Abstract
Background
The coronavirus pandemic has changed health care rapidly and dramatically.
Objective
To provide a critical synthesis of the scientific literature on the pandemic's implications for psychiatric practice.
Methods
A rapid literature review was undertaken to identify scientific literature linking psychiatric outcomes and practice changes due to coronavirus and the disease it causes (COVID-19). A structured quality assessment was used to assess those articles reporting quantitative data.
Results
Fifty articles were identified for inclusion, but only 12 contained original data. Eleven of those twelve were rated as of weak quality. The literature described psychiatric sequelae of the coronavirus and related public health interventions through cross-sectional surveys among different populations; no studies include diagnostic or functional impairment data. Populations at risk include COVID-19 survivors, health care workers, the elderly, and those with preexisting psychiatric disease. Impacts on psychiatric practice were described, again without data on changes to quality or access of care.
Conclusions
There is a quickly accumulating body of evidence on the psychiatric implications of coronavirus including psychological effects on the general public and at-risk subgroups. Similarly, psychiatric practice has witnessed substantial adaptation to the pandemic. However, there remain significant gaps in scientific knowledge. We suggest opportunities for consultation-liaison psychiatry to improve the understanding of the relationship between coronavirus and psychiatric care.
Key words: psychiatry, COVID-19, anxiety, telepsychiatry, mental health, patients
Introduction
On March 11, 2020, the World Health Organization recognized a new coronavirus (severe acute respiratory syndrome coronavirus 2 [SARS-CoV-2]) infection as the source of a global pandemic.1 Although a large emphasis has rightfully been placed on the high transmissibility and lethality of this disease, the pandemic has also wrought psychiatric sequelae and rapid change to the delivery of mental health care.1 , 2 Consultation-liaison (c-l) psychiatrists' experience managing psychiatric presentations in medical settings positions them to play an invaluable role for patient care and systems leadership during the pandemic. C-l psychiatrists are familiar with the complexities of psychiatric diagnosis among medically ill patients and delivery of behavioral health treatment within medical settings. This expertise can aid in the identification, study, and treatment of the psychiatric consequences of SARS-CoV-2 and its disease, COVID-19.
What is currently known about the coronavirus' impact on psychiatric care? Popular media have spoken about anxiety, stress, grief, and depression associated with coronavirus, COVID-19, and the public health response to the pandemic. This review aims to provide a critical synthesis of the scientific literature on coronavirus since its emergence and its relationship to psychiatric practice. We hypothesized that evidence would describe negative impacts of SARS-CoV-2 by directly causing psychiatric symptoms, exacerbating extant mental illness, and complicating the delivery of psychiatric care.
Methods
We identified literature describing the psychiatric implications of coronavirus and COVID-19. Our approach was consistent with a rapid review of a quickly evolving topic.3 A rapid review is “a type of knowledge synthesis in which components of the systematic review process are simplified or omitted to produce information in a short period of time.”4 The search terms and strategy using a single database, PubMed, are described in Table 1 . PubMed was chosen for its high scientific standard and global reach. Inclusion criteria were publications in English from December 2019 to April 13, 2020. Articles were screened for content by the authors independently and then included in the review by consensus. Articles were excluded if they did not address psychiatric care or symptoms. References from included articles were reviewed to identify additional literature. The quality of original quantitative research was assessed using the Quality Assessment Tool.5 The heterogeneous nature of these studies precluded a meta-analytic approach.
Table 1.
Search Scheme Used to Identify Relevant Citations.
| Search terms in PubMed from December 2019 to April 13, 2020 | ||
|---|---|---|
| First search term [all fields] | Second search term [all fields] | |
| [COVID-19] | + any combination | [psychiatry] |
| [COVID] | [psych] | |
| [coronavirus] | [psychology] | |
| [SARS-CoV-2] | [mental health] | |
| [2019-nCoV] | [behavioral health] | |
Results
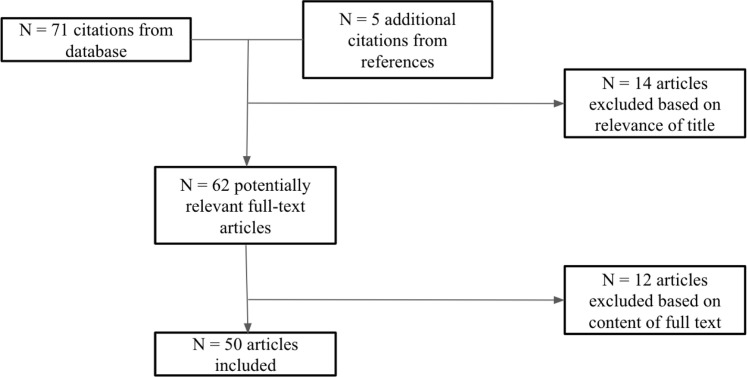
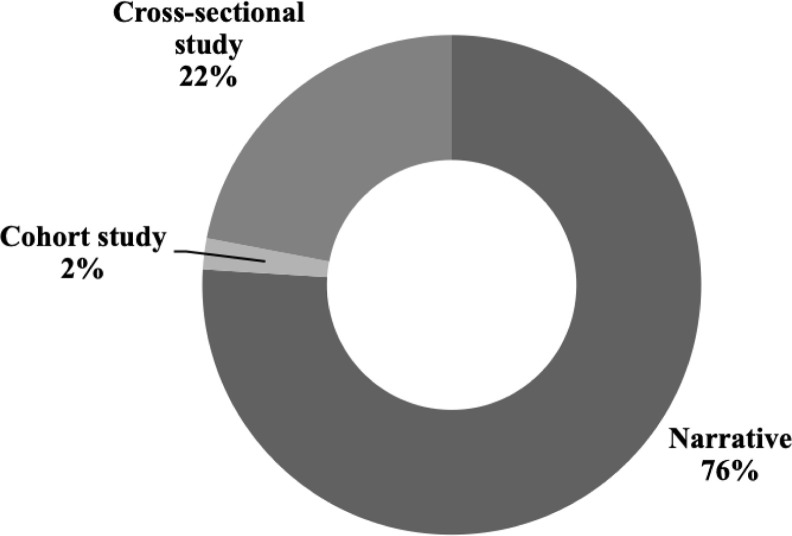
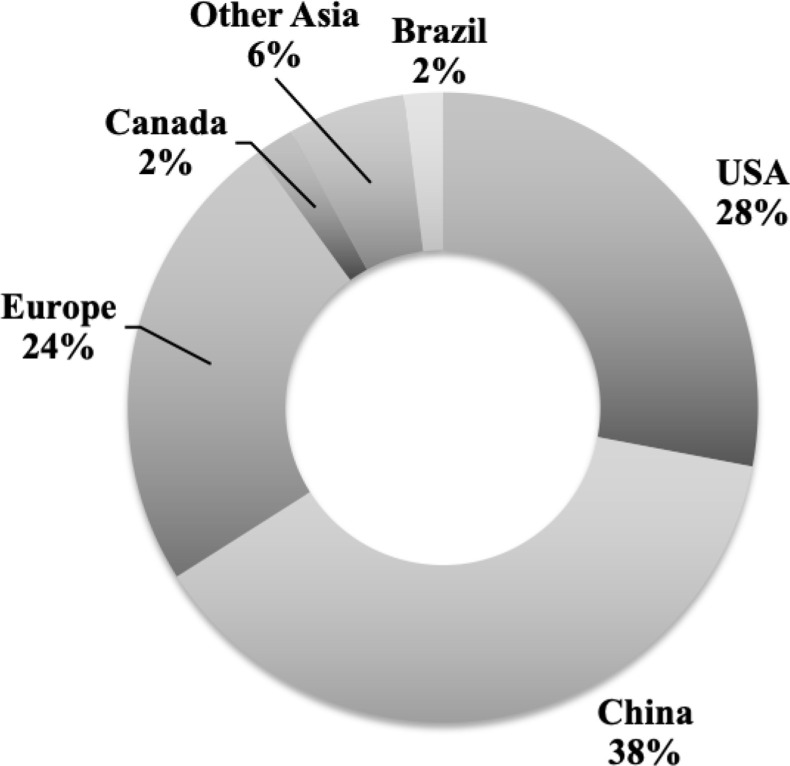
Seventy-one articles were identified in an initial search, from which fifty full-text articles were included. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram for article selection is shown in Figure 1 .6 Most articles (38/50, 76%) were narrative reports without original data (Figure 2 ). A quality assessment on articles with original data is shown in Table 2 . All but one (11 of 12) of these articles were rated as of weak quality. Articles were found from 9 countries, mostly from China (19/50, 38%) and the United States (US; 14/50, 28%) (Figure 3 ).
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Diagram for Literature Search.
Figure 2.
Publications by Study Type (n = 50).
Table 2.
Findings and Quality Assessment of Studies Reporting Original Quantitative Data
| Source | Methodology and population | Main findings | Quality assessment5 |
|---|---|---|---|
| Bo et al.7 | Cross-sectional survey of 714 Chinese COVID-19 survivors before discharge from a quarantine facility |
|
Weak |
| Cao et al.8 | Cross-sectional survey of 7143 Changzhai medical students in China |
|
Weak |
| Castro and Perlis9 | Electronic medical records review of 2,689,116 patient encounters in Massachusetts, United States |
|
Strong |
| Chung and Yeung10 | Cross-sectional survey of 69 full-time staff in Hong Kong, China |
|
Weak |
| American Psychiatric Association11 | Cross-sectional survey of 1004 residents in the United States |
|
Weak |
| Lai et al.12 | Cross-sectional survey of 1257 health care workers in Hubei, in Wuhan, outside of Wuhan, China |
|
Weak |
| Liu et al.13 | Cross-sectional survey of 285 residents and visitors in Wuhan, China |
|
Weak |
| Lu et al.14 | Cross-sectional survey of medical and administrative staff in Fujian, China |
|
Weak |
| Qiu et al.15 | Cross-sectional survey of 52,730 residents in China |
|
Weak |
| Wang et al.16 | Cross-sectional survey of 1210 members of the general public in China |
|
Weak |
| Zhang et al.17 | Cross-sectional survey of 2182 medical and nonmedical workers in Wuhan, China |
|
Weak |
| Zhu et al.18 | Cross-sectional survey of 5062 health care workers in Wuhan, China |
|
Weak |
Figure 3.
Publications by Country of Origin (n = 50).
There were two major categories of literature. Thirty-five articles described risks of psychiatric symptoms in the context of the pandemic. The second category comprised 15 articles describing changes in psychiatric practice consequent of the pandemic.
Psychiatric Risks of the Pandemic
Population-based surveys in China have demonstrated increases in distress and posttraumatic stress, anxiety, and depression symptoms over the course of the pandemic.8 , 16 In addition, posttraumatic stress symptoms were prevalent in 7% of Wuhan residents and visitors to Wuhan during the initial outbreak; these rates were higher than those in surrounding cities and did not correlate with a history of infection.13 A nationwide survey in China with 52,730 citizens from 36 provinces and three large cities showed 35% of respondents having mild psychological distress from the coronavirus pandemic; 5% reported more severe distress.15
These findings were consistent with data from the US. A month before the outbreak in the US, a national survey found that 40% of Americans were anxious about contracting or dying from COVID-19; psychiatric symptoms included more frequent insomnia (among 19% of respondents), alcohol consumption (8%), and interpersonal conflict (12%).11 The long-term impact of chronic stress due to the pandemic was widely feared in the literature, if yet unproven. “Pandemic adjustment disorder” has been proposed to describe the totality of these persisting symptoms.19 Editorialists have expressed concern about the potential for incident mental illness perhaps in part due to inflammatory dysregulation in the context of increased stress and decreased social connection.20 , 21 While survey studies have pointed to an increase in anxiety, one analysis of electronic medical records found decreasing mention of anxiety and depressive systems across multisite health systems compared with before the pandemic.9
These contrasting findings suggest that surveillance of coronavirus' mental health impacts may be nuanced and dependent on methodology. Survey studies have largely identified psychological symptoms without describing diagnoses or the functional status of respondents. No studies address the risks of physical distancing and contact denials. Generally, population-based studies were limited by the pandemic's short time course thus far.22
Other articles suggested psychiatric risks of coronavirus among specific at-risk populations
COVID-19 patients and survivors
Some cases of coronavirus and COVID-19 have been correlated with neurological symptoms such as anosmia, delirium, and cerebrovascular risk.23 It is thus reasonable to hypothesize that coronavirus may put patients at risk for other psychiatric syndromes. A survey among stabilized COVID-19 patients before discharge from quarantine facilities found that 96% of survivors endorsed posttraumatic stress symptoms.7 The extreme environmental modifications of hospital environments for infection control may increase the risk of delirium among at-risk patients.24 No studies, thus far, describe cognitive and functional outcomes among survivors of severe COVID-19.
Health care staff
The mental health consequences of coronavirus have been most studied among health care clinicians and administrators.1 , 25, 26, 27, 28 In a cross-sectional survey of 5062 health care workers in Wuhan, China, care providers who were female, had more than 10 years of experience, or worked with acutely ill patients (emergency, intensive care, respiratory care, and infectious disease clinicians) were at heightened risk of stress, depression, and anxiety.18 Other studies described increased rates of insomnia (up to 38%), anxiety (13%), depression (49%), somatization (2%), and obsessive-compulsive (5%) symptoms among providers.10 , 17 A survey of clinical staff found that 71% felt significant fear working with patients with coronavirus.12 Staff with direct patient care responsibilities experienced significantly higher psychological sequelae than staff who did not.14 Specific components exacerbating these responses from health care staff were suggested: concerns included fear of infecting family, limited amount of personal protective equipment and other resources, exhaustion from longer working hours, and dealing with patients who do not want to cooperate with current guidelines.29 , 30
Supportive interventions were described to ameliorate these negative effects among health care staff. One Chinese hospital provided medical staff supplementary space to rest outside of their homes, prepared meals, prejob training on how to address psychological problems in patients suffering from COVID-19, and explicit rules on the management of limited personal protective equipment.30 This intervention builds on factors described as protective against psychological stress, feelings of preparedness, and institutional support but was not rigorously evaluated for effectiveness.29
Health care staff are an important population facing unique stressors during the pandemic. Medical care providers are also a readily accessible population for study. Nevertheless, the generalizability of these findings and interventions is of limited utility for understanding psychological responses to the pandemic among the general population. These symptoms are more strongly related to perception of the coronavirus and its public health responses than to biological injury from SARS-CoV-2.
Persons with mental illness
Anecdotally, persons who have preexisting mental health conditions may be at risk for worse outcomes as a result of the pandemic. These risks derive from barriers in accessing timely health services and being more emotionally susceptible to stressors.31 These patients' limited access to care may result in relapse of disease.32 Access to care may be particularly problematic for individuals in substance treatment programs, such as those on medication-assisted treatments that cannot be delivered remotely.33 Psychiatrists have been asked to proactively engage patients who might not seek care out of fear of infection.21 No evidence described specific risks by psychiatric diagnosis or provided data supporting specific interventions for maintaining care quality and access for this population.
Elderly persons
Elderly persons were postulated to be among the groups at highest risk for mental health sequelae of coronavirus.34 This population was predicted to not only suffer from a greater physical risk due to coronavirus but also be more susceptible to the negative psychological impacts of social isolation.21 , 34 An increased incidence of death by suicide was observed among elder persons during the 2003 SARS epidemic; elder persons may be at similar risk yet again.34 A narrative report from China portrayed elders as disproportionately struggling with technological utilization and decreased access to public transportation.35 Patients with dementia who struggle to follow infection control guidelines could increase the risk of burnout among nursing facility staff while also increasing patients' risk of COVID-19.36 Interventions to mitigate potential psychiatric effects among the elderly population were not described.34
Other populations
Less literature described psychiatric risks of coronavirus among other populations. Correctional facilities reported difficulty maintaining social distance regulations among inmates and promoting adequate hygiene.37 Students, adolescents, and children experienced disruptions to daily routines and academic schedules.38 International Chinese college students reported experiencing discrimination given the coronavirus' origins and anxiety related to family members contracting this disease in their home country.39 Patients involved in research studies were suggested to be negatively impacted by unexpected study discontinuations or protocol changes.40
Changes to Psychiatric Practice
A second category of studies describes the pandemic's impact on the delivery of psychiatric care. Psychiatrists have been asked to adopt several roles in response to the pandemic. Psychiatrists have skills in general practice and may be required to refresh their medical knowledge to support their patients, collaborate with primary providers, and direct patients to appropriate treatment.19 , 41 C-l psychiatrists are accustomed to this role and can support efforts to integrate treatment by providing training to the staff and sharing relevant operational processes. Mental health professionals are positioned to support resilience among medical providers and volunteer for crisis support hotlines. Psychiatrists' contributions have been compared to fighting a war against the pandemic, with psychiatrists' role being to not only direct clinical care but also to engage in research on the pandemic's effects.42
Public health interventions have altered the standard of care in both hospital and outpatient settings. Psychiatric hospitals have accommodated enhanced infection control by reducing patient visitors and shortening inpatient stays.43 , 44 Published protocols provide specific guidance to enhance infection control in inpatient behavioral health units.45 No outcome data support the efficacy of these interventions or describe potential adverse impacts for delivering psychiatric care in this manner.
The rapid and widespread adoption of telepsychiatry has been the most appreciable change in psychiatric practice during the pandemic, a change predicted to have lasting implications on the accessibility and quality of mental health care after the pandemic.44 , 46 , 47 Telepsychiatry is being used not only between physicians and patients but also between c-l psychiatrists and primary teams.48 A physician in France detailed the quick implementation of telepsychiatry in her hospital, which was necessary to accommodate increased patient volumes 10 days after social isolation orders were implemented.49
Limitations of telepsychiatry have also been described. For example, electroconvulsive therapy is a life-saving procedure that cannot be performed remotely and places practitioners at high risk of contracting coronavirus.50 Some opioid-assisted therapies, particularly with methadone, require in-person treatment, and patients who cannot remain in treatment are at risk of relapse.33 In addition, telepsychiatry may not be accessible for all patients, including those who are homeless, severely cognitively impaired, technologically uncomfortable (e.g., the elderly), or young children.19 , 46 There were no descriptions of adapting telepsychiatry to these at-risk populations. While the adaptation of telepsychiatry for c-l psychiatry was noted, impacts on clinical outcomes were not studied. The expansion of telepsychiatry has not been accompanied by rigorous evaluations of quality or outcomes for patients who have been unexpectedly transitioned to this modality.
The coronavirus pandemic has implications for psychiatric prescribing. Several psychiatric drugs impact the efficacy and tolerability of antiviral therapy through P450 metabolism interactions; agents with fewer drug-drug interactions should be used preferentially (e.g., citalopram, olanzapine, or valproic acid).51 New guidelines have been published for assessing clozapine patients who presented with flu-like illness or suspected COVID-19 given those patients' risk for neutropenia.52 It is unknown whether coronavirus itself may impact the efficacy or tolerability of psychiatric medications.
These systemic changes emphasize the advantages of building adaptable health care delivery models and strong community support for mental health service before a crisis.53 , 54 C-l psychiatrists' training positions them to advocate at individual, institutional, and systems levels for integrating psychiatric surveillance and care into health systems. The global nature of the pandemic has prompted international collaboration and opportunities for such advocacy to happen on an international scale.55
Discussion
While much literature is being produced on coronavirus, even at this early stage, most articles are editorials and narrative descriptions devoid of original research. The long-term sequelae of coronavirus on psychiatric symptoms remain uncertain, and the data reported so far on the impact of coronavirus on psychiatric care are of generally poor quality. C-l psychiatry can play an invaluable role in expanding our understanding of coronavirus' implications for psychiatric care and addressing gaps in the scientific literature.
The psychiatric consequences of coronavirus and COVID-19 are unclear. Concerns have arisen as to the risk of posttraumatic stress, cognitive impairment, and suicide risk among survivors, but whether these risks are conferred by SARS-CoV-2 or concurrent medical illness and psychosocial stressors are uncertain. Similarly, coronavirus' impact on the course of psychiatric illness remains unstudied. Persons with mental illness may be at a heightened risk of both infection and psychiatric relapse due to inaccessibility of mental health care. Given their work in medical environments, c-l psychiatrists are positioned to study the psychiatric symptoms of COVID-19 and complications of the disease among at-risk populations.
The initial pandemic has induced widespread psychological unease, but no epidemiological studies applied diagnostic or functional impairment criteria to populations of interest. Mental health sequelae observed at a population level are confounded by concurrent changes in psychiatric care delivery, economic stressors, and public health interventions. Indeed, the ubiquity of distress calls into question whether an individualized psychiatric treatment approach is preferable to broader public health and political initiatives. Psychiatrists should not only seek to better understand the psychiatric consequences of the pandemic but also interpret and apply those findings in developing population-level interventions. Examples of such interventions may be how to best triage persons with nonspecific psychological anxiety related to the pandemic or how to maintain access to psychiatric services for vulnerable populations.
Adaptations in psychiatric care delivery have been frequently described, yet the implications of these changes have been incompletely considered. Telepsychiatry has been extended for use among patients who never intended to use this modality; whether this modality is in fact improving access or maintaining care quality awaits confirmation. The utility of telepsychiatry for high-risk, complex, or highly impairing psychiatric presentations in medical settings is similarly undescribed. C-l psychiatrists will need to innovate telepsychiatry and remote care models for these patients. Measuring and reporting outcomes related to quality and access to care would represent an important contribution, as these data are lacking in the literature to date.56 If specialized mental health services prove inaccessible, psychiatrists should consider how patients may be identified and best treated through extant medical systems.
The studies identified were of generally poor quality because of selective sampling and a high risk of bias. Knowing these weaknesses, c-l psychiatrists should be mindful that studies of coronavirus and COVID-19 among hospitalized patients represent a select subgroup of medically ill patients who may differ from a larger population of mildly symptomatic patients with coronavirus infection. The impact of coronavirus on immediate family members and survivors is an area of concern that requires attention. C-l psychiatrists have access to these populations through work in integrated care settings (where milder COVID-19 presentations are treated) or with families of hospitalized patients.
There are several limitations to this review. While the search was limited to English-language peer-reviewed scientific literature, many of these novel findings are yet to be fully vetted by the medical community. Long-term sequelae of coronavirus on psychiatric symptoms have not yet had an opportunity to emerge. This rapid review was limited to one medical database which limits access to articles published ahead of print or in the gray literature.
Conclusion
As COVID-19 and its related public health responses transform life around the globe, the psychiatric sequelae of the pandemic among individuals and societies are uncertain. At this early stage of the pandemic, original research remains scarce and of poor quality. High levels of distress and potentially revolutionary changes in psychiatric practice are being described, but there is a poor understanding of the pandemic’s impact on the incidence, prevalence, and prognosis of psychiatric disease and implications for access to and quality of care. Coronavirus’ potential psychiatric symptoms have not been described, although there is a reason to suspect the virus may cause direct neuronal injury. Several small interventions on reducing psychological symptoms among at-risk populations suggest the potential for psychiatry to adopt an assertive and positive response equal to a monumental task.
Footnotes
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosures: S.A.S. reports receiving royalties from Taylor & Francis. No other authors report disclosures.
References
- 1.Arden M.A., Chilcot J. Health psychology and the coronavirus (COVID-19) global pandemic: a call for research. Br J Health Psychol. 2020;25:231–232. doi: 10.1111/bjhp.12414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Torales J., O'Higgins M., Castaldelli-Maia J.M. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. 2020;66:317–320. doi: 10.1177/0020764020915212. [DOI] [PubMed] [Google Scholar]
- 3.Tricco A.C., Antony J., Zarin W. A scoping review of rapid review methods. BMC Med. 2015;13:224. doi: 10.1186/s12916-015-0465-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arksey H., O'Malley L. Scoping studies: towards a methodological framework. Int J Social Res Methodol. 2005;8:19–32. [Google Scholar]
- 5.Armijo-Olivo S., Stiles C.R., Hagen N.A. Assessment of study quality for systematic reviews: a comparison of the Cochrane collaboration risk of Bias Tool and the effective public health practice Project quality assessment Tool: methodological research. J Eval Clin Pract. 2012;18:12–18. doi: 10.1111/j.1365-2753.2010.01516.x. [DOI] [PubMed] [Google Scholar]
- 6.Moher D., Liberati A., Tetzlaff J. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62:1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 7.Bo H.X., Li W., Yang Y. Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID-19 in China. Psychol Med. 2020:1–7. doi: 10.1017/S0033291720000999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cao W., Fang Z., Hou G. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287:112934. doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Castro V.M., Perlis R.H. Impact of COVID-19 on psychiatric assessment in emergency and outpatient settings measured using electronic health records. medRxiv. 2020 doi: 10.1101/2020.03.30.20048207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chung J.P.Y., Yeung W.S. Staff mental health Self-assessment during the COVID-19 outbreak. East Asian Arch Psychiatry. 2020;30:34. doi: 10.12809/eaap2014. [DOI] [PubMed] [Google Scholar]
- 11.New Poll: COVID-19 impacting mental Well-being: Americans feeling anxious, Especially for Loved ones; older adults are less anxious. 2020. https://www.psychiatry.org/newsroom/news-releases/new-poll-covid-19-impacting-mental-well-being-americans-feeling-anxious-especially-for-loved-ones-older-adults-are-less-anxious Available from:
- 12.Lai J., Ma S., Wang Y. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3:e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu N., Zhang F., Wei C. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: gender differences matter. Psychiatry Res. 2020;287:112921. doi: 10.1016/j.psychres.2020.112921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lu W., Wang H., Lin Y. Psychological status of medical workforce during the COVID-19 pandemic: a cross-sectional study. Psychiatry Res. 2020;288:112936. doi: 10.1016/j.psychres.2020.112936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Qiu J., Shen B., Zhao M. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr. 2020;33:e100213. doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang C., Pan R., Wan X. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17 doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang W.R., Wang K., Yin L. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom. 2020:1–9. doi: 10.1159/000507639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhu Z., Xu S., Wang H. COVID-19 in Wuhan: immediate psychological impact on 5062 health workers. medRxiv. 2020 doi: 10.1101/2020.02.20.20025338. [DOI] [Google Scholar]
- 19.Goldberg J.F. Psychiatry's Niche role in the COVID-19 pandemic. J Clin Psychiatry. 2020;81 doi: 10.4088/JCP.20com13363. [DOI] [PubMed] [Google Scholar]
- 20.Ornell F., Schuch J.B., Sordi A.O. "Pandemic fear" and COVID-19: mental health burden and strategies. Braz J Psychiatry. 2020;42:232–235. doi: 10.1590/1516-4446-2020-0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Solomon H.V. COVID-19 checklist: mask, gloves, and video chatting with grandpa. Psychiatry Res. 2020;288:112986. doi: 10.1016/j.psychres.2020.112986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Specter M. The denialists: the dangerous attacks on the consensus about H.I.V. and AIDS. New Yorker. 2007;1925:32–38. [PubMed] [Google Scholar]
- 23.Russell B., Moss C., Rigg A. Anosmia and ageusia are emerging as symptoms in patients with COVID-19: what does the current evidence say? Ecancermedicalscience. 2020;14:ed98. doi: 10.3332/ecancer.2020.ed98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.LaHue S.C., James T.C., Newman J.C. Collaborative delirium prevention in the Age of COVID-19. J Am Geriatr Soc. 2020;68:947–949. doi: 10.1111/jgs.16480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fiorillo A., Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur Psychiatry. 2020:1–4. doi: 10.1192/j.eurpsy.2020.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cullen W., Gulati G., Kelly B.D. Mental health in the Covid-19 pandemic. QJM. 2020;113:311–312. doi: 10.1093/qjmed/hcaa110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ho C.S., Chee C.Y., Ho R.C. Mental health strategies to Combat the psychological impact of COVID-19 beyond Paranoia and panic. Ann Acad Med Singapore. 2020;49:1–3. [PubMed] [Google Scholar]
- 28.Kaufman K.R., Petkova E., Bhui K.S. A global needs assessment in times of a global crisis: world psychiatry response to the COVID-19 pandemic. BJPsych Open. 2020:1–11. doi: 10.1192/bjo.2020.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gavin B., Hayden J., Adamis D. Caring for the psychological Well-being of healthcare professionals in the Covid-19 pandemic crisis. Ir Med J. 2020;113:51. [PubMed] [Google Scholar]
- 30.Chen Q., Liang M., Li Y. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:e15–e16. doi: 10.1016/S2215-0366(20)30078-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yao H., Chen J.H., Xu Y.F. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry. 2020;7:e21. doi: 10.1016/S2215-0366(20)30090-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Asmundson G.J.G., Taylor S. How health anxiety influences responses to viral outbreaks like COVID-19: what all decision-makers, health authorities, and health care professionals need to know. J Anxiety Disord. 2020;71:102211. doi: 10.1016/j.janxdis.2020.102211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sun Y., Bao Y., Kosten T. Editorial: challenges to opioid use disorders during COVID-19. The Am J Addict. 2020;29:174–175. doi: 10.1111/ajad.13031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vahia I.V., Blazer D.G., Smith G.S. COVID-19, mental health and aging: a need for new knowledge to Bridge science and service. Am J Geriatr Psychiatry. 2020;28:695–697. doi: 10.1016/j.jagp.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yang Y., Li W., Zhang Q. Mental health services for older adults in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:e19. doi: 10.1016/S2215-0366(20)30079-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang H., Li T., Barbarino P. Dementia care during COVID-19. Lancet. 2020;395:1190–1191. doi: 10.1016/S0140-6736(20)30755-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wurcel A.G., Dauria E., Zaller N. Spotlight on Jails: COVID-19 mitigation policies needed Now. Clin Infect Dis. 2020:ciaa346. doi: 10.1093/cid/ciaa346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sani G., Janiri D., Di Nicola M. Mental health during and after the COVID-19 emergency in Italy. Psychiatry Clin Neurosci. 2020;74:372. doi: 10.1111/pcn.13004. [DOI] [PubMed] [Google Scholar]
- 39.Zhai Y., Du X. Mental health care for international Chinese students affected by the COVID-19 outbreak. Lancet Psychiatry. 2020;7:e22. doi: 10.1016/S2215-0366(20)30089-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Padala P.R., Jendro A.M., Padala K.P. Conducting clinical research during the COVID-19 pandemic: investigator and Participant perspectives. JMIR Public Health Surveill. 2020;6:e18887. doi: 10.2196/18887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Banerjee D. The COVID-19 outbreak: Crucial role the psychiatrists can play. Asian J Psychiatr. 2020;50:102014. doi: 10.1016/j.ajp.2020.102014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nicol G.E., Karp J.F., Reiersen A.M. "What were You before the war?" Repurposing psychiatry during the COVID-19 pandemic. J Clin Psychiatry. 2020;81 doi: 10.4088/JCP.20com13373. [DOI] [PubMed] [Google Scholar]
- 43.Xiang Y.T., Zhao Y.J., Liu Z.H. The COVID-19 outbreak and psychiatric hospitals in China: managing challenges through mental health service reform. Int J Biol Sci. 2020;16:1741–1744. doi: 10.7150/ijbs.45072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Li W., Yang Y., Liu Z.H. Progression of mental health services during the COVID-19 outbreak in China. Int J Biol Sci. 2020;16:1732–1738. doi: 10.7150/ijbs.45120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Starace F., Ferrara M. COVID-19 disease emergency operational Instructions for mental health Departments issued by the Italian society of epidemiological psychiatry. Epidemiol Psychiatr Sci. 2020:1–12. doi: 10.1017/S2045796020000372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Torous J., Jan Myrick K., Rauseo-Ricupero N. Digital mental health and COVID-19: using Technology Today to Accelerate the Curve on access and quality Tomorrow. JMIR Ment Health. 2020;7:e18848. doi: 10.2196/18848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wright J.H., Caudill R. Remote treatment delivery in response to the COVID-19 pandemic. Psychother Psychosom. 2020:1–3. doi: 10.1159/000507376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shalev D., Shapiro P.A. Epidemic psychiatry: the opportunities and challenges of COVID-19. Gen Hosp Psychiatry. 2020;64:68–71. doi: 10.1016/j.genhosppsych.2020.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Corruble E. A viewpoint from Paris on the COVID-19 pandemic: a necessary turn to telepsychiatry. J Clin Psychiatry. 2020;81 doi: 10.4088/JCP.20com13361. [DOI] [PubMed] [Google Scholar]
- 50.Colbert S.A., McCarron S., Ryan G. Images in clinical ECT: immediate impact of COVID-19 on ECT practice. J ECT. 2020 doi: 10.1097/YCT.0000000000000688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhang K., Zhou X., Liu H. Treatment concerns for psychiatric symptoms in COVID-19-infected patients with or without psychiatric disorders. Br J Psychiatry. 2020:1–3. doi: 10.1192/bjp.2020.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Siskind D., Honer W.G., Clark S. Consensus statement on the use of clozapine during the COVID-19 pandemic. J Psychiatry Neurosci. 2020;45:200061. doi: 10.1503/jpn.200061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zhang J., Wu W., Zhao X. Recommended psychological crisis intervention response to the 2019 novel coronavirus pneumonia outbreak in China: a model of West China Hospital. Precision Clin Med. 2020;00:1–6. doi: 10.1093/pcmedi/pbaa006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Duan L., Zhu G. Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiatry. 2020;7:300–302. doi: 10.1016/S2215-0366(20)30073-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ahmad A., Mueller C., Tsamakis K. Covid-19 pandemic: a public and global mental health opportunity for social transformation? BMJ. 2020;369:m1383. doi: 10.1136/bmj.m1383. [DOI] [PubMed] [Google Scholar]
- 56.Goldberg R.J., Burock J., Harrington C.J. Quality Indicators in consultation–liaison psychiatry. Psychosomatics. 2009;50:550. doi: 10.1176/appi.psy.50.5.550. [DOI] [PubMed] [Google Scholar]