Abstract
Purpose of Review
The purposes of this review are to describe the epidemiology, treatment options, and clinical outcomes of revision medial ulnar collateral ligament reconstruction in baseball pitchers.
Recent Findings
Rates of revision UCL range from 1 to 15% and have slowly increased over the past several years. Revision UCL procedures are associated with higher complication rates, likely due to the distortion of innate anatomy after primary reconstruction. Techniques for reconstruction are largely influenced by the index surgery and integrity of the ulnar and humeral bone tunnels/sockets. Current literature reporting on the outcomes following revision UCL reconstruction is limited to case series and database studies. Mean time between primary reconstruction and revision surgery is approximately 5 years and return to play rates range from 47 to 85%.
Summary
Outcomes following revision UCL reconstruction are relatively guarded compared with those of primary UCL reconstruction with the most studies reporting lower return to play rates, decreased workloads compared with pre-injury levels of play, and shorter career longevity following revision surgery. Future research regarding optimal reconstruction techniques and post-operative rehabilitation are needed as the incidence and demand for this procedure is expected to increase.
Keywords: Revision, Ulnar collateral ligament, Tommy John surgery, Return to sport, Pitching, Major League Baseball
Introduction
Surgical reconstruction of the medial ulnar collateral ligament (UCL) was first performed in 1974 and significantly changed the management of UCL injuries, specifically among competitive baseball pitchers [1]. There has been a steady rise in the prevalence of UCL reconstruction surgery over time with up to 26% of Major League Baseball (MLB) and 19% of Minor League Baseball (MiLB) pitchers undergoing UCL reconstruction at some point in their career [2]. One study evaluating a 40-year period found that the rate of revision UCL reconstructions substantially increased from 7.5 procedures per year to 20.25 procedures per year from 2007 to 2014 [3]. Camp et al. reviewed the findings of 1429 professional pitchers who underwent UCL reconstruction and also found a steadily increasing rate of surgery in both Major and Minor League Baseball (MiLB) players with MiLB players accounting for at least half of the UCL reconstruction surgeries beyond 2007 [4•]. Although UCL insufficiency was originally considered to be a career-ending injury, improvements in surgical technique, rehabilitation protocols, and appropriate return to throwing protocols have led to more recent data demonstrating that professional pitchers are now returning to play (RTP) at acceptably high rates of 80 to 90% [4•, 5–7].
With a steady rise in primary UCL reconstructions, a concurrent rise in revision procedures has been well documented, with some studies suggesting the that the rising rate of revision surgery is actually outpacing that of primary UCL surgery [4•, 8–10]. Although the surgical techniques and outcomes of primary UCL reconstruction have been well studied, the literature on revision UCL reconstructions is less robust. Accordingly, the purposes of this clinical review are to summarize the findings of the current data available for revision UCL reconstruction and discuss technical pearls and outcomes.
Epidemiology
The reported rate of revision UCL reconstruction varies from 1 to 15% [3, 5, 9•, 11–13]. Earlier studies which reported revision UCL rates of 1–2% included athletes with any overhead component, including sports such as wrestling, soccer, gymnastics, cheerleading, and pole vaulting [5]; this is in sharp contrast to the observed revision rate among baseball pitchers, which is much higher at 5–15% [5, 13]. In a study of professional baseball pitchers, there was an increasing trend of revision UCL from 2010 to 2016 in both MLB and MiLB players [10]. In this work, the overall mean revision UCL rate was 6.7%, with a rate of 9.4% in MLB and 5.2% in MiLB players (p = 0.004).
Factors associated with revision UCL reconstruction include pitchers who undergo primary UCL reconstruction at an earlier age [14•] and having less MLB experience [15•] compared with those who did not require revision surgery (Table 1). Keller et al. also found that pitchers whom progressed to revision surgery had a higher pitching workload and pitched more games compared with their pre-reconstruction state compared with those who did not require revision [14•]. Therefore, it was recommended that pitchers undergoing primary reconstructions should reduce their pitching workload in relation to their pre-reconstruction workload to reduce the risk of revision surgery.
Table 1.
Risk factors associated with UCL revision
| Younger age at initial reconstruction | |
| Shorter stature | |
| Increased frequency of fastball use | |
| Less experience in MLB before initial reconstruction | |
| Fewer pitches thrown throughout first year after initial reconstruction | |
| Longer time to return to play after initial reconstruction | |
| Increased post-reconstruction number of games pitched compared with pre-reconstruction | |
| Decreased post-reconstruction number of innings pitched compared with pre-reconstruction |
Summary of published risk factors associated with increased rates of UCL revision surgery [14•, 15•]
Interestingly, the length of recovery has demonstrated no correlation to the risk of UCL revision in MiLB and MLB pitchers [16]. Furthermore, it was found that there was no difference in UCL revision rates between MLB and MiLB players (6.7% and 4.4%, respectively, p = 0.264) [17]. Erickson et al. reported no difference in length of time between index UCL reconstruction and return to play (RTP) in those that had progressed to UCL revision and those that did not require revision at any professional level. Lastly, variables such as age, hand dominance, and pitching role have shown no significant impact on rates of UCL revision [17].
Evaluation and Workup
Evaluation of the high-level athlete with a suspected UCL re-injury begins with a thorough history. Certain details may be important in forming the diagnosis and choosing a treatment, for example, characterization of symptoms (pain, weakness, numbness, etc.), duration of symptoms (acute vs. chronic), alleviating or exacerbating factors, sport and position, and frequency of throwing or pitching. Physicians should also determine if there were any notable changes in throwing after the injury, such as reduced velocity, accuracy, or stamina. It is important to discuss any previous injuries or surgeries, particularly to the throwing shoulder, elbow, or hand, as elbow surgery prior to the index UCL reconstruction is associated with worse outcomes [18].
Given that the patient has already had a prior UCL reconstruction, details regarding surgical technique, graft type, ulnar nerve treatment, and any concomitant procedures are imperative to know when considering revision surgery. Furthermore, details of the patient’s previous therapy and throwing rehabilitation following their primary surgery should be discussed as this may represent an area needing adjustment. Lastly, motivation, career goals, level of competition, and anticipated future career length are all important factors to consider as they will likely influence treatment, outcomes, and patient expectations. It is important that patients understand UCL revisions are associated with inferior outcomes compared with primary reconstructions and that they may not return to play at the same pre-injury level of competition [19].
The physical examination of the patient with a failed UCL reconstruction is largely consistent with evaluation at the time of index injury. However, key differences include palpation along the length of the UCL to elucidate the specific location of any tears, such as humeral vs. ulnar-sided graft failure, and any gross post-operative changes. The integrity of the UCL graft should be assessed by performing maneuvers that place the elbow under valgus stress; opening of the medial aspect of the joint more than 1 mm is abnormal and may indicate partial or complete graft failure [20]. Additionally, the physician should specifically examine for other symptoms that may need to be addressed at the time of surgery, such as ulnar nerve irritation, posteromedial impingement, presence of loose bodies, osteophytes, injury to the flexor-pronator mass, or excessive scar tissue.
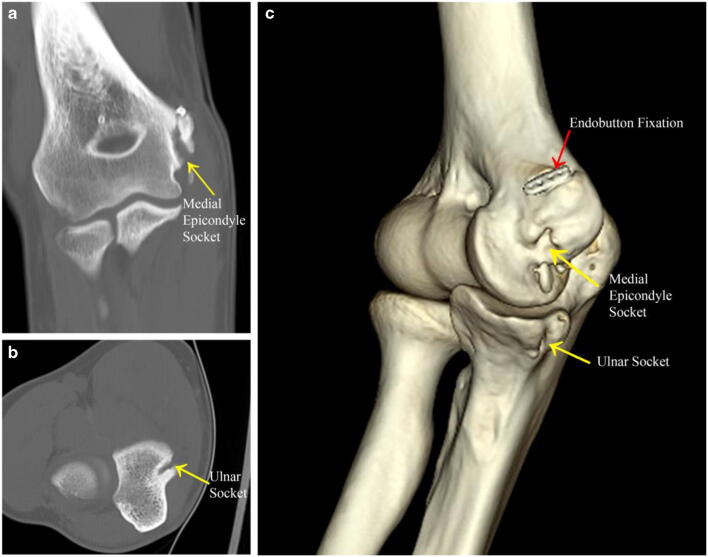
Imaging studies should start with routine radiographs, including AP and lateral views; however, these may often be negative. Occasionally, tunnel osteolysis or fracture may be visible, in addition to any metallic implants used in the index procedure. Additional radiographs may be helpful, including an oblique view to evaluate the olecranon, and a valgus stress view to assess for opening of the medial side, with > 3 mm being diagnostic [21]. These are particularly helpful in evaluating the condition of prior bone tunnels, presence of tunnel osteolysis, avulsion fragments, loose bodies, metallic implants from the index procedure, graft calcifications [22, 23], or fractures. MRI is the ideal imaging modality to best assess soft tissue structures and status of the UCL graft; however, the appearance of the primary UCL graft as it progresses through the healing and ligamentization process has not yet been fully characterized. Therefore, the appearance of the graft and overall utility of MRI will likely vary depending on the amount of time elapsed since the primary surgery. In recent years, there is growing support for ultrasound evaluation of UCL injuries, particularly in the setting of an equivocal MRI study as it allows for a dynamic assessment of instability [24, 25]. Given the variability in surgical techniques, tunnel/socket tunnel configurations, and the amount of bone removed at the time of primary UCL reconstruction, a CT scan with or without three-dimensional reconstructions may be needed to further evaluate remaining bone stock and tunnel geometry (Fig. 1).
Fig. 1.
a Coronal computed tomography (CT) image showing socket placement in the medial epicondyle of a failed UCL reconstruction. b Axial CT image showing ulnar socket placement. c Three-dimensional CT reconstruction demonstrating both ulnar and medial epicondyle sockets and prior endobutton fixation in proximal medial epicondyle
Non-Operative Treatment
Non-operative management of UCL injury may be a reasonable treatment option in a certain subset of patients with prior UCL reconstruction. Typical non-operative management for UCL injuries involves a period of rest, dedicated rehabilitation, and a progressive return to throwing. Non-operative treatment is often reserved for patients when the history, exam, and imaging are consistent with only low-grade partial tearing of the prior UCL graft. Generally speaking, complete or full thickness injuries are likely to be treated with revision surgery if the athlete desires to return to competitive pitching. In athletes with primary UCL injuries, return to previous level of play ranges from 42 to 84% with conservative management [26, 27]; however, success rates of non-operative treatment in the setting of UCL injury after prior reconstruction are less clear. Furthermore, non-operative management may not be ideal for professional pitchers who want to return to competitive play, as the best non-operative outcomes are seen in patients whom are non-throwers and put minimal strain on the elbow [28, 29].
Surgical Techniques
The procedure can be performed under regional anesthesia with sedation or general anesthesia with or without a regional nerve blockade. The patient is placed supine with the operative arm extended onto an arm table and a non-sterile tourniquet applied to the upper arm. If a gracilis tendon autograft is to be used, the ipsilateral or contralateral leg must also be prepped with a non-sterile tourniquet placed proximally on the thigh. Following graft harvest, the previous incision is utilized whenever possible to better ensure adequate wound healing. Careful review of the index surgery operative report is necessary to inform the surgeon of any alterations to the location of the ulnar nerve. Meticulous soft tissue dissection is required as development of scar tissue may make locating the ulnar nerve and the medial antebrachial cutaneous nerves challenging. All efforts should be made to identify and protect these nerves from iatrogenic injury throughout the procedure. Bipolar cautery should be utilized to coagulate any crossing vessels. There is no consensus regarding optimal surgical technique, exposure, graft selection, tunnel configuration, or other surgical variables for revision UCL reconstruction. Ideally, the technique most familiar to the surgeon is the one employed, however the primary reconstruction technique, cause of construct failure, and status of bone tunnel frequently dictate the surgical method. Thus, the revision surgery technique is typically adjusted for each patient.
There are a multitude of techniques described for primary UCL reconstruction including the original figure of 8 technique by Jobe in 1986 [1], the docking technique [6, 30], the modified Jobe [18], the DANE TJ technique [7], interference screw only [31], and a newly described anatomic reconstruction [32]. A survey of MLB orthopedic surgeons revealed a preference for the docking technique with palmaris autograft [33]. In a recent report on revision surgery in MLB and MiLB pitchers, a predilection towards the modified Jobe technique and use of hamstring autograft was reported [10].
One of the most important determinants of reconstruction technique is the condition and position of the prior bone tunnels and sockets. Tunnels that are in good condition may be used again for the revision; however, those that are compromised require alternative techniques. Options for overcoming compromised bone tunnels include use of alternative fixation techniques, avoidance of tunnels using an alternative graft configuration, creating new tunnels in a different location (if the tunnels/sockets from the primary surgery were in an inappropriate position), or bone grafting the prior tunnels and returning for reconstruction at a later date after consolidation. If the ulnar tunnel is compromised, utilization of the Anatomic UCL Reconstruction Technique [34, 35] may be reasonable to consider as the graft is configured in such a way that prior ulnar tunnels/sockets are spanned and can be completely avoided (Fig. 2). Another strategy to span compromised ulnar and/or humeral tunnels is to utilize cortical button suspension techniques which have shown efficacy in the setting of primary reconstruction [36]. Cases of insufficient bone on the humeral side are often more complex and typically arise is the setting of either a mispositioned sockets/tunnels or fracture of the medial epicondyle. In the setting of a fracture, fixation should be performed when possible. Graft integrity can be assessed afterwards. In instances where the humeral socket is severely malpositioned, a new socket can be created in an anatomic location, but bone graft should be performed to fill the prior socket. In cases were the bone deficiency is severe, a two-stage procedure may be required where the defect is graft in the first stage and the ligament reconstructed in the second [37].
Fig. 2.
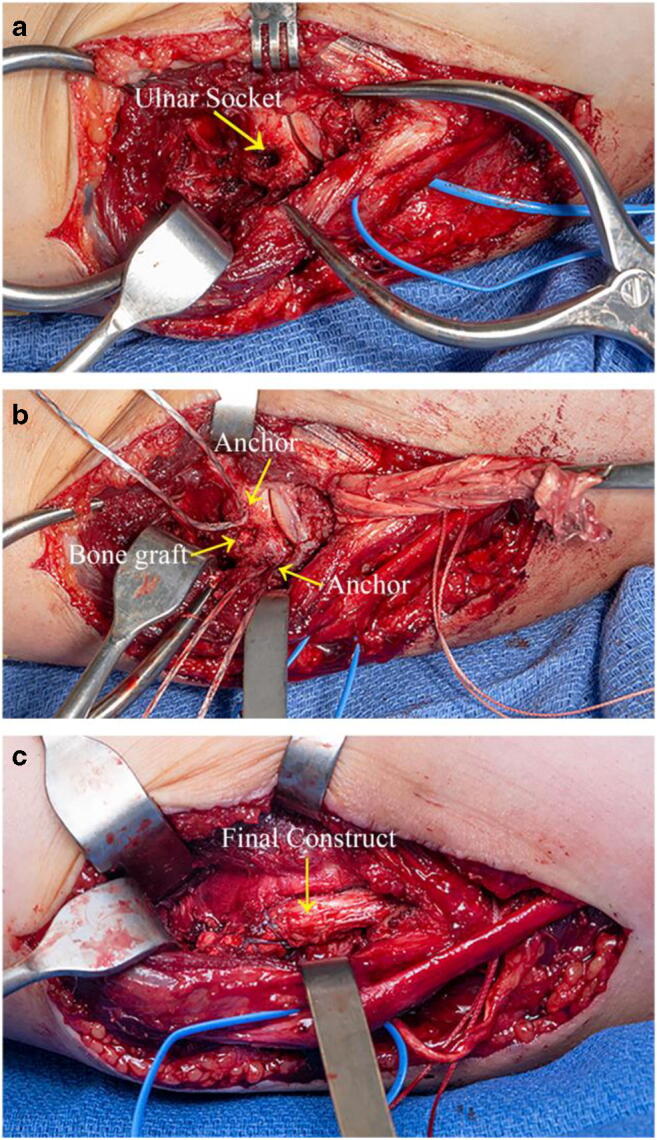
Intra-operative photographs illustrating the anatomic technique used for UCL revision reconstruction. a Intra-operative photograph showing the prior ulnar socket from prior UCL reconstruction centered in the sublime tubercle, preventing the creation of a standard ulnar tunnel that is typically used in the docking or modified Jobe techniques. Ulnar nerve is isolated posteriorly with blue vessel loop. b Remnant ulnar socket was filled with bone graft and dual ulnar all-suture suture anchors were placed on either side. c Final construct is shown. In this construct, the graft is fixed proximally to the ulna by tying each strand of the graft down with the all-suture suture anchors. It is fixed distally in the ulna using a suture anchor (not shown)
Outcomes
As the annual number of revision surgeries continues to rise, the number of studies reporting on outcomes of revision surgery continues to grow as well (Table 2). Dines et al. was the first to present clinical outcomes after UCL revision with a series of 15 competitive baseball players and found that only 33% of players were able to return to their pre-injury level of play [19]. Jones et al. reported on the outcomes of revision UCL reconstruction in 18 MLB pitchers in 2013. Although 78% (14) of these pitchers were able to return to play in MLB, only 17% of starting pitchers (1 of 6) and 38% of relieving pitchers (3 of 8) were able return to their original pre-injury workloads [8]. Overall, the relievers tended to have better pitching statistics than did the starters, including earned run averages, and strikeouts and walks per nine innings pitched.
Table 2.
Review of outcomes after UCL revision
| Primary author | Journal | Year | n | Return at any level n (%) | Return to previous level n (%) | Time to return | Career longevity after revision |
|---|---|---|---|---|---|---|---|
| Dines | Am J Sports Med | 2008 | 15 | 7 (46.6) | 5 (33.3) | N/A | 2.9 ± 2.8 |
| Jones | J Shoulder Elbow Surg | 2013 | 18 | N/A | 14 (78) | 1.6 (1–2.2) | N/A |
| Marshall | Am J Sports Med | 2015 | 33 | 28 (84.8) | 19/29 (65.5) | N/A | 4.1 ± 2.4 |
| Wilson | J Hand Surg Am | 2015 | 40 | N/A | N/A | N/A | 2.5 ± 2.4 (0–8) |
| Liu | J Shoulder Elbow Surg | 2016 | 26 | 21 (80.7) | 17 (65.4) | 1.73 | 2.64 (1–7) |
| Camp | J Shoulder Elbow Surg | 2018 | 68 | 55 (80.7) | 43 (63.5) | 1.27 ± 0.41 | 2.9 ± 2.8 |
| Camp | Orthop J Sports Med | 2019 | 47 | 76.6 | 55.3 | 1.32 ± 0.32 | N/A |
Summary of published outcomes in MLB and MiLB pitchers after UCL reconstruction surgery
Marshall et al. conducted a similar analysis using 33 MLB pitchers who underwent revision UCL reconstruction and found 85% (28/33) returned to professional play; however, only 65% (19/29) were able to return to the MLB [38]. The mean time between primary reconstruction and revision surgery was 4.7 years (range 1–13 years). Additionally, post-revision workloads were limited, consistent with the reporting from Jones et al. When compared with age- and position-matched major league controls, pitchers who underwent revision UCL reconstruction had comparable earned run averages (ERA) and walks/hits per innings pitched (WHIP), but significantly shorter careers and increased number in walks.
In 2015, Wilson et al. reported findings from a cohort of 271 MLB pitchers who underwent UCL reconstruction between 1974 and 2014 and found that 15% (40) required at least one revision UCL reconstruction [3]. The mean time between index UCL reconstruction and revision surgery was 5.2 ± 3.2 years (range 1–13 years). After undergoing UCL revision surgery, pitchers had statistically significantly shorter careers than those whom only had a single UCL reconstruction. Furthermore, career duration after UCL revision was only 2.5 ± 2.4 years compared with 4.9 ± 4.3 years after primary UCL reconstruction without revision.
Liu et al. performed a similar analysis in cohort of 235 MLB pitchers treated with UCL reconstruction between 1999 and 2014, noting that 13% (31) underwent revision surgery with 37% occurring within 3 years following index reconstruction. Of the 26 MLB pitchers included for return to play analysis after revision, 65% (17) were able to pitch at least one game; however, only 42% (11) were able to return to established play (defined as pitching in at least ten games). A higher number of relief pitchers were able to return to their previous level of play compared with starting pitchers, 57% vs 25%, respectively. A mean of 21 months of recovery and rehabilitation was required prior to returning to the MLB. Similar to the findings of Marshall et al., individual performance analysis showed pitchers who underwent revision were more likely to experience reductions in the number of pitches thrown per inning, innings pitched per season, percentage of thrown strikes, and total number of career pitches.
In the largest series to date, Camp et al. reported on 1429 UCL reconstructions in professional baseball pitchers. In that study, there was no statistically significant difference in return to play rates between primary and revision UCL operations which were 83.9% and 80.7%, respectively [4•]. Additionally, there was no statistically significant difference in return to previous level of play between primary (73.4%) and revision (63.5%) UCL operations (p = 0.145). Revision was required at an average 3.9 years (range 0.5–13.0 years) after primary reconstruction.
In a follow-up study evaluating the trends over time for 69 professional pitchers undergoing revision surgery, there was no difference in mean time to return to play between the most commonly performed repair techniques (14 months after docking vs. 17 months after modified Jobe, p = 0.296) or graft source (18 months after hamstring vs. 13 months after palmaris longus, p = 0.108) [10]. Of eligible pitchers, 76.6% (36/47) were able to return to any level of play, while 55.3% (26/47) returned to previous level of play. There was no significant difference in time until return to any of level or previous level of play at 16 months and 17 months, respectively (p = 0.336). It was also reported that MLB players returned to play at significantly higher rates after revision than MiLB players at 73.1% and 39.5%, respectively (p = 0.01). Consistent with other studies, there was a trend seen towards increasing rate of revision surgery between 2010 and 2016; however, this was not statistically significant (p = 0.104).
Complications
With most revision surgeries, there is a greater risk of complications when compared with the index procedure. Dines et al. reported a post-operative complication rate of 40% following revision UCL reconstruction with the most common complications consisting of elbow stiffness, reactive synovitis, transient ulnar neuritis, medial epicondylitis, and re-tear of the revised reconstruction requiring further surgery [19]. While re-rupture rate is a rare complication, it occurs in approximately 2% of patients after primary UCL reconstruction [37] compared with 6.7% after revision UCL reconstruction [19]. The increase in complications following revision surgery is likely due to the adaptations of the tissue in response to the trauma of the initial surgery and repetitive injuries, such as scar tissue formation leading to distortion of the original anatomy. Other known complications include continued pain, heterotopic ossification, and fracture.
Conclusions
As the rate of primary UCL reconstruction increases, there has been a corresponding increase in the rate of UCL revisions as well. Many of the same techniques used for primary reconstruction can be used in revision surgery; however, the technique may need to be modified or adapted on a case by case basis, which emphasizes the importance of careful pre-operative evaluation. When humeral or ulnar-sided bone is compromised from prior surgery, a single-stage revision can still be considered if the previous bone tunnels can be utilized, spanned, or avoided all together. When bony defects are substantial, a two-stage procedure with bone grafting techniques may need to be considered. Outcomes in professional pitchers after UCL revision surgery are relatively favorable with return to play rates averaging 46.6 to 84.8%; however, other metrics such as return to previous level of play and career length are not as optimistic compared with primary UCL surgery. Although RTP times vary widely, it appears that the majority of pitchers are able to get back to live game play at an average of 15.6 to 20.4 months. While the body of evidence investigating revision UCL reconstruction has come a long way in recent years, additional study is needed to help guide surgical decision-making and optimize clinical outcomes.
Compliance with Ethical Standards
Conflict of Interest
Lucas Keyt, Jennifer Tangtiphaiboontana, and Travis Turner declare that they have no conflict of interest.
Joshua Dines is a board or committee member for American Shoulder and Elbow Surgeons, is a paid consultant, presenter or speaker for and has received research support from Arthrex, Inc., is an editorial or governing board of Journal of Shoulder and Elbow Surgery, receives IP royalties from Linvatec, receives publishing royalties, financial or material support from Thieme, receives publishing royalties, financial or material support from Wolters Kluwer Health – Lippincott Williams & Wilkins.
Michael Knudsen received an educational grant to Columbia University Medical Center from Smith & Nephew, Inc.
Christopher Camp received hospitality and educational payments from Arthrex, Inc. and hospitality payments from Zimmer Biomet.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
Primary Location where this investigation was performed: Mayo Clinic, Rochester, MN
This article is part of the Topical Collection on Injuries in Overhead Athletes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Jobe FW, Stark H, Lombardo SJ. Reconstruction of the ulnar collateral ligament in athletes. J Bone Joint Surg Am. 1986;68(8):1158–1163. doi: 10.2106/00004623-198668080-00004. [DOI] [PubMed] [Google Scholar]
- 2.Leland DP, Conte S, Flynn N, Conte N, Crenshaw K, Wilk KE, Camp CL. Prevalence of medial ulnar collateral ligament surgery in 6135 current professional baseball players: a 2018 update. Orthop J Sports Med. 2019;7(9):2325967119871442. doi: 10.1177/2325967119871442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wilson AT, Pidgeon TS, Morrell NT, DaSilva MF. Trends in revision elbow ulnar collateral ligament reconstruction in professional baseball pitchers. J Hand Surg [Am] 2015;40(11):2249–2254. doi: 10.1016/j.jhsa.2015.07.024. [DOI] [PubMed] [Google Scholar]
- 4.Camp CL, Conte S, D’Angelo J, Fealy SA. Epidemiology of ulnar collateral ligament reconstruction in Major and Minor League Baseball pitchers: comprehensive report of 1429 cases. J Shoulder Elb Surg. 2018;27(5):871–878. doi: 10.1016/j.jse.2018.01.024. [DOI] [PubMed] [Google Scholar]
- 5.Cain EL, Jr, Andrews JR, Dugas JR, Wilk KE, McMichael CS, Walter JC, 2nd, et al. Outcome of ulnar collateral ligament reconstruction of the elbow in 1281 athletes: results in 743 athletes with minimum 2-year follow-up. Am J Sports Med. 2010;38(12):2426–2434. doi: 10.1177/0363546510378100. [DOI] [PubMed] [Google Scholar]
- 6.Rohrbough JT, Altchek DW, Hyman J, Williams RJ, 3rd, Botts JD. Medial collateral ligament reconstruction of the elbow using the docking technique. Am J Sports Med. 2002;30(4):541–548. doi: 10.1177/03635465020300041401. [DOI] [PubMed] [Google Scholar]
- 7.Dines JS, ElAttrache NS, Conway JE, Smith W, Ahmad CS. Clinical outcomes of the DANE TJ technique to treat ulnar collateral ligament insufficiency of the elbow. Am J Sports Med. 2007;35(12):2039–2044. doi: 10.1177/0363546507305802. [DOI] [PubMed] [Google Scholar]
- 8.Jones KJ, Conte S, Patterson N, ElAttrache NS, Dines JS. Functional outcomes following revision ulnar collateral ligament reconstruction in Major League Baseball pitchers. J Shoulder Elb Surg. 2013;22(5):642–646. doi: 10.1016/j.jse.2013.01.031. [DOI] [PubMed] [Google Scholar]
- 9.Liu JN, Garcia GH, Conte S, ElAttrache N, Altchek DW, Dines JS. Outcomes in revision Tommy John surgery in major league baseball pitchers. J Shoulder Elb Surg. 2016;25(1):90–97. doi: 10.1016/j.jse.2015.08.040. [DOI] [PubMed] [Google Scholar]
- 10.Camp CL, Desai V, Conte S, Ahmad CS, Ciccotti M, Dines JS, Altchek DW, D'Angelo J, Griffith TB. Revision ulnar collateral ligament reconstruction in professional baseball: current trends, surgical techniques, and outcomes. Orthop J Sports Med. 2019;7(8):2325967119864104. doi: 10.1177/2325967119864104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Erickson BJ, Gupta AK, Harris JD, Bush-Joseph C, Bach BR, Abrams GD, et al. Rate of return to pitching and performance after Tommy John surgery in Major League Baseball pitchers. Am J Sports Med. 2014;42(3):536–543. doi: 10.1177/0363546513510890. [DOI] [PubMed] [Google Scholar]
- 12.Makhni EC, Lee RW, Morrow ZS, Gualtieri AP, Gorroochurn P, Ahmad CS. Performance, return to competition, and reinjury after Tommy John surgery in Major League Baseball pitchers: a review of 147 cases. Am J Sports Med. 2014;42(6):1323–1332. doi: 10.1177/0363546514528864. [DOI] [PubMed] [Google Scholar]
- 13.Osbahr DC, Cain EL, Jr, Raines BT, Fortenbaugh D, Dugas JR, Andrews JR. Long-term outcomes after ulnar collateral ligament reconstruction in competitive baseball players: minimum 10-year follow-up. Am J Sports Med. 2014;42(6):1333–1342. doi: 10.1177/0363546514528870. [DOI] [PubMed] [Google Scholar]
- 14.Keller RA, Mehran N, Khalil LS, Ahmad CS, ElAttrache N. Relative individual workload changes may be a risk factor for rerupture of ulnar collateral ligament reconstruction. J Shoulder Elb Surg. 2017;26(3):369–375. doi: 10.1016/j.jse.2016.11.045. [DOI] [PubMed] [Google Scholar]
- 15.Keller RA, Mehran N, Marshall NE, Okoroha KR, Khalil L, Tibone JE, et al. Major League pitching workload after primary ulnar collateral ligament reconstruction and risk for revision surgery. J Shoulder Elb Surg. 2017;26(2):288–294. doi: 10.1016/j.jse.2016.11.008. [DOI] [PubMed] [Google Scholar]
- 16.Erickson BJ, Chalmers PN, Bach BR, Jr, Dines JS, Verma NN, Bush-Joseph CA, et al. Length of time between surgery and return to sport after ulnar collateral ligament reconstruction in Major League Baseball pitchers does not predict need for revision surgery. J Shoulder Elb Surg. 2017;26(4):699–703. doi: 10.1016/j.jse.2017.01.014. [DOI] [PubMed] [Google Scholar]
- 17.Griffith TB, Ahmad CS, Gorroochurn P, D’Angelo J, Ciccotti MG, Dines JS, et al. Comparison of outcomes based on graft type and tunnel configuration for primary ulnar collateral ligament reconstruction in professional baseball pitchers. Am J Sports Med. 2019;47(5):1103–1110. doi: 10.1177/0363546519831705. [DOI] [PubMed] [Google Scholar]
- 18.Azar FM, Andrews JR, Wilk KE, Groh D. Operative treatment of ulnar collateral ligament injuries of the elbow in athletes. Am J Sports Med. 2000;28(1):16–23. doi: 10.1177/03635465000280011401. [DOI] [PubMed] [Google Scholar]
- 19.Dines JS, Yocum LA, Frank JB, ElAttrache NS, Gambardella RA, Jobe FW. Revision surgery for failed elbow medial collateral ligament reconstruction. Am J Sports Med. 2008;36(6):1061–1065. doi: 10.1177/0363546508314796. [DOI] [PubMed] [Google Scholar]
- 20.Dugas J, Chronister J, Cain EL, Jr, Andrews JR. Ulnar collateral ligament in the overhead athlete: a current review. Sports Med Arthrosc Rev. 2014;22(3):169–182. doi: 10.1097/jsa.0000000000000033. [DOI] [PubMed] [Google Scholar]
- 21.Erickson BJ, Romeo AA. The ulnar collateral ligament injury: evaluation and treatment. J Bone Joint Surg Am. 2017;99(1):76–86. doi: 10.2106/jbjs.16.01277. [DOI] [PubMed] [Google Scholar]
- 22.Wear SA, Thornton DD, Schwartz ML, Weissmann RC, 3rd, Cain EL, Andrews JR. MRI of the reconstructed ulnar collateral ligament. AJR Am J Roentgenol. 2011;197(5):1198–1204. doi: 10.2214/ajr.11.6461. [DOI] [PubMed] [Google Scholar]
- 23.Andrachuk JS, Scillia AJ, Aune KT, Andrews JR, Dugas JR, Cain EL. Symptomatic heterotopic ossification after ulnar collateral ligament reconstruction: clinical significance and treatment outcome. Am J Sports Med. 2016;44(5):1324–1328. doi: 10.1177/0363546515626185. [DOI] [PubMed] [Google Scholar]
- 24.Konin GP, Nazarian LN, Walz DM. US of the elbow: indications, technique, normal anatomy, and pathologic conditions. Radiographics. 2013;33(4):E125–E147. doi: 10.1148/rg.334125059. [DOI] [PubMed] [Google Scholar]
- 25.Ferreira FB, Fernandes ED, Silva FD, Vieira MC, Puchnick A, Fernandes AR. A sonographic technique to evaluate the anterior bundle of the ulnar collateral ligament of the elbow: imaging features and anatomic correlation. J Ultrasound Med. 2015;34(3):377–384. doi: 10.7863/ultra.34.3.377. [DOI] [PubMed] [Google Scholar]
- 26.Rettig AC, Sherrill C, Snead DS, Mendler JC, Mieling P. Nonoperative treatment of ulnar collateral ligament injuries in throwing athletes. Am J Sports Med. 2001;29(1):15–17. doi: 10.1177/03635465010290010601. [DOI] [PubMed] [Google Scholar]
- 27.Ford GM, Genuario J, Kinkartz J, Githens T, Noonan T. Return-to-play outcomes in professional baseball players after medial ulnar collateral ligament injuries: comparison of operative versus nonoperative treatment based on magnetic resonance imaging findings. Am J Sports Med. 2016;44(3):723–728. doi: 10.1177/0363546515621756. [DOI] [PubMed] [Google Scholar]
- 28.Kenter K, Behr CT, Warren RF, O'Brien SJ, Barnes R. Acute elbow injuries in the National Football League. J Shoulder Elb Surg. 2000;9(1):1–5. doi: 10.1016/S1058-2746(00)80023-3. [DOI] [PubMed] [Google Scholar]
- 29.Miller CD, Savoie FH., 3rd Valgus extension injuries of the elbow in the throwing athlete. J Am Acad Orthop Surg. 1994;2(5):261–269. doi: 10.5435/00124635-199409000-00004. [DOI] [PubMed] [Google Scholar]
- 30.Smith GR, Altchek DW, Pagnani MJ, Keeley JR. A muscle-splitting approach to the ulnar collateral ligament of the elbow. Neuroanatomy and operative technique. Am J Sports Med. 1996;24(5):575–580. doi: 10.1177/036354659602400503. [DOI] [PubMed] [Google Scholar]
- 31.Ahmad CS, Lee TQ, ElAttrache NS. Biomechanical evaluation of a new ulnar collateral ligament reconstruction technique with interference screw fixation. Am J Sports Med. 2003;31(3):332–337. doi: 10.1177/03635465030310030201. [DOI] [PubMed] [Google Scholar]
- 32.Camp CL, Bernard C, Benavitz B, Konicek J, Altchek DW, Dines JS. Reconstruction of the medial ulnar collateral ligament of the elbow: biomechanical comparison of a novel anatomic technique to the docking technique. Orthop J Sports Med. 2019;7(7):2325967119857592. doi: 10.1177/2325967119857592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Erickson BJ, Harris JD, Fillingham YA, Cvetanovich GL, Bush-Joseph CA, Bach BR, Jr, et al. Treatment of ulnar collateral ligament injuries and superior labral tears by Major League Baseball team physicians. Arthroscopy. 2016;32(7):1271–1276. doi: 10.1016/j.arthro.2016.01.034. [DOI] [PubMed] [Google Scholar]
- 34.Bartoli M, Pederzini LA, Severini G, Serafini F, Prandini M. Elbow medial ulnar collateral ligament chronic isolated insufficiency: anatomical M-UCL reconstruction technique and clinical experience in a mid-term follow-up. Musculoskelet Surg. 2018;102(Suppl 1):75–83. doi: 10.1007/s12306-018-0559-3. [DOI] [PubMed] [Google Scholar]
- 35.O'Driscoll SW, Jaloszynski R, Morrey BF, An KN. Origin of the medial ulnar collateral ligament. J Hand Surg [Am] 1992;17(1):164–168. doi: 10.1016/0363-5023(92)90135-c. [DOI] [PubMed] [Google Scholar]
- 36.Myeroff C, Brock JL, Huffman GR. Ulnar collateral ligament reconstruction in athletes using a cortical button suspension technique. J Shoulder Elb Surg. 2018;27(8):1366–1372. doi: 10.1016/j.jse.2018.04.009. [DOI] [PubMed] [Google Scholar]
- 37.Rosenbaum Andrew J., Flaherty Michael A., Chin Christopher, Elattrache Neal S., Dines Joshua S. Elbow Ulnar Collateral Ligament Injury. Boston, MA: Springer US; 2015. Revision Ulnar Collateral Ligament Reconstruction; pp. 189–194. [Google Scholar]
- 38.Marshall NE, Keller RA, Lynch JR, Bey MJ, Moutzouros V. Pitching performance and longevity after revision ulnar collateral ligament reconstruction in Major League Baseball pitchers. Am J Sports Med. 2015;43(5):1051–1056. doi: 10.1177/0363546515579636. [DOI] [PubMed] [Google Scholar]