Highlights
-
•
Does subjective age moderate the relationship between loneliness and psychiatric symptoms among older adults during the COVID-19 pandemic?
-
•
Loneliness due to the COVID-19 pandemic was weakly associated with psychiatric symptoms among older adults who felt younger than their age. Older adults who had an older subjective age were more susceptible to the adverse concomitants of loneliness.
-
•
Subjective age may help identify older adults who are most at risk to suffer from loneliness during the COVID-19 pandemic, and interventions can aim at ameliorating both loneliness and older subjective age.
Key Words: Loneliness, Subjective age, Psychiatric symptoms, COVID-19
Abstract
Objective
The study examined whether subjective age moderated the relationship between loneliness due to the COVID-19 pandemic and psychiatric symptoms.
Methods
A convenience sample of older adult Israelis (N = 277, mean age = 69.58 ± 6.72) completed web-based questionnaires comprising loneliness, anxiety, depressive, and peritraumatic distress symptoms. They also reported how old they felt.
Results
The positive relationship between loneliness due to the COVID-19 pandemic and psychiatric symptoms was weak among those who felt younger than their age while this very same relationship was robust among those feeling older.
Conclusions
Young subjective age may weaken the loneliness-symptom association among older adults during the COVID-19 pandemic. Older adults holding an older age identity are more susceptible to the adverse effects of loneliness. Although preliminary, the findings may inform screening and interventions. Subjective age may help identify those at high risk in suffering from loneliness, and suggest interventions aimed at ameliorating both loneliness and older subjective ages.
OBJECTIVE
In response to the coronavirus disease 2019 (COVID-19) pandemic, a global policy of social distancing was initiated. Although circumstances necessitate such extreme measures, this social isolation places individuals at risk for adverse health effects.1 Older adults at greater risk for COVID-19 health complications will likely remain in strict self-isolation longer than other age groups; therefore, the effects of isolation and ensuing loneliness may be especially severe for them.2
Loneliness reflects subjective distress resulting from a discrepancy between desired and perceived social relationships.3 Unfortunately, loneliness causes a host of poor outcomes such as depression, anxiety, physical morbidity, and mortality.3 These findings stress the need to rapidly assess the concomitants of loneliness among older adults during the COVID-19 pandemic.
Older adults considerably vary in health status and coping mechanisms; a critical goal is to map risk assessment: who is more susceptible and who is relatively resilient to effects of loneliness. While prior works focused on chronological age as a modifier of the effects of loneliness,3 it is possible that the age at which individuals perceive themselves to be, or their subjective age, would be a more potent moderator. Evidence shows that relative to those feeling younger, older adults with an older subjective age were more prone to a myriad of adverse health outcomes including physical impairment and higher mortality risk.4 Moreover, older adults feeling older were more susceptible to the effects of stress.4
Subjective age can potentially moderate effects of loneliness on psychiatric symptoms as an older age identity may reflect the internalization of negative age stereotypes.4 Accordingly, feeling old indicates viewing oneself as weak and viewing loneliness as an unavoidable part of aging, thereby inhibiting coping behaviors when in self-isolation. Second, negative health conditions accompanying old subjective age, such as inflammation and health-risk behaviors,4 can aggravate the noxious effects of loneliness when an old age identity exists.
We therefore hypothesized that loneliness due to the COVID-19 pandemic would be related to higher levels of psychiatric symptoms (i.e., anxiety, depressive, and peritraumatic distress symptoms) among older adults, especially among those feeling older. The loneliness-symptom association was hypothesized to be weaker as subjective age is younger.
METHODS
Participants and Procedure
Using the Qualtrics web-based platform, we collected data across Israel between March 16 and April 14, 2020. On the last day of data collection, 12,361 Israelis were tested positive for the coronavirus and 123 had died. The sample included 277 older adults (mean age = 69.58 ± 6.72, range 60–92). Most of them were women (n = 191, 69.0%), married or cohabitating (n = 204, 73.6%), with tertiary education (n = 201, 72.8%). Less than half of the sample (n = 115, 42.9%) reported having chronic medical conditions suspected to increase the risk of death due to COVID-19 complications. The majority rated their health as good or very good (n = 178, 64.5%).
The online questionnaire was disseminated across multiple social media resources and contact lists provided by organizations (e.g., continuing-care retirement communities, institutions hosting educational activities for older adults). All participants provided an informed consent. Ethical approval was received from the institutional review board at the authors’ University.
Measures
Participants completed background characteristics, including age, gender, marital status, and education (rated from 1 = without formal education to 6 = formal tertiary education). They noted whether they have chronic medical conditions suspected to increase the risk of death due to COVID-19 complications (i.e., cardiovascular disease, diabetes, chronic respiratory disease, hypertension, and cancer), and rated their health on a scale ranging from 1 (not good at all) to 5 (very good). Exposure to COVID-19 pandemic-related events was the sum score of six events. Behavioral change due to the pandemic was the sum of eleven changed behaviors (details presented in the Supplementary file).
Participants completed the below measures while being asked to refer directly to feelings and symptoms they experience during the COVID-19 crisis and due to it.
Subjective age was assessed by a 4-item scale referring to mental, physical, behavioral, and appearance-related aspects of age identity.5 Each aspect was rated on a 5-point scale (1 = feeling much younger than my age to 5 = feeling much older than my age). Ratings were averaged with higher scores reflecting an older age identity. Internal reliability was good (α = 0.82).
Loneliness was assessed with the 3-item version of the UCLA Loneliness Scale.6 Items were rated on a 5-point scale (1 = not at all to 5 = almost always). Ratings were averaged with higher scores reflecting increased loneliness. Internal reliability was good (α = 0.81)
Anxiety symptoms were assessed with the 7-item Generalized Anxiety Disorder (GAD-7) scale.7 Participants rated their symptoms during the last 2 weeks on a 4-point scale (0 = not at all to 3 = almost every day). Ratings were summed with higher scores reflecting increased anxiety. Internal reliability was good (α = 0.89).
Depressive symptoms were assessed with the 9-item Patient Health Questionnaire (PHQ-9).8 Participants rated their symptoms in the last 2 weeks on a 4-point scale (0 = not at all to 3 = almost every day). Ratings were summed with higher score reflecting increased depressive symptoms. Internal reliability was good (α = 0.85).
Peritraumatic distress symptoms were assessed with the 13-item Peritraumatic Distress Inventory (PDI).9 Participants rated their symptoms on a 5-point scale (0 = not at all true to 4 = extremely true). Ratings were summed with higher scores reflecting increased distress. Internal reliability was good (α = 0.84).
RESULTS
As typical, respondents felt on average younger than their age (M = 2.45 ± 0.51). Although the mean loneliness (M = 2.28 ± 0.90) and psychiatric symptom scores (GAD-7: M = 2.95 ± 3.82, PHQ-9: M = 3.33 ± 4.10, PDI: M = 9.45 ± 6.51) were generally low, there was marked variability among respondents.
Loneliness was positively correlated with GAD-7, PHQ-9, and PDI (r(273) = 0.31, r(273) = 0.30, r(272) = 0.37, respectively, all p's <0.001,). Feeling older was also positively correlated with GAD-7, PHQ-9, and PDI (r(270) = 0.28, r(270) = 0.23, r(270) = 0.25, respectively, all p's <0.001).
Few participants reported being tested positive for the coronavirus or being in self-isolation (n = 46, 16.6%), yet most knew someone who tested positive or was in self-isolation (n = 166, 59.9%). All respondents reported changing at least one behavior due to the pandemic (ranging from buying more food and water than usual: n = 91, 32.9%, to going out less frequently: n = 246, 88.8%). For additional descriptive statistics see Supplementary file.
To test the study's hypotheses, we performed three hierarchical regression analyses. Significant interactions were probed using PROCESS.10 Psychiatric symptoms (GAD-7, PHQ-9, and PDI) were regressed on background characteristics (age, gender, education, and marital status) in Step 1, variables related to COVID-19 exposure and potential complications (self-rated health, chronic medical conditions related to COVID-19 complications, COVID-19 pandemic related events, and behavioral change due to the pandemic) in Step 2, loneliness in Step 3, subjective age in Step 4, and the Loneliness*Subjective age interaction in Step 5.
Results reveal that after controlling for demographics and COVID-19-related variables, those reporting feeling lonely (ΔR2 ranged 0.07–0.10) and those feeling older (ΔR2 ranged 0.01–0.04), also reported higher symptoms. Furthermore, all three Loneliness*Subjective age interactions were significant, explaining an additional 3%–4% variance in psychiatric symptoms (Table 1 ).
TABLE 1.
Hierarchical Linear Regression Predicting Psychiatric Symptoms
| GAD-7 |
PHQ-9 |
PDI |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| B (SE) | β | t | B (SE) | β | t | B (SE) | β | t | |
| Step 1 | ΔR2 = 0.07, F(4,255) = 4.62b | ΔR2 = 0.07, F(4,255) = 4.73b | ΔR2 = 0.07, F(4,255) = 4.77b | ||||||
| Age | −0.03 (.03) | −0.06 | −0.95 | −0.04 (0.04) | −0.06 | −0.98 | −0.11 (0.06) | −0.12 | −1.93 |
| Gender (woman) | 1.18 (0.53) | 0.14a | 2.25 | 1.35 (0.56) | 0.15a | 2.42 | 1.60 (0.90) | 0.11 | 1.78 |
| Education | −1.03 (0.27) | −0.23c | −3.81 | −1.07 (0.28) | −0.23c | −3.74 | −1.70 (0.46) | −0.23c | −3.68 |
| Marital status (married) | 0.42 (0.54) | 0.05 | 0.77 | 0.23 (0.57) | 0.03 | 0.40 | −0.13 (0.93) | −0.01 | −0.14 |
| Step 2 | ΔR2 = 0.01, F(4,251) = 0.80 | ΔR2 = 0.03, F(4,251) = 1.99 | ΔR2 = 0.05, F(4,251) = 3.33a | ||||||
| Subjective health | −0.30 (0.30) | −0.07 | −1.02 | −0.67 (0.31) | −0.15a | −2.13 | −1.39 (0.50) | −0.20b | −2.77 |
| Chronic conditions related to COVID-19 complications | −0.43 (0.56) | −0.05 | 0.76 | −0.79 (0.58) | −0.10 | −1.35 | −1.71 (0.94) | −0.13 | −1.83 |
| COVID-19 pandemic related events | 0.11 (0.22) | 0.03 | 0.46 | 0.11 (0.24) | 0.03 | 0.46 | −0.19 (0.38) | −0.03 | −0.50 |
| Behavioral change due to COVID-19 pandemic | 0.12 (0.10) | 0.08 | 1.27 | 0.17 (0.10) | 0.10 | 1.63 | 0.35 (0.17) | 0.13a | 2.11 |
| Step 3 | ΔR2 = 0.08, F(1,250) = 23.31c | ΔR2 = 0.07, F(1,250) = 22.05c | ΔR2 = 0.10, F(1,250) = 32.10c | ||||||
| Loneliness | 1.25 (0.26) | 0.29c | 4.82 | 1.28 (0.27) | 0.28c | 4.70 | 2.43 (0.43) | 0.33c | 5.66 |
| Step 4 | ΔR2 = 0.04, F(1,249) = 12.30b | ΔR2 = 0.01, F(1,249) = 3.88a | ΔR2 = 0.02, F(1,249) = 7.33b | ||||||
| Subjective age | 1.64 (0.47) | 0.22b | 3.51 | 0.99 (0.50) | 0.13a | 1.97 | 2.11 (0.78) | 0.17b | 2.71 |
| Step 5 | ΔR2 = 0.03, F(1,248) = 9.96c | ΔR2 = 0.04, F(1,248) = 13.17c | ΔR2 = 0.04, F(1,248) = 15.21c | ||||||
| Loneliness X subjective age | 1.14 (0.36) | 0.20b | 3.15 | 1.40 (0.38) | 0.23c | 3.63 | 2.34 (0.60) | 0.24c | 3.90 |
| Full model | R2 = 0.23, F(11,248) = 6.67c | R2 = 0.22, F(11,248) = 6.53c | R2 = 0.28, F(11,248) = 8.91c | ||||||
Notes: N = 260. All continuous variables were mean-centered before analyses. In each subsequent step, only the new variables are shown (and not those from previous steps). df for t test values are identical to the denominator df noted in each step (df2). We have corrected for our multiple tests using the Benjamini and Hochberg's false discovery rate method.12 All three interactions remained significant (interaction p value for GAD-7, PHQ-9, and PDI was 0.001, 0.0004, and 0.0003, respectively). GAD-7 = anxiety symptoms; PHQ-9 = depressive symptoms; PDI, peritraumatic symptoms.
p ≤0.05.
p ≤0.01.
p ≤0.001.
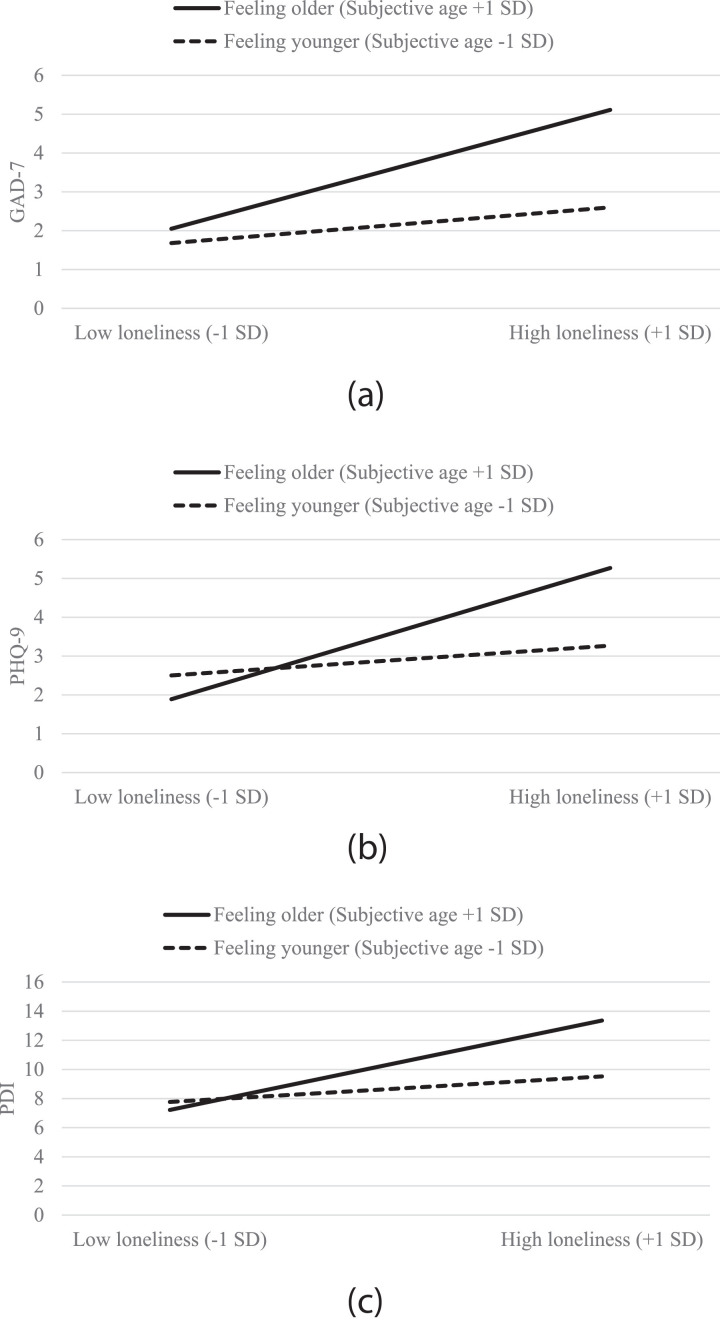
Thus, when subjective age was +1 SD above the average (i.e., having an older subjective age), the relationship between loneliness and psychiatric symptoms was strong (GAD-7: B = 1.70, t(248) = 5.62, p <0.001; PHQ-9: B = 1.88, t(248) = 5.86, p <0.001; PDI: B = 3.42, t(248) = 6.82, p <0.001). However, for young subjective ages (−1 SD below the average) the loneliness-psychiatric symptoms association was nonsignificant (GAD-7: B = 0.51, t(248) = 1.56, p = 0.12; PHQ-9: B = 0.43, t(248) = 1.23, p = 0.22; PDI: B = 0.98, t(248) = 1.81, p = 0.07) (Fig. 1 ).
Figure 1.
The interaction between loneliness and subjective age on (a) anxiety symptoms (GAD-7), (b) depressive symptoms (PHQ-9), and (c) peritraumatic symptoms (PDI).
CONCLUSIONS
To the best of our knowledge, this is the first study assessing the psychiatric correlates of loneliness among older adults during the COVID-19 pandemic. As hypothesized, the association between loneliness and psychiatric symptoms was significant and robust only among participants with older subjective ages. Among those with young subjective ages, there were no adverse correlates of loneliness. According to recently proposed criteria,11 the current standardized effect sizes for these moderation effects may be considered large.
These findings extend previous evidence highlighting the moderating effect of subjective age when considering the outcomes of stress.4 Future studies should examine the possible mechanisms through which subjective age moderates the effect of loneliness on psychiatric symptomatology. We postulated the straightforward mechanism of internalization of negative age stereotype.4 Yet other possibilities may exist, such as negative biological mechanism and other behavioral concomitants of old age identity.4
Our findings should be assessed in light of the study's limitations. The current design was cross-sectional precluding conclusions regarding causality. Moreover, the online design biased the sample towards populations with an access to or literacy in digital resources and those who may be more socially connected, at least virtually, and thus may experience lower loneliness. Finally, there was no measurement of prepandemic levels of loneliness and distress.
Still the current preliminary findings may inform screening and interventions with older adults both during the COVID-19 pandemic, and probably in assisting with post-COVID-19 damage control. Subjective age can offer some direction in identifying older adults at high risk to effects of loneliness. Moreover, online or telephone interventions targeting both loneliness3 and age identity4 may be provided to older adults enduring imposed isolation in order to bolster therapeutic effects.
AUTHOR CONTRIBUTIONS
All authors substantially contributed to the conception and design of the study and to the acquisition of data. AS performed the analysis, interpreted the data and drafted the work; all authors performed critical revision of the paper for important intellectual content and finally approved of the version to be published.
All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Disclosure
No disclosures/conflict of interest to report.
Footnotes
Supplementary material associated with this article can be found, in the online version, at https://doi.org/10.1016/j.jagp.2020.05.018.
Appendix. SUPPLEMENTARY MATERIALS
References
- 1.Brooks SK, Webster RK, Smith LE. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vahia IV, Blazer DG, Smith GS. COVID-19, mental health and aging: a need for new knowledge to bridge science and service. Am J Geriatr Psychiatry. 2020 doi: 10.1016/j.jagp.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jeste DV, Lee EE, Cacioppo S. Battling the modern behavioral epidemic of loneliness: suggestions for research and interventions. JAMA Psychiatry. 2020;77:553–554. doi: 10.1001/jamapsychiatry.2020.0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stephan Y, Sutin AR, Terracciano A. Determinants and implications of subjective age across adulthood and old age. In: Ryff C, Krueger RF, editors. The Oxford Handbook of Integrative Health Science. Oxford University Press; New York, NY: 2018. pp. 87–96. Edited by. [Google Scholar]
- 5.Kastenbaum R, Derbin V, Sabatini P. “The ages of me”: toward personal and interpersonal definitions of functional aging. Int J Aging Hum Dev. 1972;3:197–211. [Google Scholar]
- 6.Hughes ME, Waite LJ, Hawkley LC. A short scale for measuring loneliness in large surveys: results from two population-based studies. Res Aging. 2004;26:655–672. doi: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Spitzer RL, Kroenke K, Williams JB. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 8.Kroenke K, Spitzer RL, Williams JB. The PHQ‐9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brunet A, Weiss DS, Metzler TJ. The peritraumatic distress inventory: a proposed measure of PTSD criterion A2. Am J Psychiatry. 2001;158:1480–1485. doi: 10.1176/appi.ajp.158.9.1480. [DOI] [PubMed] [Google Scholar]
- 10.Hayes AF. Guilford Press; New York, NY: 2013. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. [Google Scholar]
- 11.Bodner TE. Standardized effect sizes for moderated conditional fixed effects with continuous moderator variables. Front Psychol. 2017;21:562. doi: 10.3389/fpsyg.2017.00562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc B. 1995;57:289–300. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.