Abstract
Countries around the world are currently fighting the coronavirus disease 2019 (COVID-19) pandemic, which is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). SARS-CoV-2 is a betacoronavirus, belonging to the same genus as severe acute respiratory syndrome (SARS)-CoV and Middle East respiratory syndrome (MERS)-CoV. Currently, there are no proven antiviral therapies for COVID-19. Numerous clinical trials have been initiated to identify an effective treatment. One leading candidate is remdesivir (GS-5734), a broad-spectrum antiviral that was initially developed for the treatment of Ebola virus (EBOV). Although remdesivir performed well in preclinical studies, it did not meet efficacy endpoints in a randomized trial conducted during an Ebola outbreak. Remdesivir holds promise for treating COVID-19 based on in vitro activity against SARS-CoV-2, uncontrolled clinical reports, and limited data from randomized trials. Overall, current data are insufficient to judge the efficacy of remdesivir for COVID-19, and the results of additional randomized studies are eagerly anticipated. In this narrative review, we provide an overview of Ebola and coronavirus outbreaks. We then summarize preclinical and clinical studies of remdesivir for Ebola and COVID-19.
Keywords: COVID-19, pandemic, remdesivir, SARS-CoV-2
Background
For over two decades, global health leaders have been cautioning the world about another pandemic comparable in severity and scope to the 1918 influenza epidemic. 1 Two major outbreaks afflicted the world in the 20th century, that is, the 1918 influenza epidemic and the ongoing human immunodeficiency virus (HIV) pandemic. 2 The 21st century has already seen a significant number of outbreaks: severe acute respiratory syndrome coronavirus (SARS-CoV) in 2002, the Middle East respiratory syndrome coronavirus (MERS-CoV) in 2012, and the Ebola virus (EBOV) in 2014. Currently, we are in the midst of an unprecedented pandemic due to SARS-CoV-2, coronavirus disease 2019 (COVID-19). These outbreaks have posed many challenges: an important one being the public health aspect, but also the lack of effective therapies and vaccines. Prevention of complications and supportive treatment are the standard of care for most of these recent viral disease outbreaks. 3 No treatment has been proven effective for the current COVID-19 pandemic. The medical community is under immense pressure, and many clinicians are embarking on using experimental treatments based on poorly conducted clinical trials and observational data. 4 Randomized controlled trials conducted efficiently and promptly are the only way to find effective therapies.
Remdesivir (GS-5734) is an investigational broad-spectrum antiviral drug that has demonstrated activity against ribonucleic acid (RNA) viruses of several families, including Coronaviridae (such as SARS-CoV, MERS-CoV, and strains of bat coronaviruses), Paramyxoviridae (such as Nipah virus, respiratory syncytial virus, and Hendra virus), and Filoviridae (such as EBOV). 5–9 In this narrative review, we will summarize the studies available to date for remdesivir in the context of viral outbreaks, especially its development as an antiviral agent for Ebola and coronaviruses. We searched PubMed for published clinical and preclinical reports assessing remdesivir for Ebola virus disease (EVD), SARS, MERS, and COVID-19. The search terms used were (‘Ebola virus’, ‘severe acute respiratory syndrome’, ‘SARS-CoV’, ‘Middle East respiratory syndrome’, ‘MERS-CoV’, ‘COVID-19’, ‘2019-nCoV’, ‘SARS-CoV-2’) and (‘remdesivir’ or ‘GS-5734’). The references of the selected papers were reviewed to identify additional pertinent reports.
Overview of human coronavirus outbreaks
Coronaviruses are large, enveloped, positive-strand RNA viruses that can be divided into four genera: alphacoronavirus, betacoronavirus, deltacoronavirus and gammacoronavirus. 10 Alpha and beta CoV are known to cause human disease. Until recently, human coronavirus (HCoV) received relatively less attention as they were considered low-virulence organisms and believed to cause only mild, self-limiting upper respiratory infection in humans.11,12
The first coronavirus outbreak, SARS, caused by SARS-CoV, occurred in the Guangdong Province of China in 2002–2003. The mortality rate during this outbreak was 9%, with a higher mortality rate (50%) in the elderly population. This outbreak was largely contained because of relatively inefficient transmission, which mainly occurred through direct contact with infected individuals. Hence, strict quarantine of infected patients restricted the spread of the disease, and the outbreak ceased after affecting 8098 people and causing death in 774 patients. 13
The next coronavirus outbreak occurred in the Middle East (Saudi Arabia) in 2012 and was named the MERS-CoV. This virus caused severe lower respiratory infection with a mortality rate of about 35%. Per the World Health Organization’s (WHO) report, the total number of reported cases globally was 2519, out of which 866 patients died. 13 Both MERS-CoV and SARS-CoV originated from bats. However, serologic studies for antibody testing in dromedary camels suggested that camels were the intermediate host for MERS-CoV. 14
MERS-CoV shared many clinical features with SARS-CoV, such as severe atypical pneumonia. However, there were some differences, with MERS causing prominent gastrointestinal (GI) symptoms and acute kidney injury. The investigators attributed the differences in clinical manifestations to the involvement of different receptors used by these two viruses. While MERS binds to the human dipeptidyl peptidase receptor (present in the lower airway, GI tract, and kidney), SARS binds to the angiotensin-converting enzyme (ACE)-2 receptor.12,13 The treatments for these coronavirus outbreaks largely relied on supportive care.
On December 31, 2019, China reported a cluster of atypical pneumonia cases with an unknown etiology. 15 Early cases were associated with the Huanan Seafood Wholesale Market in Wuhan, Hubei Province. Soon after that, the causative pathogen was identified as a novel betacoronavirus (SARS-CoV-2), and the disease was ultimately named COVID-19. SARS-CoV-2 has high sequence homology with bat coronaviruses (~87% identical sequences with bat-SL-CoVZC45 and bat-SL-CoVZXC21), which supports the hypothesis of bat origin. When compared with SARS-CoV and MERS-CoV, SARS-CoV-2 has a genetic similarity of 79 and 50%, respectively. 13 The clinical presentation of COVID-19 ranges from asymptomatic carriage to severe viral pneumonia causing acute respiratory distress syndrome. Fever and GI symptoms are common. At the time of this report, COVID-19 has spread across the globe with 2,397,216 confirmed cases and 162,956 deaths according to the WHO situation report. 16
Overview of Ebola virus outbreaks
Ebola viruses belong to the family Filoviridae, a taxonomic group of enveloped, non-segmented, negative-strand RNA viruses. There are five different species of EBOV that can infect humans, but they differ in their virulence and disease progression, with a case fatality rate ranging from 40% for Bundibugyo EBOV to 70–90% for Zaire EBOV. Humans infected with EBOV initially have non-specific symptoms, such as nausea, vomiting, and diarrhea, with the hemorrhagic phase occurring in half of the cases. 17 Outbreaks of EVD have mainly been limited to Africa; however, in recent times, a small number for patients have been transferred to hospitals with modern technology in the USA and Germany. The mortality rate in Africa is often very high compared to patients who have received supportive care in developed countries. There are no approved drugs for the treatment of EVD. During the 2014–2016 West African outbreak and subsequent outbreak in the Democratic Republic of Congo (DRC), several investigational treatments, such as antibody therapy and remdesivir, were evaluated in clinical trials. 18
In summary, it has been challenging to evaluate investigational drugs in randomized controlled trials during outbreak situations. The initial response to the COVID-19 outbreak was to use treatments that were not shown to be effective in properly conducted trials. Most studies thus far have lacked adequate controls, are observational, and have a very small number of patients that precludes any meaningful statistics regarding efficacy. Here, we review the available studies for the antiviral remdesivir (Gilead Sciences, Inc.) in an attempt to present an impartial review of data available for this drug, with a specific focus on outbreaks of EBOV and now SARS-CoV-2.
Chemistry and pharmacology of remdesivir
Remdesivir (previously GS-5734; chemical formula C27H35N6O8P) is a monophosphoramidate prodrug of a C-adenosine nucleoside analogue (Figure 1). 19–21 Remdesivir terminates viral RNA synthesis by inhibiting viral RNA-dependent RNA polymerase (RdRp). The active form, remdesivir triphosphate, competes with native adenosine triphosphate for chain inclusion, resulting in delayed chain termination. 22 Remdesivir displays linear pharmacokinetics and a prolonged intracellular half-life (>35 hours for the active parent triphosphate). Remdesivir triphosphate was found to accumulate in peripheral blood mononuclear cells, suggesting a loading dose that could accelerate the achievement of a steady state. 23 These characteristics support the dosing regimen used in clinical studies to date: 200 mg intravenously on the first day, followed by 100 mg intravenously once daily (5–10 days total). Detailed information regarding remdesivir metabolism and elimination is unavailable. 23
Figure 1.
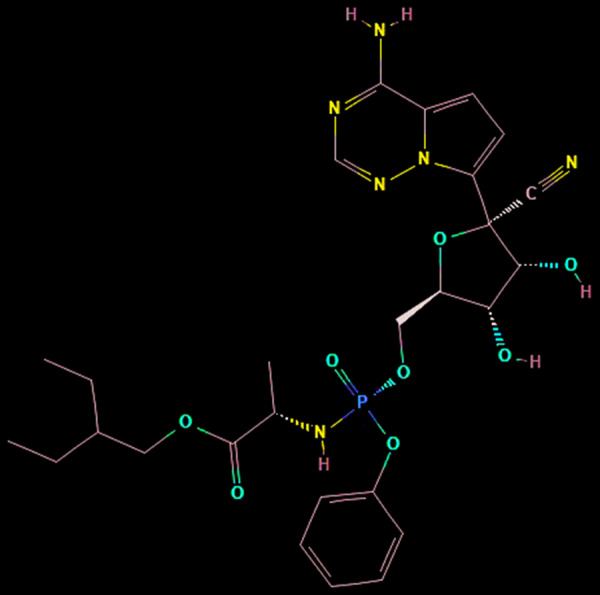
Chemical structure of remdesivir.21
Source: US National Library of Medicine.
Antiviral activity
Remdesivir exhibits broad in vitro antiviral action against zoonotic and human pathogens from multiple virus families (Table 1). Remdesivir’s activity has been consistent when tested against members of the Filoviridae, Paramyxoviridae, Pneumoviridae, and Coronaviridae. 6 Among HCoV, remdesivir inhibits three of the endemic strains associated with respiratory illness (HCoV-OC43, 229E, and NL63) as well as the less common MERS-CoV, SARS-CoV, and novel SARS-CoV-2.7–9,24 In addition, remdesivir possesses activity against SARS-like and MERS-like bat coronaviruses (HKU3, WIV1, SHC014, and HKU5). 7 Although most preclinical research has been in vitro, remdesivir was also effective in non-human primate (NHP) models of MERS, Nipah virus infection, and EVD.5,25,26
Table 1.
Broad in vitro activity of remdesivir against human viral pathogens.
| Virus | EC50 (μM) |
|---|---|
| Filoviridae6,19 | |
| Ebola | 0.003–0.09 |
| Marburg | 0.01–0.02 |
| Paramyxoviridae6 | |
| Nipah | 0.03–0.05 |
| Hendra | 0.06 |
| Parainfluenza type 3 | 0.02 |
| Measles | 0.04 |
| Pneumoviridae6 | |
| Respiratory syncytial virus | 0.02 |
| Human metapneumovirus | 0.73a |
| Coronaviridae7–9,24 | |
| HCoV-OC43 | 0.15 |
| HCoV-229E | 0.02 |
| HCoV-NL63 | See commentb |
| MERS-CoV | 0.07–0.12 |
| SARS-CoV | 0.07 |
| SARS-CoV-2 | 0.77 |
Tested against parent compound of remdesivir;
in an in vitro model, a 3 log10 reduction in viral replication was observed at 0.1 μM.
EC50: Half maximal effective concentration, HCoV, human coronavirus; MERS-CoV, Middle East respiratory syndrome coronavirus; SARS-CoV, severe acute respiratory syndrome coronavirus.
Remdesivir is less potent against the Flaviviridae, with moderate activity against Hepatitis C, Dengue, and Yellow Fever viruses. 6 Remdesivir has poor-to-negligible activity against tick-borne flaviviruses (Alkhurma hemorrhagic fever, Kyasanur forest disease, Omsk hemorrhagic fever, tick-borne encephalitis) and West Nile, Lassa, vesicular stomatitis, Rift Valley fever, and Crimean–Congo hemorrhagic fever viruses. 6
Remdesivir for Ebola
Preclinical data
Remdesivir was first identified during a broad screening for compounds with activity against emerging viruses. 19 The original screening program was primarily geared toward identifying candidates that could inhibit RNA viruses, namely Coronaviridae and Flaviviridae. Subsequent to the 2013–2016 EVD outbreak in West Africa, some previously screened compounds were further investigated against EBOV. Remdesivir was observed to have high potency against EBOV across multiple cell lines, with an anti-EBOV half maximal effective concentration (EC50) of 0.086 μM in human macrophages. Remdesivir was chosen for continued clinical development based upon its potency and a chemical structure amenable to rapid scale-up. 19 The first in vivo efficacy evaluation was completed in an non-human primate (NHP) model of EVD. 5 In the NHP EVD model, previously healthy rhesus monkeys received an intramuscular inoculation of EBOV, which results in death after a clinical course mimicking human EVD. NHP was challenged with EBOV followed by receipt of various remdesivir dosing regimens. The time from inoculation to remdesivir initiation varied between study groups (as soon as 30 minutes after viral challenge and up to 3 days after viral challenge). Lower doses (3 mg/kg daily) demonstrated a measurable antiviral effect with survival rates between 33 and 66%. However, higher doses were most promising, with 6/6 NHP surviving after receiving remdesivir 10 mg/kg daily starting on day 3. This was the first report of a molecule providing post-exposure protection from EVD and supported the further evaluation of remdesivir in human EVD.
Clinical efficacy
A limited number of case reports described the use of remdesivir for EVD through emergency compassionate use protocols prior to the completion of formal clinical trials.27,28 The first case described the use of remdesivir for EBOV meningoencephalitis in a 39-year-old woman who had fully recovered from an episode of EVD 9 months earlier. The second case involved an infant diagnosed with EVD on her first day of life following birth from an EBOV-positive mother. 28 Although both patients in these reports survived, it is difficult to make conclusions regarding the role remdesivir played in their recovery as multiple therapies were administered.
A randomized multi-intervention trial was later conducted during the EVD outbreak in the DRC. 18 Patients of any age, including pregnant women, were eligible for enrollment if they tested positive for EBOV. Patients received standard supportive care along with an assignment to one of four treatment arms in a 1:1:1:1 ratio. Study treatments included ZMapp (a triple monoclonal antibody), MAb114 (a single human monoclonal antibody derived from an Ebola survivor), REGN-EB3 (a mixture of three human immunoglobulin G1 [IgG1] monoclonal antibodies), and intravenous remdesivir. Remdesivir was administered at a dose of 200 mg on day 1, followed by 100 mg daily for 9–13 days. Weight-based doses were used for pediatric patients. The primary outcome was mortality at day 28. Nearly 700 patients had been randomized when an interim analysis led to early cessation of the trial. The data and safety monitoring board found higher mortality in the ZMapp and remdesivir groups compared to the MAb114 and REGN-EB3 groups. Further, the REGN-EB3 group had met a prespecified threshold for efficacy. A total of 673 patients were included in the final analysis. The mean age of enrolled patients was 29 years and 56% of patients were women (6% of whom were pregnant). At day 28, mortality rates were: remdesivir (53.1%), ZMapp (49.7%), MAb114 (35.1%), and REGN-EB3 (33.5%). For remdesivir, 85 and 29% of patients with high- and low-viral loads at baseline died, respectively.
In summary, despite potent in vitro activity against EBOV and unprecedented success in animal models of EVD, the journey of remdesivir for human EVD culminated in disappointing results.
Remdesivir for COVID-19
Preclinical data
Remdesivir was known to inhibit the replication of coronaviruses prior to the emergence of SARS-CoV-2. Wang and colleagues published the first report affirming that remdesivir, among other existing antivirals, could effectively inhibit SARS-CoV-2 replication. 29 The investigators evaluated the activity of seven drugs against SARS-CoV-2 in the non-human Vero E6 cells: ribavirin, penciclovir, nitazoxanide, nafamostat, chloroquine, favipiravir, and remdesivir. The EC50 was lowest for remdesivir (0.77 μM), followed by chloroquine (1.13 μM). A simulated molecular docking experiment also predicted remdesivir would bind to SARS-CoV-2 RdRp with high affinity. 30 A number of factors have led to the public and medical interest in remdesivir for the treatment of SARS-CoV-2 in recent times. First, in vitro activity against SARS-CoV-2 has been confirmed. Second, remdesivir has an established dosing and safety profile. Finally, effective treatments for COVID-19 are desperately needed.
Clinical efficacy
As the COVID-19 pandemic spread, Gilead Sciences, Inc. facilitated emergency access to remdesivir through a compassionate use program for patients with severe disease and no access to a clinical trial. Individual requests for compassionate use have since been halted in favor of a newly expanded access program (exception: compassionate use requests for pregnant women and children <18 years old are still accepted). 31 The initial clinical efficacy data for remdesivir in COVID-19 have centered on the case reports wherein patients received remdesivir through the compassionate use process. All cases described received remdesivir 200 mg intravenously on day 1, followed by 100 mg for up to 9 more days.
The first patient diagnosed with COVID-19 in the United States was treated with remdesivir. 32 The patient was a 35-year-old man with a limited past medical history and recent travel to Wuhan, China. He was admitted to a hospital for airborne isolation and monitoring. Remdesivir was initiated on hospital day 7 due to increasing oxygen requirements and ongoing pyrexia. The patient improved the following day, and was mostly asymptomatic at the time the report was published. A more recent report describes the use of remdesivir in a 40-year-old man who was hospitalized with severe COVID-19 requiring mechanical ventilation. 33 Remdesivir was not started until day 13 of illness. The patient was extubated 72 hours later, and a full recovery was expected at the time of publication. The authors hypothesize that remdesivir may retain a therapeutic effect even when started late in a disease course. A non-peer reviewed manuscript is available that describes the outcomes of the first 12 patients in the United States with COVID-19. 34 Three patients received remdesivir and all 12 patients clinically recovered. Retrospective cohort studies have been published detailing COVID-19 outcomes in patients requiring extracorporeal membrane oxygenation (ECMO) and those with a history of solid organ transplant.35,36 In the ECMO cohort, 3/5 survivors received remdesivir and 1/10 non-survivors received remdesivir. In the transplant cohort, only 2/90 patients received remdesivir and their specific outcomes were not reported.
Grein and colleagues recently reported their experience with the compassionate use of remdesivir for COVID-19 in a multicenter open label cohort that enrolled 61 patients (of note, this analysis included previously reported cases). 37 Compassionate use approvals were reserved for hospitalized patients with an oxygen saturation of ≤94% on room air or the need for oxygen support. Patients were required to have a creatinine clearance (CrCl) greater than 30 mL/min and hepatic transaminases less than five times the upper limit of normal. There were no predefined endpoints or enrollment goals. A total of 53 patients were included in the final analysis (8 patients were excluded due to missing or erroneous data). The median age was 64 years and 64% of patients were receiving invasive ventilation at baseline (including 7% receiving ECMO). The median time from symptom onset to remdesivir initiation was 12 days. After starting remdesivir, 36 of 53 patients (68%) showed improvement based on their level of oxygen support. Of those receiving invasive mechanical ventilation, 17/30 (57%) were extubated. Three out of four patients (75%) receiving ECMO were able to stop ECMO. Seven (13%) patients died. The risk of death was increased in patients who were ≥70 years of age, those with higher serum creatinine, and those requiring invasive ventilation. The authors suggest the 13% mortality rate is noteworthy given previously reported mortality rates of 17–78% in severe COVID-19. Unfortunately, conclusions regarding the clinical effect of remdesivir are hampered by the lack of a control group and delay in initiation of therapy. Additionally, the direct antiviral effect of remdesivir was not assessed with viral load measurements. The sample size was small, and a substantial proportion of patients given remdesivir were eventually excluded from analysis (8/61, 13%).
Finally, 4 months into the disease, the data from randomized trials are beginning to emerge. One of the first randomized, placebo-controlled, double-blind study in severe COVID-19 was released at the time of manuscript preparation, (NCT04257656, Table 2). 38 Wang and colleagues randomized hospitalized patients with severe COVID-19 in a 2:1 allocation to remdesivir (n=158) to matching placebo (n=78). 38 Remdesivir was given in the dose of 200 mg on day 1 followed by 100 mg daily on days 2–10. The primary endpoint was time to clinical improvement, defined as a two-point reduction in disease severity on a six-point ordinal scale. The baseline characteristics though largely balanced had higher proportion of patients with medical comorbidities and presenting later than 10 days with higher respiratory rate. At baseline, most patients required supplemental oxygen, but not mechanical ventilation. In the efficacy analysis, time to clinical improvement was similar between groups (median 21 days in the remdesivir group versus 23 days with placebo; hazard ratio [HR]: 1.23 [95% confidence interval (CI): 0.87–1.75]). Mortality at 28 days was also similar between groups (22 [14%] died in the remdesivir group versus 10 [13%] with placebo). SARS-CoV-2 RNA loads were not reduced with remdesivir compared to placebo. The trial was halted before target enrollment was reached as the COVID-19 outbreak subsided in the study region. As such, the statistical power was reduced from a planned 80 to 58%, and the study remained inconclusive.
Table 2.
Ongoing randomized trials for remdesivir registered on ClinicalTrials.gov.
| Identifier | Design | Population and Locations | Interventiona | Primary Outcome | Status |
|---|---|---|---|---|---|
| NCT04257656 | Randomized, double-blind, placebo-controlled | Severe COVID-19 (Hospitalized with a SaO2/SpO2 ≤ 94% on room air or PaO2/FiO2 ratio < 300 mgHg), cannot have eGFR ≤ 30 mL/min; China | Remdesivir for 10 days versus placebo | Time to clinical improvement | April 15, 2020: Terminated; currently no eligible patients due to control of the pandemic38 |
| NCT04252664 | Randomized, double-blind, placebo-controlled | Mild-to-moderate COVID-19 (Hospitalized with fever plus cough or respiratory rate > 24 breaths/min, and not meeting criteria for severe disease given earlier), cannot have eGFR ≤ 30 mL/min; China | Remdesivir for 10 days versus placebo | Time to clinical recovery | April 15, 2020: Suspended; currently no eligible patients due to control of the pandemic39 |
| NCT04292899 | Randomized, open-label trial | Severe COVID-19 (SpO2 ≤ 94% or requiring supplemental oxygen). Cannot be intubated at screening or have CrCl < 50 mL/min; Multiple countries worldwide | Remdesivir for 5 days versus 10 days | Odds ratio for improvement | Recruiting |
| NCT04292730 | Randomized, open-label | Moderate COVID-19 (SpO2 > 94% on room air with pulmonary infiltrates. Cannot be intubated or have CrCl < 50 mL/min); Multiple countries worldwide | Remdesivir for 5 days versus 10 days versus standard therapy | Odds ratio for improvement | Recruiting |
| NCT04280705 | Randomized, double-blind, placebo-controlled, adaptive | Hospitalized with COVID-19 and one of the following: radiographic infiltrates, rales/crackles, and SpO2 > 94% on room air, requires oxygen or mechanical ventilation. Cannot have CrCl < 50 mL/min.; Multiple countries worldwide | Remdesivir for 10 days versus placebo | Clinical status at day 15 | Recruiting |
| NCT04321616 | Randomized open-label, adaptive | Admitted to hospital ward or intensive care unit with COVID-19. Excluded if baseline QTc > 450 ms; Norway | Remdesivir for 10 days versus hydroxychloroquineb for 10 days versus placebo | In-hospital mortality | Recruiting |
| NCT04315948 | Randomized, open-label, adaptive | Hospitalized with COVID-19 and one of the following: rales/crackles and SpO2 > 94% on room air, requires oxygen or mechanical ventilation. Cannot have eGFR < 30 mL/min; France | Treatment arms include remdesivir for 10 days, lopinavir/ritonavirc for 14 days, lopinavir/ritonavir for 14 days plus interferon beta-1a 44 mcg subcutaneously on days 1, 3, and 6, hydroxychloroquined for 10 days, or standard care | Clinical status at day 15 | Recruiting |
For all studies, remdesivir is given as 200 mg intravenously on day 1, followed by 100 mg daily on subsequent days;
hydroxychloroquine 800 mg twice daily for 1 day, then 400 mg twice daily;
lopinavir/ritonavir 400 mg/100 mg twice daily;
hydroxychloroquine 400 mg twice daily for 1 day, then 400 mg once daily.
COVID-19, coronavirus disease 2019; CrCl, creatinine clearance; eGFR, estimated glomerular filtration rate.
While the results of the study from China are inconclusive, the preliminary results of the first randomized controlled study from the USA conducted under the auspices of the National Institute of Allergy and Infectious Disease, Adaptive COVID-19 Treatment Trial have also been released (NCT04280705, Table 2) on the same day through a press release. 39 Although full data release is awaited, the preliminary analysis of over 1063 enrollments showed that the median time to recovery was shorter in those who treated with remdesivir compared to those treated with placebo (11 days versus 15 days, p<0.001). The results also showed a trend toward survival benefit with remdesivir (mortality of 8% in remdesivir arm versus 11.6% in placebo, p=0.059). In absence of details, it is also uncertain as to what proportion of the population received treatment with additional therapeutic agents for COVID-19. Finally, in another press release, Gilead Sciences Inc. summarized results of an open-label study comparing the treatment regimen of 5 versus 10 days of remdesivir for severe COVID-19 (NCT04292899, Table 2). 40 Clinical improvement was similar with either regimen; however, lack of placebo arm and limitation of the study details prohibit meaningful conclusions.
Together, these reports suggest a promising role for remdesivir for COVID-19, though its effects on hard outcomes, including mortality, are still pending. Release of the full reports of these recently reported randomized studies and of the ongoing studies referenced in Table 2 will be needed to judge the true efficacy and safety of remdesivir for COVID-19.
Safety profile
Remdesivir has a low affinity for human RNA Polymerase II and human mitochondrial RNA polymerase, which is expected to contribute to a favorable safety profile in humans. 22 Safety was initially evaluated in phase one of the dose-ranging studies. 23 Single doses from 3 to 225 mg were well tolerated with no observed toxicities. Multiple administrations of remdesivir 150 mg for 7 or 14 days led to reversible grade 1 and 2 alanine aminotransferase (ALT) and aspartate transaminase (AST) elevations. Remdesivir is not considered to have reproductive or developmental toxicity. Remdesivir injection is formulated with sulfobutylether-β-cyclodextrin (SBECD). 41 Other drug products formulated with SBEDC, such as intravenous voriconazole, carry warnings for SBECD accumulation in patients with renal dysfunction. 41 However, the clinical significance of vehicle accumulation is unclear. 42 Patients with CrCl < 30 mL/min have been excluded from remdesivir compassionate use and expanded access protocols thus far. 31 Some ongoing clinical trials (Table 2) are excluding patients with CrCl ≤ 50 mL/min.
In the open-label COVID-19 compassionate use cohort, 37 32/53 (60%) patients reported adverse events, while 4/53 (8%) experienced adverse events leading to discontinuation. The most common adverse events were increased hepatic enzymes, diarrhea, rash, and renal impairment. This constellation of events is difficult to interpret as there is a significant overlap with clinical attributes of severe COVID-19. No new safety concerns were noted in the published COVID-19 randomized trial. Adverse events leading to drug discontinuation occurred in 18 (12%) remdesivir patients and 4 (5%) placebo patients. 38 Reported adverse events were uncommon in the landmark EVD trial. The full toxicity profile will be further elucidated as results emerge from additional placebo-controlled trials in COVID-19.
Looking forward
There are currently seven randomized trials involving remdesivir registered on ClinicalTrials.gov (Table 2). Two of these trials, both conducted in China (NCT04257656 and NCT04252664), were recently terminated or suspended. The information posted to ClinicalTrials.gov indicates difficulty enrolling subjects as the COVID-19 pandemic has come under control in the region. Of the two halted studies, results have only been released for NCT04257656, as described earlier. 38 The remaining active trials include comparisons with placebo, active comparators (e.g., hydroxychloroquine and lopinavir/ritonavir), short (5 days) versus long (10 days) remdesivir regimens, and patients with moderate-to-severe COVID-19.
Conclusion
Infectious disease outbreaks have shaped the course of human history, and with every new outbreak come new challenges. Today, scientists and clinicians around the globe are fighting to halt the COVID-19 pandemic. A chief concern remains: there are no antiviral treatments proven to be effective in fully published, peer-reviewed, randomized placebo-controlled trials. Remdesivir has emerged as a promising candidate based on its in vitro activity against SARS-CoV-2, uncontrolled clinical reports, and limited data from randomized trials. However, expectations should be tempered based on lessons from the past. Remdesivir has potent in vitro activity against EBOV, and was highly efficacious in an animal model of EVD. Unfortunately, early hopes for a new paradigm in EVD management were deflated with the completion of the first randomized trial. Remdesivir holds promise for COVID-19, but the first published randomized trial was underpowered and inconclusive. High-quality data are still lacking at this time. Thus, clinicians across the world now eagerly await complete results from additional randomized trials in COVID-19. Will remdesivir deliver?
Acknowledgements
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
Footnotes
Contributions: All authors contributed equally to the preparation of this review. Joe Pardo and Asmita Gupte were involved in the organization, review and critique of the manuscript. Ashutosh Shukla was involved in the conception, execution, review and critique of the manuscript. Gajapathiraju Chamarthi was involved in the review and critique of the manuscript. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosure and potential conflicts of interest: The authors declare that they have no conflicts of interest. The International Committee of Medical Journal Editors (ICMJE) Potential Conflicts of Interests form for the authors is available for download at: https://www.drugsincontext.com/wp-content/uploads/2020/05/dic.2020-4-14-COI.pdf
Funding declaration: Ashutosh M Shukla reports ongoing grant support from the Department of Veterans Affairs, Clinical Science Research and Development and Health Services Research and Developments.
Correct attribution: Copyright © 2020 Pardo J, Shukla AM, Chamarthi G, Gupte A. https://doi.org/10.7573/dic.2020-4-14. Published by Drugs in Context under Creative Commons License Deed CC BY NC ND 4.0.
Provenance: submitted; externally peer reviewed.
Peer review comments to author: 30 April 2020
Drugs in Context is published by BioExcel Publishing Ltd. Registered office: Plaza Building, Lee High Road, London, England, SE13 5PT.
BioExcel Publishing Limited is registered in England Number 10038393. VAT GB 252 7720 07.
For all manuscript and submissions enquiries, contact the Editor-in-Chief gordon.mallarkey@bioexcelpublishing.com
For all permissions, rights and reprints, contact David Hughes david.hughes@bioexcelpublishing.com
References
- 1.Gates B. Responding to Covid-19 - a once-in-a-century pandemic? N Engl J Med. 2020 doi: 10.1056/NEJMp2003762. [DOI] [PubMed] [Google Scholar]
- 2.Gates B. The next epidemic--lessons from Ebola. N Engl J Med. 2015;372(15):1381–1384. doi: 10.1056/NEJMp1502918. [DOI] [PubMed] [Google Scholar]
- 3.Bhimraj A, Morgan RL, Shumaker AH, et al. Infectious Diseases Society of America guidelines on the treatment and management of patients with COVID-19. Infectious Disease Society of America; 2020. https://www.idsociety.org/COVID19guidelines. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goodman JL, Borio L. Finding effective treatments for COVID-19: scientific integrity and public confidence in a time of crisis. JAMA. 2020 doi: 10.1001/jama.2020.6434. [DOI] [PubMed] [Google Scholar]
- 5.Warren TK, Jordan R, Lo MK, et al. Therapeutic efficacy of the small molecule GS-5734 against Ebola virus in rhesus monkeys. Nature. 2016;531(7594):381–385. doi: 10.1038/nature17180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lo MK, Jordan R, Arvey A, et al. GS-5734 and its parent nucleoside analog inhibit Filo-, Pneumo-, and Paramyxoviruses. Sci Rep. 2017;7:43395. doi: 10.1038/srep43395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sheahan TP, Sims AC, Graham RL, et al. Broad-spectrum antiviral GS-5734 inhibits both epidemic and zoonotic coronaviruses. Sci Transl Med. 2017;9(396) doi: 10.1126/scitranslmed.aal3653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sheahan TP, Sims AC, Leist SR, et al. Comparative therapeutic efficacy of remdesivir and combination lopinavir, ritonavir, and interferon beta against MERS-CoV. Nat Commun. 2020;11(1):222. doi: 10.1038/s41467-019-13940-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brown AJ, Won JJ, Graham RL, et al. Broad spectrum antiviral remdesivir inhibits human endemic and zoonotic deltacoronaviruses with a highly divergent RNA dependent RNA polymerase. Antiviral Res. 2019;169:104541. doi: 10.1016/j.antiviral.2019.104541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Woo PC, Lau SK, Huang Y, Yuen KY. Coronavirus diversity, phylogeny and interspecies jumping. Exp Biol Med (Maywood) 2009;234(10):1117–1127. doi: 10.3181/0903-MR-94. [DOI] [PubMed] [Google Scholar]
- 11.Amirian ES, Levy JK. Current knowledge about the antivirals remdesivir (GS-5734) and GS-441524 as therapeutic options for coronaviruses. One Health. 2020;9:100128. doi: 10.1016/j.onehlt.2020.100128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Paules CI, Marston HD, Fauci AS. Coronavirus infections-more than just the common cold. JAMA. 2020 doi: 10.1001/jama.2020.0757. [DOI] [PubMed] [Google Scholar]
- 13.Rabaan AA, Al-Ahmed SH, Haque S, et al. SARS-CoV-2, SARS-CoV, and MERS-COV: a comparative overview. Infez Med. 2020;28(2):174–184. [PubMed] [Google Scholar]
- 14.Memish ZA, Cotten M, Meyer B, et al. Human infection with MERS coronavirus after exposure to infected camels, Saudi Arabia, 2013. Emerg Infect Dis. 2014;20(6):1012–1015. doi: 10.3201/eid2006.140402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Holshue ML, DeBolt C, Lindquist S, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382(10):929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organization. Coronavirus disease 2019 (COVID-19) situation report 92. [Accessed April 21, 2020]. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
- 17.Feldmann H. Ebola--a growing threat? N Engl J Med. 2014;371(15):1375–1378. doi: 10.1056/NEJMp1405314. [DOI] [PubMed] [Google Scholar]
- 18.Mulangu S, Dodd LE, Davey RT, Jr, et al. A randomized, controlled trial of Ebola virus disease therapeutics. N Engl J Med. 2019;381(24):2293–2303. doi: 10.1056/NEJMoa1910993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Siegel D, Hui HC, Doerffler E, et al. Discovery and synthesis of a phosphoramidate prodrug of a pyrrolo[2,1-f][triazin-4-amino] adenine C-nucleoside (GS-5734) for the treatment of Ebola and emerging viruses. J Med Chem. 2017;60(5):1648–1661. doi: 10.1021/acs.jmedchem.6b01594. [DOI] [PubMed] [Google Scholar]
- 20.Ko WC, Rolain JM, Lee NY, et al. Arguments in favour of remdesivir for treating SARS-CoV-2 infections. Int J Antimicrob Agents. 2020 doi: 10.1016/j.ijantimicag.2020.105933. 105933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.2D structure image of remdesivir. [Accessed April 17, 2020]. PubChem Identifier: 121304016. https://pubchem.ncbi.nlm.nih.gov/compound/Remdesivir#section=2D-Structure.
- 22.Tchesnokov EP, Feng JY, Porter DP, Gotte M. Mechanism of inhibition of Ebola virus RNA-dependent RNA polymerase by remdesivir. Viruses. 2019;11(4) doi: 10.3390/v11040326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Summaries of evidence from selected experimental therapeutics as of October 2018. Appendix 4. [Accessed April 17, 2020]. https://www.who.int/ebola/drc-2018/summaries-of-evidence-experimental-therapeutics.pdf?ua=1.
- 24.Agostini ML, Andres EL, Sims AC, et al. Coronavirus susceptibility to the antiviral remdesivir (GS-5734) is mediated by the viral polymerase and the proofreading exoribonuclease. mBio. 2018;9(2) doi: 10.1128/mBio.00221-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.de Wit E, Feldmann F, Cronin J, et al. Prophylactic and therapeutic remdesivir (GS-5734) treatment in the rhesus macaque model of MERS-CoV infection. Proc Natl Acad Sci U S A. 2020;117(12):6771–6776. doi: 10.1073/pnas.1922083117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lo MK, Feldmann F, Gary JM, et al. Remdesivir (GS-5734) protects African green monkeys from Nipah virus challenge. Sci Transl Med. 2019;11(494) doi: 10.1126/scitranslmed.aau9242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jacobs M, Rodger A, Bell DJ, et al. Late Ebola virus relapse causing meningoencephalitis: a case report. Lancet. 2016;388(10043):498–503. doi: 10.1016/S0140-6736(16)30386-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dornemann J, Burzio C, Ronsse A, et al. First newborn baby to eceive experimental therapies survives Ebola virus disease. J Infect Dis. 2017;215(2):171–174. doi: 10.1093/infdis/jiw493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang M, Cao R, Zhang L, et al. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 2020;30(3):269–271. doi: 10.1038/s41422-020-0282-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Elfiky AA. Ribavirin, remdesivir, sofosbuvir, galidesivir, and tenofovir against SARS-CoV-2 RNA dependent RNA polymerase (RdRp): a molecular docking study. Life Sci. 2020 doi: 10.1016/j.lfs.2020.117592. 117592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gilead Sciences. Emergency access to remdesivir outside of clinical trials. [Accessed April 17, 2020]. https://www.gilead.com/purpose/advancing-global-health/covid-19/emergency-access-to-remdesivir-outside-of-clinical-trials.
- 32.Holshue ML, DeBolt C, Lindquist S, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382(10):929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hillaker E, Belfer JJ, Bondici A, Murad H, Dumkow LE. Delayed initiation of remdesivir in a COVID-19 positive patient. Pharmacotherapy. 2020 doi: 10.1002/phar.2403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Clinical and virologic characteristics of the first 12 patients with coronavirus disease 2019 (COVID-19) in the United States. Nat Med. Published online April 23, 2020. [DOI] [PubMed]
- 35.Jacobs JP, Stammers AH, St Louis J, et al. Extracorporeal membrane oxygenation in the treatment of severe pulmonary and cardiac compromise in COVID-19: experience with 32 patients. ASAIO J. 2020 doi: 10.1097/MAT.0000000000001185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pereira MR, Mohan S, Cohen DJ, et al. COVID-19 in solid organ transplant recipients: initial report from the US epicenter. Am J Transplant. 2020 doi: 10.1111/ajt.15941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Grein J, Ohmagari N, Shin D, et al. Compassionate use of remdesivir for patients with severe Covid-19. N Engl J Med. 2020 doi: 10.1056/NEJMoa2007016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wang Y, Zhang D, Du G, et al. Remdesivir in adults with severe COVID-19: a randomised, double-blind, placebo-controlled, multicentre trial. Lancet. 2020 doi: 10.1016/S0140-6736(20)31022-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.National Institute of Allergy and Infectious Diseases. NIH clinical trial shows remdesivir accelerates recovery from advanced COVID-19. 2020. [Accessed April 30, 2020]. https://www.niaid.nih.gov/news-events/nih-clinical-trial-shows-remdesivir-accelerates-recovery-advanced-covid-19.
- 40.Gilead Sciences. Gilead announces results from phase 3 trial of investigational antiviral remdesivir in patients with severe COVID-19. 2020. [Accessed April 30, 2020]. https://www.gilead.com/news-and-press/press-room/press-releases/2020/4/gilead-announces-results-from-phase-3-trial-of-investigational-antiviral-remdesivir-in-patients-with-severe-covid-19.
- 41.Abel S, Allan R, Gandelman K, et al. Pharmacokinetics, safety and tolerance of voriconazole in renally impaired subjects: two prospective, multicentre, open-label, parallel-group volunteer studies. Clin Drug Investig. 2008;28(7):409–420. doi: 10.2165/00044011-200828070-00002. [DOI] [PubMed] [Google Scholar]
- 42.Neofytos D, Lombardi LR, Shields RK, et al. Administration of voriconazole in patients with renal dysfunction. Clin Infect Dis. 2012;54(7):913–921. doi: 10.1093/cid/cir969. [DOI] [PubMed] [Google Scholar]

