Key Points
Question
Does doxycycline reduce the growth of small (3.5-5.0 cm in men, 3.5-4.5 cm in women) infrarenal abdominal aortic aneurysms?
Findings
In this randomized clinical trial that included 254 adults, doxycycline 100 mg orally twice daily compared with placebo did not significantly reduce aneurysm growth at 2 years as measured by a rank score accounting for change in maximum transverse diameter and clinical outcomes of death and repair (mean increase in maximum transverse diameter of abdominal aortic aneurysm, 0.36 cm vs 0.36 cm).
Meaning
Doxycycline did not significantly reduce growth of small abdominal aortic aneurysms after 2 years.
Abstract
Importance
Abdominal aortic aneurysms affect more than 3% of US older adults.
Objective
To test whether doxycycline reduces the growth of abdominal aortic aneurysm over 2 years as measured by maximum transverse diameter.
Design, Setting, and Participants
Parallel, 2-group, randomized clinical trial that was conducted at 22 US clinical centers between May 2013 and January 2017, and enrolled patients 50 years or older with small (3.5-5.0 cm for men, 3.5-4.5 cm for women) infrarenal aneurysms. The final date of follow-up was July 31, 2018.
Interventions
Patients were randomized to receive twice daily for 2 years doxycycline 100 mg orally (as capsules) (n = 133) or placebo (n = 128).
Main Outcomes and Measures
The primary outcome was change in abdominal aortic aneurysm maximum transverse diameter measured from CT images at baseline and follow-up at 2 years. Patients were assigned ranks based on the maximum transverse diameter (measured or imputed) of the aorta and also if they underwent aneurysm repair or died. The ranks were converted to scores having a normal distribution to facilitate the primary analysis (“normal scores”).
Results
Of 261 patients randomized, no follow-up CT scans were obtained on 7 (3%), leaving a final analysis set of 129 patients assigned to doxycycline and 125 to placebo (mean [SD] age, 71.0 years [7.4 years], 35 women [14%]). The outcome normal scores used in the primary analysis were based on maximum transverse diameter (measured or imputed) in 113 patients (88%) in the doxycycline group and 112 patients (90%) in the placebo group; aneurysm repair in 13 (10%) and 9 (7%), and death in 3 (2%) and 4 (3%), respectively. The primary outcome, normal scores reflecting change in aortic diameter, did not differ significantly between the 2 groups, mean change in normal scores, 0.0262 vs −0.0258 (1-sided P = .71). Mean (SD) baseline maximum transverse diameter was 4.3 cm (0.4 cm) for doxycycline and 4.3 cm (0.4 cm) for placebo. At the 2-year follow-up, the change in measured maximum transverse diameter was 0.36 cm (95% CI, 0.31 to 0.40 cm) for 96 patients in the doxycycline group vs 0.36 cm (95% CI, 0.30 to 0.41 cm) for 101 patients in the placebo group (difference, 0.0; 95% CI, −0.07 to 0.07 cm; 2-sided P = .93). No patients were withdrawn from the study because of adverse effects. Joint pain occurred in 84 of 129 patients (65%) with doxycycline and 79 of 125 (63%) with placebo.
Conclusions and Relevance
Among patients with small infrarenal abdominal aortic aneurysms, doxycycline compared with placebo did not significantly reduce aneurysm growth at 2 years. These findings do not support the use of doxycycline for reducing the growth of small abdominal aortic aneurysms.
Trial Registration
ClinicalTrials.gov Identifier: NCT01756833
This randomized trial compares the effect of doxycycline with placebo on reducing CT-measured abdominal aortic aneurysms over 2 years among patients with small infrarenal abdominal aortic aneurysms.
Introduction
Abdominal aortic aneurysm is a progressive, life-threatening vascular disorder that affects up to 3.3% of older adults.1,2 Large aneurysms are at high risk of rupture, with more than 30% case fatality among those who present to a hospital.3 Asymptomatic small aneurysms are detectable with noninvasive screening and treatable with endovascular stenting or open surgery.4
Matrix metalloproteinases (MMPs) are implicated in the development of aneurysms. In murine models, aneurysms are induced by elastase infusion or calcium chloride application, and doxycycline inhibits both MMPs and growth in these aneurysms.5,6,7 Matrix metalloproteinases mediate elastin and collagen degradation in the aortic wall, and MMP-9 levels are elevated in patients who have abdominal aortic aneurysms. Tetracyclines inhibit MMPs. Doxycycline reduces inflammation and MMP-9 content in human abdominal aortic aneurysms that are not caused by heritable connective tissue disorders.8,9
Because tetracyclines inhibit MMPs and because MMPs may play a role in aneurysm development, tetracyclines have been examined in clinical trials for their ability to reduce aneurysm expansion. These trials have been inconclusive. One published placebo-controlled randomized clinical trial of doxycycline for the treatment of abdominal aortic aneurysms suggested that doxycycline accelerated aneurysm growth but was inconclusive because the trial had substantial losses to follow-up.10 In an earlier, placebo-controlled, randomized clinical trial there was a possible benefit of doxycycline in slowing aneurysm growth but that effect may have resulted from the doxycycline group having smaller aneurysms at baseline in spite of randomization because aneurysm size is a correlate of aneurysm growth.11,12
To determine if tetracyclines can reduce aneurysm growth in humans, the Non-Invasive Treatment of Abdominal Aortic Aneurysm Clinical Trial (N-TA3CT) was performed as a placebo-controlled, phase 2b, randomized clinical trial to address the hypothesis that doxycycline could reduce the growth of small abdominal aortic aneurysms as measured by maximum transverse diameter.
Methods
Background
The design and methods of this clinical trial have been published13; the protocol and statistical analysis plan are provided in Supplement 1 and Supplement 2. The protocol was approved by the institutional review boards at all clinical sites, core laboratories, and coordinating centers. All randomized patients gave written informed consent.
Participants
Patients with small infrarenal aneurysms (3.5-5.0 cm for men and 3.5-4.5 cm for women) were randomized starting in May 2013. The initial recruitment goal of 248 was reached in July 2016. Ten additional female patients were randomized to improve representation of women within the limits of supplemental funding. Recruitment ended in January 2017.
Randomization
Treatments were assigned using computer-generated random numbers in a separate schedule for each of the 22 US clinical sites with randomly varying block sizes of 2, 4, and 6, and 1:1 ratio of doxycycline to placebo within each block, stratified by sex within each clinical site.
Intervention
The doxycycline group received 100 mg doxycycline orally (as capsules) twice daily for 2 years. The placebo group received identical-appearing capsules twice daily for 2 years.
Outcomes
The primary outcome was based on maximum transverse diameter at the 2-year follow-up, as measured by rank score adjusted for baseline rank score and clinical outcomes of death and repair. Aneurysm maximum transverse diameter was measured perpendicularly to the center line and assessed with treatment assignment concealed. The measurements were made from computed tomographic (CT) images in semiautomated fashion at baseline and 2-year follow-up by Imaging Core Laboratory technical staff under the direction of one of the authors (J.M.).
Prespecified secondary outcomes reported herein include maximum transverse diameters measured at 6, 12, 18, and 24 months; aneurysm volume; adverse effects; levels of doxycycline, MMP-9, and C-reactive protein (CRP); and occurrence of aneurysm rupture, aneurysm repair, and death.
Secondary outcomes not reported herein include acute myocardial infarction, unstable angina, aneurysm neck length and diameter, characteristics of the neck, serial measurements of aneurysm growth patterns, wall stress, stroke, arterial thromboembolism, venous thromboembolism, infections, interferon-γ levels, and quality of life.
Follow-up
Follow-up visits were conducted at 3-month intervals for prescription renewal and clinical evaluation. Abdominal and pelvic CT scans and peripheral blood were obtained at enrollment and every 6 months thereafter. The original protocol was predicated on ending follow-up for all patients on the same date with different lengths of follow-up, all at least 2 years, but was revised, before investigators knew results, to 2 years of follow-up for every patient.
Sample Size
Assuming a correlation of 0.82 between baseline and 2-year maximum transverse diameter measurements, a diameter measurement standard deviation of 7 mm, 1-sided α of .025, a 1-sided null hypothesis, and statistical test were used because the primary interest was to demonstrate efficacy of doxycycline in slowing the growth of abdominal aortic aneurysms. The criterion (“α”) set for statistical significance was 1-sided .025; use of this level means that the inference from the test result will be the same as the inference from 2-sided testing at the .05 significance level.14 We assumed a growth rate for patients in the placebo group of 0.25 cm per year—a growth rate that is conservative compared with an earlier study and the investigators’ analyses of others’ longitudinal preliminary data—and 10% nonadherence in the doxycycline group, and 15% noninformative loss of data; the required sample size was 124 patients per treatment group for statistical power of 0.90.13,15 The minimal clinically important difference was defined as a reduction in the rate of growth of 0.10 cm per year because smaller reductions in aneurysm growth would not greatly reduce requirements for surgical repair.13
Statistical Analysis
Categorical data are presented as number (%) and continuous data as mean (SDs) or median (interquartile ranges). The primary analysis was performed according to randomization group. Patients who never took the study treatment and never returned for follow-up visits or were assigned to placebo and returned for a 3-month visit but never thereafter were not included in the analyses.
For the primary analysis, diameters at baseline were ranked from smallest to largest (ranks 1-254). At the 2-year follow-up, ranks 1 through 225 were assigned to the diameters of surviving patients with no aneurysm repair (with missing values estimated by multiple imputation16,17), ranks 226 through 247 were assigned to surviving patients who underwent aneurysm repair (in order of longest to shortest time from randomization to repair), and ranks 248 through 254 were assigned to patients who died (in order of longest to shortest time from randomization to death). Each rank was converted to a normal score corresponding to the value on the standard normal curve (z score) of its percentile among all 254 ranks.
The primary analysis was based on linear regression of the change in normal scores from baseline to 2 years. Independent variables were baseline normal score, sex, and a dichotomous variable for the randomly assigned treatment group (0 for placebo, 1 for doxycycline). A term for sex-treatment interaction was also included as planned a priori in order to assess whether separate analyses for men and women were necessary (the eAppendix in Supplement 3).
The regression model for the change in the normal score was run for each of 100 imputations. For each imputation, missing 2-year diameter values were estimated from available diameter data at 6, 12, 18, and 30 months and from selected baseline variables.16,17 The imputed diameter values were then used to assign ranks and normal scores. Final coefficients were estimated as the means of the coefficients from the 100 regression analyses. Division of the final coefficient for the treatment group variable by its estimated standard error16,17 resulted in a t statistic with degrees of freedom estimated according to Barnard and Rubin,18 for which the 1-sided P value is reported as specified in the study protocol13 (Supplements 1 and 2).
Two prespecified interim analyses for efficacy were performed when approximately one-third and two-thirds of the primary outcome information was available, with significance level α set at 1-sided .0005. The final analysis was 1-sided with α = .024. A futility analysis with conditional power set at 0.20 was performed when approximately two-thirds of the primary outcome information was available.19
In secondary analysis, treatment effects were estimated for the repeated-measures biomarker data using generalized estimating equations with exchangeable correlation matrices on log-transformed values of MMP-9 and CRP.20 The α level for secondary outcome analyses (all 2-sided) was set at .01 to account for multiple comparisons. In a post hoc analysis to account for correlation of observations at the same clinical site and within the same patient, a mixed-effects model was fit to the longitudinal data. This model included random effects for site; random intercepts and maximum transverse diameter growth rates for patients; and fixed effects for treatment, time, and treatment-by-time interaction.
Medication adherence was defined as the percentage of study treatment capsules taken, based on the number of capsules returned at clinic visits between randomization and 2-year CT scan performance (or last clinic visit for those with missing 2-year scans), aneurysm repair, or death. Several per-protocol analyses were conducted based on the population of patients whose adherence was 80% or more.
Confidence intervals were calculated with exact methods for proportions and derived from t tests for differences in means. Correlations of maximum transverse diameter measurements were made with Pearson correlation.
Analyses were performed with SAS version 9.4 for Windows, 2002-2012 (SAS Institute Inc) using the following procedures: PROC FREQ, PROC GLM, PROC HPMIXED, PROC MEANS, PROC MI, PROC MIANALYZE, PROC PROBIT, PROC REPORT, and PROC TTEST.
Results
Recruitment
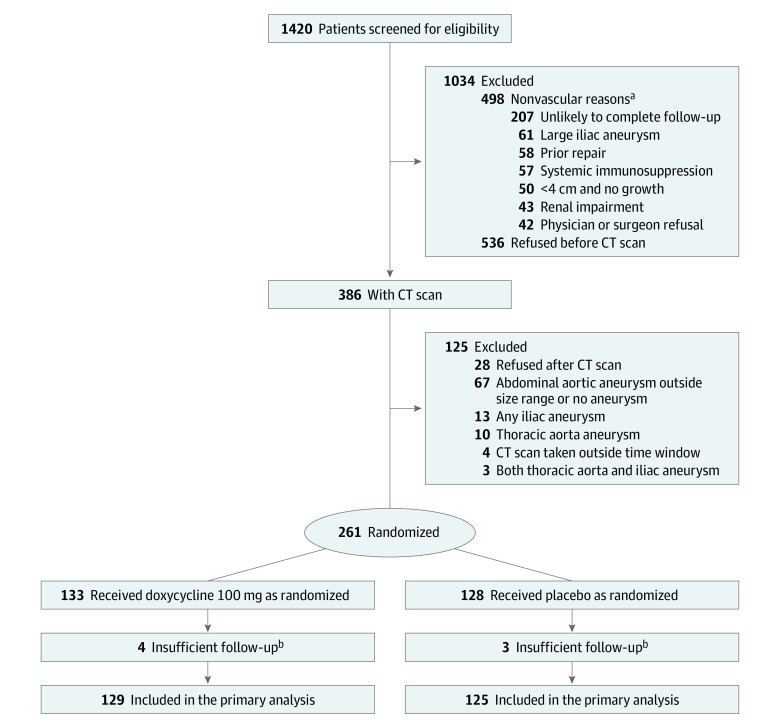
Randomization took place between May 2013 and January 2017. Of 1420 patients screened, 261 were randomized (Figure 1). There were 498 patients deemed ineligible following their initial evaluation. Ineligibility occurred because patients had a likelihood for survival of less than 2 years, were doxycycline intolerant, were immunosuppressed, or were being treated with long-term antibiotic therapy. Sixty-seven patients were determined to be ineligible because after the central reading of their baseline CT scans they were found not to have had an aneurysm or because their aneurysm size was outside the eligible range. There were 564 patients who declined to participate in the trial because of their fear of radiation from CT scans, were unable to pay the co-pay for CT scans, were already taking too many medications, or could not travel long distances to the clinical site.
Figure 1. Recruitment, Randomization, and Patient Flow Through the Non-Invasive Treatment of Abdominal Aortic Aneurysm Clinical Trial.
aPatients may have had more than 1 reason for exclusion, less frequently were allergy or intolerance of tetracycline (n = 12), use of tetracycline in last 6 months (n = 19), long-term infection and antibiotic use (n = 20), enrollment in another clinical trial (n = 15), known genetic syndrome (n = 2).
bPatients did not take treatment or did not return for follow-up.
CT indicates computed tomography.
Study participants were mostly white (76%) and male (86%) with a mean (SD) age of 71.0 years (7.4 years). Baseline characteristics of patients in the 2 treatment groups were similar (Table 1). eTable 1 in Supplement 3 provides baseline information on 7 patients who were not included in any analyses. The mean (SD) baseline maximum transverse diameter was 4.3 cm (0.4 cm) in the doxycycline group and 4.3 cm (0.4 cm) in the placebo group.
Table 1. Baseline Characteristics by Treatment Assignment.
| No. (%) of patients | ||
|---|---|---|
| Doxycycline (n = 129) |
Placebo (n = 125) |
|
| Demographics | ||
| Age, mean (SD), y | 71.0 (7.5) | 70.9 (7.3) |
| Sex | ||
| Women | 18 (14) | 17 (14) |
| Men | 111 (86) | 108 (86) |
| Health status | ||
| Smoking status | ||
| Current | 44 (34) | 43 (34) |
| Former | 75 (58) | 73 (58) |
| Never | 10 (8) | 9 (7) |
| Hypercholesterolemia | 98 (76) | 98 (78) |
| Coronary artery disease | 51 (40) | 53 (42) |
| Cancer | 44 (34) | 38 (30) |
| Chronic obstructive pulmonary disease | 30 (23) | 29 (23) |
| Diabetes | 35 (27) | 22 (18) |
| Family history of abdominal aortic aneurysm | 27 (21) | 20 (16) |
| Atrial fibrillation | 16 (12) | 17 (14) |
| Stroke | 13 (10) | 15 (12) |
| Congestive heart failure | 11 (9) | 9 (7) |
| Medications | ||
| Statin | 104 (81) | 103 (82) |
| Any antihypertensive | 105 (81) | 94 (75) |
| β-Blocker | 68 (53) | 63 (50) |
| Diuretics | 43 (33) | 40 (32) |
| Angiotensin-converting enzyme inhibitor | 51 (40) | 37 (30) |
| Calcium channel blocker | 26 (20) | 34 (27) |
| Angiotensin receptor blocker | 20 (16) | 25 (20) |
| Aspirin or other antiplatelet | 95 (74) | 92 (74) |
| Daily aspirin | 86 (67) | 89 (71) |
| Other antiplatelet | 19 (15) | 25 (20) |
| Aneurysm maximum transverse diameter, cm | ||
| Overall | ||
| No. | 129 | 125 |
| Mean (SD) | 4.3 (0.4) | 4.3 (0.4) |
| Median (IQR) | 4.3 (4.0-4.6) | 4.4 (4.0-4.7) |
| Men | ||
| No. | 111 | 108 |
| Mean (SD) | 4.3 (0.4) | 4.4 (0.4) |
| Median (IQR) | 4.3 (4.0-4.7) | 4.4 (4.1-4.7) |
| Women | ||
| No. | 18 | 17 |
| Mean (SD) | 4.1 (0.3) | 3.9 (0.3) |
| Median (IQR) | 4.1 (3.8-4.4) | 3.9 (3.7-4.1) |
| Aneurysm volume, cm3 | ||
| Overall | ||
| No. | 129 | 125 |
| Mean (SD) | 97.0 (24.0) | 95.8 (24.0) |
| Median (IQR) | 96.9 (78.5-114.1) | 92.5 (77.4-109.3) |
| Men | ||
| No. | 111 | 108 |
| Mean (SD) | 99.0 (24.3) | 99.2 (23.3) |
| Median (IQR) | 98.7 (78.9-115.8) | 94.7 (80.6-113.5) |
| Women | ||
| No. | 18 | 17 |
| Mean (SD) | 84.9 (18.5) | 74.3 (15.9) |
| Median (IQR) | 84.7 (77.0-98.3) | 72.3 (61.7-87.1) |
Abbreviation: IQR, interquartile range.
Follow-up
Measured aortic diameter at 2 years, occurrence of aneurysm repair, or death was available for 112 of 129 patients (87%) in the doxycycline group and 114 of 125 (91%) in the placebo group. Seven patients were not included in any analyses; 6 never took study treatment and never returned for a follow-up visit; and 1, assigned to placebo, returned for treatment at 3 months but never returned thereafter.
The correlation of 2-year maximum transverse diameter measurements was 0.98 with 18-month measurements, 0.96 with 12-month measurements, 0.93 with 6-month measurements, and 0.89 with baseline measurements.
Primary Outcome
The outcome normal scores used in the primary analysis were based on maximum transverse diameter (measured or imputed) in 113 patients (88%) in the doxycycline group and 112 (90%) in the placebo group, aneurysm repair in 13 patients (10%) in the doxycycline group and 9 (7%) in the placebo group, and death in 3 patients (2%) in the doxycycline group and 4 (3%) in the placebo group. In the primary analysis, normal scores reflecting the change in aortic size did not differ significantly between the groups; the mean change in normal score from baseline to 24 months was 0.0262 among patients in the doxycycline group and −0.0258 among patients in the placebo group; normal scores for growth were less favorably located in the distribution for patients in the doxycycline group than for patients in the placebo group by a small amount. After adjustment in linear regression for baseline normal score and sex, the mean difference (doxycycline minus placebo normal score change) was 0.041 (1-sided P = .71 against the null hypothesis of equal or higher growth with doxycycline); the treatment by sex interaction was not significant (P = .06) (eAppendix in Supplement 3).
After 2 years of follow-up, the mean change in measured maximum transverse diameter was 0.36 cm (95% CI, 0.31 to 0.40 cm) for 96 patients in the doxycycline group and 0.36 cm (95% CI, 0.30 to 0.41 cm) for 101 patients in the placebo group for whom CT scans were available (difference, 0 cm; 95% CI, −0.07 to 0.07 cm; 2-sided P = .93). The difference between doxycycline and placebo in mean 2-year change in maximum transverse diameter was −0.02 cm (95% CI, −0.10 to 0.05 cm; 2-sided P = .59) for men and 0.13 cm (95% CI, −0.04 to 0.29 cm; 2-sided P = .12) for women.
The mean (SD) maximum transverse diameter at 2 years was similar in the full analysis population (4.61 cm [0.52 cm] in the doxycycline group, 4.61 cm [0.53 cm] in the placebo group) and in the per-protocol population (4.54 cm [0.55 cm] in the doxycycline group, 4.66 cm [0.50 cm] in the placebo group) (Table 2).
Table 2. Maximum Transverse Diameter and Volume of Abdominal Aortic Aneurysms by Treatment Assignment.
| Doxycycline (n = 129) |
Placebo (n = 125) |
Difference (95% CI) | P valuea | |
|---|---|---|---|---|
| Full analysis population | ||||
| Maximum transverse diameter, cm | ||||
| 6 mo, No. of patients | 119 | 116 | ||
| Mean (SD) | 4.40 (0.44) | 4.40 (0.43) | 0 (−0.12 to 0.11) | .94 |
| 1 y, No. of patients | 119 | 113 | ||
| Mean (SD) | 4.49 (0.48) | 4.48 (0.44) | 0.02 (−0.10 to 0.13) | .80 |
| 2 y, No. of patients | 96 | 101 | ||
| Mean (SD) | 4.61 (0.52) | 4.61 (0.53) | 0 (−0.15 to 0.15) | .99 |
| Baseline to 2-y change | ||||
| No. of patients b | 96 | 101 | ||
| Mean (SD) | 0.36 (0.21) | 0.36 (0.28) | 0 (−0.07 to 0.07) | .93 |
| Volume, cm3 | ||||
| 6 mo, No. of patients | 119 | 116 | ||
| Mean (SD) | 102.90 (26.19) | 100.40 (26.27) | 2.52 (−4.22 to 9.26) | .46 |
| 1 y, No. of patients | 119 | 113 | ||
| Mean (SD) | 106.00 (29.13) | 105.00 (28.28) | 0.95 (−6.48 to 8.38) | .80 |
| 2 y, No. of patients | 96 | 101 | ||
| Mean (SD) | 113.60 (34.91) | 111.20 (33.14) | 2.41 (−7.16 to 11.97) | .62 |
| Baseline to 2-y change | ||||
| No. of patientsb | 96 | 101 | ||
| Mean (SD) | 18.60 (14.38) | 19.16 (15.75) | −0.56 (−4.81 to 3.68) | .79 |
| Per-protocol population | ||||
| Maximum transverse diameter, cm | ||||
| 6 mo, No. of patients | 64 | 71 | ||
| Mean (SD) | 4.35 (0.47) | 4.42 (0.41) | −0.07 (−0.21 to 0.08) | .38 |
| 1 y, No. of patients | 66 | 72 | ||
| Mean (SD) | 4.44 (0.49) | 4.51 (0.42) | −0.07 (−0.23 to 0.08) | .35 |
| 2 y, No. of patients | 61 | 67 | ||
| Mean (SD) | 4.54 (0.55) | 4.66 (0.50) | −0.12 (−0.30 to 0.06) | .21 |
| 2-y to Baseline, No. of patients b | 61 | 67 | ||
| Mean (SD) | 0.33 (0.22) | 0.36 (0.26) | −0.03 (−0.12 to 0.05) | .47 |
| Volume, cm3 | ||||
| 6 mo, No. of patients | 64 | 71 | ||
| Mean (SD) | 96.70 (25.95) | 101.60 (23.48) | −4.89 (−13.31 to 3.52) | .25 |
| 1 y, No. of patients | 66 | 72 | ||
| Mean (SD) | 100.70 (28.79) | 105.60 (25.64) | −4.93 (−14.10 to 4.23) | .29 |
| 2 y, No. of patients | 61 | 67 | ||
| Mean (SD) | 106.80 (35.67) | 114.00 (31.98) | −7.22 (−19.06 to 4.61) | .23 |
| 2-y to Baseline, No. of patients b | 61 | 67 | ||
| Mean (SD) | 15.78 (13.95) | 19.16 (16.18) | 3.38 (−8.69 to 1.93) | .21 |
Two-sample t test P values.
Mean changes in measured maximum transverse diameter and volume based on patients for whom computed tomographic scans were available.
Secondary Outcomes
At 2 years, 3 of 129 patients (2.3%) in the doxycycline group had died compared with 4 of 125 patients (3.2%) in the placebo group (difference −0.9%; 95% CI, −4.9% to 3.2%, P = .67). Thirteen of 129 patients (10.1%) in the doxycycline group had an aneurysm repair compared with 9 of 125 (7.2%) in the placebo group (difference, 2.9%; 95% CI, −4.3% to 10.0%, P = .41). No ruptures were observed during follow-up (95% CI, 0% to 1.4%).
Among patients assigned to doxycycline, doxycycline levels at 6-month follow-up ranged from 0 to 9362 ng/mL with a mean of 3100 ng/mL (95% CI, 2669-3531 ng/mL) in the full analysis population and 3681 ng/mL (95% CI, 3156-4207 ng/mL) in the per-protocol population (eTable 4 in Supplement 3).
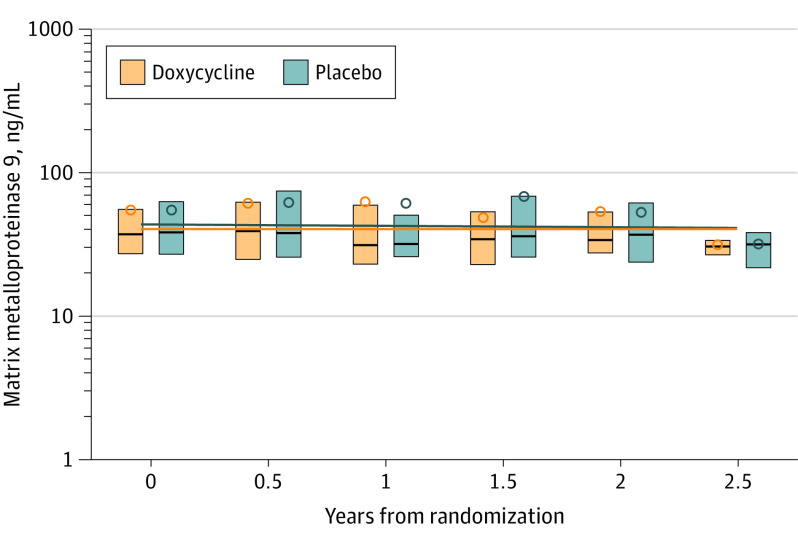
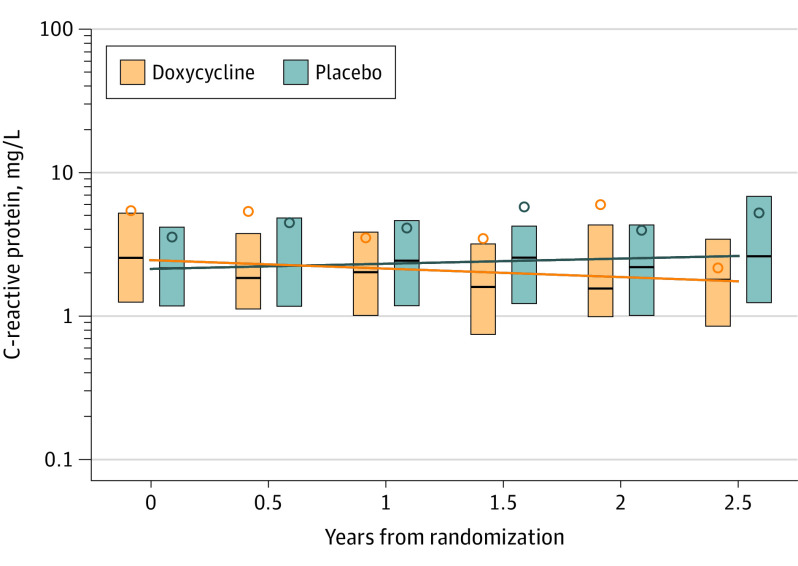
There were no significant differences in log-transformed MMP-9 (ng/mL) levels between the doxycycline (n = 521 specimens) and placebo (n = 507 specimens) groups for whom there were measurements at any of the specimen collection times or in longitudinal analysis—difference in slope per year was −0.001 (95% CI, −0.051 to 0.049, P = .86) for log(MMP-9)—using generalized estimating equations (Figure 2 and eTable 2 in Supplement 3). There was a significant difference between the groups in log-transformed CRP (mg/L) in longitudinal analysis—difference in slope per year was −0.089 (95% CI, −0.161 to −0.016, P = .002) for log(CRP)—with a decrease in CRP in the doxycycline group over time (eTable 2 Supplement 3; Figure 3).
Figure 2. Estimates of Matrix Metalloproteinase 9 Levels on a Log Scale From Generalized Estimating Equations Analysis by Treatment Assignment.
The difference between doxycycline and placebo in slope per year is −0.001 (95% CI, −0.051 to 0.049; P = .86) for log(matrix metalloproteinase 9), ng/mL. Open circles represent mean values; lines in the boxes, medians; the box ends, interquartile ranges; and lines spanning boxes, slope.
Figure 3. Estimates of C-Reactive Protein on a Log Scale From Generalized Estimating Equations Analysis by Treatment Assignment.
The difference between doxycycline and placebo in slope per year is −0.089 (95% CI, −0.161 to −0.016; P = .002) for log(C-reactive protein), mg/L. Open circles represent mean values; lines in the boxes, medians; the box ends, interquartile ranges; and lines spanning boxes, slope.
One or more prespecified adverse effects occurred in 121 of 129 patients (94%) in the doxycycline group and 111 of 125 (89%) in the placebo group (eTable 3 in Supplement 3). Patients permanently discontinued treatment in association with adverse effects in 22 of 129 patients (17%) in the doxycycline group and 9 of 125 (7%) in the placebo group. The most commonly reported adverse effect was frequent joint pains, which affected 84 of 129 patients (65%) in the doxycycline group and 79 of 125 (63%) in the placebo group. Moderate to severe sunburn occurred in 38 of 129 (29%) in the doxycycline group and 14 of 125 (11%) in the placebo group. Serious or unexpected adverse events occurred in 70 of 129 (54%) in the doxycycline group and 71 of 125 (57%) in the placebo group.
Additional Analyses
Seventy-seven of 129 patients (60%) in the doxycycline group and 86 of 125 (69%) in the placebo group had 80% or better adherence to study treatment. Less than 50% adherence was observed in 23 patients (18%) in the doxycycline group and 18 (14%) in the placebo group.
There was no significant effect of doxycycline when the primary analysis was repeated in the per-protocol population (1-sided P = .53).
In a post hoc analysis, a mixed-effects model using maximum transverse diameter measurements from baseline, 6, 12, 18, and 24 months and including clinical site as a random effect found that maximum transverse diameter growth did not differ significantly between groups (difference, 0.016 cm; 95% CI, −0.050 to 0.082 cm).
Discussion
In this trial involving patients with small infrarenal aneurysms, treatment with doxycycline compared with placebo did not significantly reduce aneurysm growth over 2 years, as determined by analysis of normal scores that incorporated measured or imputed aneurysm diameter, aneurysm repair, and death. This result differed from prior studies that either showed reduced11 or increased10 aneurysm growth attributable to doxycycline. The differences in these results might be explained by differing ways of measuring aortic diameter. Variability in aortic measurements with ultrasound, used in both prior studies, is much greater than with CT scan, used in the current study.15 Also, calcium landmarks used to define the aortic wall on ultrasound may be modified by doxycycline therapy.21 Moreover, in the study by Mosorin et al11,12 the doxycycline group had smaller aneurysms than the placebo group at baseline in spite of randomization. Given the positive correlation of aneurysm size with growth rate, this could explain the seemingly favorable effect of doxycycline on reducing abdominal aortic aneurysm growth in that study. In the Pharmaceutical Aneurysm Stabilization Trial (PHAST),10 the doxycycline dose was 100 mg daily vs 100 mg twice daily in the current study. Also, in PHAST, 27% of patients, most of whom had received some treatment, withdrew and could not be included in the analysis. In the current study, only 3% of randomized patients (only 1 of whom, a placebo-assigned patient, took any study treatment) were excluded from the final analysis.
The total dose used in the present study (200 mg/d) corresponds to the dose that results in circulating levels of doxycycline necessary to reduce aneurysm growth in studies of calcium chloride injury of the abdominal aorta in mice.7 Doxycycline levels among patients assigned to the active treatment were within the lower part of the range found efficacious in murine models. The absence of a doxycycline effect was observed in the full analysis and in the per-protocol analysis, which included patients who would have had, on average, greater exposure to doxycycline than those in the full population.
The statistical methods in the current clinical trial were selected for robustness against the possibility of informative missingness of data. Assigning worst ranks to deaths and next worst ranks to aneurysm repairs made it possible to reduce the number of patients whose outcomes were not fully taken into account in the analysis. This approach helps to reduce bias that could be introduced if death or aneurysm repair was more common in one of the groups (eg, if doxycycline treatment led to more deaths or repairs), and could obscure disease progression in that group because of less complete ascertainment of outcome on CT scans. Also, the use of multiple imputation protects against losses of statistical power due to data missing at random.
Although studies performed in animal models5,6,7 found that doxycycline had reduced systemic MMP-9 levels, the current trial showed that doxycycline did not reduce systemic MMP-9 levels compared with placebo. Short-term therapy has reduced tissue content of MMP-9 in human abdominal aortic aneurysm.8,9 Failure to influence aneurysm growth with doxycycline suggests that the role of these proteases in human disease may be different from their role in animals.
C-reactive protein levels were lower among patients who received doxycycline than among those who received placebo. The doxycycline-associated reduction in CRP occurred even though most of the patients in the current study were taking statins. Lower levels of circulating markers of inflammation have been observed with statin therapy22 and have been associated with smaller aneurysm size.23 The anti-inflammatory effects of doxycycline have been documented in vitro in cell cultures and in vivo in animal models and have been observed in treatment of periodontitis24,25 with doses lower than that used in the present study.
Reductions in levels of biomarkers of inflammation have been observed with other antibiotics, eg, azithromycin, among patients who do not have acute bacterial infections.26,27,28 Whether a doxycycline anti-inflammatory effect in older adults is of any clinical consequence is unknown.
In addition to the doxycycline-placebo comparison, this study provides information on small abdominal aortic aneurysms that is of value to clinicians and researchers. Over 2 years, maximum transverse diameters did not quickly become larger or smaller. The annual rate of growth observed is smaller than previously reported, suggesting that intervals between CT scan imaging may be lengthened. No ruptures were observed. The upper 95% CI (1.4% over a 2-year interval) of the rupture frequency in this study is less than the frequency of life-threatening complications of invasive repair—ischemic complications in approximately 9% and endograft infection in 0.4% to 3.0%.29
No pharmaceutical agent has demonstrated efficacy in reducing the rate of growth or preventing rupture of abdominal aortic aneurysms.30,31,32,33 This study found doxycycline treatment and CT scan follow-up to be feasible, but doxycycline in the dose tested in this study did not reduce the growth of small abdominal aortic aneurysms or reduce the circulating level of MMP-9, the enzyme most strongly implicated in tissue disruption in animal models. Open or endovascular repair for abdominal aortic aneurysms larger than 5.5 cm in men or 5.0 cm in women remains the only effective treatment for abdominal aortic aneurysms.
Limitations
This study has several limitations. First, follow-up was no more than 2 years for most patients and shorter for a few. It is possible that treatment effects would emerge with longer treatment and follow-up. Second, study treatment resulted in measured doxycycline levels in the lower part of the range of those found efficacious in animal models. Measurements may have underestimated peak levels because the specimens were collected without the benefit of precise timing as would be possible in a formal pharmacokinetic study. The doxycycline dose used in this study was associated with adverse events and treatment discontinuations. Larger doses are not likely to be well-tolerated over long periods. Third, the study population represented only 18% of those screened. However, the reasons patients did not agree to participate or were ineligible (other serious comorbid states, inconvenience of follow-up procedures) are not likely to be associated with aneurysm growth.
Conclusions
Among patients with small infrarenal abdominal aortic aneurysms, doxycycline compared with placebo did not significantly reduce aneurysm growth at 2 years. These findings do not support the use of doxycycline for reducing the growth of small abdominal aortic aneurysms.
Trial Protocol
Statistical Analysis Plan
eTable 1. Baseline Characteristics for Patients Not Included in the Final Analysis Plan
eAppendix 1. Sex by Treatment Interaction
eTable 2. MMP-9 and CRP Levels
eTable 3. Frequency of Expected Adverse Events
eTable 4. Doxycycline Levels
Data Sharing Plan
References
- 1.Benson RA, Poole R, Murray S, Moxey P, Loftus IM. Screening results from a large United Kingdom abdominal aortic aneurysm screening center in the context of optimizing United Kingdom National Abdominal Aortic Aneurysm Screening Programme protocols. J Vasc Surg. 2016;63(2):301-304. doi: 10.1016/j.jvs.2015.08.091 [DOI] [PubMed] [Google Scholar]
- 2.Grøndal N, Søgaard R, Lindholt JS. Baseline prevalence of abdominal aortic aneurysm, peripheral arterial disease and hypertension in men aged 65-74 years from a population screening study (VIVA trial). Br J Surg. 2015;102(8):902-906. doi: 10.1002/bjs.9825 [DOI] [PubMed] [Google Scholar]
- 3.Powell J, Sweeting MJ, Thompson MM, et al. . Endovascular or open repair strategy for ruptured abdominal aortic aneurysm: 30 day outcomes from IMPROVE randomised trial. BMJ. 2014;348:f7661. [DOI] [PubMed] [Google Scholar]
- 4.Karthikesalingam A, Vidal-Diez A, Holt PJ, et al. . Thresholds for abdominal aortic aneurysm repair in England and the United States. N Engl J Med. 2016;375(21):2051-2059. doi: 10.1056/NEJMoa1600931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Petrinec D, Liao S, Holmes DR, Reilly JM, Parks WC, Thompson RW. Doxycycline inhibition of aneurysmal degeneration in an elastase-induced rat model of abdominal aortic aneurysm: preservation of aortic elastin associated with suppressed production of 92 kD gelatinase. J Vasc Surg. 1996;23(2):336-346. doi: 10.1016/S0741-5214(96)70279-3 [DOI] [PubMed] [Google Scholar]
- 6.Curci JA, Petrinec D, Liao S, Golub LM, Thompson RW. Pharmacologic suppression of experimental abdominal aortic aneurysms: a comparison of doxycycline and four chemically modified tetracyclines. J Vasc Surg. 1998;28(6):1082-1093. doi: 10.1016/S0741-5214(98)70035-7 [DOI] [PubMed] [Google Scholar]
- 7.Prall AK, Longo GM, Mayhan WG, et al. . Doxycycline in patients with abdominal aortic aneurysms and in mice: comparison of serum levels and effect on aneurysm growth in mice. J Vasc Surg. 2002;35(5):923-929. doi: 10.1067/mva.2002.123757 [DOI] [PubMed] [Google Scholar]
- 8.Curci JA, Mao D, Bohner DG, et al. . Preoperative treatment with doxycycline reduces aortic wall expression and activation of matrix metalloproteinases in patients with abdominal aortic aneurysms. J Vasc Surg. 2000;31(2):325-342. doi: 10.1016/S0741-5214(00)90163-0 [DOI] [PubMed] [Google Scholar]
- 9.Lindeman JH, Abdul-Hussien H, van Bockel JH, Wolterbeek R, Kleemann R. Clinical trial of doxycycline for matrix metalloproteinase-9 inhibition in patients with an abdominal aneurysm: doxycycline selectively depletes aortic wall neutrophils and cytotoxic T cells. Circulation. 2009;119(16):2209-2216. [DOI] [PubMed] [Google Scholar]
- 10.Meijer CA, Stijnen T, Wasser MN, Hamming JF, van Bockel JH, Lindeman JH; Pharmaceutical Aneurysm Stabilisation Trial Study Group . Doxycycline for stabilization of abdominal aortic aneurysms: a randomized trial. Ann Intern Med. 2013;159(12):815-823. doi: 10.7326/0003-4819-159-12-201312170-00007 [DOI] [PubMed] [Google Scholar]
- 11.Mosorin M, Juvonen J, Biancari F, et al. . Use of doxycycline to decrease the growth rate of abdominal aortic aneurysms: a randomized, double-blind, placebo-controlled pilot study. J Vasc Surg. 2001;34(4):606-610. doi: 10.1067/mva.2001.117891 [DOI] [PubMed] [Google Scholar]
- 12.Lederle FA. Abdominal aortic aneurysm: still no pill. Ann Intern Med. 2013;159(12):852-853. doi: 10.7326/0003-4819-159-12-201312170-00012 [DOI] [PubMed] [Google Scholar]
- 13.Baxter BT, Matsumura J, Curci J, et al. ; N-TA(3)CT Investigators . Non-invasive Treatment of Abdominal Aortic Aneurysm Clinical Trial (N-TA(3)CT): design of a phase IIb, placebo-controlled, double-blind, randomized clinical trial of doxycycline for the reduction of growth of small abdominal aortic aneurysm. Contemp Clin Trials. 2016;48(1):91-98. doi: 10.1016/j.cct.2016.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ludbrook J. Should we use one-sided or two-sided P values in tests of significance? Clin Exp Pharmacol Physiol. 2013;40(6):357-361. doi: 10.1111/1440-1681.12086 [DOI] [PubMed] [Google Scholar]
- 15.Lederle FA, Noorbaloochi S, Nugent S, et al. . Multicentre study of abdominal aortic aneurysm measurement and enlargement. Br J Surg. 2015;102(12):1480-1487. doi: 10.1002/bjs.9895 [DOI] [PubMed] [Google Scholar]
- 16.Rubin DB. Multiple Imputation for Non-Response in Surveys. Wiley; 1987. doi: 10.1002/9780470316696 [DOI] [Google Scholar]
- 17.Rubin DB. Inference and missing data. Biometrika. 1976;63:581-592. doi: 10.1093/biomet/63.3.581 [DOI] [Google Scholar]
- 18.Barnard J, Rubin DB. Small sample degrees of freedom with multiple imputation. Biometrika. 1999;86:948-955. doi: 10.1093/biomet/86.4.948 [DOI] [Google Scholar]
- 19.Lachin JM. A review of methods for futility stopping based on conditional power. Stat Med. 2005;24(18):2747-2764. doi: 10.1002/sim.2151 [DOI] [PubMed] [Google Scholar]
- 20.Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73(1):13-22. doi: 10.1093/biomet/73.1.13 [DOI] [Google Scholar]
- 21.Bouvet C, Moreau S, Blanchette J, de Blois D, Moreau P. Sequential activation of matrix metalloproteinase 9 and transforming growth factor beta in arterial elastocalcinosis. Arterioscler Thromb Vasc Biol. 2008;28(5):856-862. doi: 10.1161/ATVBAHA.107.153056 [DOI] [PubMed] [Google Scholar]
- 22.Muehling BM, Paintner A, Marx N, Barth TF, Babiak C, Orend KH. In vivo study on the expression pattern of resistin in patients with abdominal aortic aneurysm. Vasc Endovascular Surg. 2011;45(1):63-68. doi: 10.1177/1538574410380935 [DOI] [PubMed] [Google Scholar]
- 23.Stather PW, Sidloff DA, Dattani N, et al. . Meta-analysis and meta-regression analysis of biomarkers for abdominal aortic aneurysm. Br J Surg. 2014;101(11):1358-1372. doi: 10.1002/bjs.9593 [DOI] [PubMed] [Google Scholar]
- 24.Payne JB, Golub LM, Stoner JA, et al. . The effect of subantimicrobial-dose-doxycycline periodontal therapy on serum biomarkers of systemic inflammation: a randomized, double-masked, placebo-controlled clinical trial. J Am Dent Assoc. 2011;142(3):262-273. doi: 10.14219/jada.archive.2011.0165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tüter G, Kurtiş B, Serdar M, et al. . Effects of scaling and root planing and sub-antimicrobial dose doxycycline on oral and systemic biomarkers of disease in patients with both chronic periodontitis and coronary artery disease. J Clin Periodontol. 2007;34(8):673-681. doi: 10.1111/j.1600-051X.2007.01104.x [DOI] [PubMed] [Google Scholar]
- 26.Cramer CL, Patterson A, Alchakaki A, Soubani AO. Immunomodulatory indications of azithromycin in respiratory disease: a concise review for the clinician. Postgrad Med. 2017;129(5):493-499. doi: 10.1080/00325481.2017.1285677 [DOI] [PubMed] [Google Scholar]
- 27.Parnham MJ, Erakovic Haber V, Giamarellos-Bourboulis EJ, Perletti G, Verleden GM, Vos R. Azithromycin: mechanisms of action and their relevance for clinical applications. Pharmacol Ther. 2014;143(2):225-245. doi: 10.1016/j.pharmthera.2014.03.003 [DOI] [PubMed] [Google Scholar]
- 28.Kobayashi Y, Wada H, Rossios C, et al. . A novel macrolide solithromycin exerts superior anti-inflammatory effect via NF-κB inhibition. J Pharmacol Exp Ther. 2013;345(1):76-84. doi: 10.1124/jpet.112.200733 [DOI] [PubMed] [Google Scholar]
- 29.Daye D, Walker TG. Complications of endovascular aneurysm repair of the thoracic and abdominal aorta: evaluation and management. Cardiovasc Diagn Ther. 2018;8(suppl 1):S138-S156. doi: 10.21037/cdt.2017.09.17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bicknell CD, Kiru G, Falaschetti E, Powell JT, Poulter NR; AARDVARK Collaborators . An evaluation of the effect of an angiotensin-converting enzyme inhibitor on the growth rate of small abdominal aortic aneurysms: a randomized placebo-controlled trial (AARDVARK). Eur Heart J. 2016;37(42):3213-3221. doi: 10.1093/eurheartj/ehw257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sillesen H, Eldrup N, Hultgren R, et al. ; AORTA Trial Investigators . Randomized clinical trial of mast cell inhibition in patients with a medium-sized abdominal aortic aneurysm. Br J Surg. 2015;102(8):894-901. doi: 10.1002/bjs.9824 [DOI] [PubMed] [Google Scholar]
- 32.Propanolol Aneurysm Trial Investigators Propranolol for small abdominal aortic aneurysms: results of a randomized trial. J Vasc Surg. 2002;35(1):72-79. doi: 10.1067/mva.2002.121308 [DOI] [PubMed] [Google Scholar]
- 33.Pinchbeck JL, Moxon JV, Rowbotham SE, et al. . Randomized placebo-controlled trial assessing the effect of 24-week fenofibrate therapy on circulating markers of abdominal aortic aneurysm: outcomes from the FAME-2 Trial. J Am Heart Assoc. 2018;7(19):e009866. doi: 10.1161/JAHA.118.009866 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol
Statistical Analysis Plan
eTable 1. Baseline Characteristics for Patients Not Included in the Final Analysis Plan
eAppendix 1. Sex by Treatment Interaction
eTable 2. MMP-9 and CRP Levels
eTable 3. Frequency of Expected Adverse Events
eTable 4. Doxycycline Levels
Data Sharing Plan