Abstract
In this study, we sought to examine associations between dimensions of trait perfectionism and posttraumatic stress disorder (PTSD) symptoms among a community sample of adults who experienced at least one traumatic event and determine whether the associations between trait perfectionism dimensions and PTSD symptomatology varied as a function of perceived control. A sample of 161 (57% women; M = 33.24 years, SD = 10.84 years) community adults who experienced at least one traumatic event in their lives completed self-report measures of trait perfectionism, perceived control, personality, and PTSD symptomatology. Results from multiple regression analyses indicated that socially prescribed perfectionism was associated with higher levels of PTSD symptomatology. However, this finding was qualified by a significant interaction with perceived control such that higher levels of socially prescribed perfectionism were associated with greater PTSD symptomatology only under conditions of low perceived control. Findings underscore the importance of individual differences in socially prescribed perfectionism and perceived control for PTSD symptomatology.
Keywords: Perceived control, Perfectionism, Personality, Trauma, Posttraumatic stress
Epidemiological research has indicated that exposure to traumatic events is relatively common with estimates ranging from 20 to 83% (Breslau et al. 1998; Kessler et al. 1995). Yet, the prevalence of posttraumatic stress disorder (PTSD) tends to be relatively low, with lifetime prevalence rates ranging from approximately 6 to 9% and 1-year prevalence rates ranging from 3 to 5% in Canada and the USA (Kessler et al. 2005; Koenen et al. 2017; Van Ameringen et al. 2008). These findings cast doubt on the notion that experiencing traumatic events is the primary etiological factor in the development of PTSD (Johnson and Thompson 2008). In light of evidence suggesting that personality traits play an important role in vulnerability to PTSD symptomatology (Jaksic et al. 2012), this study focused on the link between perfectionism and PTSD symptomatology in a community sample of adults.
Perfectionism is a multidimensional personality trait that is broadly characterized by the relentless pursuit of absolute perfection, harsh self-criticism, excessively negative reactions to perceived mistakes, and the inability to experience satisfaction even when excessively high standards are met (Frost et al. 1990; Hewitt and Flett 1991; Sirois and Molnar 2016). Although associations between perfectionism and anxiety have received extensive theoretical and empirical support (Affrunti and Woodruff-Borden 2018; Burgess and DiBartolo 2016; Hewitt and Flett 1991) and perfectionism has been implicated extensively in stress and stress-related health problems (Dunkley 2018; Molnar et al. 2018), the relationship between perfectionism and reactions following exposures to traumatic stressors has received little attention. There are sound theoretical reasons to expect a positive association between perfectionism and PTSD symptoms (see Flett et al. 2016). Traumatic experiences may be responded to quite negatively in individuals with elevated levels of perfectionism because these individuals have a strong need for control and are often highly stressed by events beyond their control (Flett et al. 1995; Hewitt and Flett 2002). Indeed, situations that evoke feelings of helplessness and a sense of not being in control (e.g., the COVID-19 pandemic) are felt acutely by perfectionists (see Flett and Hewitt 2020). Traumatic events also underscore for the person who needs to be perfect or who feels a pressure to be perfect that things have been far from ideal and their efforts and actions have been negatively impacted. Perfectionists are particularly at risk for experiencing PTSD symptomatology after a traumatic event because they typically feel responsible for negative outcomes and experiences (for an extended discussion, see Flett et al. 2016). Accordingly, in light of these observations, we tested a model in which the associations between trait dimensions of perfectionism and PTSD symptomatology were moderated by perceived control in a trauma-exposed community sample.
Studies employing unidimensional perfectionism measures have found some initial support for a link between perfectionism and PTSD symptom endorsement (Kolts et al. 2004; Mitchell et al. 2012; Robins et al. 1994). Research on PTSD and perfectionism as a multidimensional construct has thus far relied on the attitudinal measure of perfectionism developed by Frost et al. (1990). This inventory assesses various components including high personal standards, doubts about actions, concern over mistakes, excessive parental expectations, and excessive parental criticism. A study by Kawamura et al. (2001) examined associations among perfectionism, depression, PTSD, and obsessive-compulsive disorder in a sample of college students and found significant positive correlations between PTSD symptoms and both personal standards and the maladaptive perfectionism composite factor that combined the other four subscales.
Egan et al. (2014) tested a model in which the link between multidimensional perfectionism and PTSD symptomatology was mediated by rumination in 30 patients with PTSD. Participants completed two Frost subscales (personal standards and concern over mistakes) and a clinical perfectionism measure. PTSD symptomatology was assessed via the Posttraumatic Stress Checklist (Civilian) for DSM-IV (Weathers et al. 1991). Results demonstrated that concern over mistakes and clinical perfectionism each were positively associated with PTSD symptoms. A robust association was also found between depressive rumination and PTSD symptoms, and depressive rumination mediated the link between multidimensional perfectionism and PTSD symptoms. That is, individuals higher in perfectionism who responded by brooding were in turn more likely to experience PTSD symptoms.
We sought in the current study to extend previous research in two significant respects. First, we utilized Hewitt and Flett’s (1991) influential conceptualization of multidimensional trait perfectionism. To our knowledge, this framework has not been used to evaluate the link between perfectionism and PTSD symptomatology. The model advanced by Hewitt and Flett (1991) is unique in its emphasis of both the personal and interpersonal elements of the perfectionism construct. This conceptual model of perfectionism includes a focus on personal perfectionism (i.e., self-oriented perfectionism), but also perfection demanded from others (i.e., other-oriented perfectionism) and the sense of being target and having pressure to meet perceived perfectionistic demands imposed on the self by others (i.e., socially prescribed perfectionism). Interpersonal elements of perfectionism should be particularly relevant when PTSD symptoms arise from interpersonally based trauma and it occurs within a context of social disconnection and limited social support (see Hewitt et al. 2006, 2017).
While the possible role of socially prescribed perfectionism in PTSD has not been directly explored, theory and research support that socially prescribed perfectionism is a vulnerability factor for PTSD symptomatology. Indeed, socially prescribed perfectionism has been implicated in several types of maladjustment (Hewitt and Flett 1991; Limburg et al. 2016). A persistent theme in the PTSD literature is that there is a subset of people with PTSD who experience profound shame and social anxiety due to a sense of not living up to social expectations and tendencies to anticipate negative social experiences and negative social evaluation (e.g., Budden 2009; Collimore et al. 2010; Dorahy et al. 2013; Zayfert et al. 2005). Consequently, socially prescribed perfectionism may be a key element when posttraumatic stress is rooted in a sense of not living up to social expectations because individuals with extreme levels of socially prescribed perfectionism would be confronted continuously with a sense of failing to live up to the impossible expectations imposed on them.
Second, we tested the possibility that low perceived control interacts with trait dimensions of perfectionism to produce greater PTSD symptoms. The importance of perceived control has been underscored in both the perfectionism and PTSD literatures. With respect to perfectionism, research has established that self-oriented perfectionism and other-oriented perfectionism are associated with a greater need for control (Flett et al. 1995), so traumatic events could violate this need for control and predictability. Research has demonstrated that socially prescribed perfectionism is associated with a lack of interpersonal control (Flett et al. 1995), general perceptions of a lack of perceived control (Buhr and Dugas 2006), and low self-control (Tangney et al. 2004). The sense of low personal control and helplessness that accompanies socially prescribed perfectionism (Hewitt and Flett 1991) could set the stage for higher levels of PTSD symptoms among people with elevated socially prescribed perfectionism.
Foa et al. (1992) emphasized the role of perceived control in the development of PTSD in their seminal paper. They asserted that the uncontrollability of the event is central to the development of PTSD. Studies have established that lower perceived control in general is associated with PTSD severity (Bolstad and Zinbarg 1997; Doerfler et al. 2005; Kushner et al. 1993). Other evidence suggest that feelings of inefficacy and low perceived control contribute to distress reactions among people with high levels of perfectionism (Dunkley et al. 2020; Martin et al. 1996; Mor et al. 1995). These findings suggest that a lack of personal mastery or control could be a key factor in terms of how certain individuals with high levels of perfectionism react to traumatic stressors. It is important to note that work by Frazier and associates has clarified that the key element is current perceptions of perceived control rather than past perceived control or perceptions of anticipated control (Frazier et al. 2001, 2004). Accordingly, perceived control was also assessed in the present study.
In this study, we tested a model in which the associations between trait dimensions of perfectionism and PTSD symptomatology were moderated by perceived control in a trauma-exposed community sample. We hypothesized that higher levels of trait perfectionism and lower levels of perceived control would be associated with greater PTSD symptomatology. We also hypothesized that the relationships between trait dimensions of perfectionism and PTSD symptomatology would vary as a function of perceived control, such that those with higher levels of perfectionism and lower levels of perceived control would report higher levels of PTSD symptomatology. Neuroticism, respondent sex, age, income, education, the number of traumatic events that the participants experienced, and the average age of onset of trauma were incorporated into analyses to determine whether perfectionism provided greater incremental explanatory power over and above these constructs. This was important given that these variables have been strongly related to PTSD symptomatology (Jaksic et al. 2012), and negative emotionality is a key feature among a subset of PTSD sufferers described as internalizers (Rielage et al. 2010). Moreover, neuroticism has been strongly linked to perfectionism, particularly socially prescribed perfectionism (Enns et al. 2005; Hill et al. 1997) and it is important to ascertain how perfectionism relates to PTSD and perceived control while still taking into account the predictive utility of related individual differences in neuroticism.
Method
Participants
A community sample of adults was recruited to participate in a closed-access web-based study of personality and health through advertisements in newspapers and posters in the Southern Ontario region and through advertisements on websites. Selection criteria included that participants be at least 18 years old and computer literate with an email address. Individuals who agreed to participate (N = 249; 57% women) completed a confidential web-based questionnaire. Informed consent was obtained for this study and the University Ethics Board approved this study. Respondents were paid $25 for their participation. The average age was 33.24 years old, with age ranging from 20 to 78 years. The majority of the respondents in this sample (97%) were Canadian citizens. Ethnicity was not assessed in this study due to an omission on the questionnaire. With respect to education level, 2% had less than high school, 11% completed high school, 21% had some college training or completed college, 49% had some university training or completed their Bachelor’s degree, and 17% completed a graduate level of professional degree.
It is important to note that our participants were restricted in one key respect. Given our interest in trauma and PTSD symptomatology, we limited our focus to only those individuals who reported experiencing at least one traumatic event in their lifetime (n = 161, 56% women). It should be noted that results from independent samples t tests indicated that individuals who reported experiencing traumatic experiences were not significantly different from individuals who reported no traumatic experiences on any of the study variables with the exception of household income (t(236) = − 2.61, p = .01) and total PTSD symptoms (t(236) = − 2.06, p = .04). That is, individuals who experienced traumatic events reported greater household income and greater PTSD symptomatology than people who did not experience traumatic events.
Measures
Perfectionism
Perfectionism was assessed with the 45-item Multidimensional Perfectionism Scale (HFMPS; Hewitt and Flett 1991). The self-oriented perfectionism subscale measures the extent to which individuals place high standards on themselves (e.g., “One of my goals is to be perfect in everything I do”). The other-oriented perfectionism subscale measures the extent to which an individual places high standards of achievement on significant others (e.g., “I cannot stand to see people close to me make mistakes”). Finally, the socially prescribed perfectionism subscale measures the extent to which people feel that high standards are being imposed on them by significant others (e.g., “The people around me expect me to succeed in everything I do”). Each item is rated on a scale from 1 (strongly disagree) to 7 (strongly agree), with subscale scores ranging from 15 to 105. Higher scores indicate higher levels of perfectionism. The HFMPS subscales have demonstrated adequate reliability and validity in both clinical and non-clinical samples (Hewitt and Flett 2004).
Perceived Control
The 10-item measure of global perceived personal control (Chipperfield et al. 2004; Ruthig et al. 2007) was employed to assess perceived control. This inventory assesses perceived control over various aspects of one’s life (e.g., How much influence do you have over your life in general?). Participants make 1 to 10 ratings ranging from “almost no influence” to “total influence.” Analyses indicate that the measure has one factor with items having item-total correlations ranging from .42 to .79 (Ruthig et al. 2008). Scale scores range from 10 to 100. Higher scores reflect greater perceived control.
Trauma
The Life Events Checklist (LEC; Blake et al. 2000) assesses 16 different potentially traumatic events (PTEs) acknowledged to lead to a diagnosis of PTSD according to DSM-IV criteria or other difficulties associated with posttraumatic stress and to cue PTEs prior to the assessment of PTSD symptoms. Respondents indicate whether each trauma occurred or not by choosing a yes or no response and a total count is calculated for the number of traumas experienced. For each PTE, participants were also instructed to indicate the years since the traumatic event occurred.
PTSD Symptoms
The Modified PTSD Symptoms Scale-Self-Report (MPSS-SR; Falsetti et al. 1993; Resick et al. 1991) was used to measure posttraumatic distress. This measure assesses multiple traumas instead of only examining PTSD symptomatology that is caused by a particular traumatic experience. Participants rated the frequency and severity of 16 symptoms reflecting the DSM-IV diagnostic criteria for PTSD. A total score was calculated by summing the frequency and severity scores (APA 1994). The MPSS-SR has demonstrated good psychometric properties in treatment and community samples (Coffey et al. 1998; Falsetti et al. 1993).
Neuroticism
The neuroticism subscale from the 40-item “Mini-Markers” measure of the five-factor model (FFM) developed by Saucier (1994) was also administered. Neuroticism was assessed by eight items, each rated on a Likert scale ranging from 1 (extremely inaccurate) to 9 (extremely accurate). A composite score was created by taking the mean of the neuroticism items. Scores ranged from 1 to 9.
Data Analyses
A two-step hierarchical multiple regression was employed using SPSS 20 statistical software with bootstrapping procedures for generating 95% bias-corrected regression coefficients and accelerated confidence intervals for each effect. Interaction terms were computed for each perfectionism dimension and perceived control. Because composite variables, such as interaction terms, are correlated with their component variables, to reduce multicollinearity and to ease the interpretation and probing of significant interactions, each component variable was centered around its sample mean before the interaction terms were computed (Aiken and West 1991; Cohen et al. 2003) and only the centered variables were entered into the regression models.
Specifically, PTSD symptoms were regressed on respondent’s age, household income, education, number of traumas experienced, average age of onset of trauma, respondent’s sex, neuroticism, perfectionism dimensions, and perceived control in step 1, and the non-linear components (i.e., perfectionism dimensions by perceived control) in step 2. Significant interactions were further investigated employing a series of post hoc regression equations, referred to as simple slopes analysis by Aiken and West (1991). For example, to test the hypothesis that the relationship between socially prescribed perfectionism and PTSD symptomatology varies as a function of perceived control, simple slopes analyses were conducted to observe differences in slope by perceived control and to determine whether these slopes differed significantly from zero. Finally, given the relatively large number of variables in each model, an adaptation of Fisher’s protected t test strategy, as described in Cohen et al. (2003), was employed as a method of evaluating the statistical significance of the predictors to control for type 1 error inflation.
Results
Descriptive Statistics and Bivariate Correlations
Means, standard deviations, and correlations between all model variables are presented in Table 1. The mean HFMPS subscale scores were in keeping with norms for community samples (see Hewitt and Flett 2004). From Table 1, it is clear that individuals reported experiencing an average of approximately two traumatic experiences. The three most common traumatic experiences reported were transportation accidents (n = 94, 56%), a sudden and unexpected death of a close other (n = 60, 36%), and physical assault (n = 48, 29%), and the least common traumatic experiences being causing another individual serious injury, harm, or death (n = 3, 2%), exposure to combat (n = 2, 1%), and captivity (n = 0, 0%). Overall, 4.8% of the sample was in the clinical range for PTSD symptomatology.
Table 1.
Means, standard deviations, scale reliabilities, and bivariate correlations for model variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | ------ | |||||||||||
| 2. Education | − .01 | ------- | ||||||||||
| 3. Income | .08 | .32*** | ----- | |||||||||
| 4. Sex | .11 | .01 | .08 | ----- | ||||||||
| 5. Neuroticism | .01 | − .15t | − .13 | − .18* | ----- | |||||||
| 6. Trauma | .16* | − .19* | − .07 | − .04 | .17* | ------- | ||||||
| 7. Trauma age | .69*** | .01 | .08 | .17* | .07 | .05 | ----- | |||||
| 8. SOP | − .18* | − .02 | .11 | − .03 | .09 | .04 | − .01 | ------ | ||||
| 9. OOP | − .17* | .11 | .22* | .12 | .06 | − .02 | − .01 | .57*** | ------- | |||
| 10. SPP | − .11 | − .05 | − .01 | − .05 | .33*** | .13 | .02 | .53*** | .28*** | -------- | ||
| 11. PC | .01 | .08 | − .00 | − .12 | − .35*** | − .08 | − .13 | − .10 | − .12 | − .39*** | -------- | |
| 12. PTSD | − .15 | − .13 | − .12 | − .08 | .26** | .49*** | .00 | .14 | .06 | .33*** | − .27** | ------ |
| M | 33.24 | 5.00 | 7.75 | .44 | 4.49 | 2.39 | 23.09 | 65.20 | 56.90 | 51.45 | 8.01 | 12.95 |
| SD | 10.84 | 1.79 | 3.19 | n/a | 1.46 | 1.61 | 9.95 | 16.34 | 12.41 | 13.50 | 1.44 | 16.26 |
| α | Single item | Single item | Single item | Single item | .74 | Count variable | Single item | .89 | .79 | .86 | .92 | .98 |
n = 161. SOP, self-oriented perfectionism; OOP, other-oriented perfectionism; SPP, socially prescribed perfectionism; PC, perceived control; Trauma age, average age of onset for traumatic experiences
t p < .06, *p < .05, **p < .01, ***p < .001
At the level of bivariate associations, results indicated that socially prescribed perfectionism was the only HFMPS dimension linked with experiencing greater PTSD symptomatology. Significant positive associations were also found between each of the perfectionism dimensions. Neuroticism was positively related to socially prescribed perfectionism and PTSD symptomatology. The number of traumatic experiences was positively related to PTSD symptomatology. Finally, perceived control was negatively associated with neuroticism, socially prescribed perfectionism, and PTSD symptomatology.
Regression Analyses
Overall, the model was statistically significant, accounting for 45% of the variability in PTSD symptoms (F(14,146) = 8.36, p < .001). Results are presented in Table 2. With respect to the main effects, the number of traumas experienced, average age of onset of trauma, and socially prescribed perfectionism were each positively associated with PTSD symptomatology. Thus, individuals who experienced more frequent trauma experienced trauma at older ages, and those who reported higher levels of socially prescribed perfectionism experienced greater PTSD symptomatology. Age was negatively related to PTSD symptomatology, indicating that older individuals experienced less PTSD symptoms.
Table 2.
Summary of the regression of PTSD symptomatology on relevant demographics, number of traumas, average age of onset of trauma, neuroticism, perfectionism dimensions, perceived control, and interactions between perfectionism dimensions and perceived control
| Step | Variable | B | SE B | 95% CI | β | sr2 | |
|---|---|---|---|---|---|---|---|
| Lower bound | Upper bound | ||||||
| 1 | Age | − .52*** | .14 | − .793 | − .237 | − .34 | .054 |
| Education | .00 | .63 | − 1.234 | 1.236 | .00 | .000 | |
| Income | − .27 | .35 | − .966 | .428 | − .05 | .002 | |
| Neuroticism | .60 | .81 | − 1.007 | 2.210 | .05 | .002 | |
| Trauma | 4.95*** | .68 | 3.613 | 6.286 | .49 | .215 | |
| Trauma age | .33* | .15 | .030 | .621 | .20 | .019 | |
| Respondent sex | − 1.02 | 2.13 | − 5.238 | 3.190 | − .03 | .001 | |
| SOP | − .04 | .09 | − .218 | .138 | − .06 | .001 | |
| OOP | − .03 | .11 | − .242 | .178 | − .02 | .000 | |
| SPP | .23* | .10 | .030 | .433 | .21 | .021 | |
| Perceived control | − 1.30 | .83 | − 2.932 | .341 | − .12 | .010 | |
| 2 | SOP by perceived control | .09 | .06 | − .021 | .199 | .15 | .010 |
| OOP by perceived control | − .14 | .09 | − .311 | .031 | − .14 | .010 | |
| SPP by perceived control | − .17** | .06 | − .286 | − .063 | − .25 | .036 | |
n = 161; SOP, self-oriented perfectionism; OOP, other-oriented perfectionism; SPP, socially prescribed perfectionism; Trauma age, average age of onset for traumatic experiences
For step 1 of the regression equation, R2change = .40, Fchange(11, 149) = 9.07, p < .001. For step 2 of the regression equation, R2change = .04, Fchange(3, 146) = 3.84, p = .011
***p < .001, **p < .01, *p < .05
Socially prescribed perfectionism remained positively associated with PTSD symptoms after accounting for the demographic variables, number of traumas experienced, average age of onset of trauma, and neuroticism (see Table 2). Finally, an interaction between socially prescribed perfectionism and perceived control was observed (see Fig. 1). As hypothesized, results of follow-up simple slopes analyses indicated that a significant positive association was present between socially prescribed perfectionism and PTSD symptomatology at low levels of perceived control (b = .48, p < .001). The relationship between socially prescribed perfectionism and PTSD symptomatology was not statistically significant (b = .06, p = .63), at high levels of perceived control. None of the other associations was statistically significant. Given concerns that the inclusion of covariates could potentially bias results (see Simmons et al. 2011), the model was tested with and without the covariates. No meaningful differences in the results emerged when the covariates were not included in the model.
Fig. 1.
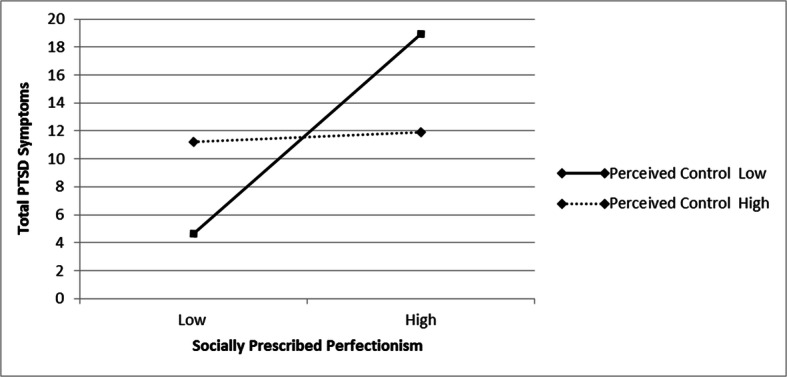
Two-way interaction of socially prescribed perfectionism and perceived control on PTSD symptoms
Discussion
The purpose of this research was to investigate how the trait perfectionism dimensions conceptualized by Hewitt and Flett (1991) are associated with PTSD symptomatology in a community sample of adults. We also investigated whether the associations between trait perfectionism dimensions and PTSD symptoms varied as a function of perceived control. Our correlational results revealed a positive link between socially prescribed perfectionism and PTSD symptoms. That is, higher levels of socially prescribed perfectionism were associated with greater PTSD symptomatology. Socially prescribed perfectionism was also associated with reduced perceived control and higher levels of neuroticism. Examination of these factors in a regression analysis that also included relevant demographics, neuroticism, the reported number of traumatic events experienced by the participants, and the average age of onset of trauma established that socially prescribed perfectionism provided incremental predictive utility with respect to PTSD symptomatology.
Subsequent tests of moderator effects found no evidence that self-oriented or other-oriented perfectionism interacted with low perceived control, but an interaction between socially prescribed perfectionism and perceived control was observed. Individuals who were characterized jointly by high socially prescribed perfectionism and low perceived control in life were particularly likely to experience elevated PTSD symptoms. This interaction is understandable and meaningful given that past research has established that individuals with higher levels of socially prescribed perfectionism also tend to exhibit a deficit in cognitive-emotion regulation abilities and demonstrate maladaptive coping tendencies (Rudolph et al. 2007). These people tend to feel controlled by others’ expectations and are often confronted with the realization that they are falling short of the lofty expectations they perceive to be imposed on them. Individuals in this situation who feel that they are not in control and perhaps lack a sense of self-efficacy are people who, in all likelihood, feel overwhelmed by previous traumatic stress along with images and cognitions related to this trauma, while also dealing with feeling like a failure for not being able to meet unrealistically high social standards. Moreover, a subset of these people will likely see their lack of control as a personal failure to the extent that they pride themselves on being people who are typically in control and who must be in control to feel efficacious and successful. This research has clear theoretical implications in terms of the need to incorporate key moderators such as perceived control into models of perfectionism and poor psychological adjustment. This focus on perceived control should extend to including appraisals of the degree to which uncontrollability is seen as a very personal failure in the ability to exert control by those who assume too much responsibility for outcomes that are perhaps beyond the control of any one person. This emphasis on key contextual factors is in keeping with the original emphasis by Hewitt and Flett (1991) on the need to conceptual dimensions of perfectionism as vulnerability factors that will be activated or amplified when life experiences and related variables come into play.
This study also has clear practical implications for the treatment of PTSD. An explicit focus on perfectionism and associated themes should be particularly beneficial to the subset of people who have PTSD and who are higher in socially prescribed perfectionism. Since cognitive-behavioral therapy is one of the most recommended therapies for PTSD, our results indicate that therapists would benefit from paying special attention to maladaptive cognitions that are associated with socially prescribed perfectionism. The benefits of promoting mindfulness among vulnerable perfectionists have also been noted (see Flett et al. in press). However, it is important to acknowledge the treatment challenges when working with traumatized individuals higher in socially prescribed perfectionism. A growing body of research indicates that individuals characterized by higher levels of perfectionism are less likely than individuals lower in perfectionism to benefit from psychological interventions and when they are undergoing treatment, they often require longer interventions (Blatt and Zuroff 2002; Hewitt et al. 2017). This is particularly the case when people higher in perfectionism are undergoing treatment (see Hewitt et al. 2008, 2018). Moreover, given the relational nature of socially prescribed perfectionism and relational outcomes evident in PTSD, treatments that have a relational focus may be particularly effective on disorders such as PTSD. Certainly, there is evidence that these psychodynamically oriented treatments are effective in both perfectionism (Hewitt et al. 2018) and in treatment of PTSD (Schottenbauer et al. 2008). One implication that follows from the apparent role of socially prescribed perfectionism in PTSD is that certain individuals with higher levels of socially prescribed perfectionism may be particularly prone to the feelings of social anxiety and shame that complicate recovery from PTSD. It is quite possible that socially prescribed perfectionism plays a role in vulnerability to PTSD, but socially prescribed perfectionism also complicates the recovery process for those individuals receiving treatment for PTSD.
The current study provided no indication of a role for self-oriented or other-oriented perfectionism in the experience and expression of PTSD. However, it seems to us that it would be decidedly premature to exclude these trait perfectionism dimensions from further consideration. Indeed, Hewitt and Flett’s (1991) conceptualization and theory of perfectionism would support the notion that traumatic events which are attributed internally to the self should impact self-oriented perfectionists who feel a strong sense of responsibility and have experienced setbacks and trauma that may have impacted their goal-related pursuits and their sense of self. However, given that self-oriented perfectionism was developed and is conceptualized as a vulnerability factor and not expected, necessarily to have main effect associations with negative outcomes, it may be that self-oriented perfectionism is only associated with PTSD symptomatology under conditions of high stress and when particular events and failures to control outcomes are seen as a personal shortcoming or failure. Thus, future research is encouraged to continue to explore the potential role of self-oriented and other-oriented perfectionism along with relevant moderators when assessing how perfectionism may contribute to greater PTSD symptomatology among individuals who have experienced trauma.
While this study yielded some unique findings, the results must be interpreted within the context of some limitations. Importantly, the cross-sectional nature of this study precludes making causal statements. Multidimensional perfectionism and PTSD must be studied from a longitudinal perspective. Reciprocal relations may be found because it is plausible that striving for perfection and trying to meet perfectionistic expectations may be adopted by some people as a way of coping with trauma. This possibility was introduced in the social reaction model of perfectionism postulated by Flett et al. (2002a). According to this formulation, people exposed to trauma and maltreatment tend to become highly focused on becoming perfect to ward off further traumatic events and mistreatment.
One strength of this study was that our hypotheses were tested with a community sample of adults, rather than with a student sample, as is typical in the literature. Although a community sample offers increased generalizability of the findings, results of this study are still restricted to a non-clinical sample in which the average for PTSD symptoms was quite low. Thus, future studies would be well served to assess the links among perfectionism, perceived control, and PTSD symptomatology in people who have been clinically diagnosed with PTSD.
It will also be important for future research to establish the unique predictive ability of perfectionism when examined within the context of other predictors associated with vulnerability to PTSD. For example, the extent to which the link between interpersonal elements of perfectionism and PTSD symptoms reflects the associations that interpersonal perfectionism and PTSD symptoms have with an insecure attachment style remains unclear (Besser et al. 2009). Future investigations would also benefit from examining the possible mediating role of factors that likely underscore the association between perfectionism and PTSD symptoms. Potentially significant factors to consider include intolerance of uncertainty and anxiety sensitivity. Both factors have been linked jointly with perfectionism and PTSD symptomatology (Asmundson and Stapleton 2008; Buhr and Dugas 2006; Fetzner et al. 2013; Flett et al. 2004) and both factors likely define the people with high levels of perfectionism who are particularly prone to PTSD.
Finally, given that research on perfectionism and PTSD is still in its early stages, it is important to explore the possible role of other conceptualizations and measures of perfectionism in PTSD, including chronic and frequent automatic thoughts about the need to be perfect (Flett et al. 1998). This cognitive aspect of the perfectionism construct tends to predict unique variance in distress beyond the variance predicted by trait perfectionism dimensions (Flett et al. 1998, 2007). The potential role of perfectionistic automatic thoughts is suggested by the results of a study by Flett et al. (2002b) which established that scores on the Perfectionism Cognitions Inventory were associated with reports of intrusive cognitive images as assessed by the Impact of Event Scale (Horowitz et al. 1979).
In summary, this study evaluated the roles of trait perfectionism dimensions and perceived control in PTSD symptomatology in adults from the community. This study uniquely established a link between socially prescribed perfectionism and PTSD symptoms and found that socially prescribed perfectionism combined interactively with low perceived control to predict elevated PTSD symptoms. Our findings suggest that individuals higher in socially prescribed perfectionism who feel a strong pressure to meet social expectations for perfection will be particularly vulnerable to the experience of posttraumatic stress symptoms after experiencing trauma, such as the COVID-19 pandemic. Presumably, these individuals in particular would benefit from attempts to bolster their resilience levels and ability to cope prior to being exposed to life situations that could involve experiencing traumatic stressors.
Funding Information
Preparation of this article was financially supported by a Tier 1 Canada Research Chair in Personality and Health awarded to Gordon L. Flett.
Compliance with Ethical Standards
Informed consent was obtained for this study and the University Ethics Board approved this study.
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Affrunti NW, Woodruff-Borden J. Perfectionism and anxiety in children. In: Stoeber J, editor. The psychology of perfectionism: theory, research, applications. New York: Routledge/Taylor & Francis Group; 2018. pp. 113–133. [Google Scholar]
- Aiken LS, West SG. Multiple regression: testing and interpreting interactions. London: Sage Publications Inc.; 1991. [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 1994. [Google Scholar]
- Asmundson GJ, Stapleton JA. Associations between dimensions of anxiety sensitivity and PTSD symptom clusters in active-duty police officers. Cognitive Behavior Therapy. 2008;37:66–75. doi: 10.1080/16506070801969005. [DOI] [PubMed] [Google Scholar]
- Besser A, Neria Y, Haynes M. Adult attachment, perceived stress, and PTSD among civilians exposed to ongoing terrorist attacks in Southern Israel. Personality and Individual Differences. 2009;47:851–857. [Google Scholar]
- Blake D, Weathers F, Nagy L, Kaloupek D, Klauminzer G, Charney D, et al. Clinician-Administered PTSD Scale (CAPS) instruction manual. Springfield: National Center for PTSD, National Technical Information Service; 2000. [Google Scholar]
- Blatt SJ, Zuroff DC. Perfectionism in the therapeutic process. In: Flett GL, Hewitt PL, editors. Perfectionism: theory, research, and treatment. Washington, DC: American Psychological Association; 2002. pp. 393–406. [Google Scholar]
- Bolstad R, Zinbarg RE. Sexual victimization, generalized perception of control, and posttraumatic stress disorder symptom severity. Journal of Anxiety Disorders. 1997;11:523–540. doi: 10.1016/s0887-6185(97)00028-5. [DOI] [PubMed] [Google Scholar]
- Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and posttraumatic stress disorder in the community. Archives of General Psychiatry. 1998;55:626–632. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- Budden A. The role of shame in posttraumatic stress disorder: a proposal for a socio-emotional model for DSM-V. Social Science and Medicine. 2009;69:1032–1039. doi: 10.1016/j.socscimed.2009.07.032. [DOI] [PubMed] [Google Scholar]
- Buhr K, Dugas MJ. Investigating the construct validity of intolerance of uncertainty and its unique relationship with worry. Journal of Anxiety Disorders. 2006;20:222–236. doi: 10.1016/j.janxdis.2004.12.004. [DOI] [PubMed] [Google Scholar]
- Burgess A, DiBartolo PM. Anxiety and perfectionism: relationships, mechanisms, and conditions. In: Sirois FM, Molnar DS, editors. Perfectionism, health, and well-being. Cham: Springer International Publishing; 2016. pp. 177–203. [Google Scholar]
- Chipperfield JG, Campbell DW, Perry RP. Stability in perceived control: implications for health among very old community-dwelling adults. Journal of Aging and Health. 2004;16:116–147. doi: 10.1177/0898264303260447. [DOI] [PubMed] [Google Scholar]
- Coffey SF, Dansky BS, Falsetti SA, Saladin ME, Brady KT. Screening for PTSD in a substance abuse sample: psychometric properties of a modified version of the PTSD Symptom Scale Self-Report. Journal of Traumatic Stress. 1998;11:393–399. doi: 10.1023/A:1024467507565. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. 3. Mahwah: Erlbaum; 2003. [Google Scholar]
- Collimore KC, Carleton RN, Hofmann SG, Asmundson GJG. Posttraumatic stress and social anxiety: the interaction of traumatic events and interpersonal fears. Depression and Anxiety. 2010;27:1017–1026. doi: 10.1002/da.20728. [DOI] [PubMed] [Google Scholar]
- Doerfler LA, Paraskos JA, Piniarski L. Relationship of quality of life and perceived control with posttraumatic stress disorder symptoms 3 to 6 months after myocardial infarction. Cardiopulmonary Rehabilitation. 2005;25:166–172. doi: 10.1097/00008483-200505000-00008. [DOI] [PubMed] [Google Scholar]
- Dorahy MJ, Corry M, Shannon M, Webb K, McDermott B, Ryan M, Dyer KFW. Complex trauma and intimate relationships: the impact of shame, guilt, and dissociation. Journal of Affective Disorders. 2013;147:72–79. doi: 10.1016/j.jad.2012.10.010. [DOI] [PubMed] [Google Scholar]
- Dunkley DM. Perfectionism and daily stress, coping, and affect: advancing multilevel explanatory conceptualizations. In: Stoeber J, editor. The psychology of perfectionism: theory, research, applications. New York: Routledge; 2018. pp. 222–342. [Google Scholar]
- Dunkley, D. M., Starrs, C. J., Gouveia, L., & Moroz, M. (2020). Self-critical perfectionism and lower daily perceived control predict depressive and anxious symptoms over four years. Journal of Counseling Psychology. Advance online publication. [DOI] [PubMed]
- Egan SJ, Hattaway M, Kane RT. The relationship between perfectionism and rumination in posttraumatic stress disorder. Behavioral and Cognitive Psychotherapy. 2014;42:211–223. doi: 10.1017/S1352465812001129. [DOI] [PubMed] [Google Scholar]
- Enns MW, Cox BJ, Clara IP. Perfectionism and neuroticism: a longitudinal study of specific vulnerability and diathesis-stress models. Cognitive Therapy and Research. 2005;29:463–478. [Google Scholar]
- Falsetti SA, Resnick HS, Resnick PA, Kilpatrick DG. The Modified PTSD Symptom Scale: a brief self-report measure of posttraumatic stress disorder. The Behavior Therapist. 1993;16:161–162. [Google Scholar]
- Fetzner MG, Horswill SC, Boelen PA, Carleton RN. Intolerance of uncertainty and PTSD symptoms: exploring the construct relationship in a community sample with a heterogeneous trauma history. Cognitive Therapy and Research. 2013;37:725–734. [Google Scholar]
- Flett GL, Hewitt PL. The perfectionism pandemic meets COVID-19: understanding the stress, distress, and problems in living for perfectionists during the global health crisis. Journal of Concurrent Disorders. 2020;2(1):80–105. [Google Scholar]
- Flett GL, Hewitt PL, Blankstein KR, Mosher SW. Perfectionism, life events, and depressive symptoms: a test of a diathesis-stress model. Current Psychology. 1995;14:112–137. [Google Scholar]
- Flett GL, Hewitt PL, Blankstein KR, Gray L. Psychological distress and the frequency of perfectionistic thinking. Journal of Personality and Social Psychology. 1998;75:1363–1381. doi: 10.1037//0022-3514.75.5.1363. [DOI] [PubMed] [Google Scholar]
- Flett GL, Hewitt PL, Oliver JM, Macdonald S. Perfectionism in children and their parents: a developmental analysis. In: Flett GL, Hewitt PL, editors. Perfectionism: theory, research, and treatment. Washington, DC: American Psychological Association Press; 2002. pp. 89–132. [Google Scholar]
- Flett GL, Madorsky D, Hewitt PL, Heisel MJ. Perfectionism cognitions, rumination, and psychological distress. Journal of Rational-Emotive & Cognitive-Behavior Therapy. 2002;20:33–47. [Google Scholar]
- Flett GL, Greene A, Hewitt PL. Dimensions of perfectionism and anxiety sensitivity. Journal of Rational-Emotive and Cognitive-Behavior Therapy. 2004;22:37–55. [Google Scholar]
- Flett GL, Hewitt PL, Whelan T, Martin TR. The Perfectionism Cognitions Inventory: psychometric properties and associations with distress and deficits in cognitive self-management. Journal of Rational-Emotive & Cognitive-Behavior Therapy. 2007;25:255–277. [Google Scholar]
- Flett GL, Molnar DS, Hewitt PL. The traumatized perfectionist: understanding the role of perfectionism in post-traumatic reactions to stress. International Journal of Emergency Mental Health and Human Resilience. 2016;18:764–765. [Google Scholar]
- Flett, G. L., Nepon, T., Hewitt, P. L., & Rose, A. L. (in press). Why perfectionism is antithetical to mindfulness: a conceptual and empirical analysis and consideration of treatment implications. International Journal of Mental Health and Addiction.
- Foa EB, Zinbarg R, Rothbaum RO. Uncontrollability and unpredictability in posttraumatic stress disorder: an animal model. Psychological Bulletin. 1992;112:218–238. doi: 10.1037/0033-2909.112.2.218. [DOI] [PubMed] [Google Scholar]
- Frazier P, Berman M, Steward J. Perceived control and posttraumatic stress: a temporal model. Applied and Preventive Psychology. 2001;10:207–223. [Google Scholar]
- Frazier P, Steward J, Mortenson H. Perceived control and adjustment to trauma: a comparison across events. Journal of Social and Clinical Psychology. 2004;23:303–324. [Google Scholar]
- Frost RO, Marten P, Lahart C, Rosenblate R. The dimensions of perfectionism. Cognitive Therapy and Research. 1990;14:449–468. [Google Scholar]
- Hewitt PL, Flett GL. Perfectionism in the self and social contexts: conceptualizations, assessment, and association with psychopathology. Journal of Personality and Social Psychology. 1991;60:456–470. doi: 10.1037//0022-3514.60.3.456. [DOI] [PubMed] [Google Scholar]
- Hewitt PL, Flett GL. Perfectionism and stress processes in psychopathology. In: Flett GL, Hewitt PL, editors. Perfectionism: theory, research, and treatment. Washington, DC: American Psychological Association; 2002. pp. 255–285. [Google Scholar]
- Hewitt PL, Flett GL. Multidimensional Perfectionism Scale: technical manual. Toronto: Multi-Health Systems Inc.; 2004. [Google Scholar]
- Hewitt PL, Flett GL, Mikail SF. Perfectionism: a relational approach to assessment, treatment, and conceptualization. New York: Guilford; 2017. [Google Scholar]
- Hewitt, P. L., Flett, G. L., Mikail, S. F., Kealy, D., & Zhang, L. C. (2018). Perfectionism in the therapeutic context: The perfectionism social disconnection model. In J. Stoeber (Ed.), The Psychology of Perfectionism. London: Routledge.
- Hewitt, P. L., Flett, G. L., Sherry, S. B., & Caelian, C. (2006). Trait Perfectionism Dimensions and Suicidal Behavior. In T. E. Ellis (Ed.), Cognition and suicide: Theory, research, and therapy (pp. 215–235). Washington, DC, US: American Psychological Association.
- Hewitt, P. L., Habke, A. M., Lee-Baggley, D. L., Sherry, S. B., & Flett, G. L. (2008). The impact of perfectionistic self-presentation on the cognitive, affective, and physiological experience of a clinical interview. Psychiatry: Interpersonal and Biological Processes, 71, 93–122. [DOI] [PubMed]
- Hewitt PL, Mikail SF, Flett GL, Dang S. Specific formulation feedback in dynamic-relational group psychotherapy of perfectionism. Psychotherapy. 2018;55:179–185. doi: 10.1037/pst0000137. [DOI] [PubMed] [Google Scholar]
- Hill RW, McIntire K, Bacharach VR. Perfectionism and the Big Five factors. Journal of Social Behavior & Personality. 1997;12:257–270. [Google Scholar]
- Horowitz MJ, Wilner N, Alvarez W. Impacts of Events Scale: a measure of subjective stress. Psychometric Medicine. 1979;41:2009–2018. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- Jaksic N, Brajkovic L, Ivezic E, Topic R, Jakovljevic M. The role of personality traits in posttraumatic stress disorder (PTSD) Psychiatria Danubina. 2012;24:256–266. [PubMed] [Google Scholar]
- Johnson H, Thompson A. The development and maintenance of posttraumatic stress disorder (PTSD) in civilian adult survivors of war trauma and torture: a review. Clinical Psychology Review. 2008;28:36–47. doi: 10.1016/j.cpr.2007.01.017. [DOI] [PubMed] [Google Scholar]
- Kawamura KY, Hunt SC, Frost RO, DiBartolo PM. Perfectionism, anxiety, and depression: are the relationships independent? Cognitive Therapy and Research. 2001;25:291–301. [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Koenen KC, Ratanatharathorn A, Ng L, McLaughlin KA, Bromet EJ, Stein DJ, Karam EG, Meron Ruscio A, Benjet C, Scott K, Atwoli L, Petukhova M, Lim CCW, Aguilar-Gaxiola S, al-Hamzawi A, Alonso J, Bunting B, Ciutan M, de Girolamo G, Degenhardt L, Gureje O, Haro JM, Huang Y, Kawakami N, Lee S, Navarro-Mateu F, Pennell BE, Piazza M, Sampson N, ten Have M, Torres Y, Viana MC, Williams D, Xavier M, Kessler RC. Posttraumatic stress disorder in the World Mental Health Surveys. Psychological Medicine. 2017;47(13):2260–2274. doi: 10.1017/S0033291717000708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolts RL, Robinson AM, Tracy JJ. The relationship of sociotropy and autonomy to posttraumatic cognitions and PTSD symptomatology in trauma survivors. Journal of Clinical Psychology. 2004;60:53–63. doi: 10.1002/jclp.10193. [DOI] [PubMed] [Google Scholar]
- Kushner MG, Riggs DS, Foa EB, Miller SM. Perceived controllability and the development of posttraumatic stress disorder (PTSD) in crime victims. Behaviour Research and Therapy. 1993;31:105–110. doi: 10.1016/0005-7967(93)90048-y. [DOI] [PubMed] [Google Scholar]
- Limburg K, Watson HJ, Hagger MS, Egan SJ. The relationship between perfectionism and psychopathology: a meta-analysis. Journal of Clinical Psychology. 2016;73(10):1301–1326. doi: 10.1002/jclp.22435. [DOI] [PubMed] [Google Scholar]
- Martin TR, Flett GL, Hewitt PL, Krames L, Szantos G. Personality correlates of depression and health symptoms: a test of a self-regulation model. Journal of Research in Personality. 1996;31:264–277. [Google Scholar]
- Mitchell KS, Wells SY, Mendes A, Resick PA. Treatment improves symptoms shared by PTSD and disordered eating. Journal of Traumatic Stress. 2012;25:535–542. doi: 10.1002/jts.21737. [DOI] [PubMed] [Google Scholar]
- Molnar DS, Sirois FM, Flett GL, Janssen WF, Hewitt PL. Perfectionism and health: the roles of health behaviors and stress-related processes. In: Stoeber J, editor. The psychology of perfectionism: theory, research, applications. London: Routledge; 2018. pp. 200–221. [Google Scholar]
- Mor S, Day HI, Flett GL, Hewitt PL. Perfectionism, control, and components of performance anxiety in professional artists. Cognitive Therapy and Research. 1995;19:207–225. [Google Scholar]
- Resick PA, Falsetti SA, Resnick HS, Kilpatrick DG. The Modified PTSD Symptom Scale-Self-Report. St. Louis: University of Missouri & Charleston, SC: Crime Victims Research and Treatment Center; 1991. [Google Scholar]
- Rielage JK, Hoyt T, Renshaw K. Internalizing and externalizing personality styles and psychopathology in OEF-OIF veterans. Journal of Traumatic Stress. 2010;23:350–357. doi: 10.1002/jts.20528. [DOI] [PubMed] [Google Scholar]
- Robins CJ, Ladd J, Welkowitz J, Blaney PH, Diaz R, Kutcher G. The Personal Style Inventory: preliminary validation studies of new measures of sociotropy and autonomy. Journal of Psychopathology and Behavioral Assessment. 1994;16:277–300. [Google Scholar]
- Rudolph SG, Flett GL, Hewitt PL. Perfectionism and deficits in cognitive emotion regulation. Journal of Rational-Emotive and Cognitive-Behavior Therapy. 2007;25:343–357. [Google Scholar]
- Ruthig JC, Chipperfield JG, Newall NE, Perry RP, Hall NC. Detrimental effects of falling on health and well-being in later life: the mediating roles of perceived control and optimism. Journal of Health Psychology. 2007;12:231–248. doi: 10.1177/1359105307074250. [DOI] [PubMed] [Google Scholar]
- Ruthig JC, Chipperfield JG, Bailis DS, Perry RP. Perceived control and risk characteristics as predictors of older adults’ health risk estimates. The Journal of Social Psychology. 2008;148:667–688. doi: 10.3200/SOCP.148.6.667-688. [DOI] [PubMed] [Google Scholar]
- Saucier G. Mini-Markers: a brief version of Goldberg’s unipolar Big-Five markers. Journal of Personality Assessment. 1994;3:506–516. doi: 10.1207/s15327752jpa6303_8. [DOI] [PubMed] [Google Scholar]
- Schottenbauer MA, Glass CR, Arnkoff DB, Gray SH. Contributions of psychodynamic approaches to treatment of PTSD and trauma: a review of the empirical treatment and psychopathology literature. Psychiatry. 2008;71(1):13–34. doi: 10.1521/psyc.2008.71.1.13. [DOI] [PubMed] [Google Scholar]
- Simmons JP, Nelson LD, Simonsohn U. False-positive psychology: undisclosed flexibility in data collection and analysis allows presenting anything as significant. Psychological Science. 2011;22:1359–1366. doi: 10.1177/0956797611417632. [DOI] [PubMed] [Google Scholar]
- Sirois, F. M., & Molnar, D. S. (Eds.) (2016). Perfectionism, Health, and Well-Being.Cham, Switzerland: Springer International Publishing.
- Tangney JP, Baumeister RF, Boone AL. High self-control predicts good adjustment, less pathology, better grades, and interpersonal success. Journal of Personality. 2004;72:271–324. doi: 10.1111/j.0022-3506.2004.00263.x. [DOI] [PubMed] [Google Scholar]
- Van Ameringen M, Mancini C, Patterson B, Boyle MH. Post-traumatic stress disorder in Canada. CNS Neuroscience & Therapeutics. 2008;14(3):171–181. doi: 10.1111/j.1755-5949.2008.00049.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers FW, Huska JA, Keane TM. PCL-C for DSM-IV. Boston: National Center for PTSD-Behavioral Science Division; 1991. [Google Scholar]
- Zayfert C, Deviva J, Hofmann SG. Comorbid PTSD and social phobia in a treatment-seeking population: an exploratory study. Journal of Nervous and Mental Disease. 2005;193:93–101. doi: 10.1097/01.nmd.0000152795.47479.d9. [DOI] [PubMed] [Google Scholar]


