Abstract
Background
Relationship status is an important factor associated with condomless anal intercourse (CAI) amongst men who have sex with men (MSM).
Methods
A multi-centre bio-behavioural survey with MSM was conducted in 13 European cities (n = 4901) exploring factors associated with CAI via bivariate and multivariate multilevel logistic regression analyses.
Results
Likelihood of CAI with casual partners was associated with being ‘out’ to a majority (AOR = 1.19;95% CI 1,1.42); knowing their HIV status (AOR = 1.86; 95% CI 1.25,2.76); using substances (1–2 AOR = 1.39; 95% CI 1.16,1.63, 2+ AOR = 1.81; 95% CI 1.35,2.42); being older (AOR = 0.98; 95% CI 0.97,0.99); successful sero-communication (AOR = 0.79; 95% CI 0.67,0.94); and, not having a recent HIV test (AOR = 0.78; 95% CI 0.66,0.92). CAI with steady partners was associated with successful sero-communication (AOR = 2.72; 95% CI 2.72,3.66); not having a recent HIV test (AOR = 1.26; 95% CI 1.09,1.46), and; being older (AOR = 0.99; 95% CI 0.98,0.99).
Conclusions
Understandings of partner type and/or relationship status in relation to CAI amongst MSM can potentially play an important role in the development of culturally appropriate HIV/STI prevention and risk-reduction efforts targeting at-risk MSM. Our results speak to the need to consider segmented and tailored public health and health promotion initiatives for MSM with differing CAI behaviours and relationship profiles.
Keywords: HIV, MSM, relationships, respondent-driven sampling, time-location sampling
Introduction
Epidemiological evidence suggests that sex between men continues to be the main mode of HIV transmission accounting for 40% of all new diagnoses in 2016 across the European Union (EU) and the European Economic Area (EEA).1 However, although there is now evidence of decreasing diagnoses amongst men who have sex with men (MSM) in some countries including Austria, Belgium, Italy, the Netherlands, Spain, and the United Kingdom,2 in other EU/EEA countries diagnoses have increased substantially.1 Such distinct trends mean that it is essential to sustain and, in some cases, strengthen HIV prevention interventions tailored to the local epidemiological context and targeting population groups most at risk; for many countries this means MSM.
In order to develop and implement community-level risk-reduction initiatives targeting MSM, it is necessary to examine not only key sexual behaviours amongst different MSM (sub) populations, but to also understand and consider the context in which they occur; relationships are one such context. Indeed, research demonstrates that relationship status and/or partnership type is an important factor associated with condomless anal intercourse (CAI) and subsequent risk for HIV and sexually transmitted infections (STIs).3–7
However, the risk for HIV and other STI acquisition is dependent on other factors than just CAI. Kramer and colleagues have drawn attention to this issue and note that although prevention initiatives commonly target individualistic-behaviours thus regarding CAI as an inherently ‘risky’ sexual behaviour, such approaches can be unhelpful as they may mask more complex and dynamic issues occurring within MSM in both steady and casual or non-steady relationships including the use of risk-reduction strategies.8–10 For instance the number of partners as well as knowledge of own and partner’s HIV serostatus, the use of ‘negotiated safety’ agreements,11 serosorting, and the effective use of anti-retroviral drugs to lower viral load as well as the use of pre-exposure prophylaxis (PreP)12,13 may be contingent on the perception of the type of relations.
Nevertheless, examining explanatory factors related to differences in CAI between MSM in steady and casual relationships can be important in order to interrogate segmented public health and health promotion initiatives for MSM with differing sexual behaviour and relationship profiles. Consequently, in this present analysis we utilize data from the EU-funded Sialon II study which was a large multi-centre biological and behavioural cross-sectional survey of MSM in community settings carried out across 13 European cities. The objectives of our analysis were to: (i) investigate CAI and explanatory variables amongst MSM in a large community sample; (ii) explore the differences in CAI between those participants who had steady partners with those who had casual or non-steady partners, and finally; (iii) potentially inform the development (and assist implementation) of risk-reduction initiatives targeting MSM.
Methods
Study design
Detailed study methods are reported elsewhere.14–16 In summary, the Sialon II study was a complex multi-centre integrated bio-behavioural cross-sectional survey with a concomitant collection of behavioural data and biological data (oral fluid or blood specimens).
Setting
The survey was implemented in 13 European cities. The decision to use Time-Location Sampling (TLS) or Respondent Driven Sampling (RDS) to recruit participants was based on preliminary formative research. TLS (also known as Venue Day Time Sampling, Temporal Spatial Sampling, and Time Venue Sampling) was used to recruit participants in Brussels, Sofia, Hamburg, Warsaw, Lisbon, Ljubljana, Barcelona, Stockholm, and Brighton (n = 3596). TLS is a quasi-probabilistic method used to recruit members of a target population at specific times in set venues.17 In this study, the venues or settings for data collection included social and/or commercial venues and cruising settings preliminarily identified through formative research and which were then selected randomly for data collection sampling calendars.18 RDS was used in Bratislava, Bucharest, Verona, and Vilnius (n = 1305). RDS is similar to snowball sampling in that it requires the target population to be socially networked so participants can invite their peers to participate. However, RDS is different in that it incorporates numerous theoretical assumptions to reduce the numerous biases found in standard snowball sampling methods (see19). Enrolment for RDS in Sialon II was based on the individuals’ social network and for the data collection, locally accredited healthcare facilities (e.g. a hospital) were used. In TLS cities, participants were recruited during 2013, whilst in RDS cities recruitment started in 2013 and finished in 2014. Prior to the survey we estimated a 50% response rate as part of the sample size calculations. A data collection procedure to record refusals was therefore developed for TLS only. However, not all sites collected this data (with exception of the Brighton site with a 59% response rate). Thus an overall response and/or refusal rate for the TLS survey is not reported.
Participants
Participants were men present in the cities at the moment of data collection (2013–14) who met the inclusion criteria (18 years or older; had sex with another man during the previous 12 months, and; agreed to donate an oral fluid or blood specimen depending on the sampling approach adopted). Exclusion criteria were being younger than the legal age of consent (18 years old) or having already participated in the study.
Instruments
A self-administered pen-and-paper questionnaire was used to collect behavioural data. The preliminary version of the questionnaire was designed by the Sialon II network in line with the Global AIDS Monitoring indicators (GAM)16,20 and previous EC-funded European projects (e.g.21,22) and then piloted amongst MSM in each study site. The English version of the questionnaire was translated into local languages and back-translated into English.
Ethics
Research protocols were submitted to, and approved by, an institutional ethical review board in each participating city, as well as by the WHO Research Project Review Panel (RP2) and the WHO Research Ethics Review Committee (ERC). All participants were given a study information sheet and the details were read out to ensure they understood what the study involved, that participation was voluntary, and that they had the right to withdraw at any time without giving a reason. Those willing to take part then signed a consent form. For TLS and RDS, a dedicated barcode system was used in order to link anonymously the different types of data collected (i.e. biological samples and behavioural data). For the TLS survey, respondents who wanted to collect their tests results could do so using their unique bar code ID. For the RDS survey where respondents were tested directly in a hospital/clinical setting, test results were available according to the local standards (including pre and post-test counselling).
Measures
Outcome variables
The primary focus of this analysis was to explore engagement in CAI measured as insertive/receptive unprotected anal intercourse in the last 6 months. Since we initially expected the ‘risk’ behaviour for those engaging in CAI in the last 6 months to differ depending on the relationship status (steady or casual partner), two separate ‘primary’ outcomes were created for two separate analyses. The first outcome indicated whether an individual had engaged in CAI with one or more (yes = 1) or zero (no = 0) steady partners. This included ‘boyfriends’ and ‘husbands’ (i.e. not being ‘single’) and excluded partners who were ‘sex buddies’. The second outcome indicated whether individuals had engaged in CAI with one or more (yes = 1) or zero (no = 0) casual partners. Casual partners were defined as: those with whom one had had sex with only once (e.g. a ‘one-night stand’); and those with whom one had sex with more than once but were not considered a steady partner (such as sex buddies). Some participants categorized current relationships as a mix of casual and steady partners since the two categorizations are not mutually exclusive.
Independent variables
Independent variables included: age (based on self-reported year of birth), education level (secondary school or lower, high school/post-secondary education/vocational school or college, or university degree/higher), migrant status (based on country of birth and country of residence: native, emigrant, immigrant or visitor), ‘outness’ (the extent to which participants reported being open about their sexual attraction towards men with others: being out to ‘less than half’ or ‘out to the majority’), overall perceived attitude towards gay or bisexual people at work/school and amongst parents/friends/acquaintances (positive, neutral or negative attitude), HIV testing in the last 12 months and results known (no or yes), knowledge of own HIV status (using both self-reported status and status based on laboratory results: newly diagnosed, negative test result, already known), sex role at last anal sex (insertive, receptive, versatile), number of substances (type specified in the questionnaire) used at last anal sex (0, 1–2, 2+), frequency of visits to gay venues during last 3 months where sex-on-premises is possible (0 ‘no’, 1–3 ‘low’ 3+ ‘high’), currently having sex with women (no or yes), serostatus communication at last anal intercourse (successful, unsuccessful; this constructed variable distinguishes between successful serostatus disclosure [i.e. a communication that establishes HIV serostatus concordance or discordance, including unilateral HIV infection disclosure], and unsuccessful serostatus disclosure [i.e. a communication where either none or only one of the involved partners disclosed his serostatus, with the exception of unilateral HIV infection disclosure]), see.23
Data analysis
Descriptive analysis
For continuous variables median and interquartile range (IQR) were used. For nominal variables count and percentages were used. The Chi-square test was used to examine the relation between CAI in casual partners and CAI in steady partners as well as to compare CAI rates between pairs of cities.
Bivariate and multivariate multilevel modelling
For all bivariate and multivariate analyses, factors associated with CAI were identified using a two-level multilevel logistic regression model with a random intercept at the city level. The random component accounts for the hierarchical nature of the data. Analyses were carried out on all available cases.
The first step to building a model was to identify those individual independent variables (from the full list above) that were statistically significantly associated with CAI using bivariate analysis. Variables from this pool of potential risk factors were then used for inclusion in the multivariate analysis. The variables were added to the null model one by one using a forward selection process choosing the most significant (P < 0.05) variable first. The likelihood ratio test was used to compare the new model with the nested model. For all statistical tests, significance was indicated by P < 0.05. The final model estimated the adjusted odds ratios (AORs) and the corresponding 95% confidence interval (95% CI) for factors associated with CAI. We then used the resulting model to explore the relationship between age and risk of engagement in CAI for each city. Analyses were first carried out for modelling CAI with casual partners and then repeated for steady partners. Stata® Version 13 was used for all analyses (College Station, TX: StataCorp LP).
Results
Of 4901 participants who completed the survey, 4340 (88.55%) had sex in the last 6 months and were included in the analysis. The median age was 32 years with an IQR of 15 years. 3624 (83.50%) had at least one casual partner, 2911 (67.07%) had at least one steady partner and 2195 (50.58%) had both. 1374 (31.66%) participants reported CAI with casual partners (median age 31 years; IQR 12 years) and 1482 (34.15%) with steady partners (median age 31 years; IQR 14 years) and 687 (15.83%) reported CAI with both types of partner (median age 30 years; IQR 13 years). Median age for the 2171 (50.02%) who did not have CAI with casual or steady partners was 33 years (IQR 16 years). There was also a significant association (P < 0.001) between participant reports of CAI with casual partners and CAI with steady partners. Those who had CAI with steady partners had 2.73 times higher odds of CAI with casual partners (odds = 0.862) compared to those who did not have CAI with steady partners (odds = 0.316).
CAI varied between cities and by relationship status (Table 1). Brussels had the lowest percentage rate of CAI with casual partners and Sofia had the highest (22.7% vs. 53.3%, respectively; P = 0.001). Barcelona saw the lowest percentage rate of CAI with steady partners (23.81%) whilst Vilnius (40.34%) had the highest (P < 0.001). Table 1 presents the main characteristics of the study population stratified by relationship status. Odds ratios from the bivariate analyses are displayed in Table 2; all statistically significant variables made up the pool of potential factors for the final model.
Table 1.
Characteristics of study participants
| Factor | Total sample | Has at least one casual partner | Percentage of total population | Has at least one steady partner | Percentage of total population | |
|---|---|---|---|---|---|---|
| Count | % | Count | % | Count | % | |
| Age | ||||||
| 18–24 | 865 | 19.9 | 321 | 37.1 | 319 | 36.9 |
| 25–34 | 1708 | 39.4 | 596 | 34.9 | 627 | 36.7 |
| 35–44 | 989 | 22.8 | 297 | 30.0 | 320 | 32.4 |
| 45–54 | 530 | 12.2 | 111 | 20.9 | 163 | 30.8 |
| 55+ | 244 | 5.6 | 48 | 19.7 | 53 | 21.7 |
| Total | 4336 | 100 | 1373 | 31.7 | 1482 | 34.2 |
| Highest education level | ||||||
| Secondary or lower | 251 | 5.9 | 69 | 27.5 | 60 | 23.9 |
| High school or post-secondary | 1599 | 37.5 | 569 | 35.6 | 550 | 34.4 |
| University or higher | 2413 | 56.6 | 712 | 29.5 | 847 | 35.1 |
| Total | 4263 | 100 | 1350 | 31.7 | 1457 | 34.2 |
| Perceived attitude towards homosexuality & bisexuality | ||||||
| Positive | 1921 | 44.7 | 596 | 31.0 | 698 | 36.3 |
| Neutral | 1655 | 38.5 | 556 | 33.6 | 577 | 34.9 |
| Negative | 725 | 16.9 | 214 | 29.5 | 196 | 27.0 |
| Total | 4301 | 100 | 1366 | 31.8 | 1471 | 34.2 |
| Outness | ||||||
| Out to less than half | 1776 | 41.6 | 558 | 31.4 | 558 | 31.4 |
| Out to majority | 2498 | 58.4 | 804 | 32.2 | 908 | 36.3 |
| Total | 4274 | 100 | 1362 | 31.9 | 1466 | 34.3 |
| HIV testing in last 12 months and test result known | ||||||
| Yes | 2335 | 57.4 | 805 | 34.5 | 803 | 34.4 |
| No | 1733 | 42.6 | 478 | 27.6 | 581 | 33.5 |
| Total | 4068 | 100 | 1283 | 31.5 | 1384 | 34.0 |
| Sex role | ||||||
| Insertive | 1379 | 36.1 | 439 | 31.8 | 479 | 34.7 |
| Receptive | 1320 | 34.6 | 487 | 36.9 | 461 | 34.9 |
| Versatile | 1119 | 29.3 | 343 | 30.7 | 426 | 38.1 |
| Total | 3818 | 100 | 1269 | 33.2 | 1366 | 35.8 |
| No. of substances used | ||||||
| No drugs | 1895 | 44.8 | 515 | 27.2 | 682 | 36.0 |
| 1–2 drugs | 1982 | 46.9 | 704 | 35.5 | 659 | 33.2 |
| > 2 drugs | 350 | 8.3 | 146 | 41.7 | 133 | 38.0 |
| Total | 4227 | 100 | 1365 | 32.3 | 1474 | 34.9 |
| HIV status/knowledge | ||||||
| Tested negative | 3716 | 91.1 | 1134 | 30.5 | 1263 | 34.0 |
| Newly diagnosed | 146 | 3.6 | 52 | 35.6 | 46 | 31.5 |
| Already known | 215 | 5.3 | 95 | 44.2 | 77 | 35.8 |
| Total | 4077 | 100 | 1281 | 31.4 | 1386 | 34.0 |
| Had sex with female partners | ||||||
| No | 3266 | 85.7 | 1050 | 32.1 | 1178 | 36.1 |
| Yes | 543 | 14.3 | 170 | 31.3 | 154 | 28.4 |
| Total | 3809 | 100 | 1220 | 32.0 | 1332 | 35.0 |
| Frequentation of sex venues | ||||||
| No (0) | 1091 | 25.9 | 344 | 31.5 | 405 | 37.1 |
| Low (1–3) | 1772 | 42.1 | 511 | 28.8 | 589 | 33.2 |
| High (3+) | 1350 | 32.0 | 495 | 36.7 | 463 | 34.3 |
| Total | 4213 | 100 | 1350 | 32.0 | 1457 | 34.6 |
| Serostatus communication | ||||||
| Unsuccessful | 2498 | 64.6 | 891 | 35.7 | 688 | 27.5 |
| Successful | 1369 | 35.4 | 413 | 30.2 | 720 | 52.6 |
| Total | 3867 | 100 | 1304 | 33.7 | 1408 | 36.4 |
| Migration Status | ||||||
| Native | 3557 | 82.2 | 1159 | 32.6 | 1201 | 33.8 |
| Emigrant | 60 | 1.4 | 26 | 43.3 | 31 | 51.7 |
| Immigrant | 492 | 11.4 | 130 | 26.4 | 156 | 31.7 |
| Visitor | 219 | 5.1 | 56 | 25.6 | 89 | 40.6 |
| Total | 4328 | 100 | 1371 | 31.7 | 1477 | 34.1 |
| City | ||||||
| Barcelona | 357 | 8.2 | 85 | 23.8 | 85 | 23.8 |
| Bratislava | 374 | 8.6 | 163 | 43.6 | 140 | 37.4 |
| Brighton | 354 | 8.2 | 97 | 27.4 | 132 | 37.3 |
| Brussels | 352 | 8.1 | 80 | 22.7 | 120 | 34.1 |
| Bucharest | 160 | 3.7 | 70 | 43.8 | 55 | 34.4 |
| Hamburg | 350 | 8.1 | 102 | 29.1 | 99 | 28.3 |
| Lisbon | 376 | 8.7 | 99 | 26.3 | 141 | 37.5 |
| Ljubljana | 346 | 8.0 | 84 | 24.3 | 134 | 38.7 |
| Sofia | 409 | 9.4 | 218 | 53.3 | 154 | 37.7 |
| Stockholm | 249 | 5.7 | 74 | 29.7 | 85 | 34.1 |
| Verona | 364 | 8.4 | 104 | 28.6 | 115 | 31.6 |
| Vilnius | 295 | 6.8 | 98 | 33.2 | 119 | 40.3 |
| Warsaw | 354 | 8.2 | 100 | 28.2 | 103 | 29.1 |
| Total | 4340 | 100 | 1374 | 31.7 | 1482 | 34.1 |
Table 2.
Results from bivariate multilevel models identifying potential risk factors for CAI with partners by relationship status
| CAI with casual partners vs no CAI with casual partners | CAI with steady partners vs no CAI with steady partners | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Independent Variables | OR | SE | z | P > z | 95% Confidence interval for Odds ratio | Chi-square | P-value | OR | SE | z | P > z | 95% Confidence interval for Odds ratio | Chi-square | P-value | |||
| Lower | Upper | Lower | Upper | ||||||||||||||
| Age | 36.29 | <0.001 | 25.33 | <0.0001 | |||||||||||||
| 0.98 | <0.01 | −6.02 | <0.001 | 0.97 | 0.99 | 0.98 | <0.01 | −5.03 | <0.001 | 0.98 | 0.99 | ||||||
| Const. | 0.92 | 0.14 | −0.57 | 0.57 | 0.68 | 1.23 | 0.89 | 0.11 | −0.98 | 0.33 | 0.70 | 1.12 | |||||
| City | Var(const) | 0.11 | 0.05 | 0.05 | 0.26 | 0.02 | 0.01 | 0.01 | 0.08 | ||||||||
| Highest Education level | 12.86 | <0.001 | 9.84 | 0.0073 | |||||||||||||
| Primary | Ref | Ref | |||||||||||||||
| High school | 1.40 | 0.22 | 2.16 | 0.031 | 1.03 | 1.90 | 1.60 | 0.25 | 2.94 | 0.003 | 1.17 | 2.18 | |||||
| University | 1.10 | 0.17 | 0.64 | 0.522 | 0.82 | 1.49 | 1.63 | 0.26 | 3.13 | 0.002 | 1.20 | 2.22 | |||||
| const | 0.38 | 0.07 | −5.36 | <0.001 | 0.27 | 0.54 | 0.33 | 0.05 | −7.10 | <0.001 | 0.24 | 0.45 | |||||
| City | Var(const) | 0.15 | 0.06 | 0.06 | 0.35 | 0.03 | 0.02 | 0.01 | 0.09 | ||||||||
| Perceived attitude towards homosexuality & bisexuality | 11.20 | 0.0037 | 25.09 | <0.001 | |||||||||||||
| Positive | Ref | Ref | |||||||||||||||
| Neutral | 0.95 | 0.07 | −0.65 | 0.513 | 0.82 | 1.10 | 0.89 | 0.06 | −1.65 | 0.099 | 0.77 | 1.02 | |||||
| Negative | 0.71 | 0.07 | −3.27 | 0.001 | 0.58 | 0.87 | 0.60 | 0.06 | −5.00 | <0.001 | 0.50 | 0.74 | |||||
| const | 0.49 | 0.06 | −5.64 | <0.001 | 0.39 | 0.63 | 0.59 | 0.04 | −7.02 | <0.001 | 0.51 | 0.68 | |||||
| City | Var(const) | 0.17 | 0.07 | 0.07 | 0.39 | 0.04 | 0.02 | 0.02 | 0.12 | ||||||||
| Outness | 15.85 | 0.0001 | 16.70 | <0.001 | |||||||||||||
| Out to less than half | Ref | Ref | |||||||||||||||
| Out to majority | 1.34 | 0.10 | 3.98 | <0.001 | 1.16 | 1.55 | 1.33 | 0.09 | 4.09 | <0.001 | 1.16 | 1.53 | |||||
| const | 0.39 | 0.05 | −7.25 | <0.001 | 0.30 | 0.50 | 0.44 | 0.03 | −10.51 | <0.001 | 0.38 | 0.51 | |||||
| City | Var(const) | 0.18 | 0.08 | 0.08 | 0.42 | 0.04 | 0.02 | 0.02 | 0.12 | ||||||||
| HIV testing in last 12 months and result known | 19.80 | <0.001 | 0.45 | 0. 5044 | |||||||||||||
| Yes | Ref | Ref | |||||||||||||||
| No | 0.73 | 0.05 | −4.45 | <0.001 | 0.63 | 0.84 | 0.96 | 0.07 | −0.67 | 0.504 | 0.84 | 1.09 | |||||
| const | 0.52 | 0.06 | −5.40 | <0.001 | 0.41 | 0.66 | 0.52 | 0.03 | −9.76 | <0.001 | 0.46 | 0.60 | |||||
| City | Var(const) | 0.16 | 0.07 | 0.07 | 0.38 | 0.03 | 0.02 | 0.01 | 0.10 | ||||||||
| Sex role | 6.98 | 0.0305 | 4.20 | 0.1222 | |||||||||||||
| Insertive | Ref | Ref | |||||||||||||||
| Receptive | 1.19 | 0.10 | 2.08 | 0.037 | 1.01 | 1.40 | 1.00 | 0.08 | −0.04 | 0.968 | 0.85 | 1.17 | |||||
| Versatile | 0.96 | 0.09 | −0.46 | 0.647 | 0.81 | 1.14 | 1.16 | 0.10 | 1.79 | 0.073 | 0.99 | 1.37 | |||||
| const | 0.47 | 0.05 | −6.53 | <0.001 | 0.37 | 0.59 | 0.53 | 0.04 | −7.96 | <0.001 | 0.46 | 0.62 | |||||
| City | Var(const) | 0.13 | 0.06 | 0.05 | ß0.31 | 0.04 | 0.02 | 0.01 | 0.11 | ||||||||
| Substances used | 56.72 | <0.001 | 5.79 | 0.0552 | |||||||||||||
| None | Ref | Ref | |||||||||||||||
| 1–2 | 1.48 | 0.11 | 5.40 | <0.001 | 1.28 | 1.70 | 0.87 | 0.06 | −1.97 | 0.049 | 0.76 | 1.00 | |||||
| >2 | 2.35 | 0.30 | 6.76 | <0.001 | 1.84 | 3.02 | 1.10 | 0.14 | 0.75 | 0.456 | 0.86 | 1.40 | |||||
| const | 0.36 | 0.04 | −8.34 | <0.001 | 0.28 | 0.46 | 0.56 | 0.04 | −8.23 | <0.001 | 0.49 | 0.65 | |||||
| City | Var(const) | 0.16 | 0.07 | 0.07 | 0.36 | 0.03 | 0.02 | 0.01 | 0.10 | ||||||||
| HIV status knowledge | 31.32 | <0.001 | 0.5931 | 0.5931 | |||||||||||||
| Tested negative | Ref | Ref | |||||||||||||||
| Newly diagnosed | 1.33 | 0.24 | 1.56 | 0.119 | 0.93 | 1.89 | 0.91 | 0.17 | −0.51 | 0.609 | 0.64 | 1.30 | |||||
| Already known | 2.21 | 0.32 | 5.46 | <0.001 | 1.67 | 2.95 | 1.14 | 0.17 | 0.86 | 0.391 | 0.85 | 1.52 | |||||
| const | 0.43 | 0.05 | −7.56 | <0.001 | 0.34 | 0.53 | 0.51 | 0.03 | −11.2 | <0.001 | 0.46 | 0.58 | |||||
| City | Var(const) | 0.15 | 0.06 | 0.06 | 0.34 | 0.03 | 0.02 | 0.01 | 0.09 | ||||||||
| Had sex with female | 2.63 | 0.1047 | 13.22 | 0.0003 | |||||||||||||
| No | Ref | Ref | |||||||||||||||
| Yes | 0.84 | 0.09 | −1.62 | 0.105 | 0.69 | 1.04 | 0.68 | 0.07 | −3.64 | <0.001 | 0.56 | 0.84 | |||||
| const | 0.47 | 0.06 | −6.13 | <0.001 | 0.37 | 0.60 | 0.56 | 0.04 | −8.60 | <0.001 | 0.49 | 0.64 | |||||
| City | Var(const) | 0.18 | 0.08 | 0.08 | 0.41 | 0.04 | 0.02 | 0.01 | 0.12 | ||||||||
| Venues frequency | 7.71 | 0.0211 | 2.53 | 0.2826 | |||||||||||||
| No(0) | Ref | Ref | |||||||||||||||
| Low (1–3) | 1.00 | 0.09 | 0.04 | 0.97 | 0.84 | 1.19 | 0.89 | 0.07 | −1.42 | 0.155 | 0.75 | 1.05 | |||||
| High (3+) | 1.27 | 0.13 | 2.27 | 0.023 | 1.03 | 1.57 | 0.87 | 0.09 | −1.40 | 0.163 | 0.72 | 1.06 | |||||
| const | 0.43 | 0.05 | −6.78 | <0.001 | 0.34 | 0.55 | 0.58 | 0.05 | −6.70 | <0.001 | 0.49 | 0.68 | |||||
| City | Var(const) | 0.14 | 0.06 | 0.06 | 0.32 | 0.03 | 0.02 | 0.01 | 0.09 | ||||||||
| Serostatus communication | 6.56 | 0.0104 | 235.77 | <0.001 | |||||||||||||
| Unsuccessful | Ref | Ref | |||||||||||||||
| Successful | 0.83 | 0.06 | −2.56 | 0.01 | 0.72 | 0.96 | 2.99 | 0.21 | 15.35 | <0.001 | 2.60 | 3.44 | |||||
| const | 0.53 | 0.06 | −5.88 | <0.001 | 0.43 | 0.66 | 0.38 | 0.03 | −12.88 | <0.001 | 0.33 | 0.44 | |||||
| City | Var(const) | 0.12 | 0.05 | 0.05 | 0.30 | 0.05 | 0.03 | 0.02 | 0.13 | ||||||||
| Migration Status | 3.27 | 0.3514 | 11.98 | 0.0075 | |||||||||||||
| Native | Ref | Ref | |||||||||||||||
| Emigrant | 1.57 | 0.43 | 1.67 | 0.095 | 0.92 | 2.68 | 2.05 | 0.54 | 2.73 | 0.006 | 1.22 | 3.42 | |||||
| Immigrant | 0.94 | 0.11 | −0.58 | 0.564 | 0.75 | 1.17 | 0.96 | 0.10 | −0.34 | 0.732 | 0.78 | 1.19 | |||||
| Visitor | 0.96 | 0.16 | −0.26 | 0.794 | 0.68 | 1.34 | 1.37 | 0.21 | 2.11 | 0.035 | 1.02 | 1.85 | |||||
| const | 0.46 | 0.05 | −7.1 | <0.001 | 0.37 | 0.57 | 0.50 | 0.03 | −11.29 | <0.001 | 0.45 | 0.57 | |||||
| City | Var(const) | 0.14 | 0.06 | 0.06 | 0.33 | 0.03 | 0.02 | 0.01 | 0.09 | ||||||||
Notes: z = test statistic for an individual category in the bivariate model; P > z = significance of an individual category in the bivariate model; Wald Chi-square statistic and P-value are used to test the significance of a whole variable in the bivariate model; SE = Standard Error; OR: Odds Ratio
Casual partners
The results from the multivariate analyses are shown in Table 3 (casual partner). The analysis showed that CAI with casual partners was more likely amongst those who were ‘out’ to a majority (AOR = 1.19; 95% CI 1,1.42, P = 0.047); who knew their HIV status (AOR = 1.86; 95% CI 1.25,2.76, P = 0.002); who used 1–2 substances (drugs/alcohol; AOR = 1.39; 95% CI 1.16,1.63, P < 0.001); and, who used two or more substances (AOR = 1.81; 95% CI 1.35,2.42, P < 0.001). Being older (AOR = 0.98; 95% CI 0.97,0.99, P < 0.001); having successful sero-communication (AOR = 0.79; 95% CI 0.67,0.94, P = 0.006); and, not having had a recent HIV test (AOR = 0.78; 95% CI 0.66,0.92, P = 0.002), were all associated with reductions in the likelihood of CAI.
Table 3.
Multilevel model results identifying risk factors for CAI with casual partners compared to no CAI with casual partners
| Risk factor | Category | AOR | SE | 95% Confidence Interval | P-value | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Outness | Out to less than half | Ref | ||||
| Out to majority | 1.19 | 0.11 | 1.00 | 1.42 | 0.047 | |
| Had HIV test in last 12 months and results known | Yes | Ref | ||||
| No | 0.78 | 0.07 | 0.66 | 0.92 | 0.002 | |
| Sex role | Insertive | Ref | ||||
| Receptive | 1.18 | 0.11 | 0.98 | 1.41 | 0.082 | |
| Versatile | 0.88 | 0.09 | 0.72 | 1.07 | 0.174 | |
| Serostatus communication | Unsuccessful | |||||
| Successful | 0.79 | 0.07 | 0.67 | 0.94 | 0.006 | |
| Highest Educational level | Secondary or lower | Ref | ||||
| High school | 1.05 | 0.20 | 0.73 | 1.54 | 0.811 | |
| University | 0.85 | 0.16 | 0.59 | 1.22 | 0.375 | |
| Age | ||||||
| Continuous | 0.98 | <0.01 | 0.97 | 0.99 | <0.001 | |
| HIV status knowledge | Tested negative | Ref | ||||
| Newly diagnosed | 1.04 | 0.22 | 0.68 | 1.56 | 0.851 | |
| Already known | 1.86 | 0.37 | 1.25 | 2.76 | 0.002 | |
| Substances used | None | Ref | ||||
| 1–2 drugs | 1.39 | 0.12 | 1.16 | 1.63 | <0.001 | |
| >2 drugs | 1.81 | 0.27 | 1.35 | 2.42 | <0.001 | |
| Constant | 0.89 | 0.25 | 0.52 | 1.53 | 0.067 | |
| City | Variance (Constant) | 0.13 | 0.06 | 0.05 | 0.32 | |
LR test vs. logistic regression: chibar2(01) = 47.57 Prob. ≥ chibar2 = 0.0000
Notes: Adjusted Odds Ratio (AOR); Standard Error (SE)
Steady partners
With reference to the multivariate analyses in Table 4 (steady partner), CAI with a steady partner was more likely for those with successful sero-communication (AOR = 2.72; 95% CI 2.72,3.66, P < 0.001) and for those who had not been tested for HIV in the last 12 months (AOR = 1.26; 95% CI 1.09,1.46, P = 0.002). It was also approaching significance for those who reported being out to a majority (AOR = 1.16; 95% CI 1.00,1.36, P = 0.054). Reduced likelihood of CAI with a steady partner was associated with increasing age for all cities (AOR = 0.99; 95% CI 0.98,0.99, p,0.001).
Table 4.
Multilevel model results identifying risk factors for CAI with steady partners vs no CAI with steady partners
| Risk factor | Category | AOR | SE | 95% confidence interval | P-value | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Serostatus communication | Unsuccessful | Ref | ||||
| Successful | 2.72 | 3.66 | 2.72 | 3.66 | <0.001 | |
| Age | ||||||
| Continuous | 0.99 | <0.01 | 0.98 | 0.99 | <0.001 | |
| Outness | Out to less than half | Ref | ||||
| Out to majority | 1.16 | 0.09 | 1.00 | 1.36 | 0.054 | |
| Had HIV test in last 12 months and results known | Yes | Ref | ||||
| No | 1.26 | 0.10 | 1.09 | 1.46 | 0.002 | |
| Constant | 0.50 | 0.08 | 0.37 | 0.67 | <0.001 | |
| City | Variance (Constant) | 0.03 | 0.02 | 0.01 | 0.11 | |
LR test vs. logistic regression: chibar2(01) = 9.17 Prob. ≥ chibar2 < 0.0012.
Notes: Adjusted Odds Ratio (AOR); Standard Error (SE)
Age
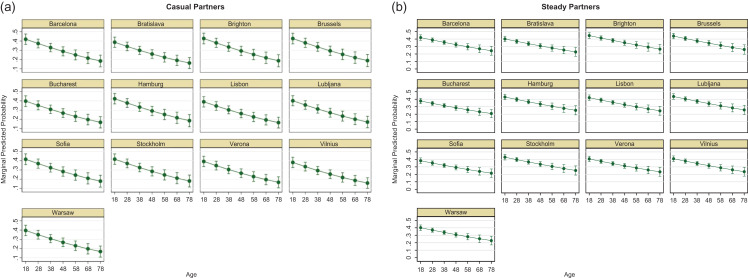
Figure 1 represents the estimated risk of CAI in respondents who have casual (a) and steady (b) partners by (continuous) age for each of the study cities. The two sets of graphs within Fig. 1 are not directly comparable because they are based on two different models incorporating different underlying theories on behaviours and risk. However, both sets show that overall young MSM are more likely to report higher levels of CAI compared to older MSM and the levels of CAI varies across cities. For instance Brighton has the largest estimated probabilities of CAI in casual partners: at age 18 years (years) P = 0.43 and this drops to P = 0.19 for older (78 yrs) MSM; Vilnius had the lowest probabilities and estimates ranged from P = 0.38 (18 years) to P = 0.16 (78 years). For steady partners, again Brighton has the largest estimated probabilities of P = 0.43 (18 years) and P = 0.26 (78 years); Bucharest had the lowest probabilities ranging from P = 0.35 (18 years) to P = 0.20 (78 years). Amongst MSM with steady partners, Barcelona, Brighton, Brussels, Hamburg, Lisbon, Ljubljana and Stockholm can all be grouped together as cities with consistently higher probabilities of CAI at each age; similarly Barcelona, Brighton, Brussels, Hamburg, Sofia and Stockholm all had higher probabilities at each age for CAI in casual partners compared to the other study sites.
Fig. 1.
Marginal predicted probabilities of CAI in casual and steady partners, by age group and city.
Discussion
Main finding of this study
A number of factors were associated with increased likelihood of CAI between MSM with casual partners including being ‘out’ to a majority, knowing one’s own HIV status, and using substances. Reductions in the likelihood of CAI were associated with being older, as well as successful sero-communication, and not having had a recent HIV test. Being older may be related to having experienced more intensive condom promotion and having witnessed the severe consequences of historically untreatable HIV infection. In terms of successful sero-communication: with casual partners sero-communication may be a surrogate for HIV-related concerns and higher intentions of self-protection, while sero-communication with steady partners may serve to confirm HIV sero-concordance and successful serosorting and to allow more ‘intimacy’ by practising CAI.
For those with at least one casual partner, having sex with a female and being a migrant were not associated with the likelihood of CAI. Similarly for MSM with at least one steady partner, the likelihood of CAI was positively associated with successful sero-communication and not having had a recent HIV test within the last 12 months; it was also negatively associated with increasing age. Interestingly, regardless of partner type, our analysis indicated a downward trend in the probability of CAI with increasing age. The gradual declining trend, and smaller 95% confidence intervals at the margins, indicated that relationships amongst steady partners are more stable whilst casual partners are more variable. These data suggest that regardless of partner type, prevention strategies may benefit from disproportionately targeting younger MSM.
What is already known on this topic
Previous studies have identified associations between CAI between MSM and relationship status.4,9,24–26 Concurring with our own findings, prior studies have also found significant associations between CAI and age with younger MSM seemingly more likely to engage in CAI with steady partners.24 In our study this was also the case although irrespective of partner type.
Of potential relevance to our analysis, a recent study from Australia has shown that a rapid increase in pre-exposure prophylaxis (PrEP) use by gay and bisexual men in Melbourne and Sydney was accompanied by an equally rapid decrease in consistent condom use with casual partners.13 Future studies may therefore wish to consider the importance of understanding the complex dynamics of partner type/relationship status for the prevention of other STIs as well as considering how CAI behavioural stratification could be used to determine who might benefit from tailored health promotion interventions including HIV PrEP.
What this study adds
Understandings of how partner type or relationship status may shape sexual behaviour such as CAI amongst MSM in European cities may help to play an important role in the development of culturally appropriate HIV/STI prevention and risk-reduction efforts targeting at-risk MSM. Our findings indicate the need for further investigation on how partner type and other partnership characteristics and dynamics may influence CAI and HIV and/or STI transmission amongst MSM.
Limitations of this study
Due to the cross-sectional nature of the study design, no causality or temporality between the associations examined can be inferred. An important limitation relates to the sampling methodology. TLS and RDS methods are considered quasi-probabilistic approaches, targeting MSM through their attendance in gay venues (TLS) or via social networks (RDS). This means that such approaches are subject to specific shortcomings such as the possible over- or under-representation of potential MSM sub-samples.27 However, TLS and RDS do nevertheless still represent one of the main and current approaches for recruiting most at-risk populations to bio-behavioural surveys.28 Survey data can of course be subject to specific biases related to the fact that some data were self-reported (excluding the data on HIV status when based on laboratory testing) limiting generalisability. This implies recall and social desirability bias given behaviours such as CAI were explored. The questionnaire has however been designed to overcome these potential biases, for instance through the active involvement of local gay NGOs in each site.29 It is also possible that although we provided descriptions of different partner types in the survey, variations regarding the interpretation of what constitutes a ‘steady’ versus a ‘non-steady/casual’ partner might not be uniform across study participants (e.g. see7).
Finally, as an EC co-funded project, the Sialon II project was designed to include cities from countries with different social and cultural contexts. As in many such EC-funded projects, cities were selected on the basis of previous research and collaboration networks and on the basis of pragmatic financial/organisational issues; therefore, some key cities with sizable gay populations have not been covered by the survey.
Despite the above limitations however, our analysis provides important information regarding the association between CAI and partnership characteristics amongst MSM in 13 European cities.
Contributor Information
Sialon II Network:
Massimo Mirandola, Christiana Nöstlinger, Ivailo Alexiev, Ulrich Marcus, Barbara Suligoi, Saulius Caplinskas, Magdalena Rosińska, Sónia Ferreira Dias, Alexandru Rafila, Danica Staneková, Irena Klavs, Cinta Folch, Inga Velicko, Igor Toskin, and Nigel Sherriff
Acknowledgements
The Sialon II Network (short list)
Massimo Mirandola, Lorenzo Gios (Infectious Diseases Section, Department of Pathology-Verona University Hospital – Veneto Region); Christiana Nöstlinger, Wim Vanden Berghe (Institute of Tropical Medicine, ITG, Antwerp, Belgium); Ivailo Alexiev (National Center of Infectious and Parasitic Diseases, Sofia, Bulgaria); Ulrich Marcus, Susanne Barbara Schink (Robert Koch Institute, Berlin, Germany); Barbara Suligoi, Vincenza Regine (Centro Operativo AIDS, Istituto Superiore di Sanità, Rome, Italy); Saulius Caplinskas, Irma Caplinskiene (Centre for Communicable Diseases and AIDS, Vilnius, Lithuania); Magdalena Rosińska, Marta Niedźwiedzka-Stadnik (NIZP-PZH, Warsaw, Poland); Sónia Ferreira Dias (Global Health and Tropical Medicine, GHTM, Instituto de Higiene e Medicina Tropical, IHMT, Universidade Nova de Lisboa, Portugal); Alexandru Rafila, Daniela Pitigoi (National Institute for infectious Diseases), Matei Bals (Carol Davila University of Medicine and Pharmacy, Bucharest, Romania); Danica Staneková, Monika Hábeková (Slovak Medical University, Bratislava, Slovakia); Irena Klavs (NIJZ - Nacionalni Institut za Javno Zdravje, Ljubljana, Slovenia); Cinta Folch, Laia Ferrer (Centre for Epidemiological Studies on HIV/STI in Catalonia CEEISCAT, Agència de Salut Pública de Catalunya, Barcelona, Spain); Inga Velicko, Sharon Kühlmann-Berenzon (Public Health Agency of Sweden, Stockholm, Sweden); Igor Toskin (Department of Reproductive Health & Research World Health Organization, Geneva, Switzerland); Nigel Sherriff (School of Health Sciences, University of Brighton, Brighton, UK).
Funding
This manuscript is based on data from the Sialon II project, co-funded under the Second Programme of Community Action in the field of Health (2008–2013) (Work Plan 2010). The sole responsibility lies with the authors of this manuscript and the Commission is not responsible for any use that may be made of the information contained therein.
Conflicts of interest
None.
Contributions
The SIALON II network participated in the design and implementation of the study. This analysis was conceived by NS, AMJ, and CL. Data were analysed by AMJ, NS, MM, and LG. The first draft was jointly written by NS and AMJ. All authors revised the manuscript for content. All authors read and approved the final manuscript.
References
- 1. European Centre for Disease. Prevention and Control/WHO Regional Office for Europe HIV/AIDS surveillance in Europe 2017–2016 data. Stockholm: ECDC, 2017. [Google Scholar]
- 2. Nwokolo N, Hill A, McOwan A et al. Rapidly declining HIV infection in MSM in central London. Lancet HIV 2017;4:E482–E3. [DOI] [PubMed] [Google Scholar]
- 3. Hart GJ, Elford J. Sexual risk behaviour of men who have sex with men: emerging patterns and new challenges. Curr Opin Infect Dis 2010;23:39–44. [DOI] [PubMed] [Google Scholar]
- 4. Cambou MC, Perez-Brumer AG, Segura ER et al. The risk of stable partnerships: Associations between partnership characteristics and unprotected anal intercourse among men who have sex with men and transgender women recently diagnosed with HIV and/or STI in Lima, Peru. PLoS One 2014;9:e102894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mercer CH, Jones KG, Johnson AM et al. How can we objectively categorise partnership type? A novel classification of population survey data to inform epidemiological research and clinical practice. Sex Transm Infect 2017;93:129–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Rocha GM, Kerr LR, de Brito AM et al. Unprotected receptive anal intercourse among men who have sex with men in Brazil. AIDS Behav 2013;17:1288–95. [DOI] [PubMed] [Google Scholar]
- 7. Van Den Boom W, Stolte I, Sandfort T et al. Serosorting and sexual risk behaviour according to different casual partnership types among MSM: the study of one-night stands and sex buddies. AIDS Care 2012;24:167–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Berg RC. High rates of unprotected sex and serosorting among men who have sex with men: a national online study in Norway. Scand J Public Health 2012;40:738–45. [DOI] [PubMed] [Google Scholar]
- 9. Kramer SC, Drewes J, Kruspe M et al. Factors associated with sexual risk behaviors with non-steady partners and lack of recent HIV testing among German men who have sex with men in steady relationships: results from a cross-sectional internet survey. BMC Public Health 2015;15:702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rosenberg ES, Sullivan PS, Dinenno EA et al. Number of casual male sexual partners and associated factors among men who have sex with men: Results from the National HIV Behavioral Surveillance system. BMC Public Health 2011;11:189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kippax S, Crawford J, Davis M et al. Sustaining safe sex: a longitudinal study of a sample of homosexual men. AIDS 1993;7:257–63. [PubMed] [Google Scholar]
- 12. Bogowicz P, Moore D, Kanters S et al. HIV testing behaviour and use of risk reduction strategies by HIV risk category among MSM in Vancouver. Int J STD AIDS 2016;27:281–7. [DOI] [PubMed] [Google Scholar]
- 13. Holt M, Lea T, Mao L et al. Community-level changes in condom use and uptake of HIV pre-exposure prophylaxis by gay and bisexual men in Melbourne and Sydney, Australia: results of repeated behavioural surveillance in 2013–17. Lancet HIV 2018;5:E448–E56. [DOI] [PubMed] [Google Scholar]
- 14. Gios L, Mirandola M, Toskin I et al. Bio-behavioural HIV and STI surveillance among men who have sex with men in Europe: the Sialon II protocols. 2016. [DOI] [PMC free article] [PubMed]
- 15. Mirandola M, Gios L, Sherriff NS et al. SIALON II: Capacity Building in Combining Targeted Prevention with Meaningful HIV Surveillance Among MSM: A Bio-behavioural Survey Amongst MSM in 13 European Cities. Verona: Cierre Grafica, 2016. [Google Scholar]
- 16. Mirandola M, Gios L, Sherriff N et al. Quantifying unmet prevention needs among MSM in Europe through a multi-site bio-behavioural survey. Euro Surveill 2018;23:1800097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Karon JM, Wejnert C. Statistical methods for the analysis of time—location sampling data. J Urban Health 2012;89:565–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Dudareva-Vizule S, Marcus U. Sialon II: Formative Research Report. Berlin: Robert Koch Institute, 2013. [Google Scholar]
- 19. Johnston LG, Sabin K. Sampling hard-to-reach populations with respondent driven sampling. Methodol Innov Online 2010;5:38–48. [Google Scholar]
- 20. UNAIDS Global AIDS Monitoring 2018. Indicators for Monitoring the 2016 United Nations Political Declaration on Ending AIDS. Geneva: UNAIDS, 2018. [Google Scholar]
- 21. Mirandola M, Folch Toda C, Krampac I et al. HIV bio-behavioural survey among men who have sex with men in Barcelona, Bratislava, Bucharest, Ljubljana, Prague and Verona, 2008–2009. Euro Surveill 2009;14:22–9. [DOI] [PubMed] [Google Scholar]
- 22. Sherriff N, Gugglberger L. A European Seal of Approval for ‘gay’ businesses: findings from an HIV-prevention pilot project. Perspect Public Health 2014;134:150–9. [DOI] [PubMed] [Google Scholar]
- 23. Marcus U, Schink S, Sherriff N et al. HIV serostatus knowledge and serostatus disclosure with the most recent anal intercourse partner in a European MSM sample recruited in 13 cities: Results from the Sialon-II study. 2017. [DOI] [PMC free article] [PubMed]
- 24. Crepaz N, Marks G, Mansergh G et al. Age-related risk for HIV infection in men who have sex with men: Examination of behavioral, relationship, and serostatus variables. AIDS Educ Prev 2000;12:405–15. [PubMed] [Google Scholar]
- 25. Forney JC, Miller RL. City Project Study T. Risk and protective factors related to HIV-risk behavior: a comparison between HIV-positive and HIV-negative young men who have sex with men. AIDS Care 2012;24:544–52. [DOI] [PubMed] [Google Scholar]
- 26. Liu J, Qu B, Ezeakile MC et al. Factors associated with unprotected anal intercourse among men who have sex with men in Liaoning Province, China. PLoS One 2012;7:e50493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kendall C, Kerr LRFS, Gondim RC et al. An empirical comparison of respondent-driven sampling, time location sampling, and snowball sampling for behavioral surveillance in men who have sex with men, Fortaleza, Brazil. AIDS Behav 2008;12:97. [DOI] [PubMed] [Google Scholar]
- 28. Gios L, Mirandola M, Toskin I et al. Bio-behavioural HIV and STI surveillance among men who have sex with men in Europe: The Sialon II protocols. BMC Public Health 2016;16:212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Rosenman R, Tennekoon V, Hill LG. Measuring bias in self-reported data. Int J Behav Health Res 2011;2:320–32. [DOI] [PMC free article] [PubMed] [Google Scholar]