Abstract
Background
COVID-19 is fast-spreading and potentially fatal, introducing home quarantine, social distancing, and increased internet usage globally. We investigated COVID-19 anxiety, general anxiety and depression symptoms, and their impact on problematic smartphone use (PSU) severity
Methods
Participants were 908 residents of a large Eastern Chinese city, surveyed from late-February to mid-March, 2020. We administered online measures including the Depression Anxiety Stress Scale-21, Smartphone Addiction Scale-Short Version, and items querying COVID-19-related news exposure and threat of death. Additionally, participants rated anxiety using the Generalized Anxiety Disorder Scale-7 with reference to COVID-19.
Results
COVID-19 anxiety correlated with severity of PSU, depression and anxiety. Using established cut-off scores, 12% of participants were identified with at least moderate depression, and 24% with moderate anxiety. Using structural equation modeling, COVID-19 anxiety related to PSU severity, mediating relations between general anxiety and PSU severity. However, controlling PSU for general anxiety and depression severity, COVID-19 anxiety no longer predicted PSU severity.
Limitations
Limitations include the cross-sectional research design and reliance on data from only one country.
Conclusions
Results are discussed in context of the I-PACE model of excessive internet use. While COVID-19 anxiety is likely a global anxiety-provoking event, other everyday worries and anxiety are additionally clinically important in driving excessive internet use.
Keywords: COVID-19, Pandemics, Smartphone addiction, Anxiety, Depression
1. Introduction
A volume of research in many countries has supported mental health symptoms, primarily depression and anxiety, positively related to greater problematic smartphone use (PSU) (reviewed by Elhai et al., 2019a; Yang et al., 2020). The theorized mechanism is that many people seek emotional relief through easily accessible means—one's smartphone and internet devices—and over-reliance on such coping can lead to adverse consequences (Brand et al., 2019, 2016; Kardefelt-Winther, 2014). The COVID-19 pandemic (Li et al., 2020), and associated home quarantine and social distancing, have widely increased anxiety and negative emotion in society (Gao et al., 2020; Qiu et al., 2020; Wang et al., 2020); therefore, our aim was to investigate COVID-19 anxiety levels and associations with PSU severity as a maladaptive coping method.
Smartphone use can offer substantial productivity (Doargajudhur and Dell, in press) and social capital advantages (Choi, 2018) at milder levels; however, excessive use has deleterious consequences. The relationship between smartphone use and adaptive functioning represents an inverted U-curve (Montag et al., 2016). PSU is defined as extreme levels of use resulting in functional problems, such as social, work or academic impairment, with symptoms resembling those in substance use disorders (e.g., withdrawal without use, tolerance, reckless use) (Elhai et al., 2019a; Ryding and Kuss, 2020). Additionally, PSU correlates with neck and hand pain from smartphone overuse (Namwongsa et al., 2019) as well as distracted driving and walking (Mourra et al., 2020). PSU is not an official mental disorder, but an important clinical concern nonetheless (Montag et al., in press).
Because excessive smartphone and internet use are conceptualized as (maladaptive) emotional coping processes for relieving negative affect (Brand et al., 2019, 2016; Kardefelt-Winther, 2014), negative affectivity has been investigated in relation to PSU. PSU severity demonstrates small-to-moderate positive associations with depression and anxiety symptoms across the literature (Elhai et al., 2019a; Yang et al., 2020). Furthermore, recent studies support additional negative affectivity correlates of PSU severity, including rumination (Elhai et al., in pressa; Elhai et al., 2020c; Liu et al., 2017), worry (Elhai et al., 2019b), and fear of missing out (FOMO) on rewarding social experiences (Elhai et al., 2020d; Sha et al., 2019).
1.1. Background on COVID-19 mental health research
COVID-19 first appeared in Wuhan, Hubei province (China) in late December 2019, spreading to nearly every other country within months, leading to home quarantine and social distancing to contain the virus (Li et al., 2020). Several peer-reviewed studies have assessed emotional distress among Chinese participants (the first affected) related to COVID-19. Surveyed in late-January 2020, probable disorder rates (from at least moderately severe scale scores) have ranged from 17–48% for depression and 23–28% for anxiety (Gao et al., 2020; Wang et al., 2020), with lower anxiety rates (4%) among college students (Cao et al., 2020). Another study used a composite mental health score, finding 35% prevalence of significant emotional distress (Qiu et al., 2020). However, these studies did not query anxiety or distress specifically from COVID-19.
Anxiety about COVID-19 and associated social isolation are not limited to China. In Iran, Ahorsu et al. (in press) investigated anxiety specifically from COVID-19, finding moderate COVID-19 anxiety and moderate associations with general anxiety and depression severity. In the U.S., McKay et al. (in press) revealed that COVID-19 anxiety had large associations with disgust propensity and sensitivity, and anxiety sensitivity. Thus far, opinion polls (non-peer-reviewed) from other countries demonstrate substantial concern about COVID-19 (e.g., Angus Reid Institute, 2020, February 5; Pew Research Center, 2020). Finally, we emphasize that some COVID-19 anxiety is adaptive in promoting social distancing needed to eradicate the virus, but excessive anxiety will cause unnecessary hospital overcrowding and morbidity (Asmundson and Taylor, 2020a).
1.2. Aims
We conducted a survey of COVID-19 anxiety and other psychopathology variables among community participants from China during the pandemic. Our primary aim was to investigate the impact of COVID-19 anxiety, general anxiety, and general depression symptoms on severity of PSU as a maladaptive emotion coping mechanism. COVID-19 is a potentially fatal disease, and its consequential social isolation from quarantine and distancing increase anxiety (Xiang et al., 2020). Given that social isolation drives emotional distress and negative affect (Hawkley and Cacioppo, 2010; Leigh-Hunt et al., 2017), general anxiety and depression as well as anxiety specific to COVID-19 should, in turn, exacerbate PSU (reviewed in Elhai et al., 2019a; Yang et al., 2020).
1.3. Theory
A prominent theoretical framework explaining excessive internet and smartphone use is the Interaction of Person-Affect-Cognition-Execution (I-PACE) model (Brand et al., 2019, 2016). I-PACE conceptualizes major categories of variables influencing excessive internet use, including background predisposing variables, affective and cognitive responses, and executive functioning impairment. Predisposing variables involve underlying individual differences, including personality, core cognitions, biology, and psychopathology. Consequences from predisposing variables involve affective and cognitive response variables, including coping, attention bias, mood dysregulation, and responses to environmental stressors. In particular, I-PACE conceptualizes response variables as mechanisms by which predisposing variables influence excessive internet use (Brand et al., 2019, 2016). I-PACE is supported by numerous studies explaining excessive internet, social media, and smartphone use (e.g., Dempsey et al., 2019; Elhai et al., 2020a; Lachmann et al., 2019).
1.4. Research model
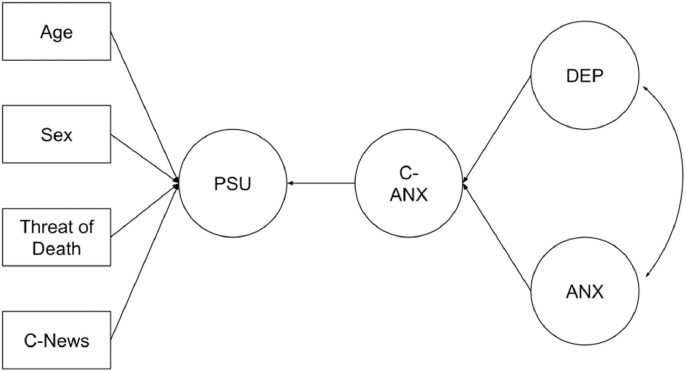
We present our hypothesized research model in Fig. 1 . We modeled general anxiety and depression symptoms as predisposing predictor variables from I-PACE. We modeled COVID-19 anxiety as an ongoing response to an environmental stressor, and mediator within the affective/cognitive response category. Our dependent variable was PSU severity. We incorporated sex and age covariates of PSU severity, because women and younger individuals evidence greater PSU severity (Vahedi and Saiphoo, 2018). We also included COVID-19-related exposure covariates, including perceived threat of death from COVID-19 and COVID-19 news exposure.
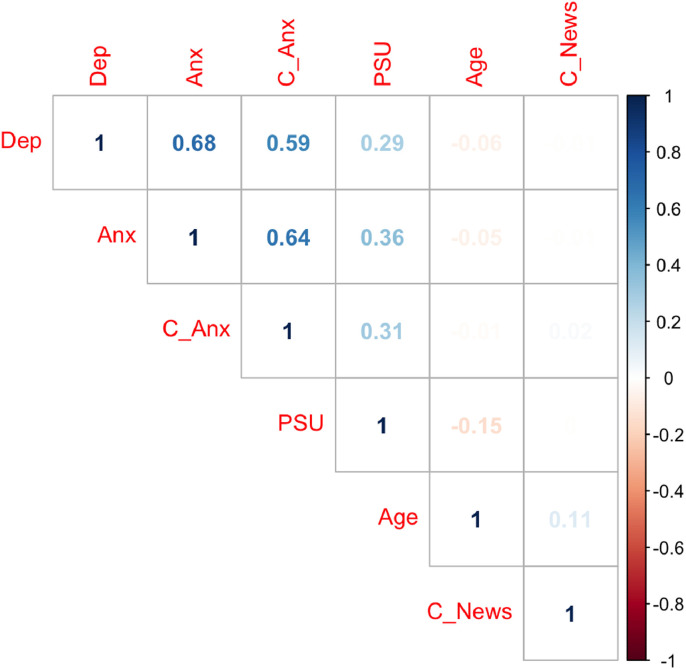
Fig. 2.
Correlation matrix of primary variables. Legend: Dep = Depression; Anx = Anxiety; C-Anx = COVID-19 anxiety; PSU = Problematic Smartphone Use; C-News = COVID-19-related news exposure. Correlations with a darker shade indicate stronger correlations, with blue indicating positive and red indicating negative correlations. Correlations greater than 0.10 in absolute size were significant at p < 0.001.
Fig. 1.
Hypothesized model. Legend: DEP = Depression; ANX = Anxiety; C-ANX = COVID-19-related anxiety; PSU = Problematic smartphone use; C-News = COVID-19-related news exposure; Threat of Death = Perceived threat of death from COVID-19. Circles represent latent variables, while rectangles indicate observed variables. For visual simplicity, factor loading paths from the latent variables are not displayed.
1.5. Hypotheses
H1. COVID-19 anxiety should positively relate to PSU severity. General anxiety is consistently associated with PSU severity (Elhai et al., 2019a; Yang et al., 2020). COVID-19 anxiety more specifically represents an affective response to environmental stressors in I-PACE (Brand et al., 2019, 2016) and affective responses influence excessive internet and PSU (e.g., Dempsey et al., 2019; Elhai et al., 2020a; Lachmann et al., 2019).
H2. General anxiety (H2a) and depression (H2b) severity should positively relate to COVID-19 anxiety. Excessive anxiety about a viral outbreak is influenced by psychological variables, including pre-existing anxiety, worry, and negative affect (Asmundson and Taylor, 2020a; Taylor, 2019). Pre-existing or general anxiety and depression (not specifically COVID-19 anxiety) represent predisposing psychopathology variables in I-PACE that influence affective/cognitive responses such as COVID-19 anxiety. Ahorsu et al. (in press) found COVID-19 anxiety related to general anxiety and depression severity.
H3. COVID-19 anxiety should mediate relations between both general anxiety (H3a) and depression (H3b) severity with PSU severity. I-PACE conceptualizes affective/cognitive responses as mediating mechanisms between predisposing variables and excessive internet and PSU (Brand et al., 2019, 2016). Therefore, COVID-19 anxiety (an affective response to environmental stressors) should demonstrate a meditational role between negative affectivity (general anxiety/depression) and PSU severity. Prior work has established numerous affective/cognitive response mediators between predisposing depression/anxiety and excessive internet/PSU severity (e.g., Elhai et al., in pressa; Wegmann et al., 2017; Wolniewicz et al., 2020).
2. Methods
2.1. Participants and procedure
We conducted a cross-sectional web-based survey of Chinese adults between February 24 and March 15, 2020. We used the widely popular Chinese social networking app “WeChat” (Montag et al., 2018) to invite participants. WeChat has location-based online communities, and we arranged for WeChat community moderators from districts within a large metropolitan city in Eastern China (Tianjin, population = 12 million) to invite their residents through the app. Interested participants were presented an online informed consent statement and, for those consenting, a Chinese language web survey hosted on Survey Star, with features to prevent bots from participation. Each participant received a reward for completion, randomly allocating a digital payment or voucher, from 3–10 Chinese RMB (roughly 0.50–$1.50 USD). We first obtained approval from Tianjin Normal University's ethics committee, following the Declaration of Helsinki.
The web survey prompted participants to complete skipped items, so no missing item-level data were present. After removing participants with dozens of consecutive identical item responses, our effective sample included 908 participants. Age averaged 40.37 years (SD = 9.27), ranging from 17–64 years. A majority were women (n = 752, 82.82%) and were of Chinese Han ethnicity (n = 875, 96.37%).
2.2. Instruments
We queried demographic characteristics including sex, age and ethnicity. Next, we administered several online measures.
2.2.1. Depression anxiety stress scale-21 (DASS-21)
The DASS-21 is a 21-item English self-report instrument, with symptom ratings over the past week. The instrument uses a Likert-type scale from “0 = Did not apply to me at all” to “3 = Applied to me very much, or most of the time.” We analyzed only depression and anxiety items (7 items each), most consistently associated with PSU severity (Elhai et al., 2019a; Yang et al., 2020). We used the Chinese instrument version, validated previously (Wang et al., 2016). The depression and anxiety subscales have adequate reliability and validity (Zanon et al., in press). Internal consistency (coefficient alpha) in our sample was 0.82 for depression, and 0.76 for anxiety.
2.2.2. Generalized anxiety disorder scale-7 (GAD-7) for COVID-19 anxiety
The GAD-7 is a 7-item English self-report measure of anxiety and worry symptoms, with ratings over the past two weeks. The GAD-7 uses a Likert-type frequency scale from “0 = Not at all” to “3 = Nearly every day.” Summed scores are reliable and valid (Plummer et al., 2016). We used the Chinese version, validated by He et al. (2010). We tailored instructions to query COVID-19 anxiety, specifying “Over the last 2 weeks, how often have you been bothered by the following problems because of the coronavirus outbreak?” Internal consistency for our sample was 0.90.
2.2.3. Smartphone addiction scale-short version (SAS-SV)
The SAS-SV is a 10-item self-report measure of smartphone-related problematic use and functional impairment, developed in Korean and English (Kwon et al., 2013). The measure uses a Likert-type scale from “1 = Strongly disagree” to “6 = Strongly agree.” Items include “I use my smartphone longer than I had intended,” and “I won't be able to stand not having a smartphone.” We voiced items in the first-person for consistency (Duke and Montag, 2017). Total scores are reliable and valid (Lopez-Fernandez, 2017). We used the Chinese SAS-SV, validated by Chen et al. (2017). Internal consistency for our sample was 0.86.
2.2.4. COVID-19 news exposure
We queried news exposure to COVID-19 by asking “How much have you heard or learned about coronavirus in the news? (By news we mean national, international, regional/local news and other topical events accessed via radio, TV, newspaper or online)?” We used a Likert-type scale from “0 = Not at all” to “4 = Quite a lot.” We adapted this English item from Newman and Levy (2014), and translated it into Chinese.
2.2.5. COVID-19 perceived threat of death
We queried perceived threat of death by asking “Have you feared that you may die from the coronavirus?” We used a “yes”/“no” binary scale. We adapted this English item from Norris et al. (2006), and we translated it into Chinese.
2.3. Analysis
We used R software 3.6.2 (R Core Team, 2020) for data processing and preliminary analyses, with R packages pastecs (for descriptive statistics), fmsb (internal consistency), corrplot (correlations), and sjstats (ANOVA effects). We summed item responses to form scale scores, which were normally distributed, with the largest skewness value of 1.66 (depression) and kurtosis of 3.23 (anxiety). We conducted Pearson correlations on continuous variables from our Research Model. We computed ANOVAs for relations between categorical variables (i.e., sex and threat of death) and continuous variables. We computed a chi-square analysis for relations between sex and threat of death.
We used Mplus version 8.4 (Muthén and Muthén, 2019) for confirmatory factor analysis (CFA) and structural equation modeling (SEM). First, we computed CFAs for psychological scales (circles) in Fig. 1 using item-level data. Items within CFAs were treated as ordinal data, involving polychoric covariance matrices, probit factor loadings, and weighted least squares estimation with mean- and variance-adjusted chi-square values (Lei and Shiverdecker, in press). The only residual covariances estimated were between SAS-SV items 1 and 2 (involving work and school impairment) and 4 and 5 (involving withdrawal). We judged goodness of fit from the comparative fit index (CFI) and Tucker-Lewis Index (TLI) > 0.94, root mean square error of approximation (RMSEA) < 0.06, and standardized root mean square residual (SRMR) < 0.08 (Maydeu-Olivares, 2017).
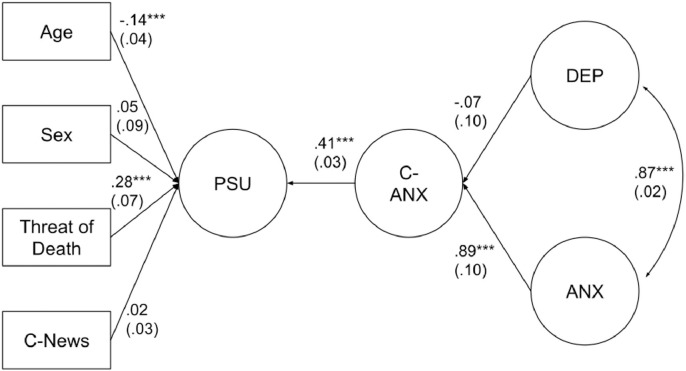
We tested our Research Model (see Fig. 1) using SEM, with the same analytic approach discussed above. The path from COVID-19 anxiety to PSU severity tests H1. Paths from depression and anxiety to COVID-19 anxiety test H2. We also tested a variation of this model (see Fig. 4), adding paths from general depression and anxiety to PSU, comparing this model variation to the original Research Model using Mplus’ DIFFTEST command.
Fig. 4.
Revised model with standardized path coefficients. Legend: DEP = Depression; ANX = Anxiety; C-ANX = COVID-19-related anxiety; PSU = Problematic smartphone use; C-News = COVID-19-related news exposure; Threat of Death = Perceived threat of death from COVID-19. Circles represent latent variables, while rectangles indicate observed variables. Standard errors are displayed in parentheses. For visual simplicity, factor loading paths from the latent variables are not displayed, but estimates can be requested from the first author. Sex was coded “1‽ for men, and “2‽ for women. Threat of death was coded “1‽ for “yes,” and “0‽ for “no.” * p < 0.05, ** p < 0.01, *** p < 0.001.
Finally, we tested mediation by computing cross-products of direct path coefficients, using the Delta method for estimating indirect effect standard errors, with 1000 non-parametric bootstrapped replications (Hayes, 2017). The mediation effects from anxiety->COVID-19 anxiety->PSU severity, and from depression->COVID-19 anxiety->PSU severity, test H3a and H3b, respectively.
3. Results
3.1. Preliminary results
We present descriptive statistics for continuous variables in Table 1 , separated by the categorical variables (i.e., sex and perceived threat of death). Men scored higher than women on depression severity. Those perceiving threat of death from COVID-19 scored higher on depression, anxiety, COVID-19 anxiety, and PSU severity. Sex was not related to perceived threat of death, χ 2(1, N = 908) = 0.54, p = 0.46, phi = 0.02. Fig. 1 displays bivariate Pearson correlations among continuous variables. COVID-19 anxiety moderately correlated with PSU severity (H1). Depression and anxiety severity both strongly correlated with COVID-19 anxiety (H2).
Table 1.
Means and standard deviations for prim
| Variable | Men M (SD) | Women M(SD) | Sex F(1,906) | p | Did Not Fear Death M (SD) | Feared Death M (SD) | Threat/Fear of Death F (1,906) | p | ||
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Depression | 3.63 | 2.59 | 14.18 | <0.001 | 0.015 | 2.42 | 2.96 | 6.18 | 0.01 | 0.007 |
| (4.00) | (2.94) | (2.91) | (3.29) | |||||||
| 2. Anxiety | 4.23 | 3.87 | 1.62 | 0.20 | 0.002 | 3.38 | 4.24 | 15.27 | <0.001 | 0.017 |
| (3.56) | (3.14) | (2.85) | (3.36) | |||||||
| 3. C-Anxiety | 4.76 | 4.23 | 2.40 | 0.12 | 0.003 | 3.46 | 4.80 | 25.87 | <0.001 | 0.028 |
| (4.40) | (3.76) | (3.48) | (4.00) | |||||||
| 4. PSU | 31.26 | 32.20 | 1.07 | 0.30 | 0.001 | 30.17 | 33.08 | 17.13 | <0.001 | 0.019 |
| (10.58) | (10.19) | (10.23) | (10.13) | |||||||
| 5. Age | 41.32 | 40.17 | 1.99 | 0.16 | 0.002 | 41.00 | 40.01 | 2.37 | 0.12 | 0.003 |
| (11.47) | (8.74) | (9.48) | (9.13) | |||||||
| 6. C—News | 2.79 | 2.69 | 2.63 | 0.11 | 0.003 | 2.69 | 2.72 | 0.63 | 0.43 | 0.001 |
| (0.74) | (0.64) | (0.68) | (0.65) |
Note: C-Anxiety = COVID-19 anxiety; PSU = Problematic smartphone use; C-News = Coronavirus news exposure. Sex was coded “1‽ for men, and “2‽ for women. Threat of death was coded “1‽ for “yes,” and 0 for “no.”.
We used validated cut-off scores to identify possible mental health cases. 106 participants (11.67%) would be identified with current moderate depression using a DASS-21 depression score >6, with 34 cases (3.74%) of severe depression using a score > 13 (Zanon et al., in press). 219 participants (24.12%) would be identified with moderate anxiety using a DASS-21 anxiety score >5, with 62 cases (6.83%) of severe anxiety with a score >7 (Zanon et al., in press). 72 participants (7.93%) would be identified with moderate COVID-19 anxiety using a GAD-7 score >9, with 24 cases (2.64%) of severe COVID-19 anxiety using a score >14 (Plummer et al., 2016). Finally, 472 participants (51.98%) would be identified with PSU using a SAS-SV score >31 (Kwon et al., 2013; Lopez-Fernandez, 2017).
3.2. SEM results
The DASS-21 anxiety CFA fit well, robust χ 2(14, N = 908) = 54.05, p < 0.001, CFI = 0.98, TLI = 0.97, RMSEA = 0.06 (90% CI: 0.04–0.07), SRMR = 0.03. Additionally, the depression CFA fit well, robust χ 2(14, N = 908) = 49.47, p < 0.001, CFI = 0.99, TLI = 0.99, RMSEA = 0.05 (90% CI: 0.04–0.07), SRMR = 0.03. The COVID-19 anxiety CFA also fit well, robust χ 2(14, N = 908) = 114.90, p < 0.001, CFI = 0.99, TLI = 0.98, RMSEA = 0.09 (90% CI: 0.07–0.11), SRMR = 0.03. Finally, the SAS-SV PSU CFA fit reasonably well except for RMSEA (as expected often with ordinal data, Shi et al., 2020), robust χ 2(33, N = 908) = 522.89, p < 0.001, CFI = 0.95, TLI = 0.93, RMSEA = 0.13 (90% CI: 0.12–0.14), SRMR = 0.05.
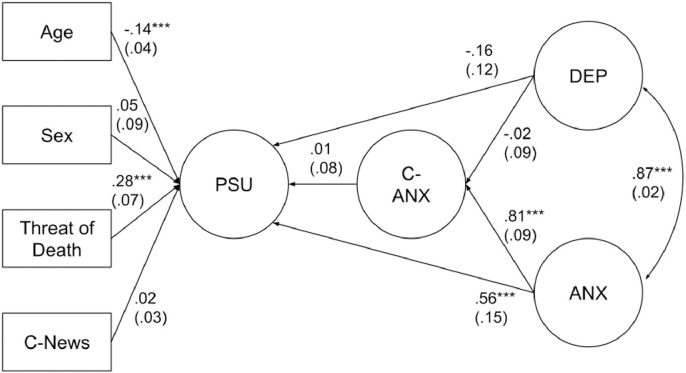
The hypothesized Research Model from Fig. 1 fit well, χ 2(548, N = 908) = 1833.51, p < 0.001, CFI = 0.95, TLI = 0.95, RMSEA = 0.05 (90% CI: 0.05–0.05), SRMR = 0.08. Fig. 3 displays direct effects, demonstrating that COVID-19 anxiety was significantly associated with general anxiety (H2a) but not with depression (H2b) severity. Controlling for covariates, COVID-19 anxiety was associated with PSU severity (H1). Younger age and perceived threat of death also related to PSU severity, controlling for covariates. COVID-19 anxiety mediated relations between general anxiety and PSU severity, β = 0.37, SE = 0.06, z = 6.27, p < 0.001 (H3a). However, COVID-19 anxiety did not mediate relations between depression and PSU severity, β = −0.03, SE = 0.05, z = −0.52, p = 0.60 (rejecting H3b).
Fig. 3.
Hypothesized model with standardized path coefficients. Legend: DEP = Depression; ANX = Anxiety; C-ANX = COVID-19-related anxiety; PSU = Problematic smartphone use; C-News = COVID-19-related news exposure; Threat of Death = Perceived threat of death from COVID-19. Circles represent latent variables, while rectangles indicate observed variables. Standard errors are displayed in parentheses. For visual simplicity, factor loading paths from the latent variables are not displayed, but estimates can be requested from the first author. Sex was coded “1‽ for men, and “2‽ for women. Threat of death was coded “1‽ for “yes,” and “0‽ for “no.” * p < 0.05, ** p < 0.01, *** p < 0.001.
We tested a variation of our Research Model by adding paths from general anxiety and depression to PSU severity (displayed in Fig. 4 ). This model fit well, robust χ 2(546, N = 908) = 1777.50, CFI = 0.95, TLI = 0.95, RMSEA = 0.05 (90% CI: 0.05–0.05), SRMR = 0.08, fitting significantly better than the hypothesized model, DIFFTEST robust , p < 0.001. Fig. 4 demonstrates that the revised model produced similar findings to the hypothesized model, with one major difference; specifically, after controlling for general anxiety and depression on PSU severity, COVID-19 anxiety was no longer a significant predictor of PSU severity. Relatedly, the anxiety->COVID-19 anxiety->PSU mediation effect was no longer significant.
4. Discussion
Our primary findings demonstrate that (a) COVID-19 anxiety was associated with PSU severity and (b) COVID-19 anxiety mediated relations between predisposing general anxiety with PSU severity. However, when adjusting for general anxiety and depression on PSU, only general anxiety (but not COVID-19 anxiety) was significantly related to PSU severity. We found possible prevalence of at least moderate anxiety in 24% of participants, and at least moderate depression in 12% of participants. These findings roughly correspond to other COVID-19 community estimates, ranging from 23–28% for moderate anxiety and 17–48% for moderate depression (Gao et al., 2020; Wang et al., 2020). Results on anxiety and depression prevalence in other countries affected by COVID-19 should become available in the near future.
Supporting H1, we discovered that COVID-19 anxiety was associated with PSU severity in bivariate analyses and SEM using our hypothesized Research Model. Anxiety correlates with PSU severity across the literature (Elhai et al., 2019a; Yang et al., 2020). The relationship between COVID-19 anxiety with PSU severity fits with the I-PACE conceptualization of responses to environmental stressors driving excessive internet use to alleviate negative emotion (Brand et al., 2019, 2016). Thus, in order to manage anxiety from COVID-19 and associated social isolation, especially in light of home quarantine and absence of numerous other activities, many people may engage in PSU. In fact, research shows that social isolation particularly influences negative affectivity (Hawkley and Cacioppo, 2010; Leigh-Hunt et al., 2017).
In our revised SEM, however, when adding and controlling for general anxiety and depression as predictors of PSU severity, COVID-19 anxiety no longer related to PSU. Thus while COVID-19 anxiety on its own (in SEM) was significantly related to PSU severity, controlling for general anxiety and depression rendered this relationship non-significant. Despite significant concerns about COVID-19, people have other everyday-life worries and anxiety (captured by our general anxiety assessment) that have not ceased, but probably increased, with COVID-19′s onset. For example, everyday anxiety involving social and intimate relationship formation and maintenance (Lindesay et al., 2006) would naturally exacerbate with home quarantine (Xiang et al., 2020), and increase the fear of missing out on rewarding experiences (Elhai et al., 2020b; Elhai et al., in pressb). Similarly, existing anxiety regarding finances, employment, and economic stability (Lindesay et al., 2006) have risen because of the economic toll of the COVID-19 pandemic (Pew Research Center, 2020). Such everyday anxieties, exacerbated because of the outbreak, may supercede COVID-19-specific anxiety, especially in low mortality risk COVID-19 groups, resulting in adverse outcomes such as PSU. But, specifically fearing death from COVID-19 (from medical vulnerability, or excessive worry) may especially result in greater PSU severity to alleviate negative emotion, consistent with our findings from bivariate and SEM models.
It is plausible that a feedback loop may operate, whereby people manage their COVID-19 anxiety by excessively using their smartphones, but in-so-doing inadvertently learn more about COVID-19 from news, further fueling their anxiety and increased smartphone use. In fact, more frequent social media exposure to COVID-19 has been shown to be positively associated with anxiety symptoms (Gao et al., 2020). However, contrary to such a feedback loop, we did not find COVID-19 news exposure related to PSU severity. People likely use many other features of their smartphones to cope with negative emotion from COVID-19, including non-social features such as entertainment from TV and movies (Kang et al., 2020, March 26), even though increased non-social smartphone use is most related to PSU severity (Elhai et al., 2020a, 2017). These findings are comparable to findings on anxiety resulting from social media use during prior recent pandemics (discussed in Taylor, 2019, pp. 74–76)
COVID-19 anxiety was bivariately related to general anxiety and depression severity, consistent with H2 and Ahorsu et al. (in press), but only related to general anxiety in our SEM models. These findings generally fit with the I-PACE conceptualization of psychopathology, such as anxiety and depression influencing excessive internet/smartphone use. In fact, anxiety and worry are known to cause greater anxiety from a viral outbreak (Asmundson and Taylor, 2020a; Taylor, 2019), especially among those with health anxiety misinterpreting physical sensations as viral symptoms (Asmundson and Taylor, 2020b). Therefore, people with pre-existing anxiety in particular may excessively worry about COVID-19, driving overwhelming demand for medical services and hospital beds (Asmundson and Taylor, 2020a). Achieving the right balance between promoting social distancing but not excessive worry is clearly important.
We discovered that COVID-19 anxiety mediated relations between general anxiety and PSU severity in our hypothesized Research Model, supporting H3. This finding is consistent with the I-PACE conceptualization of affective/cognitive responses (including responses to environmental stressors) as mechanisms explaining the psychopathology-excessive internet use relationship (Brand et al., 2019, 2016). Prior work supports this conceptualization for affective/cognitive responses (e.g., Elhai et al., in pressa; Wegmann et al., 2017; Wolniewicz et al., 2020). However, mediation results were not supported for depression in the hypothesized model, nor for either psychopathology predictor in the revised SEM.
The research reported in our paper has several limitations. We used a convenience sample from only one large city in China. Because of quarantine, we were unable to interview participants in-person; therefore, we were limited to online self-report scales, while structured diagnostic interviews would be more accurate. Relevantly, we used self-reported problematic smartphone use, while objective measurement is more accurate (Ryding and Kuss, 2020). Additionally, our data were collected cross-sectionally and, therefore, causal interpretations cannot be confidently made. Nonetheless, our results provide initial data on mental health status of people affected by COVID-19, and relations between COVID-19 anxiety with PSU severity as a coping mechanism. These results provide a foundation from which we and other researchers can pursue further investigation of the impact of the COVID-19 pandemic on smartphone use generally and in the context of developing strategies to reduce COVID-19-related PSU in particular.
Contributors
Jon Elhai, Dean McKay and Haibo Yang designed the study protocol. Haibo Yang conducted data collection and acquisition. Jon Elhai and Haibo Yang conducted data management, and Jon Elhai conducted data analyses. Jon Elhai wrote the initial manuscript, Dean McKay edited, and Gordon Asmundson substantially revised the manuscript. Jon Elhai, Dean McKay, and Haibo Yang had full access to the data.
Role of the funding source
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Availability of data and material
Data and survey materials will be made available upon request.
Declaration of Competing Interest
The authors report no conflicts of interest with this paper's study. Outside the scope of the present paper, Dr. Elhai notes that he receives royalties for several books published on posttraumatic stress disorder (PTSD); is a paid, full-time faculty member at University of Toledo; is a paid, visiting scientist at Tianjin Normal University; occasionally serves as a paid, expert witness on PTSD legal cases; and receives grant research funding from the U.S. National Institutes of Health and Department of Defense. Also outside the scope of the present paper, Dr. McKay notes that he receives royalties for several books written on anxiety disorders in adults and children, obsessive-compulsive disorder, and research methodology; is a paid full-time faculty member at Fordham University; holds a research fellow position in a joint relationship between Fordham University and Columbia University; and has private grant funding from a venture capital research corporation to investigate methods of reducing public speaking fears.
Acknowledgments
None.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jad.2020.05.080.
Appendix. Supplementary materials
References
- Ahorsu, D.K., Lin, C.-Y., Imani, V., Saffari, M., Griffiths, M.D., Pakpour, A.H., in press. The fear of COVID-19 scale: development and initial validation. Int. J. Ment. Health Addict.. [DOI] [PMC free article] [PubMed]
- Angus Reid Institute, 2020, February 5. Half of Canadians taking extra precautions as coronavirus continues to spread around the globe. http://angusreid.org/wp-content/uploads/2020/02/2020.02.04_Coronavirus.pdf.
- Asmundson G.J.G., Taylor S. Coronaphobia: fear and the 2019-nCoV outbreak. J. Anxiety Disord. 2020;70 doi: 10.1016/j.janxdis.2020.102196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asmundson G.J.G., Taylor S. How health anxiety influences responses to viral outbreaks like COVID-19: what all decision-makers, health authorities, and health care professionals need to know. J. Anxiety Disord. 2020;71 doi: 10.1016/j.janxdis.2020.102211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brand M., Wegmann E., Stark R., Muller A., Wolfling K., Robbins T.W., Potenza M.N. The interaction of person-affect-cognition-execution (I-PACE) model for addictive behaviors: update, generalization to addictive behaviors beyond internet-use disorders, and specification of the process character of addictive behaviors. Neurosci. Biobehav. Rev. 2019;104:1–10. doi: 10.1016/j.neubiorev.2019.06.032. [DOI] [PubMed] [Google Scholar]
- Brand M., Young K.S., Laier C., Wolfling K., Potenza M.N. Integrating psychological and neurobiological considerations regarding the development and maintenance of specific Internet-use disorders: an interaction of person-affect-cognition-execution (I-PACE) model. Neurosci. Biobehav. Rev. 2016;71:252–266. doi: 10.1016/j.neubiorev.2016.08.033. [DOI] [PubMed] [Google Scholar]
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287:112934. doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen B., Liu F., Ding S., Ying X., Wang L., Wen Y. Gender differences in factors associated with smartphone addiction: a cross-sectional study among medical college students. BMC Psychiatry. 2017;17:341. doi: 10.1186/s12888-017-1503-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi S. The roles of media capabilities of smartphone-based SNS in developing social capital. Behav. Inf. Technol. 2018;38:609–620. [Google Scholar]
- Dempsey A., E., O'Brien K.D., Tiamiyu M.F., Elhai J.D. Fear of missing out (FoMO) and rumination mediate relations between social anxiety and problematic Facebook use. Addict. Behav. Rep. 2019;9 doi: 10.1016/j.abrep.2018.100150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doargajudhur, M.S., Dell, P., in press. The effect of bring your own device (BYOD) adoption on work performance and motivation. J. Comput. Inf. Syst..
- Duke E., Montag C. Smartphone addiction, daily interruptions and self-reported productivity. Addict. Behav. Rep. 2017;6:90–95. doi: 10.1016/j.abrep.2017.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elhai J.D., Gallinari E.F., Rozgonjuk D., Yang H. Depression, anxiety and fear of missing out as correlates of social, non-social and problematic smartphone use. Addict. Behav. 2020;105 doi: 10.1016/j.addbeh.2020.106335. [DOI] [PubMed] [Google Scholar]
- Elhai J.D., Levine J.C., Dvorak R.D., Hall B.J. Non-social features of smartphone use are most related to depression, anxiety and problematic smartphone use. Comput. Hum. Behav. 2017;69:75–82. [Google Scholar]
- Elhai J.D., Levine J.C., Hall B.J. The relationship between anxiety symptom severity and problematic smartphone use: a review of the literature and conceptual frameworks. J. Anxiety Disord. 2019;62:45–52. doi: 10.1016/j.janxdis.2018.11.005. [DOI] [PubMed] [Google Scholar]
- Elhai, J.D., Rozgonjuk, D., Alghraibeh, A.M., Levine, J.C., Alafnan, A.A., Aldraiweesh, A.A., Aljooma, S.S., Hall, B.J., in press-a. Excessive reassurance seeking mediates relations between rumination and problematic smartphone use. Bull. Menn. Clin.. [DOI] [PubMed]
- Elhai J.D., Rozgonjuk D., Liu T., Yang H. Fear of missing out is related to repeated measurements of negative affect using experience sampling methodology. J. Affect. Disord. 2020;262:298–303. doi: 10.1016/j.jad.2019.11.026. [DOI] [PubMed] [Google Scholar]
- Elhai J.D., Rozgonjuk D., Yildirim C., Alghraibeh A.M., Alafnan A.A. Worry and anger are associated with latent classes of problematic smartphone use severity. J. Affect. Disord. 2019;246:209–216. doi: 10.1016/j.jad.2018.12.047. [DOI] [PubMed] [Google Scholar]
- Elhai J.D., Yang H., Dempsey A.E., Montag C. Rumination and negative smartphone use expectancies are associated with greater levels of problematic smartphone use: a latent class analysis. Psychiatry Res. 2020;285 doi: 10.1016/j.psychres.2020.112845. [DOI] [PubMed] [Google Scholar]
- Elhai, J.D., Yang, H., Montag, C., in press-b. Fear of missing out (FOMO): overview, theoretical underpinnings, and literature review on relations with severity of negative affectivity and problematic technology use. Braz. J. Psychiatry. [DOI] [PMC free article] [PubMed]
- Elhai J.D., Yang H., Rozgonjuk D., Montag C. Using machine learning to model problematic smartphone use severity: the significant role of fear of missing out. Addict. Behav. 2020;103 doi: 10.1016/j.addbeh.2019.106261. [DOI] [PubMed] [Google Scholar]
- Gao J., Zheng P., Jia Y., Chen H., Mao Y., Chen S., Wang Y., Fu H., Dai J. Mental health problems and social media exposure during COVID-19 outbreak. PLoS One. 2020;15 doi: 10.1371/journal.pone.0231924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley L.C., Cacioppo J.T. Loneliness matters: atheoretical and empirical review of consequences and mechanisms. Ann. Behav. Med. 2010;40:218–227. doi: 10.1007/s12160-010-9210-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes A.F. second ed. Guilford; New York, New York: 2017. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. [Google Scholar]
- He X.Y., Li C.B., Qian J., Cui H.S., Wu W.Y. Reliability and validity of a generalized anxiety disorder scale in general hospital outpatient. Shanghai Arch. Psychiatry. 2010;22:200–203. [Google Scholar]
- Kang, C., Alba, D., Satariano, A., 2020, March 26. Surging Traffic Is Slowing Down Our Internet, New York Times. New York Times. https://www.nytimes.com/2020/03/26/business/coronavirus-internet-traffic-speed.html.
- Kardefelt-Winther D. A conceptual and methodological critique of internet addiction research: towards a model of compensatory internet use. Comput. Hum. Behav. 2014;31:351–354. [Google Scholar]
- Kwon M., Kim D.J., Cho H., Yang S. The smartphone addiction scale: development and validation of a short version for adolescents. PLoS One. 2013;8:e83558. doi: 10.1371/journal.pone.0083558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lachmann B., Duke É., Sariyska R., Montag C. Who's addicted to the smartphone and/or the Internet? Psychol. Pop. Media Cult. 2019;8:182–189. [Google Scholar]
- Lei, P.W., Shiverdecker, L.K., in press. Performance of estimators for confirmatory factor analysis of ordinal variables with missing data. Struct. Equ. Model..
- Leigh-Hunt N., Bagguley D., Bash K., Turner V., Turnbull S., Valtorta N., Caan W. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health. 2017;152:157–171. doi: 10.1016/j.puhe.2017.07.035. [DOI] [PubMed] [Google Scholar]
- Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y., Ren R., Leung K.S.M., Lau E.H.Y., Wong J.Y., Xing X., Xiang N., Wu Y., Li C., Chen Q., Li D., Liu T., Zhao J., Liu M., Tu W., Chen C., Jin L., Yang R., Wang Q., Zhou S., Wang R., Liu H., Luo Y., Liu Y., Shao G., Li H., Tao Z., Yang Y., Deng Z., Liu B., Ma Z., Zhang Y., Shi G., Lam T.T.Y., Wu J.T., Gao G.F., Cowling B.J., Yang B., Leung G.M., Feng Z. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N. Engl. J. Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindesay J., Baillon S., Brugha T., Dennis M., Stewart R., Araya R., Meltzer H. Worry content across the lifespan: an analysis of 16- to 74-year-old participants in the British national survey of psychiatric morbidity 2000. Psychol. Med. 2006;36:1625–1633. doi: 10.1017/S0033291706008439. [DOI] [PubMed] [Google Scholar]
- Liu Q.-Q., Zhou Z.-K., Yang X.-J., Kong F.-C., Niu G.-F., Fan C.-Y. Mobile phone addiction and sleep quality among Chinese adolescents: a moderated mediation model. Comput. Hum. Behav. 2017;72:108–114. [Google Scholar]
- Lopez-Fernandez O. Short version of the smartphone addiction scale adapted to Spanish and French: towards a cross-cultural research in problematic mobile phone use. Addict. Behav. 2017;64:275–280. doi: 10.1016/j.addbeh.2015.11.013. [DOI] [PubMed] [Google Scholar]
- Maydeu-Olivares A. Assessing the size of model misfit in structural equation models. Psychometrika. 2017;82:533–558. doi: 10.1007/s11336-016-9552-7. [DOI] [PubMed] [Google Scholar]
- McKay D., Yang H., Elhai J.D., Asmundson G.J. Anxiety regarding contracting COVID-19 related to interoceptive anxiety sensations: The moderating role of disgust propensity and sensitivity. J. Anxiety Disord. 2020;73:102233. doi: 10.1016/j.janxdis.2020.102233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montag C., Becker B., Gan C. The multipurpose application WeChat: a review on recent research. Front. Psychol. 2018;9:2247. doi: 10.3389/fpsyg.2018.02247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montag C., Walla P., Koller M. Carpe diem instead of losing your social mind: beyond digital addiction and why we all suffer from digital overuse. Cogent Psychology. 2016;3 [Google Scholar]
- Montag, C., Wegmann, E., Sariyska, R., Demetrovics, Z., Brand, M., in press. How to overcome taxonomical problems in the study of internet use disorders and what to do with “smartphone addiction”?J. Behav. Addict. [DOI] [PMC free article] [PubMed]
- Mourra G.N., Senecal S., Fredette M., Lepore F., Faubert J., Bellavance F., Cameron A.F., Labonte-LeMoyne E., Leger P.M. Using a smartphone while walking: the cost of smartphone-addiction proneness. Addict. Behav. 2020;106 doi: 10.1016/j.addbeh.2020.106346. [DOI] [PubMed] [Google Scholar]
- Muthén B.O., Muthén L.K. Mplus, eighth ed., Los Angeles. Muthén & Muthén; California: 2019. [Google Scholar]
- Namwongsa S., Puntumetakul R., Neubert M.S., Boucaut R. Effect of neck flexion angles on neck muscle activity among smartphone users with and without neck pain. Ergonomics. 2019;62:1524–1533. doi: 10.1080/00140139.2019.1661525. [DOI] [PubMed] [Google Scholar]
- Newman N., Levy D.A.L. Reuters Institute for the Study of Journalism; 2014. Reuters Institute Digital News Report 2014, Reuters Institute for the Study of Journalism.http://www.digitalnewsreport.org/survey/2014/ [Google Scholar]
- Norris F.H., Slone L.B., Baker C.K., Murphy A.D. Early physical health consequences of disaster exposure and acute disaster-related PTSD. Anxiety Stress Coping. 2006;19:95–110. [Google Scholar]
- Pew Research Center . Pew Research Center. Pew Research Center; 2020. Worries about Coronavirus Surge, as Most Americans Expect a Recession – or Worse.https://www.people-press.org/2020/03/26/worries-about-coronavirus-surge-as-most-americans-expect-a-recession-or-worse/ [Google Scholar]
- Plummer F., Manea L., Trepel D., McMillan D. Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis. Gen. Hosp. Psychiatry. 2016;39:24–31. doi: 10.1016/j.genhosppsych.2015.11.005. [DOI] [PubMed] [Google Scholar]
- Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. General Psychiatry. 2020;33 doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team, 2020. R: a language and environment for statistical computing. https://www.R-project.org/.
- Ryding F.C., Kuss D.J. Passive objective measures in the assessment of problematic smartphone use: a systematic review. Addict. Behav. Rep. 2020:100257. doi: 10.1016/j.abrep.2020.100257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sha P., Sariyska R., Riedl R., Lachmann B., Montag C. Linking internet communication and smartphone use disorder by taking a closer look at the Facebook and WhatsApp applications. Addict. Behav. Rep. 2019;9 doi: 10.1016/j.abrep.2018.100148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi D., Maydeu-Olivares A., Rosseel Y. Assessing fit in ordinal factor analysis models: SRMR vs. RMSEA. Struct. Equ. Model. 2020;27:1–15. [Google Scholar]
- Taylor S. Cambridge Scholars Publishing; Newcastle Upon Tyne, United Kingdom: 2019. The Psychology of Pandemics: Preparing for the Next Global Outbreak of Infectious Disease. [Google Scholar]
- Vahedi Z., Saiphoo A. The association between smartphone use, stress, and anxiety: a meta-analytic review. Stress Health. 2018;34:347–358. doi: 10.1002/smi.2805. [DOI] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang K., Shi H.S., Geng F.L., Zou L.Q., Tan S.P., Wang Y., Neumann D.L., Shum D.H., Chan R.C. Cross-cultural validation of the depression anxiety stress scale-21 in China. Psychol. Assess. 2016;28:e88–e100. doi: 10.1037/pas0000207. [DOI] [PubMed] [Google Scholar]
- Wegmann E., Oberst U., Stodt B., Brand M. Online-specific fear of missing out and Internet-use expectancies contribute to symptoms of Internet-communication disorder. Addict. Behav. Rep. 2017;5:33–42. doi: 10.1016/j.abrep.2017.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolniewicz C.A., Rozgonjuk D., Elhai J.D. Boredom proneness and fear of missing out mediate relations between depression and anxiety with problematic smartphone use. Hum. Behav. Emerg. Technol. 2020;2:61–70. [Google Scholar]
- Xiang Y.-T., Yang Y., Li W., Zhang L., Zhang Q., Cheung T., Ng C.H. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7:228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang J., Fu X., Liao X., Li Y. Association of problematic smartphone use with poor sleep quality, depression, and anxiety: a systematic review and meta-analysis. Psychiatry Res. 2020;284 doi: 10.1016/j.psychres.2019.112686. [DOI] [PubMed] [Google Scholar]
- Zanon, C., Brenner, R.E., Baptista, M.N., Vogel, D.L., Rubin, M., Al-Darmaki, F.R., Gonçalves, M., Heath, P.J., Liao, H.Y., Mackenzie, C.S., Topkaya, N., in press. Examining the dimensionality, reliability, and invariance of the depression, anxiety, and stress scale–21 (DASS-21) across eight countries. Assessment. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data and survey materials will be made available upon request.