Abstract
Purpose of Review
The orientation of the spine relative to the pelvis—particularly that in the sagittal plane—has been shown in both kinematic and radiographic studies to be paramount in governance of acetabular alignment during normal bodily motion. The purpose of this review is to better understand the challenges faced by arthroplasty surgeons in treating patients that have concurrent lumbar disease and are therefore more likely to have poorer clinical outcomes after THA than in patients without disease.
Recent Findings
The concept of an “acetabular safe zone” has been well described in the past regarding the appropriate orientation of acetabular component in THA. However, this concept is now under scrutiny, and rising forth is a concept of functional acetabular orientation that is based on clinically evaluable factors that are patient and motion specific.
Summary
The interplay between the functional position of the acetabulum and the lumbar spine is complex. The challenges that are thereby faced by arthroplasty surgeons in terms of proper acetabular cup positioning when treating patients with concomitant lumbar disease need to be better understood and studied, so as to prevent catastrophic and costly complications such as periprosthetic joint dislocations and revision surgeries.
Keywords: Spinopelvic mobility, Total hip arthroplasty, Lumbar spinal fusion, Acetabular cup position
Introduction
The orientation of the acetabular component in the sagittal plane is intrinsically linked to the mobility of the lumbosacral region and the dynamic position of the pelvis. Patient specific understanding of the dynamic relationship between the spine and pelvis has led to a concept of functional acetabular orientation. Knowledge of sagittal pelvic kinematics is essential for appropriate placement of acetabular components in total hip arthroplasty to optimize and avoid instability, impingement, and dislocation.
Spinopelvic Parameters
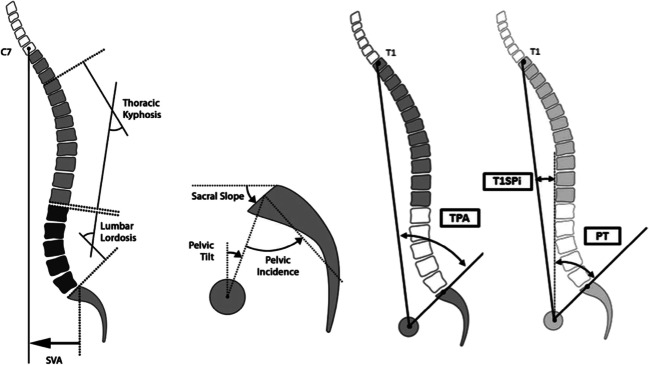
The orientation of the pelvis in the sagittal plane is commonly described utilizing three radiographic angles as measured on standing lateral lumbopelvic radiographs: pelvic tilt, sacral slope, and pelvic incidence (Fig. 1) [1]. Pelvic tilt (PT) is the angle between the vertical and a line extending from the midpoint of the superior sacral endplate to the bicoxofemoral axis [1]. Its value is positional and denotes the spatial orientation of the pelvis in relation to the spine. In hip arthroplasty literature, anterior pelvic plane (APP) is used synonymously with pelvic tilt to describe the rotational profile of the pelvis in the sagittal plane [2, 3]. Defined by a line that connects the pubic symphysis to the anterior superior iliac spine, the APP serves as a reference during navigation for implantation of acetabular components [4].
Fig. 1.
Spinopelvic parameters. From Delsole EM, Vigdorchik JM, Schwarzkopf R, Errico TJ, and Buckland AJ. Total hip arthroplasty in the spinal deformity population: does degree of sagittal deformity affect rates of safe zone placement, instability, or revision? J Arthroplasty. 2017; 32(6):1910–1917
Sacral slope (SS) is a parameter that denotes the angle between a line parallel to the superior endplate of S1 and the horizontal plane [1]. Changes in pelvic rotation have direct inverse effects on the value of the sacral slope (SS) and pelvic tilt (PT). When added to the pelvic tilt, a third value is created (SS + PT = PI), the pelvic incidence (PI). Unlike the sacral slope (SS) and pelvic tilt (PT), pelvic incidence (PI) is not position dependent and remains an anatomic constant for every person [1, 5]. Pelvic incidence is a morphologic parameter that relates the bicoxofemoral axis to the obliquity of the sacrum relative to the ilium [5]. It denotes the natural shape of the sacrum which defines the optimal and appropriate lumbar lordosis of each patient during reconstructive spinal surgeries (see the “Sagittal Spinal Deformity” section) [1].
Sagittal Spinopelvic Mobility
Changes in pelvic rotation in the sagittal plane are dependent on the flexibility of the lumbar spine [5]. In the standing position, the pelvis is in a forwardly (anteriorly) rotated position (low pelvic tilt, high lumbar lordosis) allowing the axial skeleton’s center of gravity to closely align with the center of rotation of the femoral head. With transition to sitting, the pelvis rotates posteriorly with a corresponding decrease in the curvature of the lumbar spine (increased pelvic tilt).
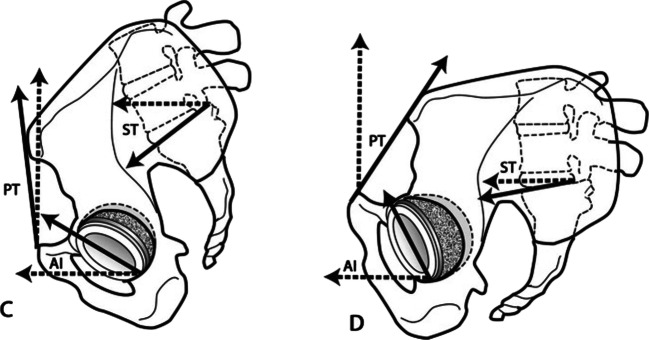
Rotation of the pelvis in the sagittal plane is directly linked to the spatial profile of the acetabulum. With forward (anterior) rotation of the pelvis (decreased PT), the anteversion of the acetabulum decreases. By contrast, a transition from standing to sitting causes the acetabulum to assume a more anteverted position and a more posteriorly rotated pelvis. (Fig. 2). Observation studies have computed that every one-degree of pelvic tilt corresponds to a 0.7-degree change in acetabular version [6].
Fig. 2.
Relationship between pelvic rotation and acetabular anteversion during postural changes. Picture on left (labeled C) is standing and right (labeled D) is sitting. From Kanawade V, Dorr LD, Wan Z. Predictability of acetabular component angular change with postural shift from standing to sitting position. J Bone Joint Surg Am. 2014; 96(12):978–986
Functional Acetabular Orientation
Knowledge of sagittal spinopelvic mobility has led to a new concept of functional acetabular orientation that has challenged the notion of a static acetabular safe zone. In 1978, Lewinnek et al. proposed that optimal positioning of the acetabular cup with anteversion of 15 ± 10° and an inclination of 40 ± 10° was associated with a decrease incidence of dislocation in primary total hip arthroplasty [7]. Over the last decade, numerous articles have demonstrated limited correlation between the Lewinnek’s safe zone and the incidence of THA dislocation. Abdel et al. reviewed 9784 primary THA and found that the majority of patients (58%) that dislocated were within the safe zone [8]. Similarly, Esposito et al. examined 147 dislocators in a database of 7040 primary THA and found no difference among the radiographic zones [9]. Furthermore, computer models depict impingement in up to 80% of individuals during squatting, picking up, and low chair rise despite acetabular component placement within Lewinnek’s safe zone [10].
Current research demonstrates dynamic pelvic rotation during physiologic changes in posture changes (PT) varies by a mean 10–14° in healthy individuals between supine and standing [11, 12]. When correlating this with acetabular changes, postural changes correspond to approximately 10-degree variations in acetabular cup version [12]. In their study, Au and colleagues demonstrated 53% of the acetabular cups thought to be inside the safe zone on supine images deviated outside the safe zone on standing images [12]. Tiberi et al. showed that 43% of acetabular cups outside the safe zone became well-positioned and 31% of well-positioned cups fell outside of the safe zone when x-rays were obtained standing [13]. Thus, a growing body of literature supports the concept that a static safe zone is overly simplistic [10]. Although any two patients may have similar spinopelvic parameters during static supine radiographs, their pelvic tilt and acetabular orientation during sitting or standing may be different depending on spinopelvic mobility [14].
Instability, Impingement, and Dislocation
The sagittal orientation of the acetabular component is intrinsically linked to total hip stability. Mechanistically, an increase in acetabular anteversion is protective against posterior dislocation due to an increase in posterior acetabular coverage and decrease risk of anterior impingement of the femoral neck on the acetabular component [11, 15]. The increased anteversion does, however, place patients at increased risk of posterior impingement and anterior dislocation. By contrast, low anteversion or neutral positioning of the acetabular component is protective against anterior dislocation but places patients at risk of anterior impingement and posterior dislocation [15].
Concurrent Lumbar Disease
Concurrent degeneration of the spine and pelvis has long been acknowledged but until recently, a knowledge gap existed in the understanding of how the appendicular and axial skeleton interacts between spine and hip surgeons [16–18]. Patients with lumbar pathology who undergo primary total hip arthroplasty have worse clinical outcomes with higher rates of dislocation and revision surgery [17–20].
Historically reported incidence of dislocation is commonly believed to occur in 1–3% of primary total hip replacements [21]. In patients with concurrent lumbar disease, rates of dislocation have been widely reported with incidence between 3 and 16% [18, 22]. The widely reported incidence is not only the result of small case series but also due to a heterogenous population of patients with and without prior spine fusion surgery. Using a state-wide database, Perffetti et al. evaluated the incidence of dislocation in patients with prior spinal fusion [20•]. Using a propensity score-matched pair analysis, a seven time–increased incidence of dislocation was observed in patients with prior fusion in comparison with controls [20•].
A time-dependent relationship has been observed in patient with lumbar fusions who has dislocation events. In their study, Perffetti et al. demonstrate that over three-fourths of dislocations that occurred in patients with prior spinal fusion occurred within 12 months postoperatively, whereas only 25% of the control group occurred during that time period [20•]. While dislocations that occur after 1 year are suggestive of polyethylene wear or stretching of soft tissues, dislocations in the first few months postoperatively likely represent mechanical instability from component mal-positioning [20•].
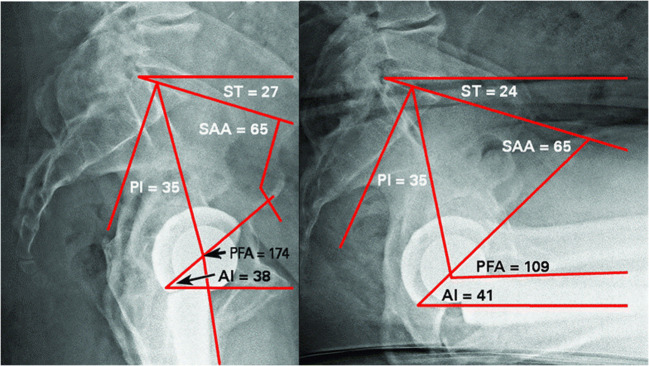
In the normal flexible spine, the pelvis undergoes natural rollback (increased PT) with postural changes from standing to sitting (Fig. 3) [22]. The resultant increase in acetabular anteversion decreases the likelihood of posterior dislocation for two reasons. First, the increased acetabular anteversion creates additional acetabular coverage posteriorly providing a buttress effect to posterior dislocation. Second, the increased anteversion makes room for the femoral prosthesis during hip flexion thereby decreasing the likelihood of anterior femoroacetabular impingement [3, 22]. In patients with prior lumbar fusion, an increased rigidity is seen in the lumbrosacral complex that prevents natural rollback of the pelvis during sitting. The acetabulum is, thus, maintained in a relatively retroverted position placing it at risk of anterior impingement and posterior dislocation [3, 22].
Fig. 3.
Standing (left image) and sitting (right image) lateral radiographs. Note increased pelvic tilt with corresponding acetabular rollback (increased anteversion) when transitioning from standing to sitting. From: 39. Stefl M, Lundergan W, Heckmann N, et al. Spinopelvic mobility and acetabular component position for total hip arthroplasty. Bone Joint J. 2017; 99-B(1 Supple A):37–45
As rigidity of the lumbar spine increases, the incidence of dislocation has been observed to increase [18, 23]. Sing et al. showed that patients with three or more fusion levels had a dislocation rate of 7.5%, whereas those with less than three levels had an incidence of 4.2% [23]. Furthermore, research has shown that patients with lumbopelvic rigidity require increased hip flexion to rise from a seated position [24, 25] Esposito et al. demonstrated patients with stiff spines have 10-degree less flexion through the lumbar spine and compensate with 10-degree additional femoroacetabular flexion when rising from a seating position [25]. The increase in pelvic-hip flexion angles places patients with lumbar rigidity at further increased risk of anterior femoroacetabular impingement and dislocation.
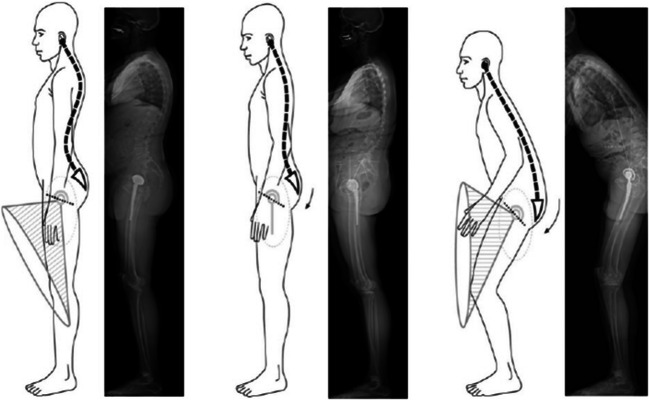
Sagittal Spinal Deformity
Natural global spinal alignment positions the head and trunk in line with the weight bearing axis of the pelvis and lower extremity. Patients with pathologic alignment of the spine develop imbalance in the sagittal plane with forward displacement of the head/trunk in relation to the pelvis [26]. To maintain upright posture, patients compensate with retroversion of the pelvis (increase pelvic tilt) with corresponding hip and knee flexion (Fig. 4) [3]. In patients undergoing spinal deformity correction, re-establishing normal economic posture has been linked to improved outcomes and quality of life [27]. Past studies have shown optimal alignment with pelvic tilt < 22° and/or lumbar lordosis within 11° of pelvic incidence [1, 27].
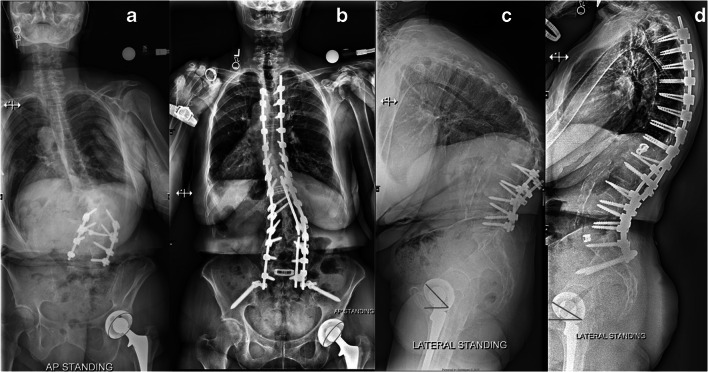
Fig. 4.
Lateral body radiographs with corresponding diagrams demonstrating worsening sagittal balance with compensatory pelvic retroversion and knee flexion. Note change in acetabular anteversion corresponding to changes in global body alignment. From: Hu J, Qian BP, Qiu Y, et al. Can acetabular orientation be restored by lumbar pedicle subtraction osteotomy in ankylosing spondylitis patients with thoracolumbar kyphosis? Eur Spine J. 2017; 26(7):1826–1832
Patients with sagittal imbalance are unique as changes in spinal alignment and pelvic tilt impacts the orientation of the acetabulum in the sagittal plane (Fig. 5). If a patient has a native acetabulum, the corresponding effect of spinal re-alignment only affects the portion of articular cartilage that bears weight. However, if a patient has a total hip arthroplasty, a change in pelvic tilt results in potential impingement and dislocation. DelSole and colleagues published outcomes data on patients with primary THA with concurrent sagittal spine deformity who have not undergone spinal treatment [28••]. They found an 8% dislocation rate and 5.8% revision rate although duration of follow-up in their study was not specified. While dislocators had a high rate of safe zone placement on both supine and standing films, the authors showed that patients with an unbalanced pelvis (increased PT and PI-LL mismatch) were statistically more common to have dislocation events than were patients with a balanced pelvis [28••].
Fig. 5.
Acetabular version changes with spinal deformity correction. From: Buckland AJ, Vigdorchik J, Schwab FJ, et al. Acetabular anteversion changes due to spinal deformity correction: bridging the gap between hip and spine surgeons. J Bone Joint Surg Am. 2015; 97(23):1913–20
Other recent studies by Buckland and Barry suggest that spinal realignment surgery in patients with prior THA has predictable changes in acetabular anteversion with correction of pelvic tilt and lumbar lordosis [3, 19]. Berry demonstrated a 7-degree change in acetabular version after three-column osteotomy of the spine [19]. Buckland showed patients with sagittal spinal deformity had a high prevalence (68%) of excessively anteverted acetabular components defined as greater than 25 degrees of anteversion [3]. With restoration of sagittal alignment, a 1-degree of acetabular retroversion occurred with every 1.1-degree change in pelvic rotation and 3.1-degree increase in lumbar lordosis [3]. Thus, patients with prior well-placed acetabular components are at risk of dislocation after spinal corrective surgery. The results by Buckland, Berry, and Shroeder suggest including the impact of spinal deformity correction on the orientation of acetabular components during informed consent in patient with prior THAs [3, 19, 29].
Ankylosing Spondylitis
Patients with ankylosing spondylitis commonly have concurrent spine and hip involvement allowing a homogenized cohort to study the interaction between the two diseases. The characteristic spinal deformity in ankylosing spondylitis is thoracolumbar kyphosis with corresponding knee flexion, hip extension, and pelvic retroversion in order to tilt the rigid lumbopelvic segment of the spine upright [30, 31]. The high pelvic tilt seen in patients with ankylosing spondylitis drives the acetabulum into a highly anteverted position. Whereas normal individuals have anteversion of approximately 20° [32], patients with thoracolumbar kyphosis secondary to ankylosing spondylitis have been observed to have mean acetabular anteversion of 31.4° [33•].
After primary total hip arthroplasty, high rates of anterior hip dislocations have been observed in patients with ankylosing spondylitis [26, 31]. Through a stereolithographic model, Tang et al. showed that patients with ankylosing spondylitis present with hip hyperextension and fixed pelvic retroversion (high PT) that do not significantly change with sitting or standing [30]. If the fixed deformity is not accounted for, intraoperative placement of acetabular components in excessive anteversion frequently occurs which may lead to posterior impingement of the prosthetic neck or greater trochanter causing anterior instability and potentially dislocation [34]. In a computer model, Tang et al. showed that positioning of the acetabular component in less acetabular anteversion is appropriate for any patient with increased pelvic tilt [30]. Through their computer model, the authors suggested adjusting the acetabular component 5° for every 10° of pelvic rotation [30].
Debate exists whether patients with ankylosing spondylitis should undergo hip arthroplasty or spine corrective surgery first. Proponents of early correction of the hip pathology advocate that the improvement in range of motion of the hip after correction of the hip flexion deformity allows for a more precise calculation of the residual spinal deformity after the hip flexion contracture is corrected [35]. In 2014, Zheng et al. observed significantly lower rates of hip dislocations in patients with ankylosing spondylitis who underwent spinal deformity correction prior to hip arthroplasty [26]. More recently, Hu et al. demonstrated normalization of global sagittal alignment after three-column osteotomy in the lumbar spine. In their patient population, pelvic tilt improved from 38 to 23° with a decrease in 11° of acetabular anteversion [33•]. The authors concluded that spinal deformity correction prior to hip arthroplasty allowed correction of patient’s pelvic retroversion with normalization of the acetabular anteversion [33•].
Conclusion
The position of the acetabular component plays a dominant role in the stability and longevity of total hip replacements [36]. Modern research supports that optimal positioning of the acetabular cup is dependent on the sagittal pelvic mobility. Future clinical outcome research is required to establish whether patient-specific, kinematic aligned acetabular components can reduce the incidence of dislocation or improve clinical outcomes. Standardized algorithms for placement of kinematically aligned acetabular components need to be developed and prospectively evaluated.
Compliance with Ethical Standards
Conflict of Interest
Thomas E. Niemeier, Bradley W Wills, Steven M Theiss, and Shane F strom declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Schwab FJ, Blondel B, Bess S, Hostin R, Shaffrey CI, Smith JS, Boachie-Adjei O, Burton DC, Akbarnia BA, Mundis GM, Ames CP, Kebaish K, Hart RA, Farcy JP, Lafage V, International Spine Study Group (ISSG) Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine. 2013;38(13):E803–E812. doi: 10.1097/BRS.0b013e318292b7b9. [DOI] [PubMed] [Google Scholar]
- 2.Legaye J. Influence of the sagittal balance of the spine on the anterior pelvic plane and on the acetabular orientation. Int Orthop. 2009;33(6):1695–1700. doi: 10.1007/s00264-008-0702-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Buckland AJ, Vigdorchik J, Schwab FJ, Errico TJ, Lafage R, Ames C, Bess S, Smith J, Mundis GM, Lafage V. Acetabular anteversion changes due to spinal deformity correction: bridging the gap between hip and spine surgeons. J Bone Joint Surg Am. 2015;97(23):1913–1920. doi: 10.2106/JBJS.O.00276. [DOI] [PubMed] [Google Scholar]
- 4.Wohlrab D, Radetzki F, Noser H, Mendel T. Cup positioning in total hip arthoplasty: spatial alignment of the acetabular entry plane. Arch Orthop Trauma Surg. 2012;132(1):1–7. doi: 10.1007/s00402-011-1379-1. [DOI] [PubMed] [Google Scholar]
- 5.Le Huec JC, Aunoble S, Philippe L, Nicolas P. Pelvic parameters: origin and significance. Eur Spine J. 2011;20(Suppl 5):564–571. doi: 10.1007/s00586-011-1940-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lembeck B, Mueller O, Reize P, Wuelker N. Pelvic tilt makes acetabular cup navigation inaccurate. Acta Orthop. 2005;76(4):517–523. doi: 10.1080/17453670510041501. [DOI] [PubMed] [Google Scholar]
- 7.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60(2):217–220. doi: 10.2106/00004623-197860020-00014. [DOI] [PubMed] [Google Scholar]
- 8.Abdel MP, Von Roth P, Jennings MT, Hanssen AD, Pagnano MW. What safe zone? The vast majority of dislocated THAs are within the Lewinnek safe zone for acetabular component position. Clin Orthop Rel at Res. 2016;474(2):386–391. doi: 10.1007/s11999-015-4432-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Esposito CI, Gladnick BP, Lee YY, Lyman S, Wright TM, Mayman DJ, Padgett DE. Cup position alone does not predict risk of dislocation after hip arthroplasty. J Arthroplast. 2015;30(1):109–113. doi: 10.1016/j.arth.2014.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mccarthy TF, Alipit V, Nevelos J, Elmallah RK, Mont MA. Acetabular cup anteversion and inclination in hip range of motion to impingement. J Arthroplast. 2016;31(9 Suppl):264–268. doi: 10.1016/j.arth.2016.01.067. [DOI] [PubMed] [Google Scholar]
- 11.Lazennec JY, Boyer P, Gorin M, Catonné Y, Rousseau MA. Acetabular anteversion with CT in supine, simulated standing, and sitting positions in a THA patient population. Clin Orthop Relat Res. 2011;469(4):1103–1109. doi: 10.1007/s11999-010-1732-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Au J, Perriman DM, Neeman TM, Smith PN. Standing or supine x-rays after total hip replacement - when is the safe zone not safe? Hip Int. 2014;24(6):616–623. doi: 10.5301/hipint.5000173. [DOI] [PubMed] [Google Scholar]
- 13.Tiberi JV, Antoci V, Malchau H, Rubash HE, Freiberg AA, Kwon YM. What is the fate of total hip arthroplasty (THA) acetabular component orientation when evaluated in the standing position? J Arthroplast. 2015;30(9):1555–1560. doi: 10.1016/j.arth.2015.03.025. [DOI] [PubMed] [Google Scholar]
- 14.Ochi H, Baba T, Homma Y, Matsumoto M, Nojiri H, Kaneko K. Importance of the spinopelvic factors on the pelvic inclination from standing to sitting before total hip arthroplasty. Eur Spine J. 2016;25(11):3699–3706. doi: 10.1007/s00586-015-4217-2. [DOI] [PubMed] [Google Scholar]
- 15.Pierrepont J, Hawdon G, Miles BP, Connor BO’, Baré J, Walter LR, Marel E, Solomon M, McMahon S, Shimmin AJ. Variation in functional pelvic tilt in patients undergoing total hip arthroplasty. Bone Joint J. 2017;99-B(2):184–191. doi: 10.1302/0301-620X.99B2.BJJ-2016-0098.R1. [DOI] [PubMed] [Google Scholar]
- 16.Mcnamara MJ, Barrett KG, Christie MJ, Spengler DM. Lumbar spinal stenosis and lower extremity arthroplasty. J Arthroplast. 1993;8(3):273–277. doi: 10.1016/S0883-5403(06)80089-6. [DOI] [PubMed] [Google Scholar]
- 17.Prather H, van Dillen LR, Kymes SM, Armbrecht MA, Stwalley D, Clohisy JC. Impact of coexistent lumbar spine disorders on clinical outcomes and physician charges associated with total hip arthroplasty. Spine J. 2012;12(5):363–369. doi: 10.1016/j.spinee.2011.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Buckland AJ, Puvanesarajah V, Vigdorchik J, et al. Dislocation of a primary total hip arthroplasty is more common in patients with a lumbar spinal fusion. Bone Joint J. 2017;99-B(5):585–591. doi: 10.1302/0301-620X.99B5.BJJ-2016-0657.R1. [DOI] [PubMed] [Google Scholar]
- 19.Barry JJ, Sing DC, Vail TP, Hansen EN. Early outcomes of primary total hip arthroplasty after prior lumbar spinal fusion. J Arthroplast. 2017;32(2):470–474. doi: 10.1016/j.arth.2016.07.019. [DOI] [PubMed] [Google Scholar]
- 20.Perfetti DC, Schwarzkopf R, Buckland AJ, Paulino CB, Vigdorchik JM. Prosthetic dislocation and revision after primary total hip arthroplasty in lumbar fusion patients: a propensity score matched-pair analysis. J Arthroplasty. 2017;32(5):1635–1640.e1. doi: 10.1016/j.arth.2016.11.029. [DOI] [PubMed] [Google Scholar]
- 21.Sanchez-sotelo J, Berry DJ. Epidemiology of instability after total hip replacement. Orthop Clin North Am. 2001;32(4):543–552. doi: 10.1016/S0030-5898(05)70225-X. [DOI] [PubMed] [Google Scholar]
- 22.Bedard NA, Martin CT, Slaven SE, Pugely AJ, Mendoza-lattes SA, Callaghan JJ. Abnormally high dislocation rates of total hip arthroplasty after spinal deformity surgery. J Arthroplast. 2016;31(12):2884–2885. doi: 10.1016/j.arth.2016.07.049. [DOI] [PubMed] [Google Scholar]
- 23.Sing DC, Barry JJ, Aguilar TU, et al. Prior lumbar spinal arthrodesis increases risk of prosthetic-related complication in total hip arthroplasty. J Arthroplasty. 2016;31(9 Suppl):227–232.e1. doi: 10.1016/j.arth.2016.02.069. [DOI] [PubMed] [Google Scholar]
- 24.Stefl M, Lundergan W, Heckmann N, et al. Spinopelvic mobility and acetabular component position for total hip arthroplasty. Bone Joint J. 2017;99-B(1 Supple A):37–45. doi: 10.1302/0301-620X.99B1.BJJ-2016-0415.R1. [DOI] [PubMed] [Google Scholar]
- 25.Esposito CI, Miller TT, Kim HJ, Barlow BT, Wright TM, Padgett DE, Jerabek SA, Mayman DJ. Does degenerative lumbar spine disease influence femoroacetabular flexion in patients undergoing total hip arthroplasty? Clin Orthop Relat Res. 2016;474(8):1788–1797. doi: 10.1007/s11999-016-4787-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zheng GQ, Zhang YG, Chen JY, Wang Y. Decision making regarding spinal osteotomy and total hip replacement for ankylosing spondylitis: experience with 28 patients. Bone Joint J. 2014;96-B(3):360–365. doi: 10.1302/0301-620X.96B3.32774. [DOI] [PubMed] [Google Scholar]
- 27.Smith JS, Klineberg E, Schwab F, Shaffrey CI, Moal B, Ames CP, Hostin R, Fu KMG, Burton D, Akbarnia B, Gupta M, Hart R, Bess S, Lafage V, International Spine Study Group Change in classification grade by the SRS-Schwab adult spinal deformity classification predicts impact on health-related quality of life measures: prospective analysis of operative and nonoperative treatment. Spine. 2013;38(19):1663–1671. doi: 10.1097/BRS.0b013e31829ec563. [DOI] [PubMed] [Google Scholar]
- 28.Delsole EM, Vigdorchik JM, Schwarzkopf R, Errico TJ, Buckland AJ. Total Hip arthroplasty in the spinal deformity population: does degree of sagittal deformity affect rates of safe zone placement, instability, or revision? J Arthroplasty. 2017;32(6):1910–1917. doi: 10.1016/j.arth.2016.12.039. [DOI] [PubMed] [Google Scholar]
- 29.Schroeder JE, Jerabek S, Sama A, Kaplan L, Girardi F, Lebl DR. The effect of 3-column spinal osteotomy on anterior pelvic plane and acetabulum position. Am J Orthop. 2014;43(7):E133–E136. [PubMed] [Google Scholar]
- 30.Tang WM, Chiu KY, Kwan MF, Ng TP. Sagittal pelvic mal-rotation and positioning of the acetabular component in total hip arthroplasty: three-dimensional computer model analysis. J Orthop Res. 2007;25(6):766–771. doi: 10.1002/jor.20225. [DOI] [PubMed] [Google Scholar]
- 31.Tang WM, Chiu KY. Primary total hip arthroplasty in patients with ankylosing spondylitis. J Arthroplast. 2000;15(1):52–58. doi: 10.1016/S0883-5403(00)91155-0. [DOI] [PubMed] [Google Scholar]
- 32.Murphy SB, Kijewski PK, Millis MB, Harless A. Acetabular dysplasia in the adolescent and young adult. Clin Orthop Relat Res. 1990;261:214–223. [PubMed] [Google Scholar]
- 33.Hu J, Qian BP, Qiu Y, et al. Can acetabular orientation be restored by lumbar pedicle subtraction osteotomy in ankylosing spondylitis patients with thoracolumbar kyphosis? Eur Spine J. 2017;26(7):1826–1832. doi: 10.1007/s00586-016-4709-8. [DOI] [PubMed] [Google Scholar]
- 34.Bhan S, Eachempati KK, Malhotra R. Primary cementless total hip arthroplasty for bony ankylosis in patients with ankylosing spondylitis. J Arthroplast. 2008;23(6):859–866. doi: 10.1016/j.arth.2007.07.014. [DOI] [PubMed] [Google Scholar]
- 35.Walker LG, Sledge CB. Total hip arthroplasty in ankylosing spondylitis. Clin Orthop Relat Res. 1991;262:198–204. [PubMed] [Google Scholar]
- 36.Kanawade V, Dorr LD, Wan Z. Predictability of acetabular component angular change with postural shift from standing to sitting position. J Bone Joint Surg Am. 2014;96(12):978–986. doi: 10.2106/JBJS.M.00765. [DOI] [PubMed] [Google Scholar]