Introduction
Over the last few months, coronavirus disease 2019 (COVID-19) has spread across the globe, infecting millions and killing hundreds of thousands [1]. Global stay-at-home orders have resulted in economic shutdown and unemployment rates reaching a historic 14.7% in the United States [2]. This disease has led to a deep financial downturn for health care systems, as hospitals cancelled elective procedures and diagnostic services to reduce potential exposures and reallocate resources for expected COVID-19 patient surges. This article discusses the financial crisis that has arisen from the COVID-19 pandemic at University of Washington (UW) Radiology and steps taken in the short term to mitigate revenue losses, as well as long-term plans to create a more resilient, healthier radiology department.
Financial Impact
The COVID-19–related financial impact on hospital systems has been broad-reaching. A survey by Piper Sandler Co of 160 physicians in 16 different specialties across 4 states (California, Massachusetts, Washington, and New York) indicated volumes across specialties are down 65% and are expected to be down for a prolonged period, even after the stay-at-home orders are lifted [3]. Those surveyed felt volumes will continue to be down for the next year, with an estimated 12% volume reduction in April 2021. Reduced volumes for ordering physicians will similarly impact radiology volumes. This sentiment is echoed by patient surveys that indicate heightened anxiety over potential exposures in hospital systems, with 36% of those polled indicating that they would not return to hospital systems for at least 3 months after the stay-at-home orders are lifted [4]. This raises concerns for an extended radiology financial downturn, creating the necessity for financial mitigation planning for the short term as well as longer-term measures that can increase the financial resiliency of radiology departments.
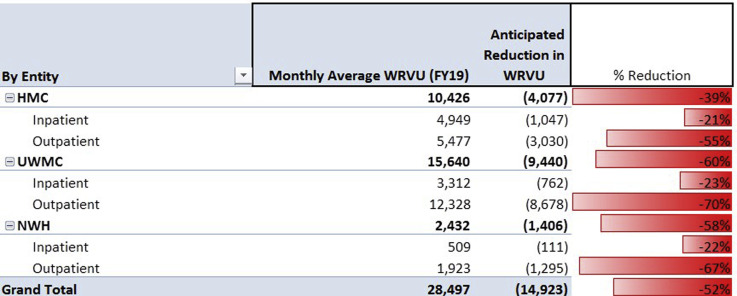
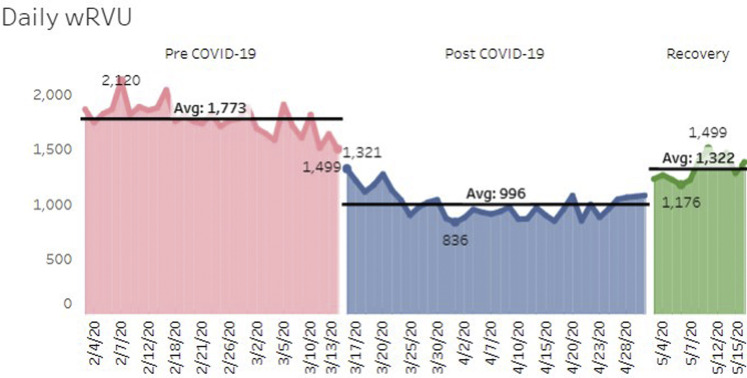
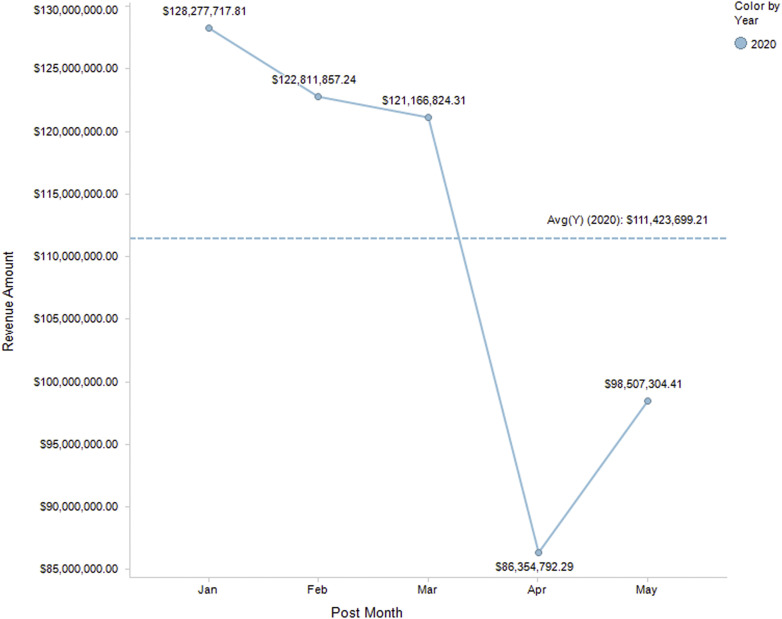
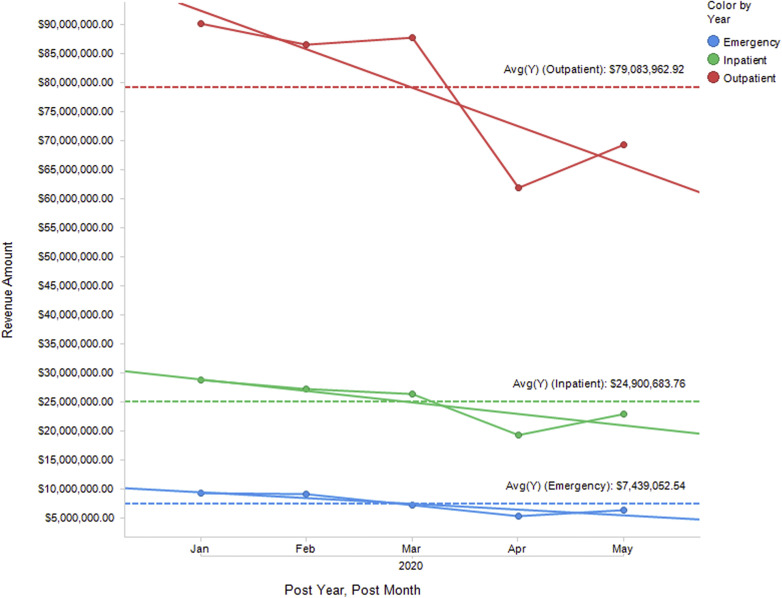
It was estimated that total work relative value unit (wRVU) loss across UW Radiology would be 52% during the COVID-19 pandemic. Between our three major hospital systems, the radiological impact would range from 39% to 60%, with outpatient imaging volume losses of 55% to 70% (Fig. 1 ). We have estimated that for UW Radiology, the net revenue loss through March 2021 will be $4,900,000. The actual daily wRVU has declined 45% during the COVID-19 shutdown period from March 16, 2020, through April 24, 2020 (average 1,785 wRVU/d pre-COVID-19 to 982 wRVU/d during COVID-19) (Fig. 2 ). The decline during this period for Seattle Cancer Care Alliance is 46%, 42% for University of Washington Medical Center (UWMC) Northwest campus, 41% for Harborview Medical Center, and 47% for UWMC-Montlake. UW Radiology gross charges showed a 30% decline in April 2020 relative to the average charges from February and March of the same year (Fig. 3 ). The most pronounced decline in gross charges was from outpatient imaging (Fig. 4 ), as would be expected considering the postponement of elective imaging. Outpatient imaging gross charges dropped by 30% from March to April 2020, inpatient charges declined by 27%, and emergency department charges declined by 26%. There was also a change in payor mix, with a decline in commercial insurance (42.02% in March 2020 compared with 37.77% in May 2020) and a rise in Medicaid over the same period (18.72% to 21.58%) (Fig. 5 ). May 2020 has shown recovery once elective imaging resumed for volumes and gross charges and improvement in payor mixes, though not to baseline volumes.
Fig 1.
Estimated WRVU loss divided into UW Medicine hospital systems, inpatient and outpatient volumes monthly average during the downturn (middle column) as compared to average monthly WRVU for fiscal year 2019 (left column). HMC = Harborview Medical Center; NWH = University of Washington-Northwest campus; UWMC = University of Washington-Montlake campus; WRVU = work relative value unit.
Fig 2.
Actual work relative value unit difference between the pre–coronavirus disease 2019 period (January 7, 2020, to March 15, 2020) and coronavirus disease 2019 period (March 16, 2020, to May 4, 2020) and the recovery period (May 2, 2020 to current). The separation between the two groups is the time point when elective imaging postponement was initiated. The separation between the coronavirus period and the recovery phase is when the slow ramp-up of elective imaging was started.
Fig 3.
Gross charges per month for 2020. There was a marked decline in April 2020, with a rebound in May 2020 once outpatient imaging was resumed, though still well below the baseline from January through March 2020. May includes through May 30, 2020. year. Avg(Y) = average for year.
Fig 4.
Gross charges per month separated into inpatient (green), outpatient (red), and emergency department (blue) volumes. The most pronounced drop in charges during April 2020 was from outpatient volumes, though there were declines in all three facets. There was some recovery in May 2020 coinciding with resumption of elective imaging in early May. May data covers through May 30, 2020. Avg(Y) = average for year.
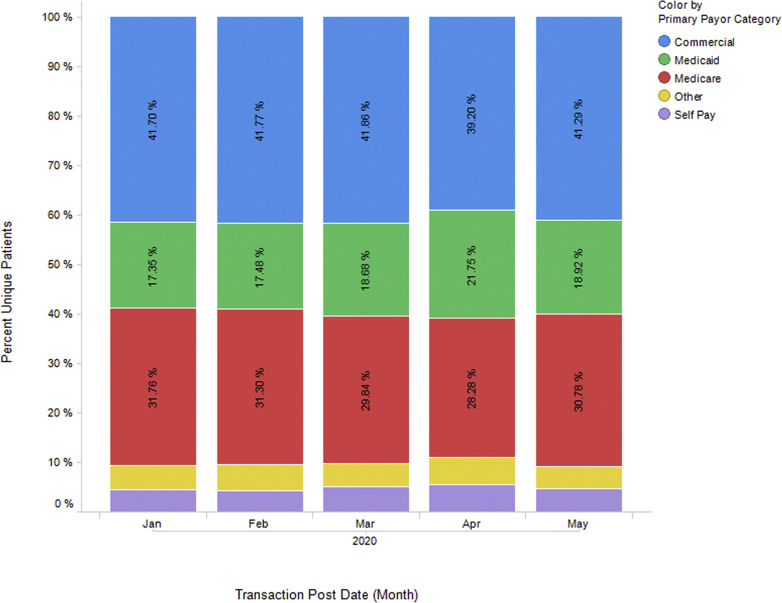
Fig 5.
Designation of payor per unique patient per month. There was a decline in commercial payors and an increase in Medicaid during April 2020 relative to the previous months, with an improvement in payor mix during May 2020. May data covers through May 30, 2020.
Short-Term Mitigation Plans for Financial Losses
In the short term, steps to mitigate department and hospital financial losses due to closure of elective imaging are necessary to keep these entities solvent, especially in situations in which reserves are limited or have been exhausted. There have been a number of approaches we have taken to reduce our expenses. These steps have been taken in an effort to maintain faculty and staff salaries and full-time equivalent levels and avoid furloughs or terminations.
First, we have eliminated a teleradiology service that was providing overnight coverage for UWMC-Northwest (our community hospital), which reduces the hospital’s monthly costs by $40,000 to $45,000. We have also eliminated internal locum temporary supplemental pay shifts at this hospital for coverage of evenings and weekends as well as some interventional radiology pay supplement shifts, reducing expenses by $1,380,000 over a full academic year. Although this money comes directly from hospital budgets, we have negotiated shared savings, with possible splitting of the unspent money. We have consolidated our coverage with the main campus hospital in a number of ways. We have extended daytime coverage hours to 7 am to 7 pm for all sections that cover emergency department volumes (neuroradiology, musculoskeletal radiology, chest radiology, and body imaging). We are also incorporating UWMC-Northwest overnight volumes into trainee overnight coverage duties. This consolidation plan was to take effect once overnight emergency room radiology coverage was instituted in the fall of 2020; however, the financial crisis has accelerated our plans, which we believe will cut costs but also provide improved patient care.
We have taken additional approaches to reducing costs. Graduation events are being consolidated into a single virtual event, with smaller fellowship events, which saved the department $90,000. We are in the process of consolidating support staff and optimizing their efforts, which will result in $400,000 of savings. New faculty hiring will be frozen for 6 months, though contracts that have been signed will be honored, and 75% of the incentive will be deferred until the next academic year, postponing payment of $300,000. In addition, leased office space used by administrative staff ($160,000 cost) will expire, and these staff members will be relocated to the main radiology department. We estimate that these cost-cutting approaches in addition to a few others will result in department spending reduction or saving of $3,257,000.
Long-Term Growth Plans
The timeline and evolution of the COVID-19 pandemic is not completely understood at this point, and as described previously, persistent patient anxieties will likely exist until a vaccine is developed. In addition, future pandemics are likely to arise that may have similar impacts on health care institutions. For these reasons, radiology departments should focus on strengthening their financial base and increasing reserves to achieve improved resiliency. The approach at academic institutions and private practices are likely to differ. Private practices can consider limiting or potentially eliminating high cost–low volume services and partnering with other practices to cover these services. Schedule optimization to match patient needs can improve the patient experience and improve business. Practices should not rely on loyalty from referral bases and should aggressively market to expand and diversify their referral base, including both small and large referrer groups. Providing high-quality and expanded services in areas that match the referral base needs and focus and working to stand out locally in that particular space can contribute financially. An example is working to develop strong cancer diagnostic and therapeutic services that would partner with local cancer care practices.
Increased revenue diversification through various operational projects are currently in development for UW Radiology. Our group has been negotiating with hospital leadership a plan to establish new outpatient imaging centers beyond the four that are currently part of UW Medicine. The new imaging centers would be part of multispecialty care centers, with a shared financial revenue model, between the radiology department and the hospitals. The department has also been collaborating with hospital leadership and multiple clinical services to create premium population health assessment services, revolving around focused organ systems, including multidisciplinary cardiovascular, joint, and brain health assessments. We have received funding approval to create an overnight faculty emergency radiology service to cover our three emergency departments. Although this measure will only have a small impact on funding due to increased imaging services provided overnight, we are working to negotiate contracts with a number of Washington state community hospitals to provide overnight teleradiology coverage. We have also expanded our contract research organization efforts with additional contracts and plan to continue this expansion. We have improved imaging efficiencies, especially in CT and MRI, with shortened scan block times, which in the long term will result in increased imaging throughput and higher scan volumes. Although a slow ramp-up in the short term may reduce financial growth potential, these programs will support long-term fiscal health and help build toward a more stable future.
Summary
The COVID-19 pandemic has had a significant impact on the finances of radiology departments and health care systems globally. Short-term mitigation plans are necessary for groups to weather the crisis, and long-term revenue diversification and growth plans are needed to strengthen departments, replenish financial reserves, and make them more crisis resilient.
Footnotes
The authors state that they have no conflict of interest related to the material discussed in this article. All authors are employees of an academic institution. Dr Mossa-Basha, Vice Chair of Clinical Operations, Radiology Chief of Service, University of Washington and NWH Medical Centers, Medical Director of MRI, University of Washington School of Medicine, Seattle, Washington. Mr Justin Deese, Director, Finance and Administration, Washington School of Medicine, Seattle, Washington. Ms Dawn Vincic, Assistant Administrator for Radiology, Washington School of Medicine, Seattle, Washington. Dr Dushyant V. Sahani, Chair of Radiology, University of Washington School of Medicine, Seattle, Washington.
References
- 1.COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU) https://coronavirus.jhu.edu/map.html Available at:
- 2.British Broadcast Corporation Coronavirus: US unemployment claims hit 33.3 million amid virus. https://www.bbc.com/news/business-52570600 Available at:
- 3.Shinkman R. Doctors say COVID-19 has slashed patient volumes, made finances shaky. Health Care Dive. https://www.healthcaredive.com/news/doctors-say-covid-19-has-slashed-patient-volumes-made-finances-shaky/575876/ Available at:
- 4.Revive Health COVID-19 consumer survey findings report - part 2. https://www.thinkrevivehealth.com/covid-19/covid-19-consumer-survey-findings-report-part-2 Available at: