Abstract
The coronavirus disease 2019 (COVID 2019) pandemic has presented myriad challenges to an underprepared health care system. Health care providers are facing unprecedented acute workplace stress compounded by a high baseline rate of physician burnout. This article discusses the relationship between acute stress disorder, posttraumatic stress disorder, and burnout through a literature review focusing on the mental health impact on health care providers after prior epidemics and natural disasters. We offer both a framework for understanding the mental health impact of the COVID-19 epidemic on physicians while proposing a systems based model to respond to these challenges.
Key Words: Burnout, COVID-19, PTSD, wellness
Background
The coronavirus disease 2019 (COVID-19) pandemic has posed unprecedented challenges to the health care system worldwide, revealing major deficiencies in this country’s epidemic preparedness. Individuals have been required to drastically modify their lifestyle in an effort to “flatten the curve” and engage in social distancing to allow an overwhelmed health care system time to respond to the novel coronavirus. In health care, this circumstance is so profound that the COVID-19 pandemic has required an adoption of the language of war. There is talk of physician redeployment to the frontline and sophisticated statistics track daily causalities while military style temporary hospitals are constructed. CNN has compared the epidemic’s impact on our civilization to that of World War II [1]. In their personal lives, radiologists are required to adapt to the myriad challenges imposed by the pandemic and also manage the stresses related to caring for patients with COVID-19 and working in a health care system with limited resources while evaluating constantly evolving knowledge surrounding containment and management of the COVID-19 illness.
This pandemic has exacerbated stressors in a health care system in which physician burnout, a response to workplace stress, is already epidemic [2]. Individual physicians and hospital administration should take proactive steps to minimize the compounding effects of high baseline physician burnout with the acute stressors of the COVID-19 pandemic.
Although posttraumatic stress disorder (PTSD) is commonly associated with active military conflict, the context and definition of what constitutes a traumatic event is, in fact, much broader and is relevant to the COVID-19 pandemic and its impact on radiologists. This article presents a conceptual paradigm for understanding the relationship between burnout, acute stress disorder, and PTSD and provides an evidence-based review and recommendations for systems-based interventions that may reduce physicians’ stress ensuring a stable and healthy radiology workforce.
Intersection of Burnout and PTSD
Mental health providers define trauma as a stressful occurrence that is outside the range of the usual human experience and that would be markedly distressing to almost anyone [3]. This type of stressor, according to the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition, involves a perceived intense threat to life, physical integrity, intense fear, helplessness, or horror [4]. By this definition the COVID-19 and the threat to personal safety and fear that it has produced meets the definition of a traumatic event.
Exposure to such traumatic and stressful events can lead to the development of acute stress disorder and finally PTSD, if symptoms persist. Similarly, burnout is a syndrome driven by increased exposure to workplace stressors that results in emotional exhaustion, depersonalization, and decreased sense of personal accomplishment [5]. In a study by Dyrbye et al, a survey using the Maslach Burnout Inventory found the rate of radiologist burnout to be 61% [6]. In this regard, the COVID-19 pandemic presents a sort of perfect storm regarding the intersection of chronic workplace stress resulting in an epidemic physician burnout rates with the acute traumatic stress imposed by the pandemic. Exploring the intersection of these two phenomena is necessary in order to inform interventions.
Symptoms related to PTSD fall into three categories that include reliving the event, a sense of emotional numbness or depersonalization, and symptoms of increased arousal (difficulty sleeping, feeling irritated or easily angered, difficulty concentrating) [3]. The diagnosis of PTSD occurs when a person has experienced symptoms for at least 1 month after a traumatic event, although symptoms may be delayed by several years [3]. In the initial month after exposure to a traumatic event, the diagnosis applied is acute stress disorder and includes similar symptoms of intrusion, dissociation, negative mood, avoidance, and arousal. The prevalence of acute stress disorder is 5% to 20% after a traumatic event [7]. Importantly, intervention in this early phase can reduce the progression to PTSD [7].
Increased exposure to stress and trauma in multiple life domains, including acutely increased workplace stress resulting from the pandemic, when combined with underlying baseline burnout, may result in rising rates of PTSD among physicians. Additionally, because there is significant overlap in drivers of both PTSD and burnout, as well as consequences and comorbidities, the intersection of these entities may have a compounding effect (Table 1 ).
Table 1.
| Drivers | Symptoms | Consequences | Interventions |
|---|---|---|---|
| Burnout | |||
| Lack of job control | Emotional exhaustion | ↓ Productivity | Organization directed∗ |
| Excessive workload | Depersonalization | ↓ Quality of patient care | ↓ Clinical demand via schedule changes |
| Prolonged work stress | Decreased sense of accomplishment | ↓ Patient satisfaction | ↑ Team work |
| Imbalance between demands and skill set | ↑ Turnover | ↑ Job control | |
| ↑ Medical errors | ↑ Shared decision making | ||
| ↑ Substance abuse | Physician directed | ||
| ↑ Depression and even suicide | Mindfulness | ||
| Disrupted relationships | CBT | ||
| PTSD | |||
| Medical illness | Intrusive thoughts | Anxiety disorders | Psychotherapy |
| Mass conflict and displacement | Nightmares or sleep disturbances | Depression | Exposure therapy |
| Combat | Flashbacks | Somatic symptoms | EMDR |
| Physical injury or assault | Avoidance | Substance abuse | CBT |
| Hypervigilance | Suicide | Medication | |
| Disrupted relationships |
CBT = cognitive behavioral therapy, EMDR = Eye Movement Desensitization and Reprocessing; PTSD = posttraumatic stress disorder.
Organization-directed interventions have been shown to be more effective in preventing and reducing burnout [5].
For example, lack of control over one’s schedule is a known driver of burnout that may acutely worsen for individual radiologists as hospital administration responds to changes in imaging volume and economic consequences by redefining work hours, staffing, and clinical responsibilities. Many radiologists also face the threat of redeployment to understaffed fields of medicine taxed by the pandemic providing an example of the way in which another known driver of burnout—imbalance between skill set and work demands—may be exacerbated by the pandemic. Theoretically, and in a worst-case scenario, if these workplace stressors were combined with the added loss of control and sense of displacement that may arise if a radiologist were exposed to or contracted COVID-19 and needed to quarantine away from home and family, the mental health consequences could be devastating.
Epidemics and Mental Health
Large-scale disasters are associated with significant increases in mental health disorders in both the immediate aftermath of the trauma and over longer periods of time with increased rates of PTSD, depression, and substance abuse disorders reported [8]. Similarly, burnout is associated with higher rates of substance abuse, depression, and suicide [6]. Those studies that specifically examined the psychological impact of epidemics, such as the 2003 severe acute respiratory syndrome (SARS) outbreak, found that up to 10% of health care workers had high SARS-related PTSD symptoms 3 years after the outbreak [9]. To compare magnitude, the 2003 SARS epidemic claimed 774 lives from November 2002 to July 2003 with 8,098 afflicted worldwide [10]. The COVID-19 pandemic has claimed approximately 83,947 lives and infected 1,384,930 individuals in the United States alone from February 2020 to May 15, 2020 [11]. This staggering statistic raises epidemiologic concerns that the COVID-19 pandemic may have an even more profound impact on the mental health of physicians.
A recent article outlines eight specific sources of physician anxiety related to the COVID-19 epidemic, including (1) access to appropriate personal protective equipment, (2) exposure to COVID-19 at work and bringing the infection home to family, (3) lack of access to testing if physicians develop COVID-19 symptoms and associated fear of propagating the infection at work, (4) uncertainty that physicians’ organization will support and take care of physicians personal needs if they become infected, (5) access to childcare during increased work hours and school closures, (6) lack of support for other personal and family needs as work demands increase, (7) being able to provide competent medical care if deployed to a new area, and (8) lack of access to up-to-date information and communication [12]. These well-articulated sources of stress and anxiety fall outside of the realm of the usual experience of the workplace and are drivers of both burnout as well as ARS and PTSD. Acutely worsening systemic stressors may have a significant and negative impact on the health care system and patient safety.
Before addressing appropriate systems-based responses to such stressors, it is both essential and just to also consider the role that racism may play with regard to increased PTSD susceptibility among minority health care providers in response to the COVID-19 pandemic. A recent survey conducted by the Association of American Medical Colleges found that 17.1% of physicians in the United States self-identified as ethnic Asian [13]. Many minority groups experience higher rates of PTSD when compared with white populations, and one theory for this vulnerability focuses on the traumatic nature of racism [14]. On May 8, 2020, the United Nations Secretary General warned against xenophobia and anti-Asian sentiment, stating that “the pandemic continues to unleash a tsunami of hate and xenophobia, scapegoating and scare-mongering” and advised governments to “act now to strengthen the immunity of our societies against the virus of hate” [15]. There is, unfortunately, an abundance of historical precedent for minority discrimination related to epidemics and pandemics. Examples include violent pogroms against the Jewish community during the Black Death (1347-1351) and, in recent history, discrimination in response to human immunodeficiency virus and acquired immunodeficiency syndrome pandemic [16]. Historians cite “the newness and mysteriousness of a disease” as a predisposing factor for igniting racial violence and minority scapegoating, and these elements certainly apply to the current state of the COVID-19 pandemic, underscoring the potential of this pandemic to incite racism [16]. It is critical that radiology leadership maintain a zero tolerance policy regarding workplace discrimination and also commit to support strong diversity training programs and efforts that focus on humanism and tolerance.
Impact and Interventions
The impact of PTSD among health care workers on patient safety has not been widely studied in radiologists. However, there is evidence that among health care providers with symptoms of PTSD, burnout is also highly prevalent, and a recent meta-analysis identified physician burnout as significantly and positively correlated with increased rates of medical error [2,17]. Physician burnout is costly, and not only in terms of the potential for increased medical error. The syndrome of burnout is associated with increased risk of physician suicide as well as substance abuse and may contribute to health care infrastructure instability by fostering increased turnover, early retirement, and decrease in percent of professional effort; these consequences are certainly undesirable in the setting of a pandemic requiring increased health care resources and reserves [2,18].
Previous conceptual models related to mitigating physician burnout focus on individual as well as systems-based interventions and suggest that the responsibility for maintaining a healthy physician work force lies not only with individual physicians but with hospital administration and department leadership [19]. Therefore, both individual strategies and systems-based interventions should be adopted in these challenging times [19].
Individual Interventions
Recent recommendations to improve individual radiologists well-being in the setting of the COVID-19 pandemic have suggested “micropractices,” or strategies requiring just a few seconds that are readily available to individual physicians to manage stress. These practices focus on managing the emotional aspects of stress and fear and leverage positive psychology, mindfulness practices, and embodiment to combat the fight-or-flight response as well as symptoms of emotional exhaustion and depersonalization [20]. Similar interventions, including mindfulness and gratitude practices, have been successful in the setting of PTSD [20, 21, 22]. The ACR Radiology Well-Being Program has compiled an online collection of resources to promote radiologist wellness during the COVID-19 pandemic and the website contains direct links to resources focusing on the arts, mindfulness, fitness, and sleep [23]. One additional, important and potentially overlooked well-being practice involves limiting one’s exposure to media coverage of the pandemic. After the Boston Marathon Bombing, one study found that those individuals with repeated related medial exposure after the event reported experiencing higher levels of acute stress than those present during the actual event itself [24]. Although individual action steps are certainly required to promote resilience and well-being during this time of crisis, an appropriate and informed response from the health care system and radiology leadership will also be required.
Systems-Based Interventions
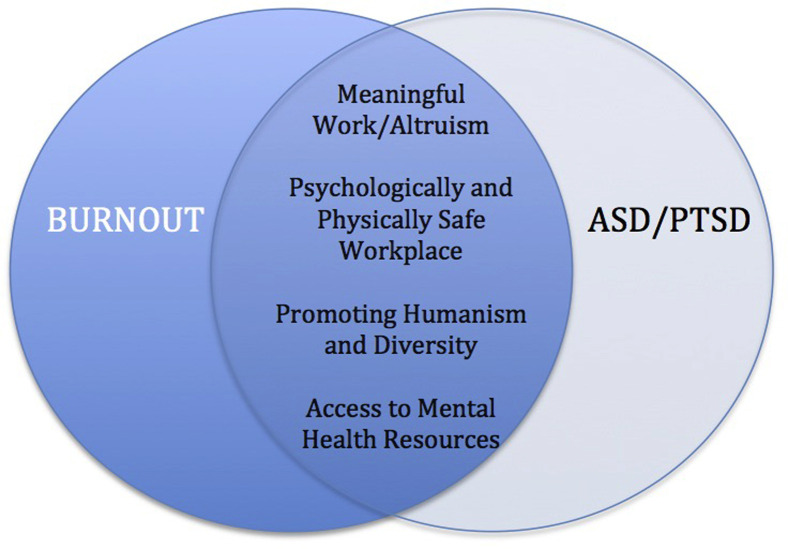
Interestingly, the incidence of PTSD in health care workers after the SARS pandemic positively correlated with the perceived risk of exposure and was negatively associated with provider identification with their work as altruistic [9]. These are important factors that may be considered in informing the allocation of department resources and efforts to minimize physician burnout and PTSD. A framework of suggested interventions to prevent burnout and treat PTSD in the radiology workforce are outlined herein and in Table 2 and Figure 1 .
Table 2.
Construct for interventions to prevent burnout, ASD, and PTSD related to the COVID-19 pandemic
| Interventions to Prevent Burnout, ASD, and PTSD | Potential Benefits |
|---|---|
| Support an infrastructure that allows radiologists and staff to work from home | Decreases exposure and mitigates concerns about contracting the virus and promotes schedule flexibility |
| Increase education treatment about burnout, ASD, and PTSD via expert panel discussions and access to mental health | Increases awareness and early intervention, reduce stigma |
| Employ nontraditional methods of physician engagement (eg, narrative medicine) | Facilitates cognitive reframing and self-compassion, reinforces a sense of altruism in work |
| Clear communication from leadership | Increases sense of safety and stability, increases team work |
| Engage radiologists in scheduling | Increases engagement and prevent burnout, promotes schedule flexibility |
ASD = acute stress disorder; COVID-19 = coronavirus disease 2019; PTSD = posttraumatic stress disorder.
Fig 1.
A systems-based model for minimizing physician workplace stress and promoting policies that simultaneously minimize burnout and acute stress disorder (ASD) and decrease the risk of subsequent posttraumatic stress disorder (PTSD).
In addition to promoting those individual-based interventions discussed previously, radiology leadership should direct departmental resources toward creating a physically safe work environment and support the development of an infrastructure that allows radiologists and staff to work from home. This specific strategy is in line with many public health policies promoting containment and individual well-being such as the “Safer at Home” guidelines, advocated by the government of the State of Colorado [25]. The capacity to work from home is an advantage of the digital era and may have a positive impact on radiologist mental as well as physical health. For example, a flexible workplace environment centered at home mitigates several previously outlined sources of physician anxieties related to the pandemic, including fear about bringing the virus home to family and stress regarding the impact that contracting the virus may have on family resources, while also helping those who may be vulnerable, such as single parents or households where both parents work and are now required to cope with childcare requirements without outside resources [12]. Additionally, maintaining a healthy radiologist workforce in the setting of a pandemic requires the type of social distancing that is maximized with home quarantine. Therefore, developing an infrastructure whereby radiologists may care for patients directly from home is an asset that will support radiologist personal and family needs in multiple unforeseen ways in the era of COVID-19 and should be a key component of future pandemic preparedness.
Creating a work environment and culture where mental illness is not stigmatized may be challenging, but it is a critical step in establishing policies and practices whereby physicians are enabled to cura te ipsum, “heal themselves” [26] Developing psycho-educational seminars on the symptoms of PTSD and burnout with direction to the appropriate resources may be an essential first step for those who are affected but might not recognize the illness or symptoms in themselves. Additional efforts that may contribute to a culture where burnout and mental illness is not stigmatized may involve coordinating expert panel discussions on stress and PTSD, allowing dedicated time away from work to attend to mental health appointments and, in unprecedented times, considering nontraditional methods of physician engagement. For example, the field of narrative medicine leverages the arts and humanities as well as reflective writing exercises that allow health care providers the time and space necessary to access emotions and process experiences in a structured manner [27]. This contemplative environment facilitates cognitive reframing and self-compassion while helping to solidify professional identity and reinforce a sense of altruism at work, a factor previously shown to be protective from PTSD after a pandemic [7].
Finally, a sense of safety can be fostered through increased communication in an era in which information is constantly evolving. Clear and open lines of communication should be established between physicians and radiology leadership, and this should be a conversation with both value and time given to the voice of those with “boots on the ground” knowledge and experience. Optimizing high-performing teams in the workplace requires a culture of psychological safety and key components of psychological safety include trusting that one will not be punished for making a mistake or speaking one’s mind [28].
Finally, responding to the COVID-19 pandemic may be a time to recognize diverse personnel as a resource in the department. Radiology leadership may ask to hear from voices of those that may have worked through prior natural disasters, such as Hurricane Katrina or the World Trade Center terrorist attacks, when creating policies and procedures. These unique perspectives may add elements of both wisdom and hope to those of us navigating the complex uncharted territory of the COVID-19 pandemic.
As much as social distancing is being leveraged as a critical method of COVID-19 containment, both individual- and systems-based practices will be required to reduce workplace stress and burnout and minimize the acute stress response and risk of subsequent PTSD among health care providers. The mental health consequences for physicians related to this pandemic may be significant given the common drivers of burnout and PTSD and the high rate of underlying baseline burnout among radiologists [18]. As the COVID-19 pandemic has highlighted, the health care system in the United States is marred by imperfections. Taking good care of the physical as well the psychological well-being of physicians on the frontline of the COVID-19 pandemic should not be among them.
Take-Home Points
-
▪
Burnout and PTSD are both syndromes attributable to external stressors that have overlapping drivers, consequences, and interventions.
-
▪
Large-scale natural disasters and pandemics are associated with significant increases in mental health disorders among health care providers.
-
▪
High baseline physician burnout rates may exacerbate the acute traumatic stress posed by the COVID-19 pandemic, increasing the risk of mental health injury among health care providers.
-
▪
Early interventions may mitigate the mental health impact on providers.
-
▪
Both individual and systems-based strategies to reduce stress should be employed.
Footnotes
The authors state that they have no conflict of interest related to the material discussed in this article.
References
- 1.Collinson S. Virus confronts leader’s with one of modern history’s gravest challenges. CNN. https://www.cnn.com/2020/03/18/politics/donald-trump-coronavirus-leadership-challenge/index.html Available at: Published March 18, 2020. Accessed April 15, 2020.
- 2.Panagioti M., Geraghty K., Johnson J. Association between physician burnout and patient safety, professionalism, and patient satisfaction: a systematic review and meta-analysis. JAMA Intern Med. 2018;178:1317–1331. doi: 10.1001/jamainternmed.2018.3713. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 3.Post traumatic stress disorder: the management of PTSD in adults and children in primary and secondary care. NICE Clinical Guidelines, No. 26, National Collaborating Center for Mental Health. Gaskell; Leicester, UK: 2005. [PubMed] [Google Scholar]
- 4.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC; 2013.
- 5.Panagioti M., Panagopoulou E., Bower P. Controlled interventions to reduce burnout in physicians: a systematic review and meta-analysis. JAMA Intern Med. 2017;177:195. doi: 10.1001/jamainternmed.2016.7674. [DOI] [PubMed] [Google Scholar]
- 6.Dyrbye L.N., West C.P., Satele D. Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med. 2014;89:443–451. doi: 10.1097/ACM.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 7.UpToDate Acute stress disorder in adults: epidemiology, pathogenesis, clinical manifestations, course, and diagnosis. https://www.uptodate.com/contents/acute-stress-disorder-in-adults-epidemiology-pathogenesis-clinical-manifestations-course-and-diagnosis?search=acute%20stress%20disorder&source=search_result&selectedTitle=1∼41&usage_type=default&display_rank=1#H6576019 Available at:
- 8.Galea S., Merchant R.M., Lurie N. The mental health consequences of COVID-19 and physical distancing: the need for prevention and early intervention [E-pub ahead of print] JAMA Intern Med. 2020;180:817–818. doi: 10.1001/jamainternmed.2020.1562. [DOI] [PubMed] [Google Scholar]
- 9.Wu P., Fang Y., Guan Z. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry. 2009;54:302–311. doi: 10.1177/070674370905400504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Center for Disease Control and Prevention (CDC) Severe acute respiratory syndrome (SARS). SARS Basic Fact Sheet. https://www.cdc.gov/sars/about/fs-sars.html Available at:
- 11.Center for Disease Control and Prevention (CDC) Coronavirus 2019. Case of coronavirus (COVID-19) in the U.S. https://www.cdcgov/coronavirus/2019-ncov/cases-updates/cases-in-us.html Available at:
- 12.Shanafelt T., Ripp J., Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. 2020;323:2133–2134. doi: 10.1001/jama.2020.5893. [DOI] [PubMed] [Google Scholar]
- 13.Association of American Medical Colleges Diversity in facts and figures 2019. https://www.aamc.org/data-reports/workforce/interactive-data/figure-18-percentage-all-active-physicians-race/ethnicity-2018 Available at:
- 14.Williams M.T., Metzger I.W., Leins C., DeLapp C. Assessing racial trauma within a DSM–5 framework: The UConn Racial/Ethnic Stress & Trauma Survey. Practice Innovations. 2018;3:242–260. [Google Scholar]
- 15.National Action Plans Needed to Counter Intolerance COVID-19 fueling anti-Asian racism and xenophobia worldwide. Human Rights Watch. https://www.hrw.org/news/2020/05/12/covid-19-fueling-anti-asian-racism-and-xenophobia-worldwide Available at: Published May 12, 2020. Accessed May 14, 2020.
- 16.Cohen S.K. Pandemics: waves of disease, waves of hate from the plague of Athens to AIDS. Hist J. 2012;85:535–555. doi: 10.1111/j.1468-2281.2012.00603.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mealer M., Burnham E.L., Goode C.J., Rothbaum B., Moss M. The prevalence and impact of post-traumatic stress disorder and burnout syndrome in nurses. Depress Anxiety. 2009;26:1118–1126. doi: 10.1002/da.20631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chetlen A.L., Chan T.L., Ballard D.H. Adressing burnout in radiologists. Acad Radiol. 2019;26:526–533. doi: 10.1016/j.acra.2018.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shanefeldt T.D., Noseworthy J.H. Executive leadership and physician well-being: nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. 2017;92:129–146. doi: 10.1016/j.mayocp.2016.10.004. [DOI] [PubMed] [Google Scholar]
- 20.Fessell D., Cherniss C. Coronavirus disease 2019 (COVID-19) and beyond: micropractices for burnout prevention and emotional wellness [E-pub ahead of print] J Am Coll Radiol May 1 2020. 2020;17:746–748. doi: 10.1016/j.jacr.2020.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Israel-Cohen Y., Uzefovsky F., Kashy-Rosenbaum G., Kaplan O. Gratitude and PTSD symptoms among Israeli youth exposed to missile attacks: examining the mediation of positive and negative affect and life satisfaction. J Posit Psychol. 2015;10:99–106. [Google Scholar]
- 22.Hopwood T.L., Schutte N.S. A meta-analytic investigation of the impact of mindfulness-based interventions on post traumatic stress. Clin Psychol Rev. 2017;57:12–20. doi: 10.1016/j.cpr.2017.08.002. [DOI] [PubMed] [Google Scholar]
- 23.The American College of Radiology (ACR): Combatting the COVID-19 Pandemic: A collection of well being resources for radiologists. https://www.acr.org/Member-Resources/Benefits/Well-Being/COVID-19-Well-Being-Resources Available at:
- 24.Holman A., Garfin D.R., Silver R.C. Boston Marathon bombings, media, and acute stress. Proc Natl Acad Sci U S A. 2014;111:93–98. doi: 10.1073/pnas.1316265110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Colorado Department of Public Health and Environment Safer at home. https://covid19.colorado.gov/safer-at-home Available at:
- 26.The Phrase Finder Physician heal thyself: meaning and origin. Phrases.Org. https://www.phrases.org.uk/meanings/281850.html Available at:
- 27.Charon R. Narrative medicine: a model for empathy, reflection, profession and trust. JAMA. 2001;286:1897–1902. doi: 10.1001/jama.286.15.1897. [DOI] [PubMed] [Google Scholar]
- 28.Delazona L. High performing teams need psychological safety. Here’s how to create it. Harv Bus Rev August 24, 2017. https://hbr.org/2017/08/high-performing-teams-need-psychological-safety-heres-how-to-create-it Available at: