Abstract
A 60-year-old, South-Asian male patient presented with a dark brown lesion on his left conjunctiva surface near the limbus for 2 years. Examination showed a globular, dark brown-coloured mass near the temporal limbus at 4 to 5 o'clock position, measuring 3 × 3 × 2 mm. There were a few scattered flat pigmented lesions near the mass and also a few prominent vessels. The mass underwent wide local excision, with a clear margin, followed by double freeze cryotherapy of the conjunctival margins along with the application of Mitomycin C. The bare sclera was covered by amniotic membrane. Histology surprisingly revealed a nodular basal cell carcinoma (BCC) containing melanin. The melanin was present in the tumour cell cytoplasm, within melanophages and within dendritic, Melan A-positive melanocytes. The BCC was immunohistochemically positive for BerEP4 and negative for EMA. The clinically observed smaller nodules flanking the main pigmented BCC corresponded histologically to pigmented superficial growth pattern BCC connected to the under surface of the conjunctival epithelium. This is the first report of a pigmented BCC of the conjunctiva, mimicking a conjunctival melanoma. Pigmented BCC should be considered in the differential diagnosis of pigmented tumours of the conjunctiva.
Keywords: Pigmented basal cell carcinoma, Conjunctival melanoma, Conjunctival non-melanocytic pigmented tumours, Basal cell carcinoma
Established Facts
Basal cell carcinoma (BCC) is a common eyelid skin tumour that can arise very rarely from the conjunctiva.
The pigmented variant of BCC accounts for 6% of skin BCCs but has never been reported in the conjunctiva.
Novel Insights
This is the first report of a pigmented BCC of the conjunctiva, mimicking a conjunctival melanoma.
The pigmented BCC showed prominent melanocyte hyperplasia, melanophages and tumour cell cytoplasmic melanin.
Pigmented BCC should be considered in the differential diagnosis of pigmented, non-melanocytic tumours of the conjunctiva.
Introduction
Pigmented conjunctival neoplasms can be divided into melanocytic and non-melanocytic. Common pigmented melanocytic neoplasms include naevi and melanoma. An example of a well-described pigmented non-melanocytic tumour is squamous carcinoma, occurring in patients with brown or black skin [1]. Basal cell carcinoma (BCC) has been very rarely reported to arise as a primary tumour of the conjunctiva [2, 3, 4, 5]. Pigmented BCC is well documented in the dermatopathology literature and accounts for around 6% of all cutaneous BCCs [6]. We describe the clinical and histopathological features of a dark brown mass at the left inferotemporal limbal area of a South-Asian male, thought to be a melanoma, but which histologically was a pigmented BCC and represents the first description of this rare subtype in the conjunctiva.
Case Report
A 60-year-old, South-Asian, Bangladeshi male patient attended the Orbit and Oculoplastic Department of the Chittagong Eye Infirmary and Training Complex (CEITC) in Bangladesh, with a dark brown lesion on his left conjunctiva surface near the limbus for 2 years, gradually increasing in size for 1 year. There was no history of trauma and no other systemic complaints.
On ocular examination, his best-corrected visual acuity was 20/30 in both eyes, and intraocular pressure was within normal limits. The biomicroscopic examination of the left eye showed a raised, globular, irregular, dark brown-coloured pigmented mass near the temporal limbus at 4 to 5 o'clock position, measuring about 3 × 3 × 2 mm (Fig. 1a). There were a few scattered flat pigmented lesions near the mass, and also a few prominent vessels were seen around the growth. The cornea was clear without any pigmentation. The posterior segment examination in both eyes revealed no abnormality. There was no evidence of preauricular or submandibular lymphadenopathy. There was no evidence of systemic endocrinopathy and no documented history of medication that could increase pigmentation (e.g., tetracyclines). The working clinical diagnosis was invasive conjunctival melanoma.
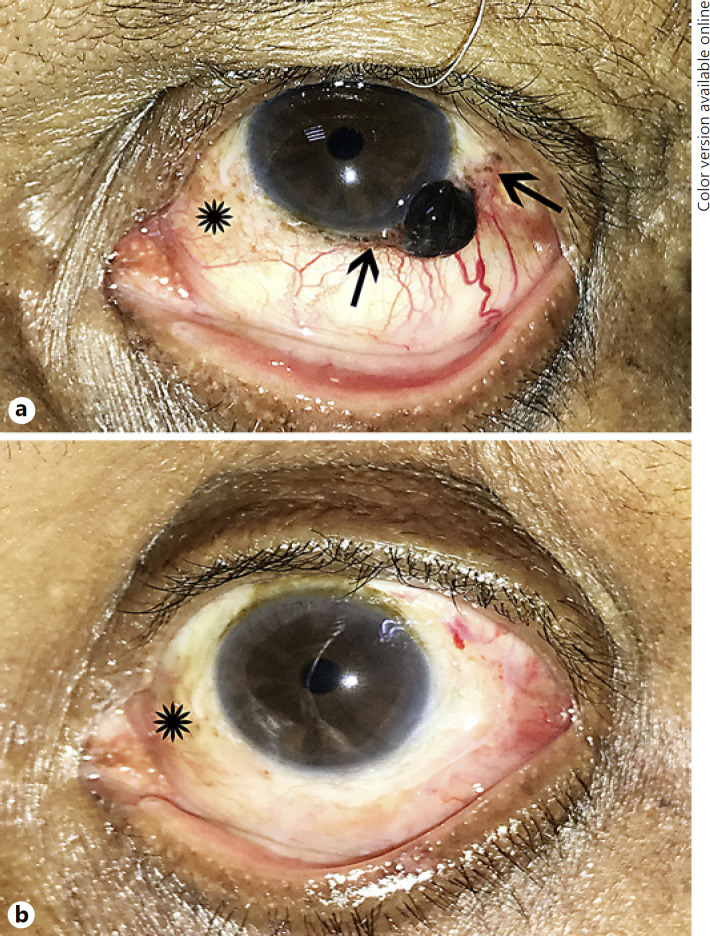
Fig. 1.
a Clinical photograph of the left ocular surface showing the black dome-shaped pigmented BCC. The asterisk indicates racial/complexion-associated benign melanosis. The arrow points to smaller black lesions either side of the main tumour mass. These are areas of pigmented superficial growth pattern BCC. b The post-surgical appearance of the left ocular surface. The asterisk indicates racial/complexion-associated benign melanosis.
The mass was removed by wide local excision of the tumour, with a clear margin of 4 mm, followed by double freeze cryotherapy of the conjunctival margins along with the application of Mitomycin C. The bare sclera was covered by amniotic membrane (Fig. 1b). The lesion was sent for histopathology. Postoperative recovery was uneventful. He was prescribed topical Mitomycin C (MMC) 0.04% as a surgical adjunct. The patient has been followed up for 2 months with no evidence of recurrence.
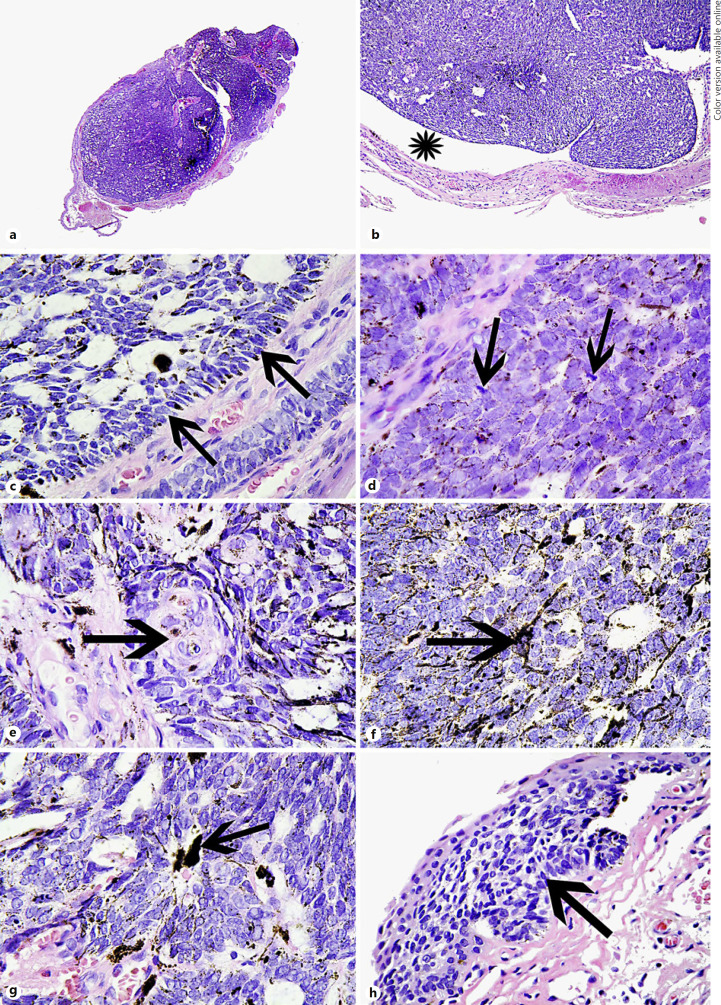
Histology showed a well-defined, mitotically active basaloid tumour, focally connected to the overlying epithelium (Fig. 2a). Between the tumour and surrounding stroma, artefactual clefts were present (Fig. 2b). The tumour cells were basaloid with a peripheral palisade (Fig. 2c), and the requisite cells were mitotically active (Fig. 2d) and some contained brown pigment in minimal cytoplasm (Fig. 2d). Focal squamous differentiation was identified (Fig. 2e). Pigmented dendritic melanocytes were diffusely present in the tumour (Fig. 2f) along with melanophages (Fig. 2g). Separate superficial tumour deposits were seen flanking the main lesion, connected to the under surface of the conjunctival epithelium (Fig. 2h).
Fig. 2.
a Haematoxylin and eosin (HE)-stained section at scanning power of the BCC. b Artefactual processing cleft between the BCC and background conjunctival stroma. c HE. A peripheral palisade where the cells are lined up parallel to one another (arrows). d HE of the tumour cells showing mitotically active (arrows) tightly packed basaloid cells. Many tumour cells contain brown pigment in their minimal cytoplasm. e HE showing focal squamous differentiation (arrow). f HE. Arrow points to a dendritic pigmented melanocyte within the tumour. g HE. Arrow points to a melanophage in the tumour. h HE. The arrow points to a superficial pattern BCC connected to the under surface of the conjunctival epithelium. This corresponds to the smaller pigmented nodules flanking the main tumour (see Fig. 1a).
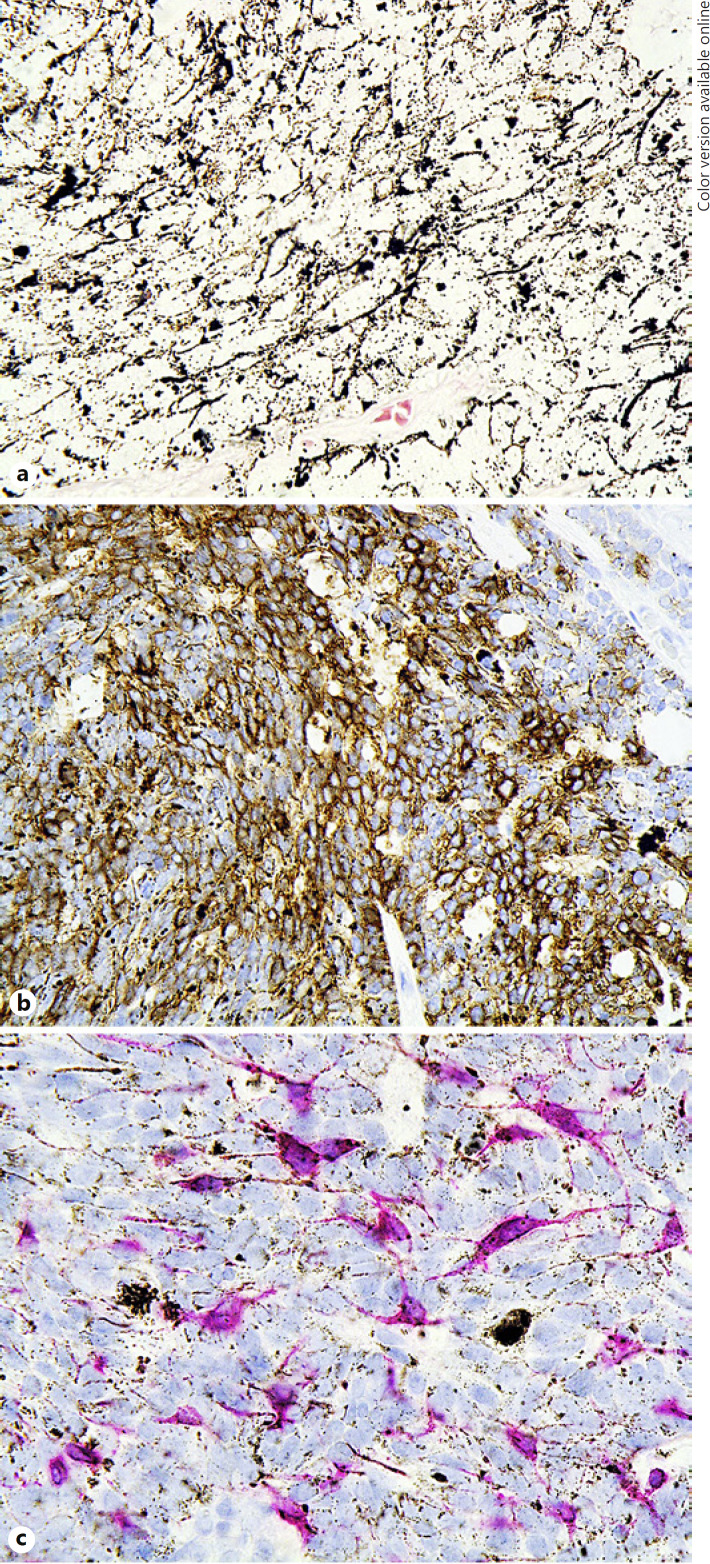
A Masson-Fontana stain confirmed the dense network of melanin granules present in the tumour (Fig. 3a). Immunohistochemistry showed that the basaloid cells were positive for BerEP4 (Fig. 3b) and BCL2 (not shown) and negative for EMA, CK20 and TTF1 (not shown). Melan A showed an evenly distributed population of spindle to dendritic, pigmented and non-pigmented melanocytes through the tumour (Fig. 3c) with the background epithelial cells not unstained. No lymphatic, blood vessel or perineural invasion was identified. There was no evidence of a primary melanocytic malignancy. The features were those of a conjunctival primary pigmented BCC of nodular type with a smaller superficial component. One peripheral margin was contaminated by tumour.
Fig. 3.
a Masson-Fontana stain indicating the extensive presence of melanin pigment in dendritic melanocytes in the BCC. b BerEP4 immunohistochemistry showing that the BCC stains positively (brown = positive staining). c Melan A immunohistochemistry showing cytoplasmic staining in intra-tumoral dendritic melanocytes (red = positive staining).
Discussion
We report a primary pigmented BCC of the left inferotemporal conjunctiva in a South-Asian male, which mimicked conjunctival melanoma clinically. It is far more common to observe BCC of the eyelid with secondary conjunctival involvement [7]. Rarer still are examples of primary caruncle BCC with secondary conjunctival involvement [8]. Primary BCC of the conjunctiva has only been reported on 4 previous occasions and none of these were of the pigmented variety [2, 3, 4, 5]. Table 1 summarises the features of these previously reported cases compared with the present case.
Table 1.
Details of the previous cases of primary conjunctival basal cell carcinoma of the conjunctiva, in relation to the present case
| Studies | Sex and age, Race years | Eye, L/R | Location on conjunctiva | Appearance | Histological diagnosis | Follow up data | |
|---|---|---|---|---|---|---|---|
| Aftab and Percival [2], 1973 | M, 82 | Unspecified | Unspecified | Nasally in the palpebral aperture between the limbus and the plica | Pedunculated, fleshy, mobile, 4 mm | BCC (type unspecified) with focal squamous differentiation | No recurrence for 2 months |
| Apte et al. [3], 1975 | F, 69 | Presumed South Asian | R | Nasally in the palpebral aperture between the limbus and the plica | Fleshy, pedunculated, 2 × 1.5 inches, mobile, and lobulated surface with irregular margin | BCC (type unspecified) | No recurrence, but period not specified |
| Husain et al. [4], 1993 | M, 66 | Not specified | L | Nasal limbus | Nodular, fleshy, vascular | BCC (type unspecified) with focal squamous differentiation | No recurrence for 12 months |
| Cable et al. [5], 2000 | M, 69 | Not specified | L | Temporal limbus | 6 × 6 mm, elevated nodule at the 3-o'clock position with overlying conjunctival hyperemia | BCC-morphoeic type | Intraocular invasion by BCC, no further follow-up data |
| Present case, 2019 | M, 60 | South Asian (Bangladeshi) | L | Temporal limbus 4 to 5 o'clock | Sessile, non-mobile, black hemispherical nodule with feeder vessels | Nodular and superficial BCC, focal squamous differentiation | No recurrence for 2 months |
M, male; F, female; L, left; R, right; BCC, basal cell carcinoma.
Regarding skin BCC, the pigmented variant accounts for 6% of all cases and presents in all BCC growth patterns. Melanin pigment can be present in melanocytes, melanophages and tumour cells [6]. There have been rare reports of colonisation of BCC by in situ melanoma [9], cutaneous melanoma metastasizing to BCC [10] and skin collision tumours of BCC and melanoma [11]. Brankov et al. [12] investigated pigmented skin BCC using immunohistochemistry with the melanocytic markers MART-1 and Melan A and established that “the mean melanocyte count per high powered field in pigmented BCCs from sun-exposed skin was 101.9 and from intermittently sun-exposed skin was 122.5, as compared to the controls (nodular non-pigmented BCC) of 27.4 (p = 0.002) and 34.9 (p = 0.002), respectively.” Therefore, they concluded that the pigmentation was attributable to increased melanin and to increased melanocytes [12]. In our case, melanin pigment was present in tumour cell cytoplasm, in dendritic melanocytes and in melanophages in the main nodular tumour and within the peripheral superficial component, identical to that reported in the skin. The melanocyte count per ×40 objective on an Olympus BX51 microscope was 98 melanocytes (counted over 3 × 40 fields), comparable to the melanocyte counts in pigmented skin BCC quoted above [12].
A key question relates to the pathogenesis of BCC in the conjunctiva. Possible mechanisms include (a) metaplasia of the conjunctival epithelium to epidermis or hair follicular type tissue with ultraviolet damage and induction of BCC; (b) BCC development within a dermoid choristoma; and (c) metastatic BCC from skin (eyelid and non-eyelid). The patient had no skin tumours, ruling out metastasis. This leaves the first two possibilities, with the first example more plausible because of the absence of a choristoma from the histopathology. Other conjunctival neoplasms that are known to mimic conjunctival melanoma are pigmented squamous cell carcinomas, which occurs in patients with brown or black skin [1]. Like our case of pigmented BCC, the pigment is found in some tumour cells but is mainly concentrated within dendritic intra-tumour melanocytes [1].
In summary, we report a unique case of pigmented primary conjunctival BCC, manifesting as a dark brown conjunctival tumour, resembling melanoma. We suggest that pigmented BCC be considered in the differential diagnosis of pigmented neoplasms of the conjunctiva.
Statement of Ethics
The study was conducted ethically in accordance with the World Medical Association's Declaration of Helsinki. The subject has given his written informed consent to publish his case (including publication of images).
Disclosure Statement
The authors have no conflicts of interest to declare.
Funding Sources
This study attracted no funding.
Author Contributions
H.S.M. wrote the paper and contributed the pathology figures. S.R.R. and F.H. were the surgeons and documented the case. M.N. wrote and edited the paper.
References
- 1.Shields CL, Manchandia A, Subbiah R, Eagle RC, Jr, Shields JA. Pigmented squamous cell carcinoma in situ of the conjunctiva in 5 cases. Ophthalmology. 2008 Oct;115((10)):1673–8. doi: 10.1016/j.ophtha.2008.01.020. [DOI] [PubMed] [Google Scholar]
- 2.Aftab M, Percival SP. Basal cell carcinoma of the conjunctiva. Br J Ophthalmol. 1973 Nov;57((11)):836–7. doi: 10.1136/bjo.57.11.836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Apte PV, Talib VH, Patil SD. Basal cell carcinoma of conjunctiva. Indian J Ophthalmol. 1975 Oct;23((3)):33–4. [PubMed] [Google Scholar]
- 4.Husain SE, Patrinely JR, Zimmerman LE, Font RL. Primary basal cell carcinoma of the limbal conjunctiva. Ophthalmology. 1993 Nov;100((11)):1720–2. doi: 10.1016/s0161-6420(93)31411-9. [DOI] [PubMed] [Google Scholar]
- 5.Cable MM, Lyon DB, Rupani M, Matta CS, Hidayat AA. Case reports and small case series: primary basal cell carcinoma of the conjunctiva with intraocular invasion. Arch Ophthalmol. 2000 Sep;118((9)):1296–8. doi: 10.1001/archopht.118.9.1296. [DOI] [PubMed] [Google Scholar]
- 6.Maloney ME, Jones DB, Sexton FM. Pigmented basal cell carcinoma: investigation of 70 cases. J Am Acad Dermatol. 1992 Jul;27((1)):74–8. doi: 10.1016/0190-9622(92)70160-h. [DOI] [PubMed] [Google Scholar]
- 7.Shields CL, Alset AE, Boal NS, Casey MG, Knapp AN, Sugarman JA, et al. Conjunctival Tumors in 5002 Cases. Comparative Analysis of Benign Versus Malignant Counterparts. The 2016 James D. Allen Lecture. Am J Ophthalmol. 2017 Jan;173:106–33. doi: 10.1016/j.ajo.2016.09.034. [DOI] [PubMed] [Google Scholar]
- 8.Østergaard J, Boberg-Ans J, Prause JU, Heegaard S. Primary basal cell carcinoma of the caruncle with seeding to the conjunctiva. Graefes Arch Clin Exp Ophthalmol. 2005 Jun;243((6)):615–8. doi: 10.1007/s00417-004-1086-5. [DOI] [PubMed] [Google Scholar]
- 9.Burkhalter A, White WL. Malignant melanoma in situ colonizing basal cell carcinoma. A simulator of invasive melanoma. Am J Dermatopathol. 1997 Jun;19((3)):303–7. doi: 10.1097/00000372-199706000-00019. [DOI] [PubMed] [Google Scholar]
- 10.Cowley GP, Gallimore A. Malignant melanoma metastasising to a basal cell carcinoma. Histopathology. 1996 Nov;29((5)):469–70. doi: 10.1046/j.1365-2559.1996.d01-518.x. [DOI] [PubMed] [Google Scholar]
- 11.de Almeida Barbosa A, Jr, Sales Guimarães N, de Lourdes Lopes M, Sadigursky M, Bittencourt M. Malignant melanoma and basal cell carcinoma in a combined tumour. Br J Dermatol. 1999 Feb;140((2)):360–1. doi: 10.1046/j.1365-2133.1999.02679.x. [DOI] [PubMed] [Google Scholar]
- 12.Brankov N, Prodanovic EM, Hurley MY. Pigmented basal cell carcinoma: increased melanin or increased melanocytes? J Cutan Pathol. 2016 Dec;43((12)):1139–42. doi: 10.1111/cup.12819. [DOI] [PubMed] [Google Scholar]