This systematic review and meta-analysis examines whether preterm and term-born neonates with intrauterine growth restriction who are small for gestational age have worse childhood cognitive outcomes than those born appropriate for gestational age.
Key Points
Question
Do preterm and term-born neonates with intrauterine growth restriction and small for gestational age have worse childhood cognitive outcomes than those born appropriate for gestational age?
Findings
In this systematic review and meta-analysis of 89 samples from 60 studies including 52 822 children (aged 1-12 years), compared with children born appropriate for gestational age, children who had intrauterine growth restriction and who were small for gestational age had significantly lower cognitive scores.
Meaning
The findings suggest that preventive strategies should be directed to pregnancies and deliveries of fetuses and neonates with intrauterine growth restriction and that pediatric follow-up care should be tailored to address the potential cognitive problems in children who were born with intrauterine growth restriction and were small for gestational age.
Abstract
Importance
The magnitude of the association of intrauterine growth restriction (IUGR) and small for gestational age (SGA) status with cognitive outcomes in preterm and term-born children has not been established.
Objective
To examine cognitive outcomes of preterm and term-born children who had IUGR and were SGA compared with children who were appropriate for gestational age (AGA) during the first 12 years of life.
Data Sources
For this systematic review and meta-analysis, the Scopus, PubMed, Web of Science, Science Direct, PsycInfo, and ERIC databases were searched for English-language, peer-reviewed literature published between January 1, 2000, and February 20, 2020. The following Medical Subject Heading terms for IUGR and SGA and cognitive outcomes were used: intrauterine growth restriction, intrauterine growth retardation, small for gestational age AND neurodevelopment, neurodevelopmental outcome, developmental outcomes, and cognitive development.
Study Selection
Inclusion criteria were assessment of cognitive outcomes (full-scale IQ or a cognitive subscale), inclusion of an AGA group as comparison group, and inclusion of gestational age at birth and completion of cognitive assessment up to 12 years of age.
Data Extraction and Synthesis
The Meta-analysis of Observational Studies in Epidemiology (MOOSE) reporting guidelines were followed. Data were double screened for full-text articles, and a subset were independently coded by 2 authors. Standardized mean differences (SMDs) and odd ratios from individual studies were pooled by applying random-effects models.
Main Outcomes and Measures
Cognitive outcomes, defined as mental, cognitive, or IQ scores, estimated with standardized practitioner-based cognitive tests or as borderline intellectual impairment (BII), defined as mental, cognitive, or IQ scores at least 1 SD below the mean cognitive score.
Results
In this study of 89 samples from 60 studies including 52 822 children, children who had IUGR and were SGA had significantly poorer cognitive outcomes (eg, cognitive scores and BII) than children with AGA in childhood. For cognitive scores, associations are consistent for preterm (SMD, −0.27; 95% CI, −0.38 to −0.17) and term-born children (SMD, −0.39; 95% CI, −0.50 to −0.28), with higher effect sizes reported for term-born IUGR and AGA group comparisons (SMD, –0.58; 95% CI, –0.82 to –0.35). Analyses on BII revealed a significantly increased risk in the preterm children who had IUGR and were SGA (odds ratio, 1.57; 95% CI, 1.40-1.77) compared with the children with AGA.
Conclusions and Relevance
Growth vulnerabilities assessed antenatally (IUGR) and at the time of birth (SGA) are significantly associated with lower childhood cognitive outcomes in preterm and term-born children compared with children with AGA. These findings highlight the need to develop interventions that boost cognitive functions in these high-risk groups.
Introduction
Intrauterine growth restriction (IUGR) is an abnormal fetal growth pattern that occurs in approximately 8% to 10% of pregnancies1 and is associated with neonatal morbidity and mortality.2 IUGR refers to an impoverished fetal growth with fetal, maternal, or placental causes (ie, congenital or chromosomal anomalies, infections, and vascular disorders) of a detrimental cascade in which oxygen reduction (up to hypoxemia) and nutritional deficiencies lead to cardiovascular deterioration, extreme blood flow resistance, and decreased fetal growth rate.3 In pregnancies in which IUGR occurs, the fetus attempts to prevent damage by slowing its growth and shortening its gestation4; however, the adaptive responses to cope with in utero malnutrition have long-lasting consequences associated with adverse developmental and health-related outcomes throughout life.5
Individuals who had IUGR experience a range of poorer developmental outcomes, encompassing cognitive, socioemotional, and behavioral domains, compared with individuals who were born appropriate for gestational age (AGA).6 Regarding cognitive outcomes, gold standard measures include IQ, mental quotient, and cognitive developmental quotient, which are all concise indicators of general cognitive functioning. Previous systematic reviews and meta-analyses5,7 have investigated the association between IUGR and such cognitive outcomes. However, some key issues remain undefined, such as potential differences between preterm and term-born children who had IUGR and between children who had IUGR and those who were small for gestational age (SGA). In most cases, fetuses IUGR are delivered SGA, a neonatal classification that describes newborns with birth weight below the 10th percentile for gestational age.8 Despite the high comorbidity between SGA and IUGR, it is important to define and differentiate between the 2 conditions. IUGR reflects fetal distress, whereas SGA only provides a measure of size and not a direct measure of antenatal growth quality. That is, SGA status is not sufficient to identify antenatal growth restriction; children who were SGA are usually described as former constitutionally small fetuses.9 Postnatal differentiation between IUGR and SGA can be arduous, and several antenatal factors (eg, umbilical artery Doppler assessment) have been proposed to increase accuracy in antenatal diagnosis. Despite this, SGA could represent a delayed or attenuated subtype of IUGR or even a different kind of antenatal environmental alteration; therefore, a pathological origin of SGA cannot be excluded.10
An important variable to consider when studying IUGR and SGA development is preterm birth (<37 gestational weeks), which can occur in both conditions. It is still unclear whether the intrauterine environment offers a better long-term outcome for the growth-restricted infant than an early exposure to the extrauterine environment.11 Consequently, preterm birth interacts with the potential association of antenatal growth restriction with child development and represents a major confounding factor when studying IUGR and SGA outcomes.
This meta-analysis investigates the association between in utero IUGR or SGA birth and childhood cognitive outcomes. The primary aim was to evaluate whether individuals who had IUGR and were SGA have significantly lower cognitive scores compared with individuals who were AGA, examining those born preterm and at term separately. The secondary aim was to compare the risk of borderline intellectual impairment (BII), defined as a cognitive score at least 1 SD below the mean cognitive score between children who had IUGR and were SGA and children with AGA. This study highlights the importance of accounting for antenatal and perinatal risk factors of childhood sequelae when fostering interventions and guiding professionals in parent counseling in the neonatal period and beyond with regular clinical follow-up visits. In addition, identifying the association among IUGR, SGA, and cognitive outcomes could guide further studies to explore their potential underpinning mechanisms (ie, neurophysiological and socioemotional).
Methods
This systematic review and meta-analysis was conducted following the Meta-analysis of Observational Studies in Epidemiology (MOOSE) reporting guidelines. Multiple methods were used to identify eligible studies. Literature searches were conducted using the following databases: Scopus, PubMed, Web of Science, Science Direct, PsycInfo, and ERIC. Medical Subject Heading terms for IUGR and SGA as well as cognitive outcomes were used as keywords: intrauterine growth restriction, intrauterine growth retardation, small for gestational age AND neurodevelopment, neurodevelopmental outcome, developmental outcomes, and cognitive development. The last screening was performed on February 20, 2020. Research was limited to studies published after January 2000 as a proxy of data collection within the antenatal corticosteroid and surfactant era. Eligibility was limited to peer-reviewed scientific articles published in the English language. Review articles, conference proceedings, book chapters, thesis dissertations, case reports, and all non–English-language materials were excluded. In addition, the reference sections of previous systematic reviews on this topic were searched for relevant references.
Study Selection
Inclusion criteria were defined as follows. First, target samples consisted of children who had IUGR and were SGA. IUGR studies were included if they reported antenatal evidence of growth restriction, whereas SGA studies were selected if they referred to birth weight below the 10th to 15th centile for gestational age. Antenatal assessment and birth weight cutoffs varied across studies and are reported in eTables 1 to 3 in the Supplement. The second criterion was the presence of a comparison group of individuals born AGA, defined as a mean birth weight greater than the 10th to 15th centile for gestational age, and matched for age at delivery in the 2 groups of preterm and term-born children. Third, articles included gestational age at birth (ie, mixed samples of preterm and term-born children were excluded). Fourth, cognitive outcome was based on mean cognitive score (ie, mental or cognitive standardized assessment score or full-scale IQ) or BII, defined as the percentage of children scoring at least less than 1 SD of the mean on a cognitive measure or full-scale IQ. Fifth, cognitive outcome assessment was based on a standardized practitioner-based test. Sixth, age at outcome assessment was up to 12 years (age range, 1 month to 11.11 years).
Data Management
All studies were double screened by 2 researchers, including one of us (C.S.), for inclusion, and selected studies were coded by 1 of us (C.S.), recording authors and year of publication, sample size, national setting, sample characteristics (diagnosis, age at outcome, and type of cognitive outcome measure), and data to compute the effect sizes. A subset of studies (40 [53%]) were independently coded (C.M.); interrater reliability was 90%. In the rare cases (n = 4) of disagreement among coders on values to be extracted, possible discrepancies were discussed until agreement was met. In case of eligible articles not reporting information necessary to compute effect size, corresponding authors were contacted to provide the missing information. Requested data were received for 1 of 12 requests.
Data are organized according to time of diagnosis (in utero IUGR vs at birth SGA) and mean gestational age at birth (preterm vs term-born). Gestational age at birth is presented as the number of completed gestational weeks. Preterm birth was classified as gestational age at delivery younger than 37 weeks. When studies considered preterm and term-born children, only those including less than 30% of children born at less than 37 weeks of gestation were included in the term subgroup. Likewise, 1 study12 that considered preterm children involved 23% of children born at 37 or more weeks of gestation and was therefore included in the analysis.
Studies are grouped on the basis of outcome: findings are analyzed separately for mean cognitive scores and percentage of BII. To avoid sample overrepresentation, when the same cohort was followed up at multiple time points, only the study that included the largest number of participants was included in this meta-analysis. Studies that reported cognitive scores and BII were included in the meta-analyses, and the different types of data were analyzed separately.
Statistical Analysis
Two separate meta-analyses were conducted on (1) studies that reported mean cognitive scores for each group (effect size was computed as standardized mean difference [SMD] for heteroscedastic population variances13,14) and (2) studies that reported the percentage of children with BII (effect size was computed as odds ratio [OR]: the odds for the IUGR and SGA groups over the odds for the AGA group). Throughout the study, the term cognitive scores refers to data on the mean cognitive score comparisons; BII refers to group comparison on ORs. The target group was then compared with its relative AGA group (ie, preterm IUGR vs preterm AGA and term-born IUGR vs term-born AGA).
Data from individual studies were pooled by applying random-effects models. Potential publication bias was evaluated in different ways. First, we tested for funnel plot asymmetry.15 Second, we checked whether additional studies needed to be imputed according to the Duval and Tweedie trim and fill method.16,17 Heterogeneity was assessed with Q statistics (which is distributed as χ2 with df = k − 1, where k represents the number of effect sizes), with a significant P value representing heterogeneity18; the I2 statistic is also reported, indicating the proportion of observed variance that reflects real differences in effect size.19 Analyses were performed in IUGR preterm, IUGR term, SGA preterm, and SGA term groups separately. When heterogeneity was observed in the data, we tested moderating effects by applying mixed-effects models: gestational age at delivery, IUGR vs SGA classification, and mean age at outcome assessment were used as covariates. Within each meta-analysis (preterm and term-born groups), subgroup meta-analyses were also conducted on IUGR and SGA subsamples. In addition, within the meta-analysis on BII (cognitive score <1 SD), subgroup analysis was performed including the subset of studies that reported rates of children with cognitive scores 2 SDs below the mean cognitive score, which are regarded as reflecting intellectual impairment.20
Overall, to test for the robustness of the observed association, supplemental analyses were performed repeating the primary meta-analyses in the subsets of studies with prospective design only, as a reflection of a good quality of study design (eResults in the Supplement).
Data analyses were performed using the software R (R Project for Statistical Computing)21; library compute.es was used to compute effect sizes, library metafor was used to run meta-analyses, and library forestplot was used to graphically represent findings. Two-tailed P values were used for random-effects and mixed-effects meta-analyses; 1-tailed P values were used for Q statistics. P < .05 was considered statistically significant.
Results
Study Sample
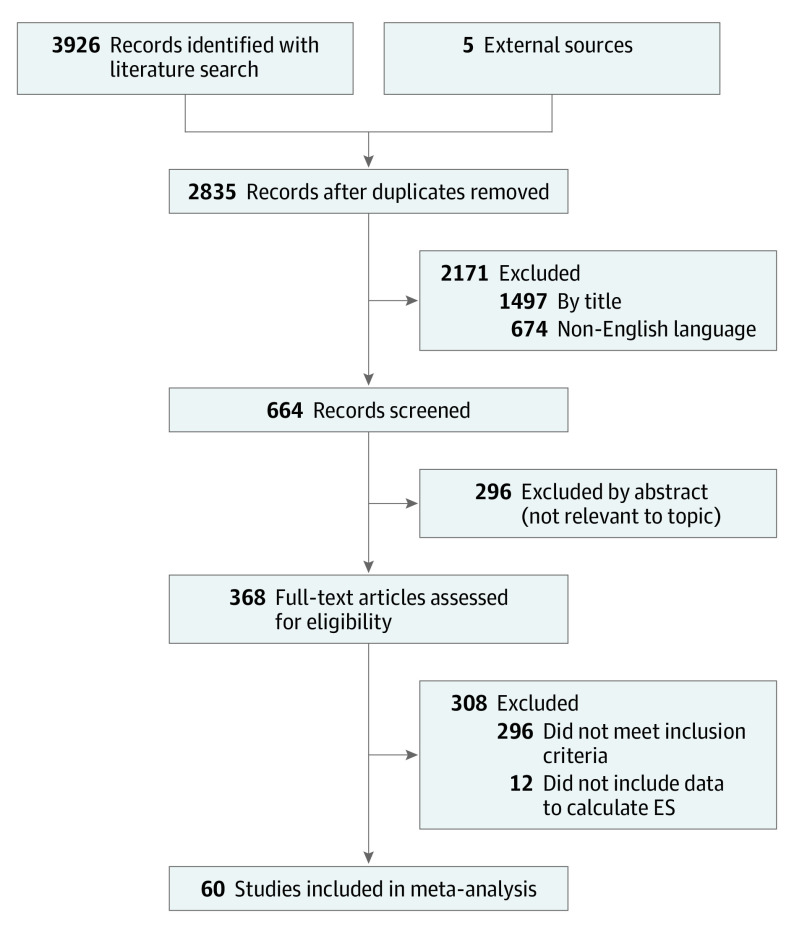
Results of the search process are provided in Figure 1. In total, 89 samples from 60 studies including 52 822 children compared preterm and term-born children who had IUGR and were SGA with children with AGA with respect to cognitive outcomes. A total of 48 studies12,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68 reported results for mean cognitive scores, and 24 studies reported the percentages of group-specific children with BII.12,23,28,31,34,38,39,41,45,46,50,69,70,71,72,73,74,75,76,77,78,79,80
Figure 1. Flow Diagram of Study Inclusion.
ES indicates effect size.
Cognitive Scores in Preterm Children Who Had IUGR and Were SGA
In total, 30 studies provided the 34 participant samples included in the analysis and reported data for 1352 preterm children who had IUGR and were SGA (mean [SD] birth weight, 989.20 [283.00] g; mean [SD] gestational age, 30.52 [2.83] weeks). Fifteen samples included an antenatal IUGR diagnosis, whereas 19 included children with SGA diagnosed at birth (eTable 1 in the Supplement). Preterm children who had IUGR and were SGA had significantly lower cognitive scores compared with those born AGA (SMD [SE], −0.27 [0.05]; 95% CI, −0.38 to −0.17; z = −5.20; P < .001). Figure 2 shows the forest plot of this meta-analysis, with IUGR and SGA subgroups shown separately (95% CIs overlapped indicating no significant differences). No funnel plot asymmetry was observed (t32 = −0.86, P = .40). However, the trim and fill method16,17 suggested the imputation of 3 additional studies on the right side (eFigure 1 in the Supplement). Test for homogeneity among studies showed heterogeneity (Q33 = 62.53, P = .001, I2 = 48.08%). Therefore, moderating effects were tested. Cognitive scores were lower in target groups (IUGR and SGA) compared with the AGA group (t32 = 1.40, P = .26) regardless of gestational age at delivery (F1,30 = 0.18, P = .67) and age at outcome (F1,32 = 0.40, P = .53).
Figure 2. Forest Plot for Cognitive Scores in Preterm Individuals Who Had Intrauterine Growth Restriction (IUGR) and Were Small for Gestational Age (SGA).
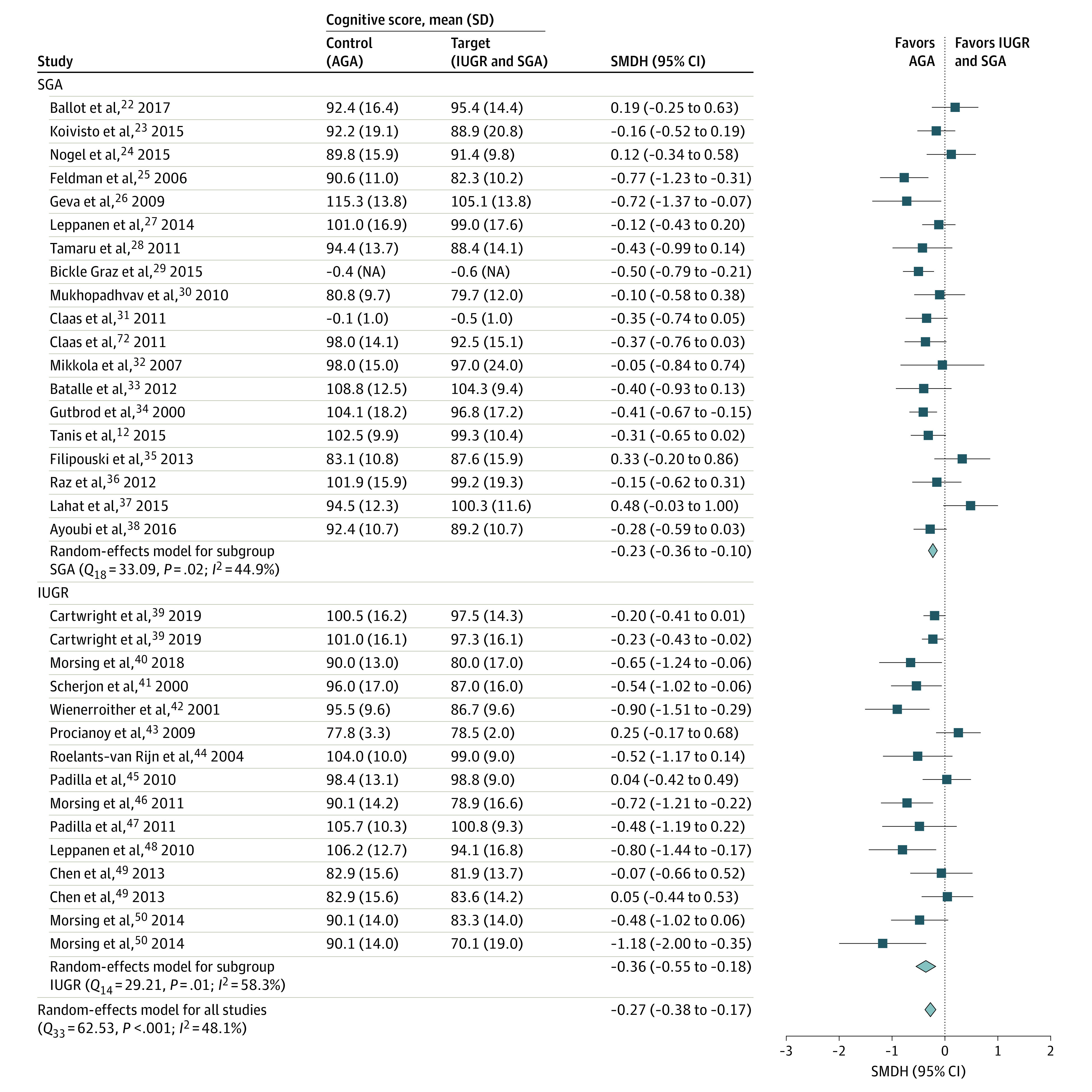
Forest plot for random-effects meta-analysis of the association between preterm IUGR and SGA and childhood cognitive scores. Effect size is expressed as the standardized mean difference for heteroscedastic population variances (SMDH). Squares indicate estimates, with the size of the square being proportional to the study's weight in the analysis. AGA indicates appropriate for gestational age; NA, not applicable.
Cognitive Scores in Term-Born Children Who Had IUGR and Were SGA
Overall, 19 studies provided data for 24 samples. A total of 2230 term-born children who had IUGR or were SGA were included in the analyses (mean [SD] birth weight, 2325.39 [323.48] g; mean [SD] gestational age, 38.24 [0.93] weeks). Five studies included antenatal IUGR diagnosis, whereas 14 studies included children diagnosed with SGA at birth (eTable 2 in the Supplement). Term-born children who had IUGR and were SGA had significantly lower cognitive scores compared with the children with AGA (SMD [SE], −0.39 [0.06]; 95% CI, −0.50 to −0.28; z = −7.07; P < .001). Figure 3 shows a forest plot of this meta-analysis with overall and subgroup (IUGR and SGA) estimates. No funnel plot asymmetry was observed (t22 = 1.06, P = .30). The trim and fill method16,17 did not suggest the imputation of additional studies. Test for homogeneity among studies showed heterogeneity (Q23 = 63.18, P < .001, I2 = 67.63%). However, IUGR vs SGA classification did not play a moderating role in accounting for heterogeneity in effect size (t24 = 3.74, P = .05). Age at outcome assessment did not significantly moderate the association between IUGR and SGA and cognitive scores (F1,22 = 0.92, P = .35).
Figure 3. Forest Plot for Cognitive Scores in Term-Born Individuals Who Had Intrauterine Growth Restriction (IUGR) and Were Small for Gestational Age (SGA).
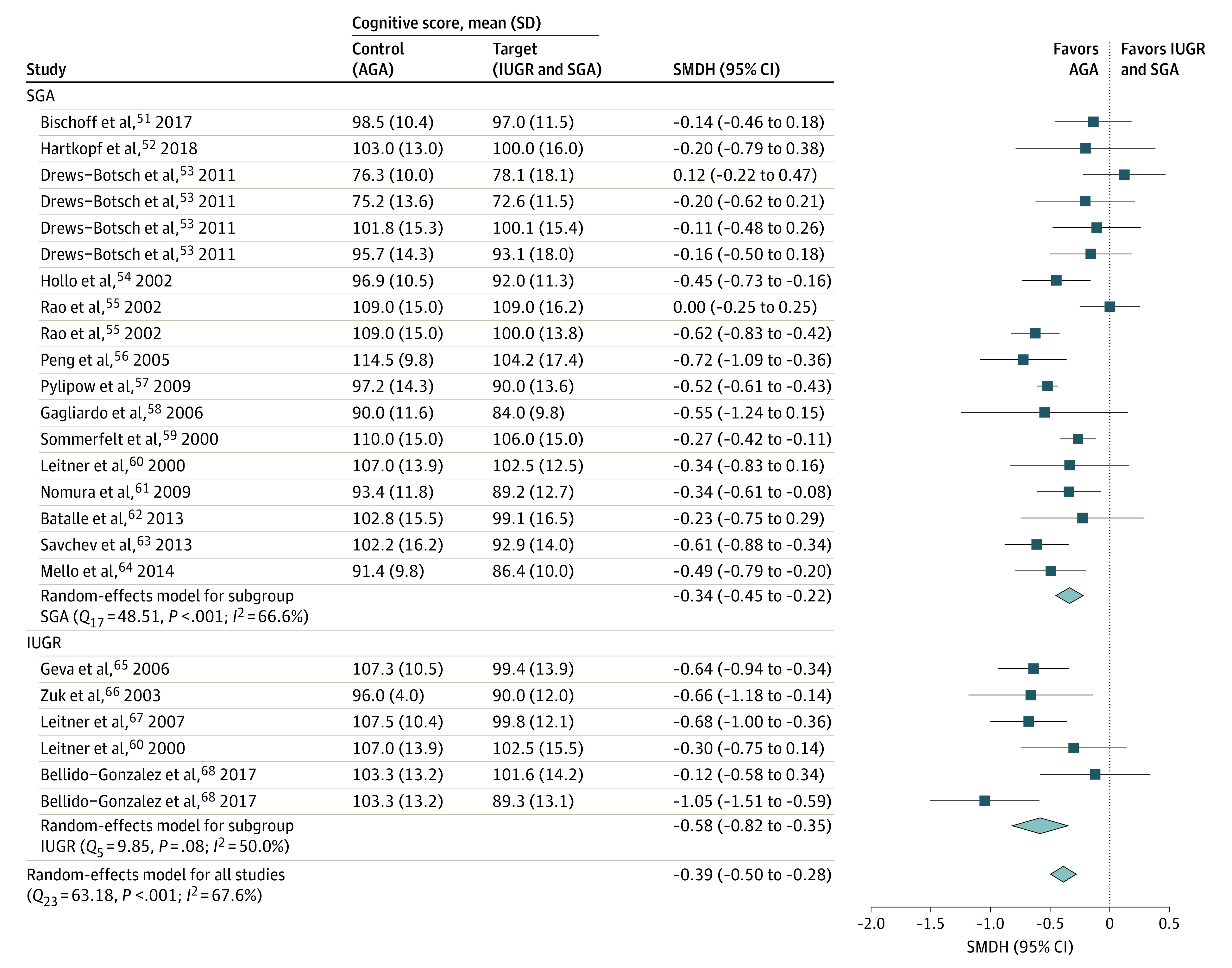
Forest plot for random-effects meta-analysis of the association between term-born IUGR and SGA and childhood cognitive scores. Effect size is expressed as the standardized mean difference for heteroscedastic population variances (SMDH). Squares indicate estimates, with the size of the square being proportional to the study's weight in the analysis. AGA indicates appropriate for gestational age.
BII in Children Who Had IUGR and Were SGA
Only 2 studies56,81 included term-born children with SGA, who had a significantly higher risk of BII compared with children with AGA (OR, 1.75; 95% CI, 1.50-2.04). Of the 24 studies conducted on preterm samples, 7 included antenatal IUGR diagnoses and 17 included children with former SGA. Characteristics of these studies are summarized in eTable 3 in the Supplement. In total, 2202 children (615 who had IUGR and 1587 with SGA) with a mean (SD) birth weight of 979.32 (349.60) g and a mean (SD) gestational age of 29.74 (2.79) weeks were assessed. Preterm children who had IUGR and were SGA were more likely to have BII than preterm children with AGA (OR, 1.57; 95% CI, 1.40-1.77; z = 7.64; P < .001). Figure 4 shows the forest plot of this meta-analysis, with IUGR and SGA subgroups also shown separately. Funnel plot asymmetry was observed through the Egger regression test (t29 = 2.38, P = .02). The Duval and Tweedy trim and fill method16,17 suggested the imputation of 5 additional studies on the left side of the funnel plot (eFigure 2 in the Supplement).
Figure 4. Forest Plot for Borderline Intellectual Impairment (BII) in Children Who Had Intrauterine Growth Restriction (IUGR) and Were Small for Gestational Age (SGA).
Forest plot for random-effects meta-analysis of the association between IUGR and SGA and childhood BII. Effect size is expressed as the odds ratio. Squares indicate estimates, with the size of the square being proportional to the study's weight in the analysis. AGA indicates appropriate for gestational age.
Test for homogeneity among studies found no heterogeneity (Q30 = 39.63, P = .11, I2 = 0%). Subgroup meta-analysis on studies presenting data on cognitive scores less than 2 SDs revealed that preterm children who had IUGR and were SGA were more likely to display intellectual impairment compared with preterm children with AGA (OR, 2.77; 95% CI, 1.28-6.00; z = 2.60; P = .009).
Discussion
The present meta-analyses found poorer cognitive function during the first 12 years of life in children who had IUGR and were SGA compared with the children with AGA matched for gestational age. Such findings were observed in preterm and term-born individuals at various ages at outcome assessment and in terms of outcome measured (cognitive scores and BII).
When considering preterm children, those who had IUGR and were SGA had significantly lower cognitive scores compared with those with AGA, with an overall small mean effect size. Preterm birth is a major perinatal risk factor for neurodevelopment,82 and the literature highlights heterogeneity in developmental outcomes of preterm children, emphasizing the need for a stratification based on differential developmental trajectories. Our findings suggest that IUGR and SGA are associated with a small additional risk to that associated with preterm birth alone. Preterm children who had IUGR and were SGA were also 1.57 times more likely than those with AGA to have BII (cognitive score <1 SD) and 2.77 times more likely to have intellectual impairment (cognitive score <2 SDs). These results suggest an association between preterm IUGR and SGA and neurodevelopmental sequelae.
When considering term-born children, those who had IUGR and were SGA had significantly lower cognitive scores compared with those with AGA. Effect sizes ranged from small to medium, with a small mean estimate. Our findings suggest that term-born children who had IUGR and were SGA have cognitive outcomes that are comparable to those observed in preterm children; however, they are unlikely to receive postnatal follow-up care and be invited to take part in rehabilitative training.61 The results of this meta-analysis therefore point to the importance of identifying those children at risk of developing cognitive sequelae as early as possible, monitoring their development, and effectively intervening if and when needed to strengthen their cognitive profile.
The results of the meta-analyses (cognitive scores and BII in preterm and term-born children) found no significant cognitive differences between the IUGR and SGA subgroups, although the putative etiopathological differences between the 2 were not addressed. Using robust methods, we found that preterm and term-born children with SGA had lower cognitive scores compared with those with AGA. These results are clinically relevant because currently term-born neonates without antenatal evidence of perinatal risk are not likely to receive postnatal care. Of course, we cannot exclude the fact that retrospective study designs or unreported antenatal diagnoses might bias our results by the inclusion of children who had IUGR in the SGA group. Further research is needed to disentangle the neurodevelopmental effect of smallness associated with a typical and atypical antenatal environment (ie, growth restriction).
With regard to children’s age at outcome assessment, children who had IUGR and were SGA had a cognitive disadvantage compared with those with AGA from infancy to middle childhood. On a methodologic note, the studies selected for the meta-analysis overrepresent the first 2 years of life, highlighting the need for long-term follow-up.
The biological mechanisms that could explain our findings are not fully understood but are likely to involve antenatal brain developmental processes. Placental insufficiency, exposing the fetus with IUGR to undernutrition and decrease in growth rate, is likely to affect in utero brain developmental processes. Such suboptimal trophic inputs may lead to the structural and functional brain alterations observed in infants who had IUGR,83,84,85 which potentially underscore the emergence of high-order cognitive processes.86
Strengths and Limitations
Strengths of this meta-analytic study include the large number of samples across countries as well as the age span of participants, ranging from 1 to 12 years. The study has several limitations. First, information about demographic and perinatal variables was not always accessible, making it difficult to study the association of potential relevant factors with outcome (ie, sex, clinical procedure received during neonatal intensive care, or family socioeconomic status). Future studies should investigate putative antenatal and pregnancy-related risk factors for IUGR and SGA as well as childhood cognitive outcomes. A second limitation that was mentioned earlier is the potential inclusion of individuals with antenatal IUGR in the SGA groups. This issue prevents us from addressing potential etiopathological differences between constitutional SGA and former IUGR and SGA subgroups. Another limitation refers to the exclusion of the so-called gray literature and unpublished data, which might lead to publication bias. However, statistical analyses were conducted to assess the risk of such bias.
Conclusions
This study suggests that IUGR and SGA are adversely associated with cognitive development. Growth vulnerability assessed antenatally (IUGR) and at the time of birth (SGA) was associated with cognitive risk in preterm and term-born individuals from infancy to middle childhood. These findings indicate that to improve the outcomes in children who had IUGR and were SGA, the following appear to be needed: (1) advances in antenatal IUGR diagnosis to detect as early as possible the onset of growth restriction; (2) further research comparing cognitive outcomes between children who had antenatal IUGR and those who were SGA (with a clinically defined exclusion of those with antenatal IUGR) to disentangle antenatal vs perinatal effects; and (3) implementations of targeted interventions that boost the cognitive profile of children who had IUGR and were SGA.
eTable 1. Study Characteristics of Preterm (<37 GA) IUGR and SGA Children Assessed for Cognitive Scores
eTable 2. Study Characteristics of Term-Born (≥37 GA) IUGR and SGA Children Assessed for Cognitive Score
eTable 3. Study Characteristics of Preterm IUGR and SGA Children Assessed for Borderline Intellectual Impairment (BII)
eResults. Sensitivity Analysis
eFigure 1. Funnel Plot for Asymmetry in Studies on Cognitive Scores in IUGR and SGA Preterm Children
eFigure 2. Funnel Plot for Asymmetry in Studies on BII
eReferences
References
- 1.Alkalay AL, Graham JM Jr, Pomerance JJ. Evaluation of neonates born with intrauterine growth retardation: review and practice guidelines. J Perinatol. 1998;18(2):142-151. [PubMed] [Google Scholar]
- 2.Lees C, Marlow N, Arabin B, et al. ; TRUFFLE Group . Perinatal morbidity and mortality in early-onset fetal growth restriction: cohort outcomes of the Trial of Randomized Umbilical and Fetal Flow in Europe (TRUFFLE). Ultrasound Obstet Gynecol. 2013;42(4):400-408. doi: 10.1002/uog.13190 [DOI] [PubMed] [Google Scholar]
- 3.Miller SL, Huppi PS, Mallard C. The consequences of fetal growth restriction on brain structure and neurodevelopmental outcome. J Physiol. 2016;594(4):807-823. doi: 10.1113/JP271402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gluckman PD, Hanson MA. The consequences of being born small—an adaptive perspective. Horm Res. 2006;65(suppl 3):5-14. doi: 10.1159/000091500 [DOI] [PubMed] [Google Scholar]
- 5.Chatmethakul T, Roghair RD. Risk of hypertension following perinatal adversity: IUGR and prematurity. J Endocrinol. 2019;242(1):T21-T32. aop. doi: 10.1530/JOE-18-0687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Murray E, Fernandes M, Fazel M, Kennedy SH, Villar J, Stein A. Differential effect of intrauterine growth restriction on childhood neurodevelopment: a systematic review. BJOG. 2015;122(8):1062-1072. doi: 10.1111/1471-0528.13435 [DOI] [PubMed] [Google Scholar]
- 7.Chen J, Chen P, Bo T, Luo K. Cognitive and behavioral outcomes of intrauterine growth restriction school-age children. Pediatrics. 2016;137(4):e20153868. doi: 10.1542/peds.2015-3868 [DOI] [PubMed] [Google Scholar]
- 8.Battaglia FC, Lubchenco LO. A practical classification of newborn infants by weight and gestational age. J Pediatr. 1967;71(2):159-163. doi: 10.1016/S0022-3476(67)80066-0 [DOI] [PubMed] [Google Scholar]
- 9.Nardozza LMM, Caetano ACR, Zamarian ACP, et al. . Fetal growth restriction: current knowledge. Arch Gynecol Obstet. 2017;295(5):1061-1077. doi: 10.1007/s00404-017-4341-9 [DOI] [PubMed] [Google Scholar]
- 10.Simões RV, Cruz-Lemini M, Bargalló N, Gratacós E, Sanz-Cortés M. Brain metabolite differences in one-year-old infants born small at term and association with neurodevelopmental outcome. Am J Obstet Gynecol. 2015;213(2):210.e1-210.e11. doi: 10.1016/j.ajog.2015.04.011 [DOI] [PubMed] [Google Scholar]
- 11.Bassan H, Stolar O, Geva R, et al. . Intrauterine growth-restricted neonates born at term or preterm: how different? Pediatr Neurol. 2011;44(2):122-130. doi: 10.1016/j.pediatrneurol.2010.09.012 [DOI] [PubMed] [Google Scholar]
- 12.Tanis JC, Van Braeckel KNJA, Kerstjens JM, Bocca-Tjeertes IFA, Reijneveld SA, Bos AF. Functional outcomes at age 7 years of moderate preterm and full term children born small for gestational age. J Pediatr. 2015;166(3):552-8.e1. doi: 10.1016/j.jpeds.2014.11.043 [DOI] [PubMed] [Google Scholar]
- 13.Bonett DG. Confidence intervals for standardized linear contrasts of means. Psychol Methods. 2008;13(2):99-109. doi: 10.1037/1082-989X.13.2.99 [DOI] [PubMed] [Google Scholar]
- 14.Bonett DG. Meta-analytic interval estimation for standardized and unstandardized mean differences. Psychol Methods. 2009;14(3):225-238. doi: 10.1037/a0016619 [DOI] [PubMed] [Google Scholar]
- 15.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629-634. doi: 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Duval S, Tweedie R. A nonparametric “trim and fill” method of accounting for publication bias in meta-analysis. J Am Stat Assoc. 2000;95(449):89-98. doi: 10.1080/01621459.2000.10473905 [DOI] [Google Scholar]
- 17.Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56(2):455-463. doi: 10.1111/j.0006-341X.2000.00455.x [DOI] [PubMed] [Google Scholar]
- 18.Lipsey MW, Wilson DB. Practical Meta-analysis. Sage Publications Inc; 2001. [Google Scholar]
- 19.Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557-560. doi: 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Parmenter TR. What is intellectual disability? how is it assessed and classified? Int J Disabil Dev Educ. 2011;58(3):303-319. doi: 10.1080/1034912X.2011.598675 [DOI] [Google Scholar]
- 21.R Development Core Team R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing; 2008, doi: 10.1007/978-3-540-74686-7. [DOI] [Google Scholar]
- 22.Ballot DE, Ramdin T, Rakotsoane D, et al. . Assessment of developmental outcome in very low birth weight infants in Southern Africa using the Bayley Scales of Infant Development (III). BMJ Paediatr Open. 2017;1(1):e000091. doi: 10.1136/bmjpo-2017-000091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Koivisto A, Klenberg L, Tommiska V, et al. ; Finnish ELBW Cohort Study Group (FinELBW) . Parents tend to underestimate cognitive deficits in 10- to 13-year-olds born with an extremely low birth weight. Acta Paediatr. 2015;104(11):1182-1188. doi: 10.1111/apa.13087 [DOI] [PubMed] [Google Scholar]
- 24.Nögel SC, Deiters L, Stemmler M, Rascher W, Trollmann R. Preterm small-for-gestational age children: predictive role of gestational age for mental development at the age of 2 years. Brain Dev. 2015;37(4):394-401. doi: 10.1016/j.braindev.2014.06.012 [DOI] [PubMed] [Google Scholar]
- 25.Feldman R, Eidelman AI. Neonatal state organization, neuromaturation, mother-infant interaction, and cognitive development in small-for-gestational-age premature infants. Pediatrics. 2006;118(3):e869-e878. doi: 10.1542/peds.2005-2040 [DOI] [PubMed] [Google Scholar]
- 26.Geva R, Yosipof R, Eshel R, Leitner Y, Valevski AF, Harel S. Readiness and adjustments to school for children with intrauterine growth restriction (IUGR): an extreme test case paradigm. Except Child. 2009;75(2):211-230. doi: 10.1177/001440290907500205 [DOI] [Google Scholar]
- 27.Leppänen M, Lapinleimu H, Lind A, et al. ; PIPARI Study Group . Antenatal and postnatal growth and 5-year cognitive outcome in very preterm infants. Pediatrics. 2014;133(1):63-70. doi: 10.1542/peds.2013-1187 [DOI] [PubMed] [Google Scholar]
- 28.Tamaru S, Kikuchi A, Takagi K, et al. . Neurodevelopmental outcomes of very low birth weight and extremely low birth weight infants at 18 months of corrected age associated with prenatal risk factors. Early Hum Dev. 2011;87(1):55-59. doi: 10.1016/j.earlhumdev.2010.10.004 [DOI] [PubMed] [Google Scholar]
- 29.Bickle Graz M, Tolsa JF, Fischer Fumeaux CJ. Being small for gestational age: does it matter for the neurodevelopment of premature infants? a cohort study. PLoS One. 2015;10(5):e0125769. doi: 10.1371/journal.pone.0125769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mukhopadhyay K, Malhi P, Mahajan R, Narang A. Neurodevelopmental and behavioral outcome of very low birth weight babies at corrected age of 2 years. Indian J Pediatr. 2010;77(9):963-967. doi: 10.1007/s12098-010-0149-3 [DOI] [PubMed] [Google Scholar]
- 31.Claas MJ, Bruinse HW, Koopman C, van Haastert IC, Peelen LM, de Vries LS. Two-year neurodevelopmental outcome of preterm born children ≤ 750 g at birth. Arch Dis Child Fetal Neonatal Ed. 2011;96(3):F169-F177. doi: 10.1136/adc.2009.174433 [DOI] [PubMed] [Google Scholar]
- 32.Mikkola K, Kushnerenko E, Partanen E, et al. . Auditory event-related potentials and cognitive function of preterm children at five years of age. Clin Neurophysiol. 2007;118(7):1494-1502. doi: 10.1016/j.clinph.2007.04.012 [DOI] [PubMed] [Google Scholar]
- 33.Batalle D, Eixarch E, Figueras F, et al. . Altered small-world topology of structural brain networks in infants with intrauterine growth restriction and its association with later neurodevelopmental outcome. Neuroimage. 2012;60(2):1352-1366. doi: 10.1016/j.neuroimage.2012.01.059 [DOI] [PubMed] [Google Scholar]
- 34.Gutbrod T, Wolke D, Soehne B, Ohrt B, Riegel K. Effects of gestation and birth weight on the growth and development of very low birthweight small for gestational age infants: a matched group comparison. Arch Dis Child Fetal Neonatal Ed. 2000;82(3):F208-F214. doi: 10.1136/fn.82.3.F208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Filipouski GR, Silveira RC, Procianoy RS. Influence of perinatal nutrition and gestational age on neurodevelopment of very low-birth-weight preterm infants. Am J Perinatol. 2013;30(8):673-680. doi: 10.1055/s-0032-1331030 [DOI] [PubMed] [Google Scholar]
- 36.Raz S, Debastos AK, Newman JB, Batton D. Intrauterine growth and neuropsychological performance in very low birth weight preschoolers. J Int Neuropsychol Soc. 2012;18(2):200-211. doi: 10.1017/S1355617711001767 [DOI] [PubMed] [Google Scholar]
- 37.Lahat A, Van Lieshout RJ, Saigal S, Boyle MH, Schmidt LA. Small for gestational age and poor fluid intelligence in childhood predict externalizing behaviors among young adults born at extremely low birth weight. Dev Psychopathol. 2015;27(1):181-188. doi: 10.1017/S0954579414000662 [DOI] [PubMed] [Google Scholar]
- 38.El Ayoubi M, Patkai J, Bordarier C, et al. . Impact of fetal growth restriction on neurodevelopmental outcome at 2 years for extremely preterm infants: a single institution study. Dev Med Child Neurol. 2016;58(12):1249-1256. doi: 10.1111/dmcn.13218 [DOI] [PubMed] [Google Scholar]
- 39.Cartwright RD, Crowther CA, Anderson PJ, Harding JE, Doyle LW, McKinlay CJD. Association of fetal growth restriction with neurocognitive function after repeated antenatal betamethasone treatment vs placebo: secondary analysis of the ACTORDS randomized clinical trial. JAMA Netw Open. 2019;2(2):e187636. doi: 10.1001/jamanetworkopen.2018.7636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Morsing E, Malova M, Kahn A, et al. . Brain volumes and developmental outcome in childhood following fetal growth restriction leading to very preterm birth. Front Physiol. 2018;9(Nov):1583. doi: 10.3389/fphys.2018.01583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Scherjon S, Briët J, Oosting H, Kok J. The discrepancy between maturation of visual-evoked potentials and cognitive outcome at five years in very preterm infants with and without hemodynamic signs of fetal brain-sparing. Pediatrics. 2000;105(2):385-391. doi: 10.1542/peds.105.2.385 [DOI] [PubMed] [Google Scholar]
- 42.Wienerroither H, Steiner H, Tomaselli J, Lobendanz M, Thun-Hohenstein L. Intrauterine blood flow and long-term intellectual, neurologic, and social development. Obstet Gynecol. 2001;97(3):449-453. [DOI] [PubMed] [Google Scholar]
- 43.Procianoy RS, Koch MS, Silveira RC. Neurodevelopmental outcome of appropriate and small for gestational age very low birth weight infants. J Child Neurol. 2009;24(7):788-794. doi: 10.1177/0883073808331087 [DOI] [PubMed] [Google Scholar]
- 44.Roelants-van Rijn AM, van der Grond J, Stigter RH, de Vries LS, Groenendaal F. Cerebral structure and metabolism and long-term outcome in small-for-gestational-age preterm neonates. Pediatr Res. 2004;56(2):285-290. doi: 10.1203/01.PDR.0000132751.09067.3F [DOI] [PubMed] [Google Scholar]
- 45.Padilla N, Perapoch J, Carrascosa A, Acosta-Rojas R, Botet F, Gratacós E. Twelve-month neurodevelopmental outcome in preterm infants with and without intrauterine growth restriction. Acta Paediatr. 2010;99(10):1498-1503. doi: 10.1111/j.1651-2227.2010.01848.x [DOI] [PubMed] [Google Scholar]
- 46.Morsing E, Åsard M, Ley D, Stjernqvist K, Marsál K. Cognitive function after intrauterine growth restriction and very preterm birth. Pediatrics. 2011;127(4):e874-e882. doi: 10.1542/peds.2010-1821 [DOI] [PubMed] [Google Scholar]
- 47.Padilla N, Falcón C, Sanz-Cortés M, et al. . Differential effects of intrauterine growth restriction on brain structure and development in preterm infants: a magnetic resonance imaging study. Brain Res. 2011;1382:98-108. doi: 10.1016/j.brainres.2011.01.032 [DOI] [PubMed] [Google Scholar]
- 48.Leppänen M, Ekholm E, Palo P, et al. ; PIPARI Study Group . Abnormal antenatal Doppler velocimetry and cognitive outcome in very-low-birth-weight infants at 2 years of age. Ultrasound Obstet Gynecol. 2010;36(2):178-185. doi: 10.1002/uog.7694 [DOI] [PubMed] [Google Scholar]
- 49.Chen C-Y, Wang K-G, Wang S-M, Chen C-P. Two-year neurological outcome of very-low-birth-weight children with prenatal absent or reversed end-diastolic flow velocity in the umbilical artery. Taiwan J Obstet Gynecol. 2013;52(3):323-328. doi: 10.1016/j.tjog.2012.04.039 [DOI] [PubMed] [Google Scholar]
- 50.Morsing E, Maršál K. Pre-eclampsia- an additional risk factor for cognitive impairment at school age after intrauterine growth restriction and very preterm birth. Early Hum Dev. 2014;90(2):99-101. doi: 10.1016/j.earlhumdev.2013.12.002 [DOI] [PubMed] [Google Scholar]
- 51.Bischoff AR, Pokhvisneva I, Léger É, et al. ; MAVAN Research Team . Dynamic interaction between fetal adversity and a genetic score reflecting dopamine function on developmental outcomes at 36 months. PLoS One. 2017;12(5):e0177344. doi: 10.1371/journal.pone.0177344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hartkopf J, Schleger F, Keune J, et al. . Impact of intrauterine growth restriction on cognitive and motor development at 2 years of age. Front Physiol. 2018;9(SEP):1278. doi: 10.3389/fphys.2018.01278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Drews-Botsch C, Schieve LA, Kable J, Coles C. Socioeconomic differences and the impact of being small for gestational age on neurodevelopment among preschool-aged children. Rev Environ Health. 2011;26(3):221-229. doi: 10.1515/reveh.2011.030 [DOI] [PubMed] [Google Scholar]
- 54.Hollo O, Rautava P, Korhonen T, Helenius H, Kero P, Sillanpää M. Academic achievement of small-for-gestational-age children at age 10 years. Arch Pediatr Adolesc Med. 2002;156(2):179-187. doi: 10.1001/archpedi.156.2.179 [DOI] [PubMed] [Google Scholar]
- 55.Rao MR, Hediger ML, Levine RJ, Naficy AB, Vik T. Effect of breastfeeding on cognitive development of infants born small for gestational age. Acta Paediatr. 2002;91(3):267-274. doi: 10.1111/j.1651-2227.2002.tb01713.x [DOI] [PubMed] [Google Scholar]
- 56.Peng Y, Huang B, Biro F, Feng L, Guo Z, Slap G. Outcome of low birthweight in China: a 16-year longitudinal study. Acta Paediatr. 2005;94(7):843-849. doi: 10.1111/j.1651-2227.2005.tb01999.x [DOI] [PubMed] [Google Scholar]
- 57.Pylipow M, Spector LG, Puumala SE, Boys C, Cohen J, Georgieff MK. Early postnatal weight gain, intellectual performance, and body mass index at 7 years of age in term infants with intrauterine growth restriction. J Pediatr. 2009;154(2):201-206. doi: 10.1016/j.jpeds.2008.08.015 [DOI] [PubMed] [Google Scholar]
- 58.Gagliardo HGRG, Gonçalves VM, Lima MC, Francozo MdeF, Aranha Netto A. Visual function and fine-motor control in small-for-gestational age infants. Arq Neuropsiquiatr. 2004;62(4):955-962. doi: 10.1590/S0004-282X2004000600005 [DOI] [PubMed] [Google Scholar]
- 59.Sommerfelt K, Andersson HW, Sonnander K, et al. . Cognitive development of term small for gestational age children at five years of age. Arch Dis Child. 2000;83(1):25-30. doi: 10.1136/adc.83.1.25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Leitner Y, Fattal-Valevski A, Geva R, et al. . Six-year follow-up of children with intrauterine growth retardation: long-term, prospective study. J Child Neurol. 2000;15(12):781-786. doi: 10.1177/088307380001501202 [DOI] [PubMed] [Google Scholar]
- 61.Nomura Y, Halperin JM, Newcorn JH, et al. . The risk for impaired learning-related abilities in childhood and educational attainment among adults born near-term. J Pediatr Psychol. 2009;34(4):406-418. doi: 10.1093/jpepsy/jsn092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Batalle D, Muñoz-Moreno E, Figueras F, Bargallo N, Eixarch E, Gratacos E. Normalization of similarity-based individual brain networks from gray matter MRI and its association with neurodevelopment in infants with intrauterine growth restriction. Neuroimage. 2013;83:901-911. doi: 10.1016/j.neuroimage.2013.07.045 [DOI] [PubMed] [Google Scholar]
- 63.Savchev S, Sanz-Cortes M, Cruz-Martinez R, et al. . Neurodevelopmental outcome of full-term small-for-gestational-age infants with normal placental function. Ultrasound Obstet Gynecol. 2013;42(2):201-206. doi: 10.1002/uog.12391 [DOI] [PubMed] [Google Scholar]
- 64.Mello B, Gagliardo H, Gonçalves V. Neurodevelopment of small-for-gestational age infants: behavioral aspects in first year. Arq Neuropsiquiatr. 2014;72(7):517-523. doi: 10.1590/0004-282X20140096 [DOI] [PubMed] [Google Scholar]
- 65.Geva R, Eshel R, Leitner Y, Valevski AF, Harel S. Neuropsychological outcome of children with intrauterine growth restriction: a 9-year prospective study. Pediatrics. 2006;118(1):91-100. doi: 10.1542/peds.2005-2343 [DOI] [PubMed] [Google Scholar]
- 66.Zuk L, Harel S, Leitner Y, Fattal-Valevski A. Neonatal general movements: an early predictor for neurodevelopmental outcome in infants with intrauterine growth retardation. J Child Neurol. 2004;19(1):14-18. doi: 10.1177/088307380401900103011 [DOI] [PubMed] [Google Scholar]
- 67.Leitner Y, Fattal-Valevski A, Geva R, et al. . Neurodevelopmental outcome of children with intrauterine growth retardation: a longitudinal, 10-year prospective study. J Child Neurol. 2007;22(5):580-587. doi: 10.1177/0883073807302605 [DOI] [PubMed] [Google Scholar]
- 68.Bellido-González M, Díaz-López MA, López-Criado S, Maldonado-Lozano J. Cognitive functioning and academic achievement in children aged 6-8 years, born at term after intrauterine growth restriction and fetal cerebral redistribution. J Pediatr Psychol. 2017;42(3):345-354. doi: 10.1093/jpepsy/jsw060 [DOI] [PubMed] [Google Scholar]
- 69.Orcesi S, Olivieri I, Longo S, et al. . Neurodevelopmental outcome of preterm very low birth weight infants born from 2005 to 2007. Eur J Paediatr Neurol. 2012;16(6):716-723. doi: 10.1016/j.ejpn.2012.05.006 [DOI] [PubMed] [Google Scholar]
- 70.Fernandez-Carrocera LA, Chavez-Torres R, Casanueva E, Barrera-Reyes RH, Ibarra-Reyes MD, Martinez-Cruz C. Intrauterine growth retardation and neurodevelopment at one year of age in Mexican children. Nutr Res. 2003;23(1):1-8. doi: 10.1016/S0271-5317(02)00385-8 [DOI] [Google Scholar]
- 71.Guellec I, Lapillonne A, Marret S, et al. ; Étude Épidémiologique sur les Petits Âges Gestationnels (EPIPAGE [Epidemiological Study on Small Gestational Ages]) Study Group . Effect of intra- and extrauterine growth on long-term neurologic outcomes of very preterm infants. J Pediatr. 2016;175:93-99.e1. doi: 10.1016/j.jpeds.2016.05.027 [DOI] [PubMed] [Google Scholar]
- 72.Claas MJ, de Vries LS, Koopman C, et al. . Postnatal growth of preterm born children ≤ 750g at birth. Early Hum Dev. 2011;87(7):495-507. doi: 10.1016/j.earlhumdev.2011.04.009 [DOI] [PubMed] [Google Scholar]
- 73.Guellec I, Lapillonne A, Renolleau S, et al. ; EPIPAGE Study Group . Neurologic outcomes at school age in very preterm infants born with severe or mild growth restriction. Pediatrics. 2011;127(4):e883-e891. doi: 10.1542/peds.2010-2442 [DOI] [PubMed] [Google Scholar]
- 74.Beaino G, Khoshnood B, Kaminski M, et al. ; EPIPAGE Study Group . Predictors of the risk of cognitive deficiency in very preterm infants: the EPIPAGE prospective cohort. Acta Paediatr. 2011;100(3):370-378. doi: 10.1111/j.1651-2227.2010.02064.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Charkaluk M-L, Marchand-Martin L, Ego A, et al. ; EPIPAGE Study Group . The influence of fetal growth reference standards on assessment of cognitive and academic outcomes of very preterm children. J Pediatr. 2012;161(6):1053-1058. doi: 10.1016/j.jpeds.2012.05.037 [DOI] [PubMed] [Google Scholar]
- 76.Kiechl-Kohlendorfer U, Ralser E, Pupp Peglow U, Reiter G, Trawöger R. Adverse neurodevelopmental outcome in preterm infants: risk factor profiles for different gestational ages. Acta Paediatr. 2009;98(5):792-796. doi: 10.1111/j.1651-2227.2009.01219.x [DOI] [PubMed] [Google Scholar]
- 77.De Jesus LC, Pappas A, Shankaran S, et al. ; Eunice Kennedy Shriver National Institute of Health and Human Development Neonatal Research Network . Outcomes of small for gestational age infants born at <27 weeks’ gestation. J Pediatr. 2013;163(1):55-60.e1, 3. doi: 10.1016/j.jpeds.2012.12.097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Pinello L, Manea S, Visonà Dalla Pozza L, Mazzarolo M, Facchin P. Visual, motor, and psychomotor development in small-for-gestational-age preterm infants. J AAPOS. 2013;17(4):352-356. doi: 10.1016/j.jaapos.2013.03.026 [DOI] [PubMed] [Google Scholar]
- 79.Leviton A, Fichorova RN, O’Shea TM, et al. ; ELGAN Study Investigators . Two-hit model of brain damage in the very preterm newborn: small for gestational age and postnatal systemic inflammation. Pediatr Res. 2013;73(3):362-370. doi: 10.1038/pr.2012.188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Spinillo A, Gardella B, Preti E, Zanchi S, Stronati M, Fazzi E. Rates of neonatal death and cerebral palsy associated with fetal growth restriction among very low birthweight infants: a temporal analysis. BJOG. 2006;113(7):775-780. doi: 10.1111/j.1471-0528.2006.00974.x [DOI] [PubMed] [Google Scholar]
- 81.Jelliffe-Pawlowski LL, Hansen RL. Neurodevelopmental outcome at 8 months and 4 years among infants born full-term small-for-gestational-age. J Perinatol. 2004;24(8):505-514. doi: 10.1038/sj.jp.7211111 [DOI] [PubMed] [Google Scholar]
- 82.Allotey J, Zamora J, Cheong-See F, et al. . Cognitive, motor, behavioural and academic performances of children born preterm: a meta-analysis and systematic review involving 64 061 children. BJOG. 2018;125(1):16-25. doi: 10.1111/1471-0528.14832 [DOI] [PubMed] [Google Scholar]
- 83.Lodygensky GA, Seghier ML, Warfield SK, et al. . Intrauterine growth restriction affects the preterm infant’s hippocampus. Pediatr Res. 2008;63(4):438-443. doi: 10.1203/PDR.0b013e318165c005 [DOI] [PubMed] [Google Scholar]
- 84.Tolsa CB, Zimine S, Warfield SK, et al. . Early alteration of structural and functional brain development in premature infants born with intrauterine growth restriction. Pediatr Res. 2004;56(1):132-138. doi: 10.1203/01.PDR.0000128983.54614.7E [DOI] [PubMed] [Google Scholar]
- 85.Batalle D, Eixarch E, Muñoz-Moreno E, et al. . Altered structural brain network topology in infants with intrauterine growth restriction In: Proceedings of the 2012 9th IEEE International Symposium on Biomedical Imaging (ISBI). IEEE; 2012:554-557. doi: 10.1109/ISBI.2012.6235608 [DOI] [Google Scholar]
- 86.Baschat AA. Neurodevelopment following fetal growth restriction and its relationship with antepartum parameters of placental dysfunction. Ultrasound Obstet Gynecol. 2011;37(5):501-514. doi: 10.1002/uog.9008 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Study Characteristics of Preterm (<37 GA) IUGR and SGA Children Assessed for Cognitive Scores
eTable 2. Study Characteristics of Term-Born (≥37 GA) IUGR and SGA Children Assessed for Cognitive Score
eTable 3. Study Characteristics of Preterm IUGR and SGA Children Assessed for Borderline Intellectual Impairment (BII)
eResults. Sensitivity Analysis
eFigure 1. Funnel Plot for Asymmetry in Studies on Cognitive Scores in IUGR and SGA Preterm Children
eFigure 2. Funnel Plot for Asymmetry in Studies on BII
eReferences