Abstract
This study describes the growth of telestroke capacity in US hospitals and compares the characteristics of the hospitals with and without telestroke capacity.
Reperfusion via intravenous alteplase or mechanical thrombectomy reduces the damage of an acute ischemic stroke, but these treatments must be administered within a narrow time frame after onset of symptoms and not all patients can safely receive reperfusion. Larger hospitals typically have on-call stroke teams that quickly assess patients with suspected stroke; patients receiving care at hospitals without this expertise may be less likely to receive appropriate treatment.1 Telestroke has emerged as a potential solution by which remote stroke experts guide local emergency physicians through the neurological examination, review of imaging, and management decisions.1
Limited evidence exists on the prevalence of telestroke capacity in hospitals.2,3 There is no comprehensive survey of when hospitals introduced their telestroke programs, and the use of telestroke cannot be reliably identified in insurance claims.4 We describe the growth of telestroke capacity in US hospitals and compare the characteristics of the hospitals with and without telestroke capacity.
Methods
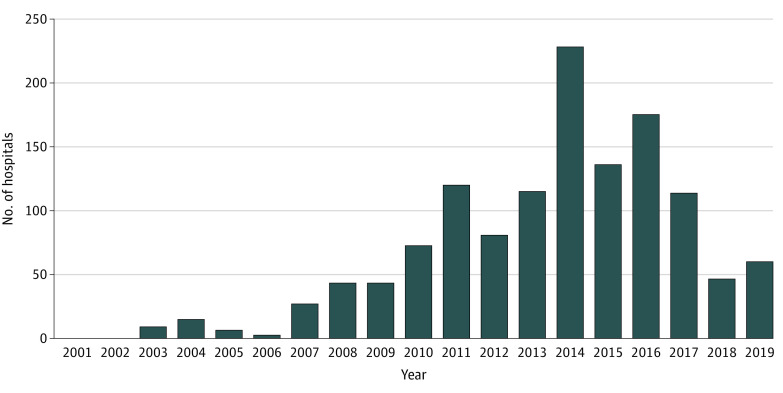
In consultation with stroke experts about existing telestroke programs in the US and review of the literature, we identified and contacted 15 health care systems and private companies with known telestroke capacity (Figure). All agreed to participate and provided the names and contract start dates of hospitals in their networks on the requesting end of telestroke consults (spoke hospitals). This is a convenience sample and does not capture all telestroke sites and most likely underrepresents smaller networks. Harvard Medical School waived insitutional review board approval for this study because the study did not involve human subjects data.
Figure. Number of Hospitals in the US Incorporating Telestroke by Year, 2001-2019 (N = 1306).
Free-standing emergency departments with telestroke capacity were linked to their affiliated hospital. The 15 organizations contributing data are Blue Sky Neurology, Integris, InTouch, Mayo Clinic, Medical University of South Carolina, Northwestern Memorial Hospital, Partners HealthCare, Providence Health, SOC Telemed (formerly Specialists on Call), Stanford Health Care, University of Pittsburg Medical Center, University of Utah Hospital, Vanderbilt University Medical Center, Virginia Mason, and Wake Forest Baptist Health. These networks may provide telestroke services to hospitals across several states.
Our sample included all short-term acute care hospitals and critical access hospitals open in 2017 (using most recent data available) with at least 1 stroke hospitalization in Medicare fee-for-service data. We linked our list of hospitals with telestroke capacity to this list using hospital name and city.
We described telestroke uptake from January 2001 to December 2019 and then compared characteristics of hospitals with telestroke capacity by 2019 vs those without via χ2 tests. Hospital characteristics came from 2017 Medicare data for hospital rural/urban status, census region, and bed count, 2016 Centers for Disease Control and Prevention data for neurologists per capita ratio by hospital county, and 2017 American Hospital Association survey data for all other characteristics (Table). P values were 2-sided, and the signifiance threshold was .05.
Table. Characteristics of Hospitals With and Without Telestroke Capacity by 2019.
| Hospital characteristic | Telestroke capacity, No. (%) | P valuea | |
|---|---|---|---|
| Yes | No | ||
| Census region | |||
| Northeast | 170 (28.8) | 421 (71.2) | <.001 |
| Midwest | 270 (19.2) | 1139 (80.8) | |
| South | 530 (29.4) | 1270 (70.6) | |
| West | 336 (35.3) | 615 (64.7) | |
| Location of hospital | |||
| Urban | 856 (30.2) | 1979 (69.8) | <.001 |
| Rural | 450 (23.5) | 1466 (76.5) | |
| Teaching hospitalb | |||
| Yes | 51 (20.1) | 203 (79.9) | .01 |
| No | 1254 (27.9) | 3242 (72.1) | |
| No. of beds (quartile) | |||
| 0-25 (first) | 201 (14.8) | 1154 (85.2) | <.001 |
| 26-72 (second) | 167 (22.2) | 586 (77.8) | |
| 73-186 (third) | 415 (38.4) | 666 (61.6) | |
| >187 (fourth) | 523 (33.5) | 1039 (66.5) | |
| Hospital type | |||
| Short-term acute care hospital | 1077 (31.7) | 2323 (68.3) | <.001 |
| Critical-access hospital | 229 (17.0) | 1122 (83.0) | |
| Ownership | |||
| For profit | 303 (37.1) | 514 (62.9) | <.001 |
| Nonprofit | 780 (28.2) | 1984 (71.8) | |
| Government | 194 (19.3) | 809 (80.7) | |
| NAc | 29 (17.4) | 138 (82.6) | |
| Intensive care unit in hospital | |||
| Yes | 843 (33.5) | 1672 (66.5) | <.001 |
| No | 434 (21.0) | 1635 (79.0) | |
| NAc | 29 (17.4) | 138 (82.6) | |
| Neurologists per 100 000 people in county | |||
| <2 | 194 (38.3) | 312 (61.7) | <.001 |
| 2-4.9 | 382 (34.7) | 720 (65.3) | |
| 5-9.9 | 257 (26.7) | 707 (73.3) | |
| >10 | 91 (22.1) | 320 (77.9) | |
| NAc | 382 (21.6) | 1386 (78.4) | |
Abbreviation: NA, not applicable.
Based on χ2 test.
Defined as a major member of the Council of Teaching Hospitals.
Hospitals did not respond to question on American Hospital Association survey or county data was reported to be insufficient by Centers for Disease Control and Prevention’s Interactive Atlas of Heart Disease and Stroke.
Results
By 2019, 1306 of 4751 hospitals (27.4%) had telestroke capacity. Uptake grew slowly and peaked in 2014 (Figure). Of hospitals open in 2017, hospitals with telestroke capacity were larger (523 [33.5%] in the highest quartile with telestroke capacity vs 201 [14.8%] in the lowest; P < .001; χ2 = 212.1), more likely to be short-term acute care hospitals (1077 [31.7%] vs 229 [17.0%] of critical-access hospitals; P < .001; χ2 = 105.2), and in urban areas (856 [30.2%] vs 450 [23.5%] rural; P < .001; χ2 = 25.8). They were also more likely to be in the West, in counties with fewer neurologists per capita, have for-profit ownership, and have intensive care units (Table).
Discussion
In one of the first national compilations of telestroke capacity to our knowledge, we found that approximately a quarter of hospitals now have access to this technology for patients in their emergency departments. Given that telestroke capacity is associated with greater use of reperfusion,5 the growing use of telestroke in the US hopefully leads to more reperfusion and improved outcomes.
Smaller, rural, and critical access hospitals, the group of hospitals that might benefit most from telestroke,6 are relatively less likely to have adopted this technology. It is unclear what barriers these hospitals face in introducing telestroke capacity. Potential barriers include lack of capital investment, lack of high-speed internet in rural communities, and regulatory barriers (eg, Stark Laws limit the material support that can be provided to referring hospitals).
The key limitation to this research is that our sample of telestroke networks was identified primarily through consultations with experts and as such may overrepresent larger systems of care anchored by teaching hospitals or using private telestroke companies.
References
- 1.Wechsler LR, Tsao JW, Levine SR, et al. ; American Academy of Neurology Telemedicine Work Group . Teleneurology applications: report of the Telemedicine Work Group of the American Academy of Neurology. Neurology. 2013;80(7):670-676. doi: 10.1212/WNL.0b013e3182823361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Silva GS, Farrell S, Shandra E, Viswanathan A, Schwamm LH. The status of telestroke in the United States: a survey of currently active stroke telemedicine programs. Stroke. 2012;43(8):2078-2085. doi: 10.1161/STROKEAHA.111.645861 [DOI] [PubMed] [Google Scholar]
- 3.Zachrison KS, Boggs KM, M Hayden E, Espinola JA, Camargo CA. A national survey of telemedicine use by US emergency departments. J Telemed Telecare. Published online December 17, 2018. doi: 10.1177/1357633X18816112 [DOI] [PubMed] [Google Scholar]
- 4.Zhang D, Wang G, Zhu W, et al. Expansion of telestroke services improves quality of care provided in super rural areas. Health Aff (Millwood). 2018;37(12):2005-2013. doi: 10.1377/hlthaff.2018.05089 [DOI] [PubMed] [Google Scholar]
- 5.Müller-Barna P, Schwamm LH, Haberl RL. Telestroke increases use of acute stroke therapy. Curr Opin Neurol. 2012;25(1):5-10. doi: 10.1097/WCO.0b013e32834d5fe4 [DOI] [PubMed] [Google Scholar]
- 6.Lichtman JH, Leifheit-Limson EC, Jones SB, Wang Y, Goldstein LB. 30-Day risk-standardized mortality and readmission rates after ischemic stroke in critical access hospitals. Stroke. 2012;43(10):2741-2747. doi: 10.1161/STROKEAHA.112.665646 [DOI] [PMC free article] [PubMed] [Google Scholar]