Abstract
Background
Although patients with cardiovascular disease face excess risks of severe illness with coronavirus disease-2019 (COVID-19), there may be indirect consequences of the pandemic on this high-risk patient segment.
Objectives
This study sought to examine longitudinal trends in hospitalizations for acute cardiovascular conditions across a tertiary care health system.
Methods
Acute cardiovascular hospitalizations were tracked between January 1, 2019, and March 31, 2020. Daily hospitalization rates were estimated using negative binomial models. Temporal trends in hospitalization rates were compared across the first 3 months of 2020, with the first 3 months of 2019 as a reference.
Results
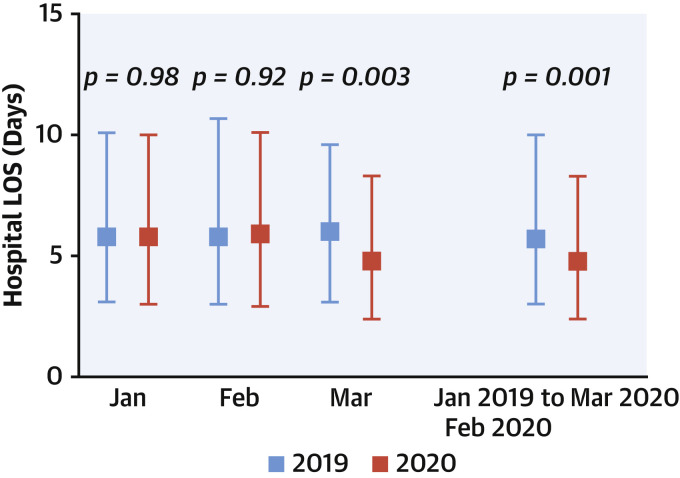
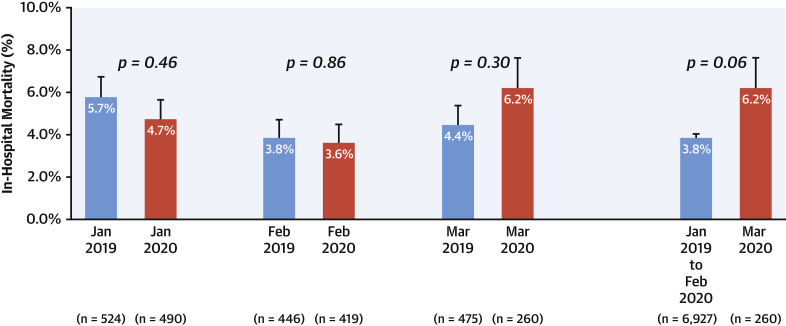
From January 1, 2019, to March 31, 2020, 6,083 patients experienced 7,187 hospitalizations for primary acute cardiovascular reasons. There were 43.4% (95% confidence interval [CI]: 27.4% to 56.0%) fewer estimated daily hospitalizations in March 2020 compared with March 2019 (p < 0.001). The daily rate of hospitalizations did not change throughout 2019 (–0.01% per day [95% CI: –0.04% to +0.02%]; p = 0.50), January 2020 (–0.5% per day [95% CI: –1.6% to +0.5%]; p = 0.31), or February 2020 (+0.7% per day [95% CI: –0.6% to +2.0%]; p = 0.27). There was significant daily decline in hospitalizations in March 2020 (–5.9% per day [95% CI: –7.6% to –4.3%]; p < 0.001). Length of stay was shorter (4.8 days [25th to 75th percentiles: 2.4 to 8.3 days] vs. 6.0 days [25th to 75th percentiles: 3.1 to 9.6 days]; p = 0.003) and in-hospital mortality was not significantly different (6.2% vs. 4.4%; p = 0.30) in March 2020 compared with March 2019.
Conclusions
During the first phase of the COVID-19 pandemic, there was a marked decline in acute cardiovascular hospitalizations, and patients who were admitted had shorter lengths of stay. These data substantiate concerns that acute care of cardiovascular conditions may be delayed, deferred, or abbreviated during the COVID-19 pandemic.
Key Words: cardiovascular, coronavirus, COVID-19, hospitalizations
Abbreviations and Acronyms: ACS, acute coronary syndromes; COVID-19, coronavirus disease-2019; HF, heart failure; STEMI, ST-segment elevation myocardial infarction
Central Illustration
The rapidly evolving coronavirus disease-2019 (COVID-19) pandemic has demanded major shifts in resource allocation worldwide. Health care systems have engaged in significant restructuring efforts to prepare for the expected surge of patients with COVID-19 illness, including the repurposing of inpatient beds into dedicated special pathogen units and expanding intensive care unit capacity. The pandemic has also led to deferral or cancellation of nonessential procedures, in-person patient visits, and routine diagnostic evaluations. Public messaging has focused around stay-at-home measures and appropriate physical distancing to mitigate transmission.
While patients with cardiovascular disease are recognized to face excess risks of severe illness with COVID-19 (1,2), there may be an indirect impact of the pandemic on these high-risk patients, even among those without direct viral infection or exposure. Anecdotal reports have identified a lower volume of hospital presentations for non–COVID-19 illnesses during the pandemic. Initial data suggest declines in cardiac catheterization laboratory activations for ST-segment elevation myocardial infarction (STEMI), a condition that requires prompt in-hospital treatment and intervention, without which patients have significant morbidity and mortality (3, 4, 5, 6). These early reports have raised concerns that similar reductions may be seen across other important acute cardiovascular conditions that generally require early in-hospital evaluation and treatment, including chest pain syndromes, heart failure (HF), and stroke, among others, although this has not been well characterized. We therefore examined longitudinal trends in hospitalizations for acute cardiovascular conditions before and during the COVID-19 pandemic in a large, tertiary care, integrated health system.
Methods
Hospitalizations for acute cardiovascular conditions with a primary discharge date between January 1, 2019 and March 31, 2020 were retrospectively examined across the tertiary care Mass General Brigham health system. Hospitalizations were categorized by primary admitting diagnosis according to International Classification of Diseases–10th Revision coding into the following categories: chest pain syndromes (including acute coronary syndromes [ACS]), HF, stroke, and other select acute cardiovascular conditions (Supplemental Table 1).
Prior to March 1, 2020, there was only a single case of COVID-19 in the state of Massachusetts, occurring in a patient who had traveled from Wuhan city in early February and who had undergone the recommended quarantine protocols. As such, demographic characteristics, length of stay, discharge disposition, and in-hospital mortality were compared between patients admitted in March 2020 and patients admitted before March 2020. Recognizing seasonal/temporal variations in cardiovascular admissions, characteristics and in-hospital clinical course were also compared between patients admitted in March 2020 and patients admitted in March 2019. Length of stay was defined as days from hospital admission to death (if occurring during hospitalization) or discharge from hospital. Continuous variables were summarized as mean ± SD or median (25th to 75th percentiles) and categorical variables as proportions; variables were compared using Student’s t-tests, Wilcoxon rank sum tests, and chi-square tests, as appropriate.
Daily hospitalization rates for acute cardiovascular conditions were estimated by using negative binomial models. Models were separately constructed for each month in 2020 to identify temporal changes in hospitalization rates. Temporal changes were analyzed across the first 3 months of 2019 for reference. Trends in hospitalization rates were analyzed for individual types of acute cardiovascular hospitalizations. Daily cardiovascular hospitalization rates were modeled as a continuous variable using restricted cubic splines; the number of knots was selected to minimize the Akaike information criterion. All p values <0.05 were considered significant.
For comparative purposes, daily confirmed cases of COVID-19 in Massachusetts were extracted based on state records (7). The study was reviewed and approved by the institutional review board of Mass General Brigham. All statistical analyses were performed using STATA (StataCorp, College Station, Texas). Tableau software (Seattle, Washington) was used for geomapping using zip codes of patients’ primary residences.
Results
Analytic cohort
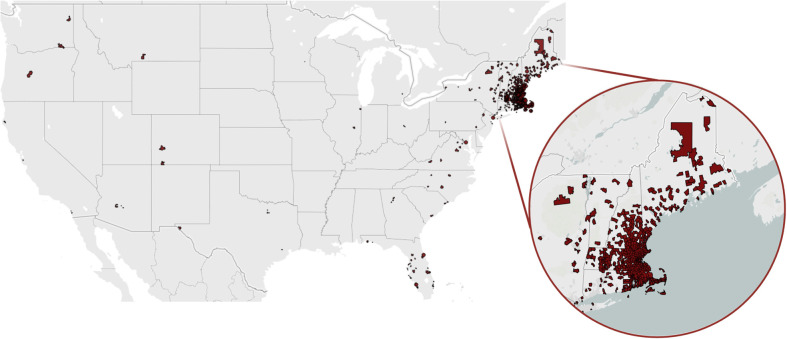
From January 1, 2019, to March 31, 2020, 6,083 unique patients experienced 7,187 hospitalizations for primary acute cardiovascular reasons. Hospitalized patients had primary residences spanning 26 states in the continental United States (Figure 1 ). Of all hospitalizations, 2,933 (40.8%) had primary discharge diagnoses of HF, followed by 2,217 (30.8%) for chest pain syndromes/ACS, 1,566 (21.8%) for stroke, and 471 (6.6%) for other select acute cardiovascular conditions. Overall, 2,076 (28.9%) admissions were to hospitals other than the 2 large academic teaching hospitals in the health system.
Figure 1.
Geographic Distribution of Patients Admitted to a Large Tertiary Care Health System
Geographic distribution of the primary residences of 6,083 patients admitted for acute cardiovascular reasons across the Mass General Brigham health care system from January 1, 2019, to March 31, 2020. Tableau software (Seattle, Washington) was used for geomapping by the zip codes of patients’ primary residences.
Baseline patient characteristics
Baseline demographic profiles of patients were compared between those admitted in March 2020 to those admitted before March 2020 and those admitted in March 2019 (Table 1 ). There were no significant differences in age, sex, and race distributions among groups; approximately 80% of admitted patients were white. Although the volume of hospitalizations was substantially lower in March 2020 compared with March 2019, the relative distribution of primary admission diagnoses was comparable; HF was the most common cause of cardiovascular hospitalization, occurring in 41.5% and 35.0% of patients admitted in March 2019 and March 2020, respectively. The proportion of total cardiovascular hospitalizations that were for STEMI was comparable between March 2020 and before March 2020 (3.1% vs. 3.7%; p = 0.59). Similar results were seen when comparing March 2020 to March 2019 (3.1% vs. 5.1%; p = 0.21).
Table 1.
Select Patient Characteristics and In-Hospital Course Before and During the COVID-19 Pandemic
| January 2019 to February 2020 | March 2019 | March 2020 | p Value∗ | p Value† | |
|---|---|---|---|---|---|
| Patient characteristics | |||||
| Patients | 5,852 | 404 | 231 | ||
| Age, yrs | 70.8 ± 13.8 | 71.1 ± 13.8 | 70.3 ± 15.1 | 0.60 | 0.51 |
| Men | 3,447 (58.9) | 233 (57.7) | 128 (55.4) | 0.56 | 0.58 |
| Race | 0.63 | 0.74 | |||
| White | 4,719 (80.6) | 332 (82.2) | 189 (81.8) | ||
| Black | 481 (8.2) | 31 (7.7) | 15 (6.5) | ||
| Other | 652 (11.1) | 41 (10.1) | 27 (11.7) | ||
| Hospital course | |||||
| Admissions | 6,927 | 475 | 260 | ||
| Hospitalization category | 0.22 | 0.34 | |||
| Chest pain syndrome | 2,133 (30.8) | 144 (30.3) | 84 (32.3) | ||
| Heart failure | 2,842 (41.0) | 197 (41.5) | 91 (35.0) | ||
| Stroke | 1,502 (21.7) | 97 (20.4) | 64 (24.6) | ||
| Other cardiovascular condition | 450 (6.5) | 37 (7.8) | 21 (8.1) | ||
| LOS, days | 5.7 (3.0–10.0) | 6.0 (3.1–9.6) | 4.8 (2.4–8.3) | 0.001 | 0.003 |
| Discharge home‡ | 4,816 (69.5) | 330 (69.5) | 192 (73.8) | 0.13 | 0.21 |
| In-hospital mortality | 265 (3.8) | 21 (4.4) | 16 (6.2) | 0.06 | 0.30 |
Values are n, mean ± SD, n (%), or median (25th to 75th percentiles).
COVID-19 = coronavirus disease-2019; LOS = length of stay.
The p values reflect comparisons between January 2019 to February 2020 and March 2020 (first and third columns).
The p values reflect comparisons between March 2019 and March 2020 (second and third columns).
Excludes discharge to home with hospice services.
Hospitalization rates for acute cardiovascular conditions
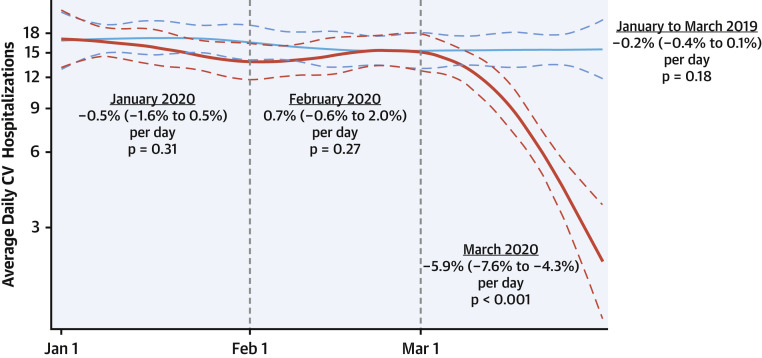
The estimated volume of daily acute cardiovascular hospitalizations was similar in January 2020 compared with month-matched hospitalizations in January 2019 (difference: –6.5%; 95% confidence interval [CI]: –17.9 to 6.6; p = 0.31) and in February 2020 compared with February 2019 (difference: –9.3%; 95% CI: –21.2% to 4.4%; p = 0.17). Conversely, there was a significant decline of 43.4% (95% CI: −27.4% to −56.0%) in the total number cardiovascular hospitalizations in March 2020 compared with March 2019 (260 hospitalizations vs. 475 hospitalizations; p < 0.001).
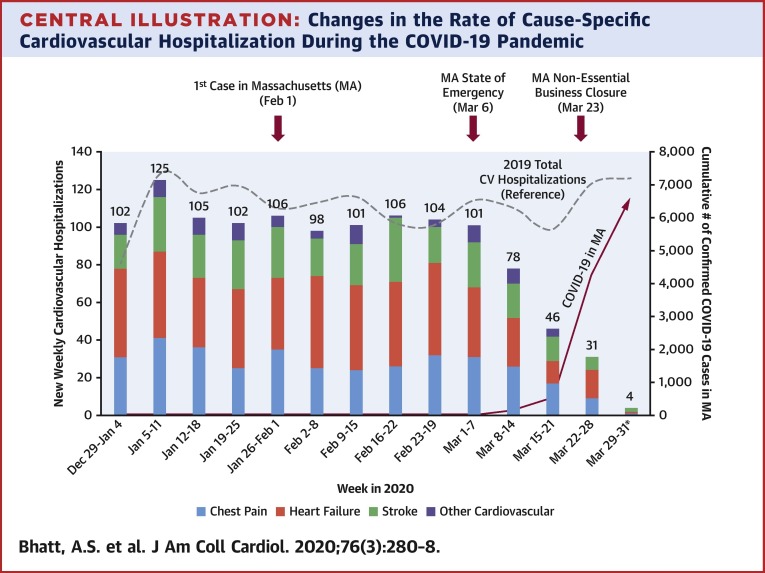
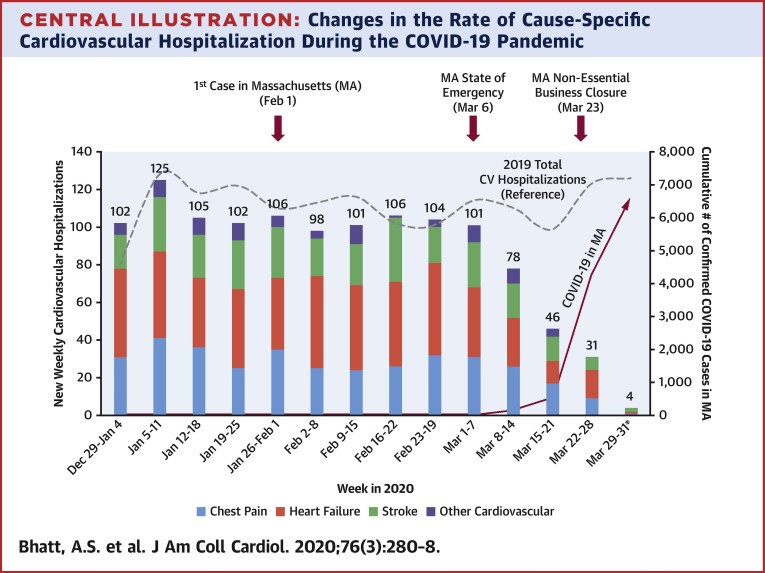
In addition to differences in volume of hospitalizations, the rate of change in admissions differed over time. There were no significant changes in the daily rates of cardiovascular hospitalizations throughout 2019 (–0.01% per day [95% CI: –0.04% to +0.02%]; p = 0.50), including during the first 3 months of 2019 (–0.2% per day [95% CI: –0.4% to +0.1%]; p = 0.18). Similarly, there were no significant changes in daily cardiovascular hospitalization rates in January 2020 (–0.5% per day [95% CI: –1.6% to +0.5%]; p = 0.31) and February 2020 (+0.7% per day [95% CI: –0.6% to +2.0%]; p = 0.27). In contrast, there was a significant incremental daily decline in cardiovascular admissions across the health system in March 2020 (–5.9% per day [95% CI: –7.6% to –4.3%]; p < 0.001) (Figure 2 ). This decline in hospitalization rates was observed irrespective of the primary reason for cardiovascular admission in March 2020 (all p ≤ 0.004): HF (–5.8% per day [95% CI: –8.3% to –3.3%]), chest pain/ACS (–5.5% per day [95% CI: –8.0% to –3.0%]), stroke (–4.9% per day [95% CI: –7.7% to –2.0%]), and other cardiovascular conditions (–10.5% per day [95% CI: –17.0% to –3.5%]). These declines corresponded with key COVID-19–related events, state guidance, and a rise in cumulative confirmed cases of COVID-19 in Massachusetts (Central Illustration ). By March 31, 2020, there were 6,620 confirmed cases and 89 deaths attributed to COVID-19 in Massachusetts.
Figure 2.
Changes in the Daily Rate of Cardiovascular Hospitalization During the COVID-19 Pandemic
Changes in estimated daily hospitalization rates for acute cardiovascular conditions from January 1, 2020, through March 31, 2020. The blue line delineates daily changes in hospitalization rate for acute CV conditions for the corresponding time period in calendar year 2019 as a reference. The dashed lines represent 95% confidence intervals. COVID-19 = coronavirus disease-2019; CV = cardiovascular.
Central Illustration.
Changes in the Rate of Cause-Specific Cardiovascular Hospitalization During the COVID-19 Pandemic
Change in total and cause-specific acute cardiovascular hospitalizations by week from January 1, 2020, to March 31, 2020. The dashed gray line represents the total acute CV hospitalization for the corresponding time period in calendar year 2019 for reference. The red line represents the cumulative number of confirmed COVID-19 cases in Massachusetts. The red arrows demarcate key dates in the COVID-19 pandemic in Massachusetts. ∗Indicates a partial week. CV = cardiovascular; COVID-19 = coronavirus disease-2019.
In-hospital clinical course
Data regarding length of stay and in-hospital mortality were available for all hospitalizations. Median length of stay was significantly shorter in patients admitted in March 2020 compared with those admitted before March 2020 (4.8 [25th to 75th percentiles: 2.4 to 8.3] days vs. 5.7 [25th to 75th percentiles: 3.0 to 10.0] days; p = 0.001) and compared with month-matched patients admitted in March 2019 (4.8 [25th to 75th percentiles: 2.4 to 8.3] days vs. 6.0 [25th to 75th percentiles: 3.1 to 9.6] days; p = 0.003) (Figure 3 ). Overall, there were 281 deaths observed during hospitalization from January 1, 2019, to March 31, 2020. In-hospital all-cause mortality rates were numerically higher in patients admitted in March 2020 compared with those admitted before March 2020 (6.2% vs. 3.8%; p = 0.06), although this was not statistically significant. In-hospital mortality rates were not different between patients admitted in March 2020 compared with patients admitted in March 2019 (6.2% vs. 4.4%; p = 0.30) (Figure 4 ).
Figure 3.
Hospital LOS Before and During the COVID-19 Pandemic
Total hospital LOS of cardiovascular hospitalizations in March 2020 and before March 2020 and separately for the first 3 months of 2019 and 2020. Each square represents the median LOS, and the bars reflect the 25th and 75th percentiles. LOS = length of stay; other abbreviations as in Figure 2.
Figure 4.
In-Hospital Mortality Before and During the COVID-19 Pandemic
All-cause mortality observed during cardiovascular hospitalizations in March 2020 and before March 2020 and separately for the first 3 months of 2019 and 2020. The error bars reflect standard errors. Abbreviations as in Figure 2.
Discussion
In this temporal analysis of more than 7,000 hospitalizations, a marked decline in total hospitalizations was observed for acute cardiovascular conditions in a large, tertiary care, integrated health care system in Massachusetts beginning in March 2020. During this month, total COVID-19 cases in Massachusetts increased from 1 on March 1, 2020, to 6,620 by March 31, 2020. Hospitalizations for a primary diagnosis of HF, chest pain syndromes/ACS, and stroke declined during this period (Central Illustration). We identified a 43% reduction in acute cardiovascular hospitalizations in March 2020 compared with March 2019. In addition, there was an incremental decline in the daily hospitalization rate by 6% each day in March 2020. Although patients admitted during the COVID-19 pandemic had comparable demographic characteristics, length of stay was shorter. In-hospital mortality was also numerically higher in patients admitted during the COVID-19 pandemic, suggesting greater severity of illness.
Presentations for HF, chest pain syndromes, and stroke are considered urgent and often require early invasive or pharmacological therapy in addition to careful inpatient monitoring to avoid associated morbidity and mortality. Although prior analyses have described temporal changes in STEMI-related cardiac catheterization laboratory activations (3,4), this is among the first descriptions of the change in a broad range of cardiovascular hospitalizations during the COVID-19 pandemic.
Beyond the concerning likelihood that patients are remaining at home with acute cardiovascular diseases, other reasons for these recent trends should be investigated. It is plausible that there is a true population-level reduction in cardiovascular events necessitating health care attention. Ecological factors such as shifts in dietary patterns—for instance, decreased consumption of high-sodium, fast-food intake (8)—and reduced exposure to ambient air pollution (9) may contribute to reduced daily risks. In addition, the emergence and widespread adoption of more accessible forms of communication between patients and their providers, including telemedicine (10), may be able to avert certain lower-acuity hospitalizations. Finally, the expected decline in ambulatory cardiovascular visits, outpatient testing, and deferral of elective procedures may have contributed to the lower rate of hospitalizations, because these often may serve as points of referral for inpatient hospitalization.
Patient and provider aversion to seeking care in medical centers with documented or suspected patients with COVID-19, a notion that has been well captured in the lay media (11, 12, 13, 14), represents a more concerning reason for our observed findings. These behaviors may be substantiated by stay-at-home messaging from major associations, governmental bodies, and media outlets, potentially leading to patients delaying or deferring hospital admission for acute cardiovascular conditions. Recent evidence has shown marked reductions in the rates of hospitalization for ACS during the pandemic in Austria and Italy (5,15). Our analysis supports and extends the findings in these European countries to a U.S. health system. In addition, our analysis provides evidence that hospitalization rates for other acute cardiovascular hospitalizations, such as HF and stroke, may be similarly reduced during the COVID-19 pandemic. The trend toward increased in-hospital mortality in March 2020 compared with earlier time periods also raises concerns that patients admitted for acute cardiovascular conditions during the COVID-19 pandemic may present later in their acute illness and, therefore, may have higher acuity. Indeed, provisional death counts from the Centers for Disease Control and Prevention already show trends toward excess mortality in Massachusetts. From February 1, 2020, to April 11, 2020, there have been 13,615 all-cause deaths reported, which is 1% greater than expected based on the average number of deaths across the same weeks in 2017 to 2019 (16); these findings are likely conservative because of underreporting of more recent deaths (17). Early global reports from areas affected earlier in the COVID-19 pandemic corroborate this experience and further suggest that excess mortality may in part be due to causes not directly related to infection with severe acute respiratory syndrome coronavirus 2 (18). Emerging data from the Lombardy region of Italy found substantial increases in out-of-hospital cardiac arrests during the COVID-19 pandemic compared with 2019 (19). Potential missed acute cardiovascular events may add to the composite detrimental effects of the COVID-19 pandemic on this high-risk patient segment (20).
Reasons for the observed shorter lengths of stay in patients admitted in March 2020 are likely multifactorial. There may be pressure from both patients and clinicians for early discharge, given concerns of heightened COVID-19 exposure risk in health care settings. In addition, given declines in elective cardiovascular procedures, wait times for certain necessary procedures may be reduced, facilitating earlier discharges.
Study strengths and limitations
Importantly, this study examines trends in acute cardiovascular hospitalizations across a large, integrated health system with broad patient membership across multiple states. In addition, the health system consists of care entities spanning the spectrum of clinical care facilities, from large urban academic centers to smaller, more rural community hospitals, improving the generalizability of our findings. In addition, seasonal variations in acute cardiovascular admissions were accounted for by comparing daily hospitalization rates to month-matched controls from 2019, highlighting a clear divergence in March 2020 from typical temporal fluctuations in acute cardiovascular admissions that can be expected, for example, because of declines in cardiopulmonary illnesses at the end of the seasonal influenza season.
Despite these strengths, this analysis has several important limitations. First, reliance on administrative coding may have led to misclassification of primary reasons for hospitalization. In particular, patients presenting with cardiopulmonary symptoms may have been coded for suspected COVID-19 disease or to nonspecific diagnoses despite a presentation ultimately more consistent with HF or chest pain syndromes. This issue may be amplified by the initial lack of rapid-turnaround COVID-19 testing capabilities and diagnostic tools. This misclassification may have contributed to the trends toward lower hospitalizations for acute cardiovascular conditions as COVID-19 cases rose in Massachusetts, although it would be unlikely to fully account for the substantial magnitude of reductions observed; similar reductions were seen in stroke, which generally has distinct symptomatology from that of COVID-19. Second, concurrent illness with COVID-19 among patients with cardiovascular disease may also contribute to the observed numerically higher in-hospital mortality rate. Formal diagnostic codes for COVID-19 were introduced only on April 1, 2020, and therefore could not be captured in this experience. Third, this analysis does not include emergency department presentations and, therefore, does not assess total initial presentations to the hospital for acute cardiovascular conditions. Fourth, it is possible that patients may have traveled outside of the region to less densely populated areas or may have been directed to other medical centers, although the health system cares for a broad geographic population and did not have any formal guidance for diversion to alternative centers. In addition, estimates during the period of this study in Massachusetts show adequate floor bed and intensive care unit capacity, reducing the likelihood of need for transfer to alternative centers (21). Fifth, our study had a low proportion of nonwhite patients, and given reports that certain racial groups are disproportionately affected by COVID-19 (22), this issue requires dedicated study in more diverse health care settings. Finally, we were not able to ascertain cause-specific mortality.
Conclusions
During the first phase of the COVID-19 pandemic in Massachusetts and surrounding areas, there was a corresponding marked reduction in daily hospitalizations for acute cardiovascular conditions in a large, multisite integrated health system, resulting in an almost halving of the volume of daily select acute cardiovascular hospitalizations in March 2020 as compared with March 2019. These conditions typically require prompt in-hospital evaluation and treatment to avoid significant morbidity and mortality. These findings may inform important policy considerations, including appropriation of funds in the Coronavirus Aid, Relief, and Economic Security (CARES) Act, which includes a provision for lost revenue by health care systems due to the COVID-19 pandemic (23). Establishment of dedicated facilities for the care (and post-acute care) of patients with COVID-19 may partially allay concerns on the part of patients and physicians about using health resources (24). Although reasons for the observed decline in hospitalizations are likely multifactorial, educational platforms and formal guidance for high-risk patients regarding when to seek emergency care are needed. This high-risk population should be longitudinally followed to determine the potential impact of the COVID-19 pandemic on long-term cardiovascular health, including among patients not directly exposed to or infected with severe acute respiratory syndrome-coronavirus-2.
Perspectives.
COMPETENCY IN SYSTEMS BASED PRACTICE: During the first phase of the COVID-19 pandemic in the United States, hospitalizations for acute cardiovascular conditions and length of stay decreased, suggesting that acute care was delayed, deferred, or abbreviated.
TRANSLATIONAL OUTLOOK: The reasons for shifts in patient behavior, impact on clinical outcomes, and alternative strategies for urgent clinical evaluation and management during such major societal perturbations require further investigation.
Footnotes
Dr. A.S. Bhatt has received honoraria from Sanofi Pasteur and participates in clinical endpoint committees of a trial sponsored by the National Institutes of Health (NIH). Dr. Claggett has received consultancy fees from Boehringer Ingelheim, Gilead, AOBiome, and Corvia. Dr. D.L. Bhatt has served on the Advisory Boards of Cardax, Cereno Scientific, Elsevier Practice Update Cardiology, Level Ex, Medscape Cardiology, PhaseBio, PLx Pharma, and Regado Biosciences; has served on the Board of Directors for Boston VA Research Institute, Society of Cardiovascular Patient Care, and TobeSoft; has served as the chair of the American Heart Association Quality Oversight Committee; has served on Data Monitoring Committees for the Baim Institute for Clinical Research (formerly Harvard Clinical Research Institute, for the PORTICO trial, funded by St. Jude Medical, now Abbott), Cleveland Clinic (including for the ExCEED trial, funded by Edwards), Duke Clinical Research Institute, Mayo Clinic, Mount Sinai School of Medicine (for the ENVISAGE trial, funded by Daiichi-Sankyo), and Population Health Research Institute; has received honoraria from the American College of Cardiology (ACC) (senior associate editor, Clinical Trials and News, ACC.org; vice-chair, ACC Accreditation Committee), Baim Institute for Clinical Research (formerly Harvard Clinical Research Institute; RE-DUAL PCI clinical trial steering committee funded by Boehringer Ingelheim; AEGIS-II executive committee funded by CSL Behring), Belvoir Publications (Editor-in-Chief, Harvard Heart Letter), Duke Clinical Research Institute (clinical trial steering committees, including for the PRONOUNCE trial, funded by Ferring Pharmaceuticals), HMP Global (Editor-in-Chief, Journal of Invasive Cardiology), Journal of the American College of Cardiology (guest editor; associate editor), Medtelligence/ReachMD (CME steering committees), Level Ex, MJH Life Sciences, Population Health Research Institute (for the COMPASS operations committee, publications committee, steering committee, and U.S. national coleader, funded by Bayer), Slack Publications (chief medical editor, Cardiology Today’s Intervention), Society of Cardiovascular Patient Care (secretary/treasurer), WebMD (CME steering committees); reports relationships with Clinical Cardiology (deputy editor), the NCDR-ACTION Registry Steering Committee (chair), and VA CART Research and Publications Committee (chair); has received research funding from Abbott, Afimmune, Amarin, Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Cardax, Chiesi, CSL Behring, Eisai, Ethicon, Ferring Pharmaceuticals, Forest Laboratories, Fractyl, Idorsia, Ironwood, Ischemix, Lexicon, Lilly, Medtronic, Pfizer, PhaseBio, PLx Pharma, Regeneron, Roche, Sanofi, Synaptic, and The Medicines Company; has received royalties from Elsevier (editor, Cardiovascular Intervention: A Companion to Braunwald’s Heart Disease); has served as site coinvestigator for Biotronik, Boston Scientific, CSI, St. Jude Medical (now Abbott), and Svelte; has served as a trustee for the American College of Cardiology; and has performed unfunded research for FlowCo, Merck, Novo Nordisk, and Takeda. Dr. Januzzi is a trustee of the ACC; has received grant support from Novartis Pharmaceuticals and Abbott Diagnostics; has received consulting income from Abbott Diagnostics, Janssen, MyoKardia, Novartis, and Roche Diagnostics; and participates in Clinical Endpoint Committees/Data Safety Monitoring Boards for Abbott, AbbVie, Amgen, Bayer, CVRx, Janssen, and Takeda. Dr. Butler is a consultant to Abbott, Adrenomed, Amgen, Applied Therapeutics, Array, AstraZeneca, Bayer, BerlinCures, Boehringer Ingelheim, Cardior, CVRx, Foundry, G3 Pharma, Imbria, Impulse Dynamics, Innolife, Janssen, LivaNova, Luitpold, Medtronic, Merck, Novartis, NovoNordisk, Relypsa, Roche, Sanofi, Sequana Medical, V-Wave Limited, and Vifor. Dr. Solomon has received research grants from Alnylam, Amgen, AstraZeneca, Bellerophon, Bayer, Bristol-Myers Squibb, Celladon, Cytokinetics, Eidos, Gilead, GlaxoSmithKline, Ionis, Lone Star Heart, Mesoblast, MyoKardia, NIH/National Heart, Lung, and Blood Institute, NeuroTronik, Novartis, Respicardia, Sanofi Pasteur, and Theracos; and has consulted for Akros, Alnylam, Amgen, Arena, AstraZeneca, Bayer, Bristol-Myers Squibb, Cardior, Cardurion, Corvia, Cytokinetics, Daiichi-Sankyo, Gilead, GlaxoSmithKline, Ironwood, Merck, MyoKardia, Novartis, Roche, Takeda, Theracos, Quantum Genetics, Cardurion, AOBiome, Janssen, Cardiac Dimensions, Tenaya, Sanofi Pasteur, DiNAQOR, and Tremeau. Dr. Vaduganathan is supported by the KL2/Catalyst Medical Research Investigator Training award from Harvard Catalyst (NIH/National Center for Advancing Translational Sciences Award UL 1TR002541); serves on Advisory Boards for Amgen, AstraZeneca, Baxter Healthcare, Bayer AG, Boehringer Ingelheim, Cytokinetics, and Relypsa; and participates on clinical endpoint committees for studies sponsored by Novartis and the NIH. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the JACCauthor instructions page.
Appendix
For a supplemental table, please see the online version of this paper.
Appendix
References
- 1.Guan W.-J., Ni Z.-Y., Hu Y. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Clerkin K.J., Fried J.A., Raikhelkar J. Coronavirus disease 2019 (COVID-19) and cardiovascular disease. Circulation. 2020;141:1648–1655. doi: 10.1161/CIRCULATIONAHA.120.046941. [DOI] [PubMed] [Google Scholar]
- 3.Garcia S., Albaghdadi M.S., Meraj P.M. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rodríguez-Leor O., Cid-Alvarez B., Ojeda S. Impacto de la pandemia de COVID-19 sobre la actividad asistencial en cardiología intervencionista en España. REC Interv Cardiol [serial online] April 2020 https://www.recintervcardiol.org/es/articulo-original/impacto-de-la-pandemia-de-covid-19-sobre-la-actividad-asistencial-en-cardiologia-intervencionista-en-espana Available at: [Google Scholar]
- 5.Metzler B., Siostrzonek P., Binder R.K., Bauer A., Reinstadler S.J. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur Heart J. 2020;41:1852–1853. doi: 10.1093/eurheartj/ehaa314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bangalore S., Sharma A., Slotwiner A. ST-segment elevation in patients with covid-19—a case series. N Engl J Med. 2020;382:2478–2480. doi: 10.1056/NEJMc2009020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Commonwealth of Massachusetts Archive of COVID-19 cases in Massachusetts. https://www.mass.gov/info-details/archive-of-covid-19-cases-in-massachusetts Available at:
- 8.Ceriello A., Taboga C., Tonutti L. Evidence for an independent and cumulative effect of postprandial hypertriglyceridemia and hyperglycemia on endothelial dysfunction and oxidative stress generation: effects of short- and long-term simvastatin treatment. Circulation. 2002;106:1211–1218. doi: 10.1161/01.cir.0000027569.76671.a8. [DOI] [PubMed] [Google Scholar]
- 9.Pranata R., Vania R., Tondas A.E., Setianto B., Santoso A. A time-to-event analysis on air pollutants with the risk of cardiovascular disease and mortality: a systematic review and meta-analysis of 84 cohort studies. J Evid Based Med. 2020;13:102–115. doi: 10.1111/jebm.12380. [DOI] [PubMed] [Google Scholar]
- 10.Wang X., Bhatt D.L. COVID-19: an unintended force for medical revolution? J Invasive Cardiol. 2020;32(4):E81–E82. [PubMed] [Google Scholar]
- 11.Neville S., Bounds A., Dickie M., Cocco F., Staton B. Empty non-coronavirus beds raise fears that sickest are avoiding NHS. Financial Times. https://www.ft.com/content/d5ac0a79-6647-4f49-bb64-d1cc66362043 Available at:
- 12.Krumholz H.M. Where have all the heart attacks gone? The New York Times. https://www.nytimes.com/2020/04/06/well/live/coronavirus-doctors-hospitals-emergency-care-heart-attack-stroke.html Available at:
- 13.Sheth K. Hospital admissions for strokes appear to have plummeted, a doctor says, a possible sign people are afraid to seek critical help. Washington Post. https://www.washingtonpost.com/national/health-science/hospital-admissions-for-strokes-appear-to-have-plummeted-a-doctors-says-a-possible-sign-people-are-afraid-to-seek-critical-help/2020/04/08/2048b886-79ac-11ea-b6ff-597f170df8f8_story.html Available from:
- 14.Bernstein L., Sellers F.S. Patients with heart attacks, strokes and even appendicitis vanish from hospitals. Washington Post. https://www.washingtonpost.com/health/patients-with-heart-attacks-strokes-and-even-appendicitis-vanish-from-hospitals/2020/04/19/9ca3ef24-7eb4-11ea-9040-68981f488eed_story.html Available at: Accessed April 6, 2020.
- 15.De Filippo O., D’Ascenzo F., Angelini F. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in Northern Italy. N Engl J Med. 28 April 2020 doi: 10.1056/NEJMc2009166. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.National Center for Health Statistics Provisional death counts for coronavirus disease (COVID-19) https://www.cdc.gov/nchs/nvss/vsrr/covid19/index.htm Available at:
- 17.Spencer M.R., Ahmad F. Vital Statistics Rapid Release; December 2016. Timeliness of death certificate data for mortality surveillance and provisional estimates.https://www.cdc.gov/nchs/data/vsrr/report001.pdf Available at: Accessed April 6, 2020. [Google Scholar]
- 18.Covid-19’s death toll appears higher than official figures suggest. The Economist; April 4, 2020. https://www.economist.com/graphic-detail/2020/04/03/covid-19s-death-toll-appears-higher-than-official-figures-suggest Available at: [Google Scholar]
- 19.Baldi E., Sechi G.M., Mare C. Out-of-hospital cardiac arrest during the covid-19 outbreak in Italy. N Engl J Med. 2020 April 29 doi: 10.1056/NEJMc2010418. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rosenbaum L. The untold toll—the pandemic’s effects on patients without covid-19. N Engl J Med. 2020;382:2368–2371. doi: 10.1056/NEJMms2009984. [DOI] [PubMed] [Google Scholar]
- 21.Commonwealth of Massachusetts Hospital bed availability April 17, 2020. https://www.mass.gov/doc/hospital-bed-availability-april-17-2020 Available at:
- 22.Yancy C.W. COVID-19 and African Americans. JAMA. 2020 April 15 doi: 10.1001/jama.2020.6548. [E-pub ahead of print] [DOI] [PubMed] [Google Scholar]
- 23.CARES Act, S 3548, 116th Cong (2020) https://www.congress.gov/bill/116th-congress/senate-bill/3548 Available at:
- 24.Grabowski D.C., Joynt Maddox K.E. Postacute care preparedness for COVID-19: thinking ahead. JAMA. 2020 Mar 25 doi: 10.1001/jama.2020.4686. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.