Introduction
The American Association of Gynecologic Laparoscopists joins the American Society of Reproductive Medicine, the American Urogynecologic Society, International Federation of Fertility Societies, International Gynecologic Cancer Society, Society of Family Planning, Society of Gynecologic Oncology, Society of Gynecologic Surgeons, and the Society for Reproductive Surgeons, in providing the following recommendations for obstetrician-gynecologists during the COVID-19 pandemic.
Traditionally, surgical procedure prioritization depends on illness acuity and resource availability after shared decision making with patients. During an emergency such as the coronavirus disease (COVID-19) pandemic, decisions must take into consideration new influences on the safety of benign gynecologic procedures. The prioritization of patients must be fluid as the pandemic waxes and wanes and is likely different in the peaks than the troughs of infection incidence. At the peak of the infectious curve, all surgeries except those that are a threat to life or limb are cancelled, as the risk to individuals coming out of self-isolation is high and could overwhelm already taxed healthcare resources. The trough represents a new normal, in which the risk of COVID-19 infection still remains but at a diminished rate. In the trough, the risk of infection to individuals scheduled for surgery must be weighed against the morbidity of their benign condition. In this scenario, surgeries for patients with severe comorbidities or those who would require rehabilitation or a skilled nursing facility after surgery should likely be delayed until a vaccine or effective therapy is available. (If surgery cannot be realistically postponed until a vaccine or effective therapy is available, counseling about potential associated COVID-19 infection with accompanying morbidity and mortality should be a component of informed consent when patients are anticipated to need rehabilitation or a skilled nursing facility). Between peak and trough, the decision to proceed with surgery lies in between the 2 extremes. In the deceleration phase, liberalizing restrictions should start with individuals with urgent conditions who are severely affected by their gynecologic condition, weighed against their underlying health condition. How to prioritize surgeries, weighed against the risk to patients undergoing surgery during a pandemic, has necessitated the development of tiered systems that can adapt to quickly changing environments.
The American College of Surgeons (ACS) developed several tiered ranking systems for prioritization of surgeries [1,2]. The first scale outlines how an institution should prioritize staffing and use of resources and ranges from “Alert” to “Condition Zero” on the basis of the number of patients with COVID-19 who are admitted to the hospital. The second scale is the “Elective Surgery Acuity Scale.” This is a tiered scale ranging from 1 to 3; the first tier is elective surgeries, the middle tier is urgent surgeries, and the third tier is emergency surgeries. Each tier is further dichotomized into patients with and without significant comorbidities. Similar to the ACS tiered response, Goldman and Haber [3] described a tiered system ranging from 0, emergency surgeries and outpatient procedures that should be performed at the peak of the curve to 4, nonessential surgeries that can be delayed until the threat of infection has subsided for urologic procedures In addition, there has been a publication by Weber LeBrun et al [4] that outlines the initial response to the COVID-19 pandemic but does not follow the ACS tier system.
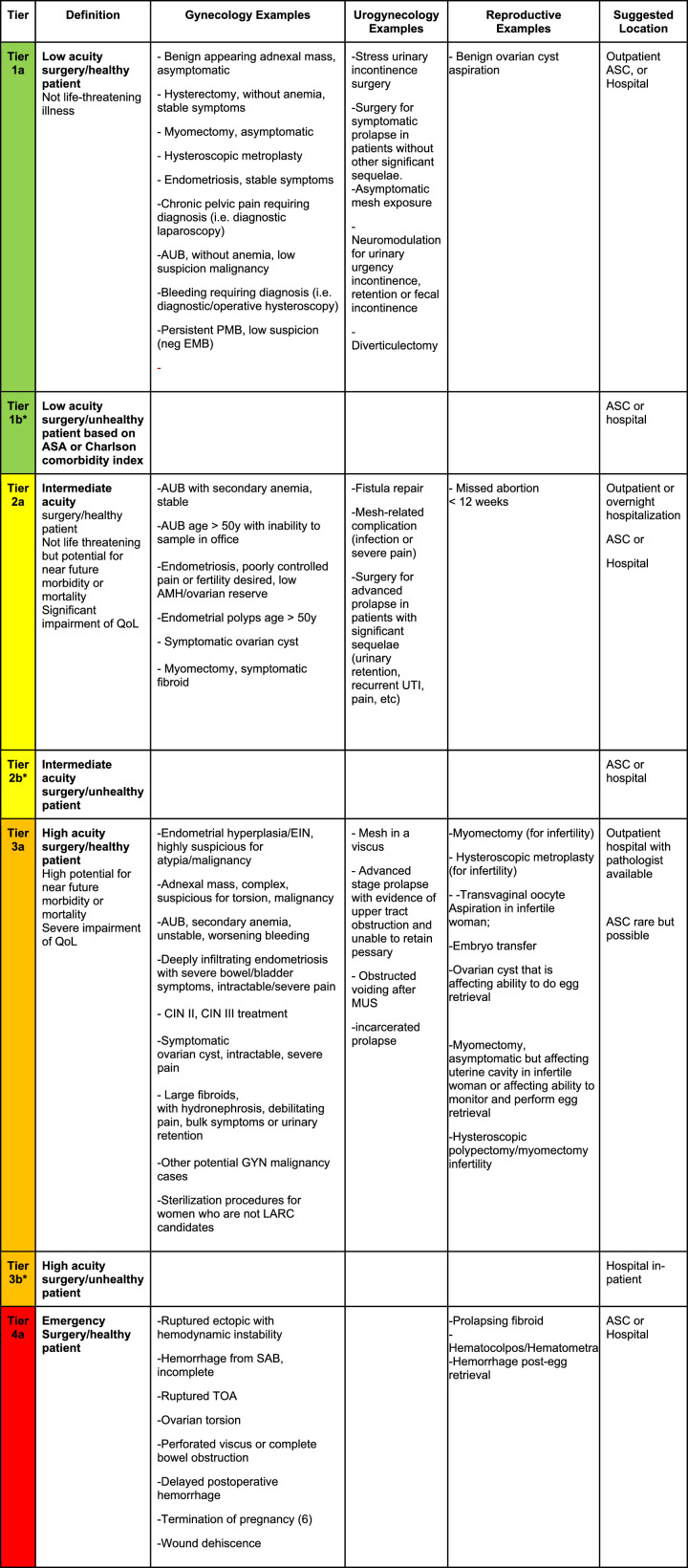
We have adapted the ACS tiered ranking list to develop guidance for urogynecologic and benign gynecologic surgeons (Fig. 1 ). The system is meant to help surgeons and their healthcare systems decide who should go to the operating room as the pandemic unfolds and does not list all elective surgeries in each tier. This guidance is not meant as a substitute for clinical judgment of an individual surgeon and the process of shared decision making with patients. This is particularly important for women with medical comorbidities in whom increased exposure to infected individuals outside the home outweighs the urgency of their gynecologic condition. The continued use of telemedicine to address symptom management while surgery is delayed may be helpful.
Fig. 1.
Modified Elective Surgery Acuity Scale for benign gynecologic indications and surgeries. *Tier b indicates patients with complicated medical conditions that, in the environment of COVID-19, may place them at high-risk for ICU admission and increased perioperative morbidity and mortality. This will likely affect the order of prioritization of individuals for surgery. For example, in an environment where we are just opening surgical suites, we may determine that even though the acuity of the surgical problem is high, the tier 3b women would not go to surgery before the tier 2a women. By contrast, when the risk of COVID-19 morbidity and mortality is lower, a tier 3b woman might go ahead of a tier 2a woman who is healthy. Ranking of the tiers is dependent on the COVID-19 environment.
AMH = antimüllerian hormone; ASA = American Society of Anaesthesiologists; ASC = ambulatory surgery center; AUB = abnormal uterine bleeding; CIN = CPP = chronic pelvic pain; EIN = endometrial intraepithelial neoplasm; EMB = endometrial biopsy; GYN = gynecologic; ICU = intensive care unit; LARC = long-acting reversible contraception; MUS = midurethral sling; PMB = postmenopausal bleeding; SAB = spontaneous abortion; SIS = saline infusion sonography; TOA = tubo-ovarian abscess; TVUS = transvaginal ultrasonography; UDS = urodynamics; UTI = urinary tract infection.
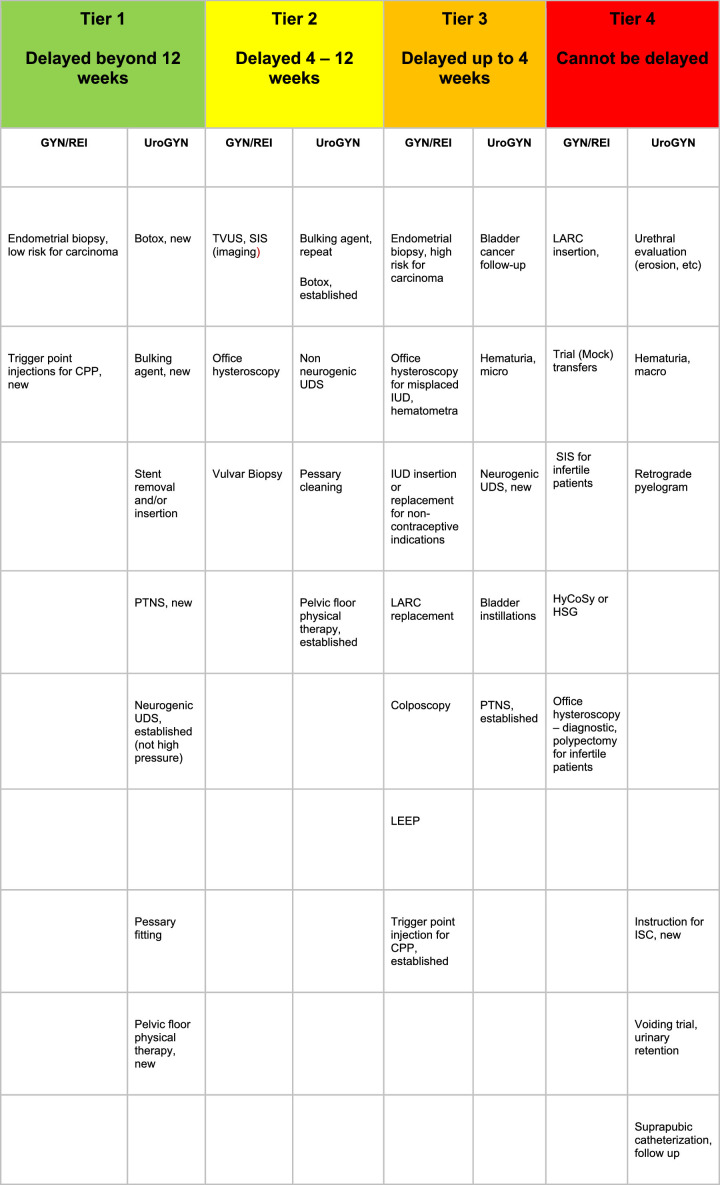
In addition, we have applied the tiered system to outpatient procedures (Fig. 2 ). All decisions should be made in the context of local and state directives. Many places across the globe have been in the “Condition Zero” level of planning in which all but emergency surgeries are cancelled, regardless of the prevalence of COVID-19 cases in a specific area. As we approach reopening surgical services to women with nonemergent surgical problems, a new calculus is needed. The tiered system must take into account the patient's gynecologic condition, as well as their medical comorbidities, and be able to adapt to changing conditions, as we reopen and reclose gynecologic surgery services for women through the pandemic. Surgical technique and personal protective equipment availability must also be considered [5]. Local disease prevalence and reopening strategies may supersede this document, and we defer to clinical decision making in coordination with other local resource considerations [6].
Fig. 2.
Acuity scale for office-based gynecologic procedures. CPP = chronic pelvic pain; GYN = gynecology; HSG = hysterosalpingogram; ISC = intermittent self-catheterization; IUD = intrauterine device; LARC = long-acting, reversible contraception; LEEP = loop electrosurgery excision procedure; PTNS = percutaneous tibial nerve stimulation; REI = reproductive endocrinology and infertility; SIS = saline infusion sonography; TVUS = transvaginal ultrasonography; UDS = urodynamics; UroGYN = urogynecology.
Footnotes
Issued: 4/29/2020
References
- 1.American College of Surgeons. COVID-19: guidance for triage of non-emergent surgical procedures. Available at:https://www.facs.org/covid-19/clinical-guidance/triage. Accessed 21 April 2020.
- 2.Ross SW, Lauer CW, Miles WS. Maximizing the calm before the storm: tiered surgical response plan for COVID-19. Am J Coll Surg. 2020;230:1080–1091. doi: 10.1016/j.jamcollsurg.2020.03.019. e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goldman HB, Haber GP. Editorial Comment. J Urol. 2020;203 doi: 10.1097/JU.0000000000000576.01. 609–609. [DOI] [PubMed] [Google Scholar]
- 4.Weber LeBrun EE, Moawad NS, Rosenberg EI. Coronavirus disease 2019 pandemic: stage management of surgical services for gynecology and obstetrics. Am J Obstet Gynecol. 2020 Apr 3 doi: 10.1016/j.ajog.2020.03.038. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American Society Reproductive Medicine. A message from the SRS and ASRM regarding surgery during the COVID-19 pandemic. Available at: https://www.asrm.org/news-and-publications/news-and-research/announcements/a-message-from-the-srs-and-asrm-regarding-surgery-during-the-covid-19-pandemic/. Accessed June 8, 2020.
- 6.American College of Obstetricians and Gynecologists. Joint statement on abortion access during the COVID-19 Outbreak. Available at:https://www.acog.org/news/news-releases/2020/03/joint-statement-on-abortion-access-during-the-covid-19-outbreak. Accessed 22 April 2020.