS-K:2011 study sample all started school in September 2019 (i.e., kindergarteners in 2019 would share the same height and weight distribution as those in 2011), interpolated their height and weight using restricted cubic spline regressions until March 2020, and then simulated changes in BMIz and childhood obesity prevalence from April 2020 to March 2021 under the control and 4 alternative scenarios. Based on the U.S. Centers for Disease Control and Prevention reports, the childhood obesity rate among children aged 6–11 years increased only modestly from 17.7% in 2011–2012 to 18.4% in 2017–2018.20,33 Since the microsimulation model aimed to project the change in BMIz and childhood obesity rate rather than their baseline level, the discrepancy resulting from a modest difference in childhood obesity rate between 2010–2011 (i.e., the baseline of the ECLS-K:2011) and 2019–2020 (i.e., the baseline of the microsimulation model) is unlikely to cause significant estimation bias.
2.3. Anthropometric measurement
In the ECLS-K:2011, children's height and weight were measured during each wave of data collection.34 A Shorr board (i.e., a tall wooden stand with a ruled edge used for measuring height) and a digital scale were used to obtain the measurements.34 Trained assessors recorded children's height (in inches to the nearest 1-quarter inch) and weight (in pounds to the nearest one-half pound) on a standardized recording form and then entered the measurements into a laptop computer.34 Children were asked to remove their shoes before measurement.34 Each measurement was taken and recorded twice to ensure reliability.34
During the 6-year study period of the ECLS-K:2011, children's height and weight were measured in 9 waves—once per academic semester from kindergarten to 2nd grade and once per academic year from 3rd to 5th grade.31,34 Restricted cubic spline regressions were performed to interpolate each child's height and weight by month. Using the interpolated height and weight together with children's recorded sex and age (in months), BMIz were calculated using the 2000 U.S. Centers for Disease Control and Prevention age- and sex-specific growth chart.35 Childhood obesity is defined as BMIz in the 95th percentile or higher in the growth chart.36
2.4. EE
In comparison to the control scenario without the COVID-19 pandemic, the reduction in EE in the 4 alternative scenarios with COVID-19 is assumed to result from 2 independent sources—canceled PE classes during the academic months and decreased PA during the summer break (June–August). More specifically, the model assumes that no PE classes would be offered if schools were closed during a regular academic term (e.g., April and May in the spring of 2020, and September–December in the fall). Two recent review studies of national data provided estimates on the weekly instruction time of PE classes among U.S. kindergarteners.37,38 A weekly PE instruction time of 131.81 min was used in the microsimulation model, which averaged the 2 estimates of 110.10 min by Kahan and McKenzie37 and 153.52 min by Bednar and Rouse.38 Following Kahan and McKenzie,37 Eq. 1 was used to calculate EE (kcal/month) resulting from PE class participation:
| (Eq. 1) |
In Eq. 1, MVPA and light PA are assumed to occupy 50.3% and 49.7%, respectively, of the weekly PE instruction time and have a metabolic equivalent (MET) of task of 4.5 and 1.8 kcal/kg/h, respectively.37
Besides PE classes, kindergarteners typically engage in additional PA during recess and before- or after-school programs. Therefore, counting reduced EE exclusively from canceled PE classes during school closure is likely to provide a conservative estimate regarding the impact of COVID-19 on EE among kindergarteners.
Due to nationwide stay-at-home restrictions and closures of exercise facilities (e.g., YMCA, gyms, and recreation centers),29,30 kindergarteners’ PA is likely to be adversely affected during the 2020 summer break. On average, elementary school children in the United States participate in 88 min of PA per day.23 Although no published work to date has estimated the influence of COVID-19 on PA among U.S. children, data collected from U.S. adult Fitbit users revealed a reduction in daily PA by about 12%.32 The microsimulation model thus assumes a 10%, or 8.8-min, reduction in daily PA among U.S. kindergarteners, equally divided between MVPA (4.5 METs) and light PA (1.8 MET) time. Eq. 2 was used to calculate EE (kcal/month) resulting from reduced PA during the summer break:37
| (Eq. 2) |
2.5. Modeling COVID-19 impact on BMIz and childhood obesity
Following Hennessy et al.,39 the microsimulation model assumes that an energy surplus or deficit translates into weight change at a rate of 3492.66 kcal per pound. All agents (i.e., 15,631 kindergarteners in the ECLS-K:2011) start their academic year in September 2019, with their height and weight updated by the end of each month. Monthly BMIz and childhood obesity status are also calculated accordingly. From April 2020 to March 2021, the mean BMIz scores and childhood obesity prevalence among agents are compared between the control scenario without the COVID-19 pandemic and the 4 alternative scenarios with COVID-19.
2.6. Modeling COVID-19 impact by population subgroup
The microsimulation model estimated the impact of COVID-19 on BMIz and childhood obesity prevalence among all agents and by sex (i.e., boys and girls) and race/ethnicity (i.e., non-Hispanic whites, non-Hispanic blacks, non-Hispanic Asians, non-Hispanic other race, and Hispanics).
2.7. Model assumptions
The microsimulation model is based on 2 primary assumptions. First, children's reduction in PA during the academic months is assumed to be entirely attributable to the cancelation of PE classes. In reality, schools provide many other PA opportunities besides PE classes, such as recess, walk or bike to school programs, and after-school sports programs. In such cases, the microsimulation model would provide a conservative estimate for the impact of COVID-19 on PA reduction and childhood obesity. Admittedly, children may make up for their lost PA opportunities at school by engaging in additional PA at home. However, given the widespread community transmission of COVID-19 and nationwide stay-at-home orders, it is unlikely for the majority of children to adequately compensate for their reduced PA due to school closures.29,30 Second, children's energy imbalance (i.e., surplus) is influenced by reduced PA only. In reality, many other factors related to the COVID-19 pandemic may impact children's EE, such as a change in diet (e.g., school meals vs. family meals), sleeping, and stress or anxiety level.40,41
2.8. Sensitivity analyses
Two sets of sensitivity analyses were conducted to assess changes in the estimated impact of COVID-19 on BMIz and childhood obesity in response to changes in model assumptions. First, the reduction in PA resulting from PE class cancellations was allowed to vary from 90% to 110% of its mean. Second, the reduction in PA during the summer break was allowed to vary from 8% to 12% of the total daily PA duration (i.e., 88 min). The microsimulation model was re-estimated for each specific case accordingly.
2.9. Simulation setting
The microsimulation model was built in R (Version 3.6.3; R Development Core Team, Vienna, Austria). Each model was simulated 1000 times using bootstrapped samples of the same size as the original ECLS-K:2011 (n = 15,631), based on which the mean, standard error, and 95% confidence interval (CI) of the impacts of COVID-19 under different scenarios were estimated. The ECLS-K:2011 sampling weights were incorporated in the effect estimation to facilitate modeling result generalization to the national kindergarten population.34
3. Results
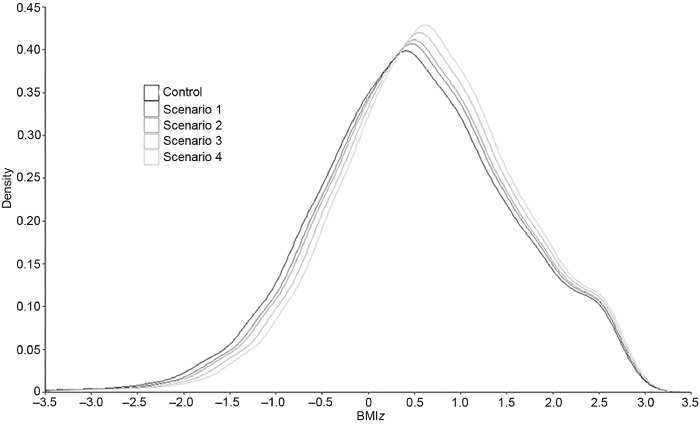
Fig. 1 shows the simulated kernel density distributions of BMIz in March 2021 under the control and 4 alternative scenarios. In comparison to the BMIz distribution under the control scenario without COVID-19, model estimates under the 4 alternative scenarios gradually shifted to the right with higher peaks, reflecting a monotonic growth in the mean BMIz when the duration of COVID-19 increased (i.e., from April–May to November–December 2020).
Fig. 1.
Simulated kernel density distributions of body mass index z-scores (BMIz) in March 2021 under the control and 4 alternative scenarios. A microsimulation model was built to simulate the trajectory of a U.S. nationally representative kindergarten cohort's BMIz from April 2020 to March 2021 under the control scenario without coronavirus disease-2019 (COVID-19) and under the 4 alternative scenarios with COVID-19—Scenario 1: a 2-month nationwide school closure in April and May 2020; Scenario 2: Scenario 1 followed by a 10% reduction in daily physical activity (PA) in the summer from June to August; Scenario 3: Scenario 2 followed by a 2-month school closure in September and October; and Scenario 4: Scenario 3 followed by an additional 2-month school closure in November and December.
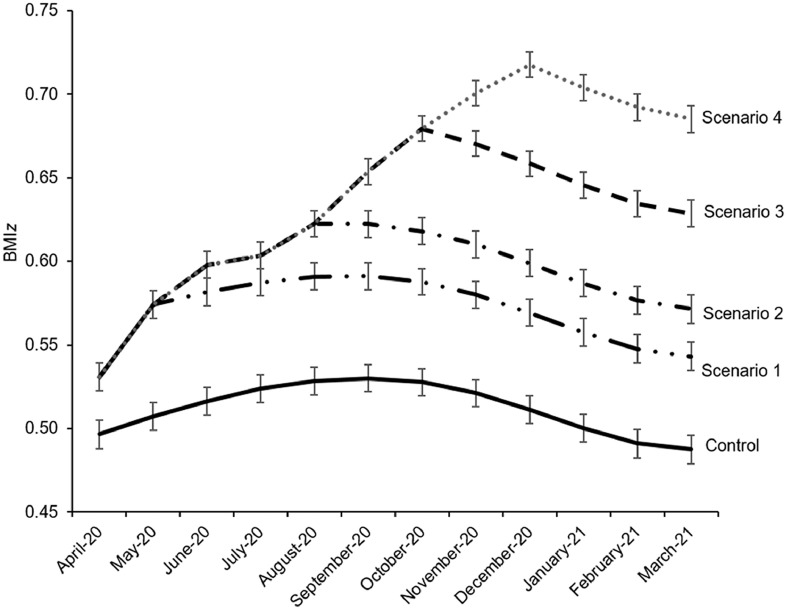
Fig. 2 shows the simulated change in BMIz from April 2020 to March 2021 under the control and 4 alternative scenarios. In the absence of the COVID-19 pandemic, the mean BMIz among U.S. kindergarteners gradually increased from 0.497 (95%CI: 0.480–0.513) in April 2020 to 0.530 (95%CI: 0.514–0.546) in September 2020 and subsequently declined to 0.487 (95%CI: 0.470–0.504) in March 2021. In contrast, under Scenarios 1, 2, 3, and 4 with COVID-19, the mean BMIz started at 0.531 (95%CI: 0.515–0.547) in April 2020, further increased to a value of 0.591 (95%CI: 0.576–0.607) in September, 0.623 (95%CI: 0.607–0.638) in August, 0.679 (95%CI: 0.664–0.695) in October, and 0.718 (95%CI: 0.703–0.733) in December, and subsequently declined to 0.543 (95%CI: 0.526–0.560), 0.572 (95%CI: 0.555–0.588), 0.629 (95%CI: 0.612–0.645), and 0.685 (95%CI: 0.669–0.701) in March 2021, respectively.
Fig. 2.
Simulated trend in body mass index z-scores (BMIz) from April 2020 to March 2021 under the control and 4 alternative scenarios. A microsimulation model was built to simulate the trajectory of a U.S. nationally representative kindergarten cohort's BMIz from April 2020 to March 2021 under the control scenario without coronavirus disease-2019 (COVID-19) and under the 4 alternative scenarios with COVID-19—Scenario 1: a 2-month nationwide school closure in April and May 2020; Scenario 2: Scenario 1 followed by a 10% reduction in daily physical activity (PA) in the summer from June to August; Scenario 3: Scenario 2 followed by a 2-month school closure in September and October; and Scenario 4: Scenario 3 followed by an additional 2-month school closure in November and December. The error bars denote the estimated standard errors.
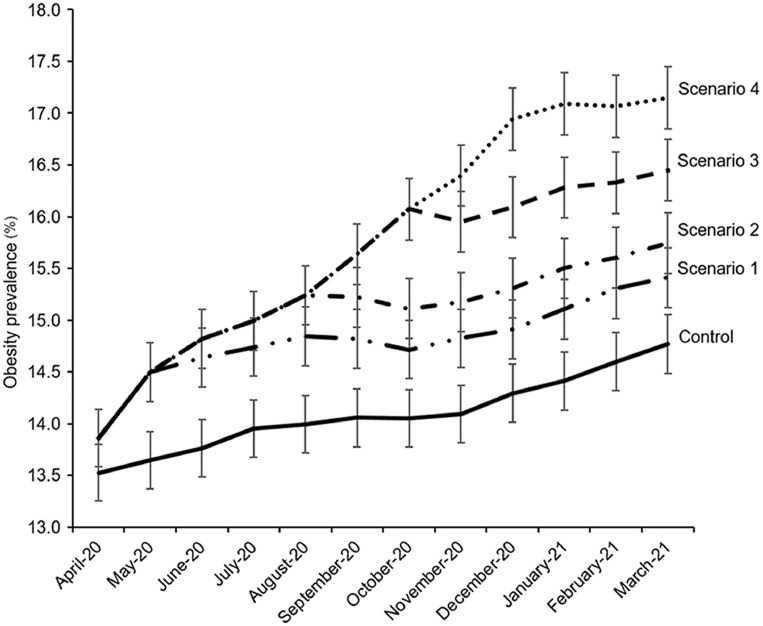
Fig. 3 shows the simulated change in childhood obesity prevalence from April 2020 to March 2021 under the control and 4 alternative scenarios. In the absence of COVID-19, obesity prevalence among U.S. kindergarteners gradually increased from 13.52% (95%CI: 12.99%–14.06%) in April 2020 to 14.77% (95%CI: 14.22%–15.33%) in March 2021. In contrast, under Scenario 1, 2, 3, and 4 with COVID-19, despite some modest periodical fluctuations, childhood obesity prevalence in large observed a steady increase from 13.86% (95%CI: 13.32%–14.41%) in April 2020 to 15.41% (95%CI: 14.85%–15.98%), 15.74% (95%CI: 15.17%–16.32%), 16.45% (95%CI: 15.87%–17.03%), and 17.15% (95%CI: 16.55%–17.74%) in March 2021, respectively.
Fig. 3.
Simulated trend in childhood obesity prevalence from April 2020 to March 2021 under the control and 4 alternative scenarios. A microsimulation model was built to simulate the trajectory of a U.S. nationally representative kindergarten cohort's childhood obesity prevalence from April 2020 to March 2021 under the control scenario without coronavirus disease-2019 (COVID-19) and under the 4 alternative scenarios with COVID-19—Scenario 1: a 2-month nationwide school closure in April and May 2020; Scenario 2: Scenario 1 followed by a 10% reduction in daily physical activity (PA) in the summer from June to August; Scenario 3: Scenario 2 followed by a 2-month school closure in September and October; and Scenario 4: Scenario 3 followed by an additional 2-month school closure in November and December. Childhood obesity is defined as body mass index (BMI) z-scores at the 95th percentile or higher in the 2000 U.S. Centers for Disease Control and Prevention age- and sex-specific growth chart. The error bars denote the estimated standard errors.
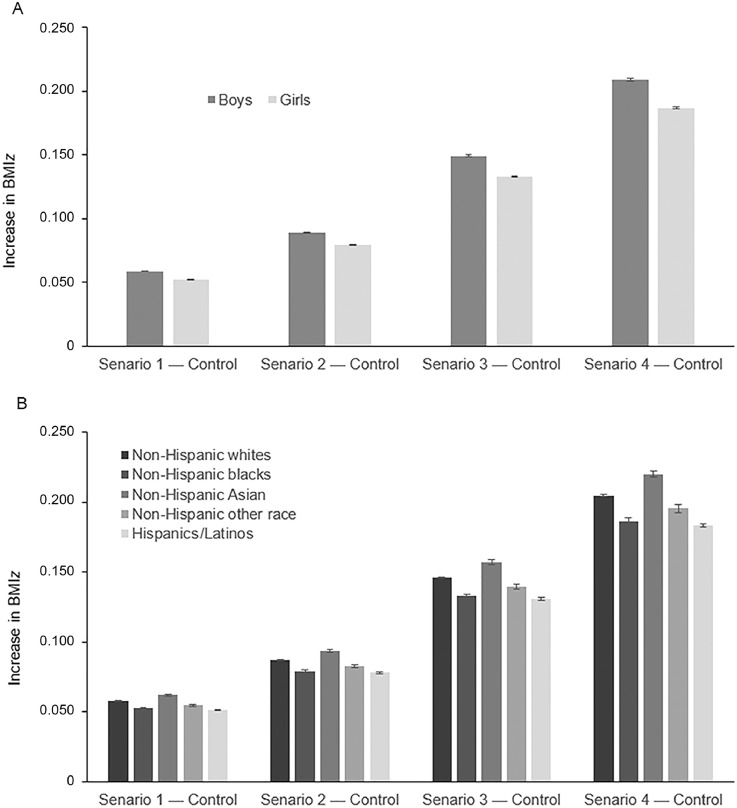
Fig. 4A and Fig. 4B report the simulated increase in BMIz between the control scenario and the 4 alternative scenarios in March 2021 by sex and race/ethnicity. Compared to the control scenario without COVID-19, Scenarios 1, 2, 3, and 4 were associated with an increase in the mean BMIz among all kindergarteners by 0.056 (95%CI: 0.055–0.056), 0.084 (95%CI: 0.084–0.085), 0.141 (95%CI: 0.140–0.142), and 0.198 (95%CI: 0.197–0.199), respectively. The estimated impact of COVID-19 on BMIz was modestly larger among boys than among girls. Compared to the control scenario without COVID-19, Scenarios 1, 2, 3, and 4 were associated with an increase in the mean BMIz by 0.059 (95%CI: 0.058–0.059), 0.089 (95%CI: 0.088–0.090), 0.149 (95%CI: 0.148–0.150), and 0.209 (95%CI: 0.207–0.211) among boys, and 0.052 (95%CI: 0.052–0.053), 0.079 (95%CI: 0.078–0.080), 0.133 (95%CI: 0.132–0.134), and 0.187 (95%CI: 0.185–0.188) among girls, respectively (p < 0.05). The estimated impact of COVID-19 on BMIz was largest among non-Hispanic Asians, followed by non-Hispanic whites, non-Hispanic other race, non-Hispanic blacks, and Hispanics/Latinos. The increase in mean BMIz among non-Hispanic Asians, non-Hispanic whites, non-Hispanic other race, non-Hispanic blacks, and Hispanics/Latinos was 0.062 (95%CI: 0.061–0.064), 0.058 (95%CI: 0.057–0.058), 0.055 (95%CI: 0.053–0.056), 0.052 (95%CI: 0.051–0.052), and 0.052 (95%CI: 0.051–0.052) under Scenario 1; 0.094 (95%CI: 0.092–0.096), 0.087 (95%CI: 0.086–0.088), 0.083 (95%CI: 0.081–0.085), 0.079 (95%CI: 0.078–0.081), and 0.078 (95%CI: 0.077–0.079) under Scenario 2; 0.157 (95%CI: 0.154–0.161), 0.146 (95%CI: 0.145–0.147), 0.139 (95%CI: 0.136–0.143), 0.133 (95%CI: 0.130–0.136), and 0.131 (95%CI: 0.129–0.133) under Scenario 3; and 0.220 (95%CI: 0.215–0.225), 0.205 (95%CI: 0.203–0.207), 0.196 (95%CI: 0.190–0.201), 0.187 (95%CI: 0.183–0.190), and 0.183 (95%CI: 0.181–0.186) under Scenario 4, respectively (p < 0.05).
Fig. 4.
Simulated increase in body mass index z-scores (BMIz) between the control and 4 alternative scenarios in March 2021 by (A) sex and (B) race/ethnicity. A microsimulation model was built to simulate the trajectory of a U.S. nationally representative kindergarten cohort's BMIz from April 2020 to March 2021 under the control scenario without coronavirus disease-2019 (COVID-19) and under the four alternative scenarios with COVID-19—Scenario 1: a 2-month nationwide school closure in April and May 2020; Scenario 2: Scenario 1 followed by a 10% reduction in daily physical activity (PA) in the summer from June to August; Scenario 3: Scenario 2 followed by a 2-month school closure in September and October; and Scenario 4: Scenario 3 followed by an additional 2-month school closure in November and December. The error bars denote the estimated standard errors.
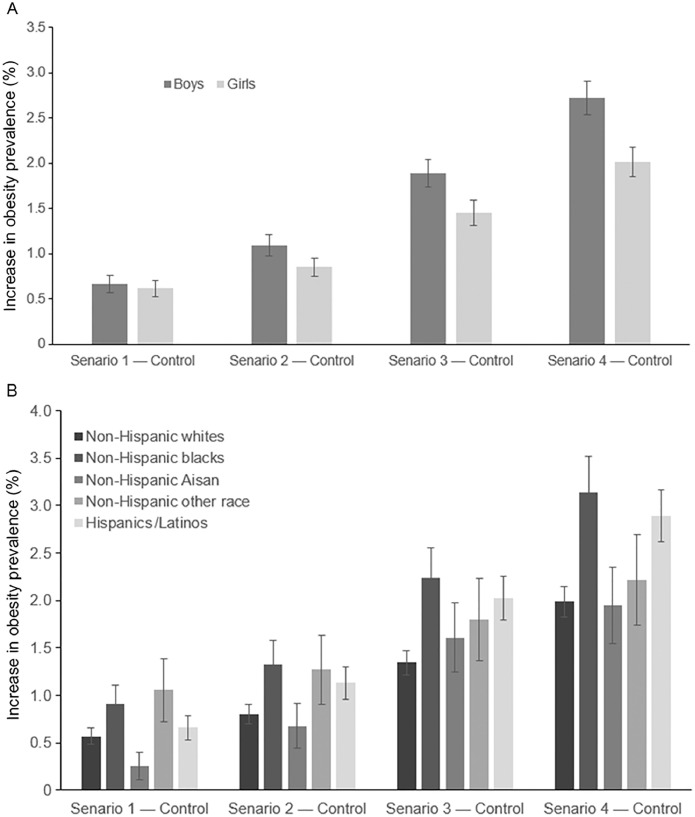
Fig. 5A and Fig. 5B report the simulated difference in childhood obesity prevalence between the control scenario and the 4 alternative scenarios in March 2021 by sex and race/ethnicity. Compared to the control scenario without COVID-19, Scenarios 1, 2, 3, and 4 were associated with an increase in childhood obesity prevalence among all kindergarteners by 0.640 (95%CI: 0.515–0.765), 0.972 (95%CI: 0.819–1.126), 1.676 (95%CI: 1.475–1.877), and 2.373 (95%CI: 2.135–2.612) percentage points, respectively. The estimated impact of COVID-19 on childhood obesity prevalence was modestly larger among boys than among girls. Compared to the control without the COVID-19 pandemic, Scenarios 1, 2, 3, and 4 were associated with an increase in childhood obesity prevalence of 0.664 (95%CI: 0.486–0.842), 1.090 (95%CI: 0.862–1.318), 1.892 (95%CI: 1.593–2.191), and 2.719 (95%CI: 2.362–3.075) percentage points among boys, and 0.614 (95%CI: 0.439–0.790), 0.850 (95%CI: 0.644–1.056), 1.451 (95%CI: 1.183–1.719), and 2.013 (95%CI: 1.699–2.328) percentage points among girls, respectively (p > 0.05 for Scenarios 1 and 2; and p < 0.05 for Scenarios 3 and 4). In general, the estimated impact of COVID-19 on childhood obesity prevalence tended to be larger among non-Hispanic blacks and Hispanics, whereas it was smaller among non-Hispanic whites and Asians. Compared to the control scenario without COVID-19, Scenarios 1, 2, 3, and 4 were associated with an increase in childhood obesity prevalence of 0.903 (95%CI: 0.499–1.307), 1.331 (95%CI: 0.841–1.821), 2.234 (95%CI: 1.602–2.865), and 3.137 (95%CI: 2.392–3.882) percentage points among non-Hispanic blacks; 0.657 (95%CI: 0.400–0.914), 1.131 (95%CI: 0.795–1.467), 2.025 (95%CI: 1.577–2.472), and 2.892 (95%CI: 2.360–3.425) percentage points among Hispanics/Latinos; 0.566 (95%CI: 0.397–0.735), 0.803 (95%CI: 0.602–1.004), 1.343 (95%CI: 1.084–1.602), and 1.988 (95%CI: 1.674–2.302) percentage points among non-Hispanic whites; and 0.254 (95%CI: –0.033 to 0.541), 0.677 (95%CI: 0.209–1.145), 1.609 (95%CI: 0.891–2.327), and 1.948 (95%CI: 1.159–2.736) percentage points among non-Hispanic Asians, respectively.
Fig. 5.
Simulated increase in childhood obesity prevalence between the control and 4 alternative scenarios in March 2021 by (A) sex and (B) race/ethnicity. A microsimulation model was built to simulate the trajectory of a U.S. nationally representative kindergarten cohort's childhood obesity prevalence from April 2020 to March 2021 under the control scenario without coronavirus disease-2019 (COVID-19) and under the 4 alternative scenarios with COVID-19—Scenario 1: a 2-month nationwide school closure in April and May 2020; Scenario 2: Scenario 1 followed by a 10% reduction in daily physical activity (PA) in the summer from June to August; Scenario 3: Scenario 2 followed by a 2-month school closure in September and October; and Scenario 4: Scenario 3 followed by an additional 2-month school closure in November and December. Childhood obesity is defined as body mass index (BMI) z-scores at the 95th percentile or higher in the 2000 U.S. Centers for Disease Control and Prevention age- and sex-specific growth chart. The error bars denote the estimated standard errors.
In the sensitivity analyses, when the reduction in PA resulting from PE class cancellations varied from 90% to 110% of its mean, Scenarios 1, 2, 3, and 4 were associated with an increase in childhood obesity prevalence among all kindergarteners from 0.557 (95%CI: 0.440–0.673) to 0.697 (95%CI: 0.567–0.828), 0.928 (95%CI: 0.777–1.078) to 1.024 (95%CI: 0.866–1.181), 1.541 (95%CI: 1.349–1.735) to 1.798 (95%CI: 1.589–2.006), and 2.226 (95%CI: 1.995–2.458) to 2.617 (95%CI: 2.366–2.867) percentage points in comparison to the control scenario without COVID-19, respectively. When the reduction in PA during the summer break varied from 8% to 12% of the total daily PA duration, Scenarios 2, 3, and 4 were associated with an increase in childhood obesity prevalence among all kindergarteners from 0.928 (95%CI: 0.777–1.078) to 1.024 (95%CI: 0.866–1.181), 1.606 (95%CI: 1.409–1.803) to 1.740 (95%CI: 1.535–1.945), and 2.316 (95%CI: 2.080–2.552) to 2.431 (95%CI: 2.190–2.673) percentage points in comparison to the control scenario without COVID-19, respectively. Scenario 1 incurred no change because no reduction in PA was assumed during the summer break.
4. Discussion
Relative to the control scenario without COVID-19, Scenarios 1, 2, 3, and 4 were associated with an increase in the mean BMIz by 0.056, 0.084, 0.141, and 0.198 units, respectively, and an increase in childhood obesity prevalence by 0.640, 0.972, 1.676, and 2.373 percentage points, respectively. Compared to girls and non-Hispanic whites and Asians, the impact of COVID-19 on childhood obesity was modestly larger among boys and non-Hispanic blacks and Hispanics, respectively.
To date, the vast majority of research on COVID-19 has focused on disease pathology and clinical or pharmaceutical interventions.1,2,42 In contrast, the social impact of the pandemic and resulting mitigation policies are much less studied.43 The social effects of COVID-19, if unaddressed by timely, effective, targeted countermeasures, may lead to profound, long-term health and economic consequences on a scale much larger than the disease infection.43 Childhood obesity has been a leading public health concern in the United States, and its prevalence is at a record high.16,17 The model predicts that even a 2-month school closure alone could result in an increase in the childhood obesity rate by 0.640 percentage points among U.S. kindergarteners. If school closures continue to the end of 2020 due to unsubdued community transmission of COVID-19, the childhood obesity rate in the United States might further increase by 2.373%. If such an impact is universal among all U.S. children aged 5–17 years, by March 2021 approximately 1.27 million new childhood obesity cases will develop under the COVID-19 pandemic than otherwise.
The estimated sex difference in the impact of COVID-19 on childhood obesity is mainly attributable to the differential EE reduction between boys and girls. EE is a positive function of body weight.36 Because boys, in general, are heavier than girls,44 the same decrease in PA duration will result in a more substantial energy surplus among boys than among girls.
The primary contributing factor to the estimated racial/ethnic differences in the impact of COVID-19 on childhood obesity pertains to their differential baseline BMIz distribution. Compared to non-Hispanic whites (0.404) and Asians (0.218), the mean BMIz in April 2020 is significantly higher among non-Hispanic blacks (0.569) and Hispanics (0.726). Therefore, the same reduction in PA duration across races/ethnicities is more likely to induce childhood obesity among non-Hispanic blacks and Hispanics. Customized policy interventions are warranted to prevent further deterioration of weight-related health outcomes among these 2 socioeconomically disadvantaged racial/ethnic minority groups.
For the coming months or longer, the majority of children in the United States may not fully resume their daily PA routines due to the nationwide closure of schools, gyms, recreation centers, and parks and cancellations of sports activities.12, 13, 14, 15 Policy countermeasures that aim to mitigate the adverse impact of COVID-19 need to consider innovative, robust, and highly adaptable strategies to promote PA at home or in residential settings that minimize social gathering. Some researchers have made a call to action for PA engagement as a valuable tool for controlling COVID-19 infections and maintaining quality of life.45
Answers to the following research questions may better inform relevant policy countermeasures. What PAs can be performed individually or jointly by family members that have few or no restrictions on location, facility, and equipment, and how can we promote them? How can we integrate PA into everyday stay-at-home routines to meet the daily PA level recommended in the guidelines? 22 How can we best utilize available resources at home and in close surroundings to optimize PA? How can we educate children and other family members about the importance of daily PA, ensure safety, and prevent PA-related injuries?
The contributions of this study are 3-fold. First, it serves as the first attempt to project the impact of COVID-19 on PA and childhood obesity. Second, it constructs a microsimulation model based on data from a nationally representative longitudinal survey of a kindergarten cohort first interviewed in 2010–2011, whose height and weight was repeatedly and objectively measured. Third, it provides the impact estimates specific to child population subgroups by sex and race/ethnicity, which may inform targeted interventions.
Despite these contributions, several limitations of this study should be noted. First, it is a simulation study based on observational data. Due to the lack of sample randomization, the modeling results do not infer causality. Second, the scope of this study is limited to the kindergarten years of a nationally representative study cohort so that the findings may not be fully generalizable to all children and adolescents in the United States. Third, the microsimulation model assumes that children's energy surplus under COVID-19 entirely results from PE class cancellations due to school closures during the academic months. In reality, a multitude of factors may impact children's EE and weight gain under the pandemic, including, but not limited to, elevated stress and change in diet, daily routine, and sleeping patterns.40,41 Nevertheless, given the variety of PA opportunities typically offered at school and given the nationwide stay-at-home orders,27,28 the model assumption on forgone PE classes could only produce a conservative estimate. The sensitivity analyses indicated that within a reasonable range, changes in the assumptions on PA reductions during the academic months and the summer break did not cause substantial changes in modeling results. Fourth, the model assumes that the impact of COVID-19 on PA is uniformly distributed among children, which does not capture the population heterogeneity in response to the pandemic. In reality, some children may cope with the pandemic better or worse than average and engage in more or less PA to mitigate their energy surplus due to school and facility closures. In this case, the model estimates the average response and outcome at the population level but not at the level of individual differences.
5. Conclusion
Using a microsimulation modeling approach, this study projected the change in U.S. kindergarteners’ BMIz and childhood obesity under the COVID-19-induced uncertainties. Our simulation results indicate that compared to the control scenario without COVID-19, both BMIz and childhood obesity prevalence under COVID-19 are expected to rise, and the magnitude of the increase is proportional to the length and severity of the pandemic. Public health interventions are urgently called for if we wish to promote an active lifestyle and engagement in PA among children and want to mitigate the adverse impact of COVID-19 on unhealthy weight gains and childhood obesity.
Competing interests
The author declares that he has no competing interests.
Footnotes
Peer review under responsibility of Shanghai University of Sport.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jshs.2020.05.006.
Appendix. Supplementary materials
References
- 1.Kakodkar P., Kaka N., Baig M.N. A comprehensive literature review on the clinical presentation, and management of the pandemic coronavirus disease 2019 (COVID-19) Cureus. 2020;12:e7560. doi: 10.7759/cureus.7560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Helmy Y.A., Fawzy M., Elaswad A., Sobieh A., Kenney S.P., Shehata A.A. The COVID-19 pandemic: a comprehensive review of taxonomy, genetics, epidemiology, diagnosis, treatment, and control. J Clin Med. 2020;9:E1225. doi: 10.3390/jcm9041225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.White House. Proclamation on declaring a national emergency concerning the novel coronavirus disease (COVID-19) outbreak. Available at: https://www.whitehouse.gov/presidential-actions/proclamation-declaring-national-emergency-concerning-novel-coronavirus-disease-covid-19-outbreak. [accessed 12.05.2020].
- 4.New York Times. See which states and cities have told residents to stay at home. Available at: https://www.nytimes.com/interactive/2020/us/coronavirus-stay-at-home-order.html. [accessed 12.05.2020].
- 5.Hartley D.M., Perencevich E.N. Public health interventions for COVID-19: emerging evidence and implications for an evolving public health crisis. JAMA. 2020 Apr 10 doi: 10.1001/jama.2020.5910. [DOI] [PubMed] [Google Scholar]
- 6.National Conference of State Legislatures. State action on coronavirus (COVID-19). COVID-19 related legislation. Available at:https://www.ncsl.org/research/health/state-action-on-coronavirus-covid-19.aspx. [accessed 12.05.2020].
- 7.Institute for Public Policy and Social Research, Michigan State University. State policies to address COVID-19 school closure. Available at: http://ippsr.msu.edu/state-policies-address-covid-19-school-closure. [accessed 12.05.2020].
- 8.National Conference of State Legislatures. Public education's response to the coronavirus (COVID-19) pandemic. Available at: https://www.ncsl.org/research/education/public-education-response-to-coronavirus-covid-19.aspx. [accessed 12.05.2020].
- 9.Centers for Disease Control and Prevention. Considerations for school closure. Available at: https://www.cdc.gov/coronavirus/2019-ncov/downloads/considerations-for-school-closure.pdf. [accessed 12.05.2020].
- 10.National Broadcasting Company. When will school open? Here's a state-by-state list. Available at: https://www.today.com/parents/when-will-school-open-here-s-state-state-list-t179718. [accessed 12.05.2020].
- 11.National Public Radio. Half of U.S. public school students are home for the school year. Available at: https://www.npr.org/sections/coronavirus-live-updates/2020/04/16/835941050/nearly-half-of-u-s-public-school-students-are-home-for-the-school-year. [accessed 12.05.2020].
- 12.USA Today. When will schools reopen? Not soon, education leaders say, despite Trump's declarations. Available at: https://www.usatoday.com/story/news/education/2020/04/21/coronavirus-schools-reopen-closures-fall-2020/5167726002. [accessed 12.05.2020].
- 13.Centers for Disease Control and Prevention. Guidance for cleaning and disinfecting public spaces, workplaces, businesses, schools, and homes. Available at: https://www.cdc.gov/coronavirus/2019-ncov/community/pdf/Reopening_America_Guidance.pdf. [accessed 12.05.2020].
- 14.Rundle A.G., Park Y., Herbstman J.B., Kinsey E.W., Wang Y.C. COVID-19-related school closings and risk of weight gain among children. Obesity (Silver Spring) 2020;28:1008–1009. doi: 10.1002/oby.22813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pietrobelli A., Pecoraro L., Ferruzzi A., Heo M. Effects of COVID‐19 lockdown on lifestyle behaviors in children with obesity living in Verona, Italy: a longitudinal study. Obesity (Silver Spring) 2020 doi: 10.1002/oby.22861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kumar S., Kelly A.S. Review of childhood obesity: from epidemiology, etiology, and comorbidities to clinical assessment and treatment. Mayo Clin Proc. 2017;92:251–265. doi: 10.1016/j.mayocp.2016.09.017. [DOI] [PubMed] [Google Scholar]
- 17.Hruby A., Hu F.B. The epidemiology of obesity: a big picture. Pharmacoeconomics. 2015;33:673–689. doi: 10.1007/s40273-014-0243-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ogden C.L., Carroll M.D., Lawman H.G., Fryar C.D., Kruszon-Moran D., Kit B.K. Trends in obesity prevalence among children and adolescents in the United States, 1988-1994 through 2013-2014. JAMA. 2016;315:2292–2299. doi: 10.1001/jama.2016.6361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lifshitz F. Obesity in children. J Clin Res Pediatr Endocrinol. 2008;1:53–60. doi: 10.4008/jcrpe.v1i2.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention. Childhood obesity facts. Prevalence of childhood obesity in the United States. Available at: https://www.cdc.gov/obesity/data/childhood.html. [accessed 12.05.2020].
- 21.Chi D.L., Luu M., Chu F. A scoping review of epidemiologic risk factors for pediatric obesity: implications for future childhood obesity and dental caries prevention research. J Public Health Dent. 2017;77(Suppl. 1):S8–31. doi: 10.1111/jphd.12221. [DOI] [PubMed] [Google Scholar]
- 22.U.S. Department of Health and Human Services. Physical activity guidelines for Americans, 2nd edition. Available at:https://health.gov/sites/default/files/2019-09/Physical_Activity_Guidelines_2nd_edition.pdf. [accessed 12.05.2020].
- 23.National Physical Activity Plan Alliance. The 2018 United States report card on physical activity for children and youth. Available at:http://www.physicalactivityplan.org/projects/reportcard.html. [accessed 12.05.2020].
- 24.Sisson S.B., Church T.S., Martin C.K., Tudor-Locke C., Smith S.R., Bouchard C. Profiles of sedentary behavior in children and adolescents: the US National Health and Nutrition Examination Survey, 2001–2006. Int J Pediatr Obes. 2009;4:353–359. doi: 10.3109/17477160902934777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.An R., Ji M., Clarke C., Guan C. Impact of state laws governing physical education on attendance among US high school students, 2003 to 2017. Am J Health Promot. 2019;33:1144–1151. doi: 10.1177/0890117119858016. [DOI] [PubMed] [Google Scholar]
- 26.National Association for Sport and Physical Education. Guidance document: instructional framework for fitness education in physical education. Available at:https://www.shapeamerica.org/upload/Instructional-Framework-for-Fitness-Education-in-Physical-Education.pdf. [accessed 12.05.2020].
- 27.Guan H., Okely A.D., Aguilar-Farias N., del Pozo Cruz B., Draper C.E., Hamdouchi A.E. Promoting healthy movement behaviors among children during the COVID-19 pandemic. Lancet Child Adolesc Health. 2020;4:416–418. doi: 10.1016/S2352-4642(20)30131-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fawkner S, Niven A, Hanson S, Williamson C, Hanson CL. Physical activity for children and young people aged 5–18 years during COVID-19. Stay safe; be active. Available at: https://blogs.bmj.com/bjsm/2020/04/13/physical-activity-for-children-and-young-people-aged-5-18-years-during-covid-19-stay-safe-be-active. [accessed 12.05.2020].
- 29.Pinto A, Dunstan DW, Owen N, Bonfá E, Gualano B. Combating physical inactivity during the COVID-19 pandemic. Available at: https://www.nature.com/articles/s41584-020-0427-z. [accessed 12.05.2020]. [DOI] [PMC free article] [PubMed]
- 30.American Psychological Association. How and why to get children moving now. Available at: https://www.apa.org/topics/covid-19/children-exercise-strategies. [accessed 12.05.2020].
- 31.National Center for Education Statistics. Kindergarten Class of 2010-11 (ECLS-K:2011). Available at: https://nces.ed.gov/ecls/kindergarten2011.asp. [accessed 12.05.2020].
- 32.Fitbit. The impact of coronavirus on global activity. Available at: https://blog.fitbit.com/covid-19-global-activity. [accessed 12.05.2020].
- 33.U.S. Department of Health and Human Services. Health Resources and Services Administration, Maternal and Child Health Bureau. Child Health USA. Available at: https://mchb.hrsa.gov/chusa14. [accessed 12.05.2020].
- 34.National Center for Education Statistics. Early childhood longitudinal study, kindergarten class of 2010–11 (ECLS-K:2011). Available at: https://nces.ed.gov/pubs2017/2017285.pdf. [accessed 12.05.2020].
- 35.Centers for Disease Control and Prevention. Overview of the CDC growth charts. Available at: https://www.cdc.gov/nccdphp/dnpa/growthcharts/training/modules/module2/text/module2print.pdf. [accessed 12.05.2020].
- 36.Centers for Disease Control and Prevention. Defining childhood obesity. Available at: https://www.cdc.gov/obesity/childhood/defining.html. [accessed 12.05.2020].
- 37.Kahan D., McKenzie T.L. Energy expenditure estimates during school physical education: potential vs. reality? Prev Med. 2017;95:82–88. doi: 10.1016/j.ypmed.2016.12.008. [DOI] [PubMed] [Google Scholar]
- 38.Bednar S., Rouse K. The effect of physical education on children's body weight and human capital: new evidence from the ECLS-K:2011. Health Econ. 2020;29:393–405. doi: 10.1002/hec.3990. [DOI] [PubMed] [Google Scholar]
- 39.Hennessy E., Ornstein J.T., Economos C.D., Herzog J.B., Lynskey V., Coffield E. Designing an agent-based model for childhood obesity interventions: a case study of ChildObesity180. Prev Chronic Dis. 2016;13:E04. doi: 10.5888/pcd13.150414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sasaki J.E., Howe C., John D., Hickey A., Steeves J., Conger S. Energy expenditure for 70 activities in children and adolescents. J Phys Act Health. 2016;13(Suppl. 1):S24–S28. doi: 10.1123/jpah.2015-0712. [DOI] [PubMed] [Google Scholar]
- 41.Thivel D., Aucouturier J., Doucet É., Saunders T.J., Chaput J.P. Daily energy balance in children and adolescents. Does energy expenditure predict subsequent energy intake? Appetite. 2013;60:58–64. doi: 10.1016/j.appet.2012.09.022. [DOI] [PubMed] [Google Scholar]
- 42.Sanders J.M., Monogue M.L., Jodlowski T.Z., Cutrell J.B. Pharmacologic treatments for coronavirus disease 2019 (COVID-19): a review. JAMA. 2020 doi: 10.1001/jama.2020.6019. [DOI] [PubMed] [Google Scholar]
- 43.Nicola M., Alsafi Z., Sohrabi C., Kerwan A., Al-Jabir A., Iosifidis C. The socioeconomic implications of the coronavirus and COVID-19 pandemic: a review. Int J Surg. 2020;78:185–193. doi: 10.1016/j.ijsu.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kirchengast S. Gender differences in body composition from childhood to old age: an evolutionary point of view. J Life Sci. 2010;2:1–10. [Google Scholar]
- 45.Sallis J, Pratt M. A call to action: physical activity and COVID-19. Available at: https://www.exerciseismedicine.org/support_page.php/stories/?b=896. [accessed 12.05.2020].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.