Abstract
These recommendations for physicians who perform bronchoscopy will help to protect those patients (un)-affected by the current COVID-19 pandemic, minimize the risk of transmission, and maintain clinical care for all patients.
Keywords: Bronchoscopy, COVID-19, Interventional pneumology
Introduction
Coronaviruses are a large family of viruses that are known to cause illness ranging from the common cold to more severe diseases such as Middle East respiratory syndrome (MERS) and severe acute respiratory syndrome (SARS). As the official disease name was established after material creation, any mention of nCoV refers to COVID-19, the infectious disease caused by the most recently discovered coronavirus [1].
Starting in December 2019, COVID-19 has led to an increasing number of infections worldwide. Affected patients most often complain of fever, cough, anosmia, rhinitis, with moderate to severe cases presenting with shortness of breath; gastrointestinal symptoms, although rare, have been observed and comprise of vomiting and diarrhea [2]. Reported illnesses have ranged from mild symptoms to severe illness and death for COVID-19 cases. The majority of COVID-19 infections are mild (80%), some require hospitalization and oxygen therapy (15%), and approximately 5% require intensive care, associated with over 50% mortality [3, 4].
The respiratory virus spreads primarily through droplets and microdroplets generated by an infected person. The biological details of transmission of COVID-19 are known in general terms: these viruses can pass from one individual to another through exhaled droplets, aerosol, contamination of surfaces, and possibly through fecal-oral contamination [5, 6]. Hence, patients with both suspected and confirmed COVID-19 infection should preferably be cared for with protective gowns, gloves, safety glasses or face shields, if available, and with filtering facepiece (FFP) masks. The preferred standard is an FFP3 mask where the total leakage must not exceed 5% and should filter 99% of all particles measuring up to 0.6 μm. Bronchoscopy is an aerosol-generating procedure that leads to a pronounced formation of aerosols and thus poses a high risk of infection to proximate healthcare staff [7]. According to the guidelines of the Centers for Disease Control and Prevention, in the event of a lack of protective masks, these should be used primarily for procedures with pronounced aerosol formation such as bronchoscopy [8]. The theoretical basis for its risk as an aerosol-generating procedure is clear, although the evidence from studies, albeit of low quality, is not apparent [9]. Nevertheless, careful preparation and precautions are necessary considering the significant number of healthcare workers infected by the virus in China or Italy.
Considerations before Bronchoscopy
Bronchoscopy remains an important diagnostic and therapeutic tool in critically ill patients.
Strict indication for performing bronchoscopies; elective procedures should be postponed.
Ask about the epidemiological history, especially the history of travel and COVID-19 patient contact.
Measure the temperature of the patient before the procedure (with a noncontact device if available).
Nasopharyngeal swab test for SARS-CoV-2 reverse transcriptase ribonucleic acid (RT-DNA PCR) before the procedure (if available). Asymptomatic carriage is a significant source of transmission during the pandemic [10, 11].
The patient should be categorized according to their COVID-19 status as (1) Confirmed, (2) Probable, (3) Not Probable, or (4) Negative. Patients with history, clinical findings, or CT pattern typical for COVID-19 should be categorized aso “Probable” irrespective of the result of the nasopharyngeal swab and only patients with negative nasopharyngeal swab and clinical appearance which is atypical for COVID-19 should be labeled as “Negative.”
Performing Bronchoscopy in the Bronchoscopy Suite
These recommendations for physicians who perform bronchoscopy will help to protect those patients (un)-affected by the current COVID-19 pandemic, minimize the risk of transmission, and maintain clinical care for all patients.
Bronchoscopy in All Patients
Reduction of the staff (bronchoscopist, bronchoscopy assistant, anesthesia team if necessary) to a core team, who carry out all the interventions of the day to minimize staff exposure.
No observers, students, apprentices, or trainees should be in the examination room.
Patient should wear a surgical mask in the pre-procedure area, bronchoscopy suite, and recovery area.
Use of disposable gowns, disposable gloves, cap, and FFP2 mask, for everyone present in the procedure room.
Use of personal disposable safety glasses (can also be used on subsequent days after reprocessing) and/or a face shield for the doctor and bronchoscopy assistant.
Consideration of the national health authority's guideline (like NICE, RKI) for procedures to put on (don) and take off (doff) the protective masks [12, 13].
For flexible bronchoscopy, transnasal access is preferred with the additional use of a slotted mouth and nose protector for the patient.
Replace rigid bronchoscopy with JET ventilation, if medically justifiable, with closed ventilation systems (tube, laryngeal mask).
If rigid bronchoscopy is unavoidable, then conventional ventilation and reduction of the aerosol leakage, e.g., using the FLUVOG© attachment, should be preferred.
Bronchoscopy in SARS-CoV-2 (COVID-19) Confirmed or Probable Positive Patients
The indication for bronchoscopy in the case of confirmed or suspected COVID-19 disease should be made very strict and should only be considered if:
Diagnostic reason:
the nasopharyngeal smear is negative two times and clinically there is still diagnostic uncertainty of COVID-19 infection.
Other diagnoses are considered that would significantly change clinical management.
Therapeutic reason:
An urgent life-saving intervention is necessary (hemoptysis, higher-grade benign or malignant central airway stenosis or foreign body aspiration).
If bronchoscopy is performed for diagnostic reason, tracheobronchial lavage using a few milliliters or bronchoalveolar lavage (BAL) only is recommended. No other diagnostic procedures such as transbronchial biopsy or needle aspiration should be performed in the same procedure.
Perform procedures in an adequately ventilated room − that is, natural ventilation with air flow of at least 160 L/s per patient or ideally in negative pressure rooms with at least 12 air changes per hour and controlled direction of air flow when using mechanical ventilation.
FFP3 mask (if not available FFP2 masks) should be used. The respirator should be discarded after the procedure.
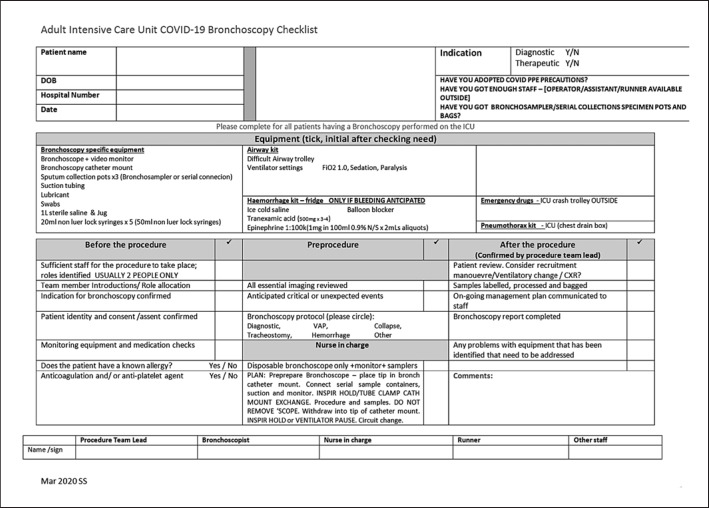
The procedure should be carried out by an experienced examiner. If available, a special planning and procedure checklist should be used (Table 1; Fig. 1).
Table 1.
Bronchoscopy in intubated COVID+ patients
| Indications and benefits |
| Secretion management |
| Radiological worsening, nosocomial overinfection |
| Hemoptysis |
| Artificial airway management (orotracheal tube position, difficult intubation, tracheostomy guidance) |
| Potential risk |
| Respiratory deterioration |
| Staff contamination |
| Findings |
| Normal mucosa or hyperemia (frequent) |
| Mucous plugs, thick jelly secretions (frequent) |
| Blood clots (infrequent) |
| Recommended procedures |
| Direct suction |
| Instillation of mucoactive agents for secretions (hypertonic saline, hyaluronic acid, N-acetylcysteine, rhDNAse) |
| Mini-BAL for microbiological studies |
|
Practical tips for safe, effective, and shortest duration bronchoscopic sampling a. Check all equipment is ready − see checklist b. 100% FiO2, +/– ECMO flow/sweep gas increase for the procedure c. Neuromuscular paralysis for bronchoscopy unless contraindicated d. Staff check of personal protective equipment and set FiO2 at 1.0 e. Pre-prepare the bronchoscope/sampler/catheter mount 1 Connect the bronchosampler to the scope; connect the scope to a view monitor 2 Put the tip of the bronchoscope into the catheter mount 3 Prior to exchanging the catheter mount, tube clamp and perform an inspiratory hold on the ventilator during circuit breaks 4 See the simple instruction for the bronchosampler 5 At completion, DO NOT remove the bronchoscope; withdraw the tip into the end of the catheter mount; clamp the endotracheal tube, inspiratory hold, then quick circuit change, unclamp, and resume ventilation |
Fig. 1.
Checklist for bronchoscopy from the Royal Brompton Hospital, London, UK (permission granted by Dr. Singh).
In patients with suspected endobronchial infection, particularly viral, bronchoalveolar sampling increases diagnostic sensitivity compared with nasopharyngeal aspirates. There is an increased risk of false-negative results, particularly for viral infections such as SARS-CoV-2, if the nasopharyngeal aspirate test is performed after 48 h of the onset of symptoms. In this situation BAL has been more sensitive, although inline tracheal aspirates are a recommended nursing alternative.
Bronchoscopy in the ICU
Given that associated bacterial, viral, and fungal co-infection should not be underestimated, the value of directed sampling as well as mycology and Galactomannan are important in these sickest patients [14]. Moreover, ventilator-associated pneumonia occurs in up to ∼30% patients, and accurate sampling can reduce unnecessary antibiotics [15].
The cause of lobar collapse in the critical care setting is often multifactorial. A combination of predisposing disease-related risks, procedural impact on the lung, nonphysiological impacts of sedation, position, inadequate airway clearance mechanisms, and lack of spontaneous ventilatory effort all contribute to lobar collapse. High inspiratory oxygen fraction (FiO2) can in itself lead to reabsorption atelectasis through nitrogen washout.
Bronchoscopy is commonly used in lobar and complete lung collapse during mechanical ventilation, where physiotherapy, prone positioning, or recruitment maneuvers have been unsuccessful. It may identify bronchial migration of the endotracheal tube as a cause of the collapse. Directed suction is usually combined with forced saline flushing. Repeated episodes may be necessary. If time and patient tolerance allow, exploration of the left and right bronchial tree repeatedly is advisable, so as to aspirate delayed emergence of distal secretions some minutes after forced lavage.
General anesthesia with muscle relaxant is recommended in COVID-19 patients to reduce aerosol production.
Wear disposable working cap, medical comprehensive respirator or positive pressure head hood, medical mask (FFP3 or FFP2), disposable protective suit, protective clothing, disposable latex gloves, and disposable shoe cover.
A WHO style checklist and Timeout is of great importance to minimize risk. Whilst highly unlikely, emergency drills including cardiac resuscitation protocols for the COVID-19 patient should be noted for safe adoption in need.
For patients with intubation and mechanical ventilation, FiO2 should be adjusted to 100%. Volume control, pressure-limited mode, is preferred and PEEP should be kept at the same level during the procedure. Adjustments can be made dynamically, with a prior risk assessment of the anticipated risks (e.g., lung derecruitment, airway obstruction and desaturation, circuit breaks, arrhythmias, pneumothorax).
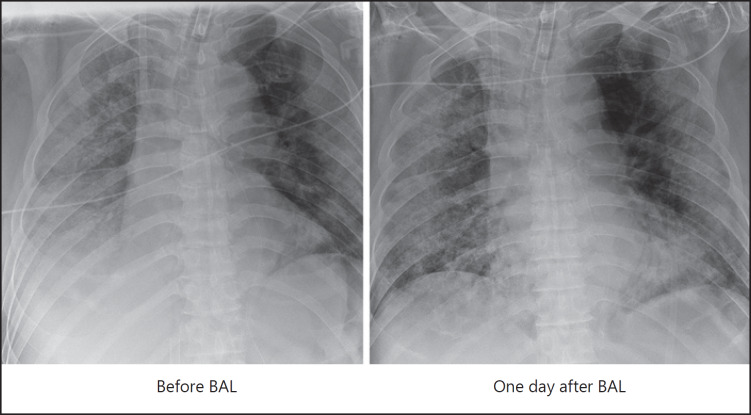
In dedicated cases a therapeutic BAL might be indicated (Fig. 2).
Monitor the SpO2 during the procedure and stop the procedure if SpO2 drops. Avoid BAL in patients with obvious hypoxia (SpO2 <92%, especially if already on supplemental oxygen support).
For the patient on veno-venous ECMO support, anticoagulation should have been stopped a few hours before the procedure, and clotting time tested pre-procedure. Platelets should be >50/μL. BAL may be performed. Therapeutic lavage will help to wash out the mucus in the distal airway (Fig. 3).
Specimens should be stored and processed according to the biosafety requirement.
A negative pressure suite with at least 10 cycles/h exchange is preferred for the procedure if possible. Otherwise, the examination room should be disinfected and an air disinfection machine may be applied.
All staff must remove personal protective equipment according to the appropriate training and leave the examination area only after ensuring strict hand hygiene.
Fig. 2.
Male patient, aged 66 years. Admission to hospital presenting with cough and fever for 10 days. He had COPD and hypertension. The patient was intubated and ventilated on March 15, 2020, following progressive hypoxemic respiratory failure despite high-flow nasal oxygen therapy (HFNO). Veno-venous ECMO was instituted on day 2 due to refractory severe acute respiratory distress syndrome (SARDS). Chest radiography demonstrated worsening opacification in the right low zone. Hence, bronchoscopy was performed on day 4. Therapeutic BAL was performed in the right lower lobe basal segments. A large quantity of mucus was cleared. A chest X-ray the following day showed clearing of the lung fields and restored visibility of the right hemidiaphragm.
Fig. 3.
Protection during bronchoscopy on a ventilated COVID-19 patient.
Postprocedural Necessities
Following completion of the bronchoscopy, a review of the patient and physiological parameters as well as the ventilator settings (particularly delivered volume) is advised. A short recruitment maneuver may be necessary to improve oxygenation, and a chest radiograph should be ordered to exclude a pneumothorax.
Where possible utilize disposable single-use bronchoscopes if timely and validated reprocessing of the bronchoscopes is not ensured.
If timely and validated reprocessing of the bronchoscopes is ensured, the reprocessing process for disinfecting the devices does not have to be changed [16, 17]. However, the bronchoscope should be transported and sterilized separately from other patients.
Statement of Ethics
The consensus of experts was used to formulate the recommendation.
Disclosure Statement
The authors have no conflicts of interest to declare related to the publication.
References
- 1.World Health Organization Emerging respiratory viruses, including COVID-19: methods for detection, prevention, response and control (cited 2020 April 6) https://openwho.org/courses/introduction-to-ncov. [DOI] [PMC free article] [PubMed]
- 2.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. China Medical Treatment Expert Group for Covid-19 Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020 doi: 10.1056/NEJMoa2002032. Available from: https://www.ncbi.nlm.nih.gov/pubmed/32242738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Du Y, Tu L, Zhu P, Mu M, Wang R, Yang P, et al. Clinical Features of 85 Fatal Cases of COVID-19 from Wuhan: A Retrospective Observational Study. Am J Respir Crit Care Med. 2020 doi: 10.1164/rccm.202003-0543OC. Available from: https://www.ncbi.nlm.nih.gov/pubmed/32242738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020 Feb;323((11)):1061. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ferretti L, Wymant C, Kendall M, Zhao L, Nurtay A, Abeler-Dörner L, et al. Quantifying SARS-CoV-2 transmission suggests epidemic control with digital contact tracing. Science. 2020 Mar;31:eabb6936. doi: 10.1126/science.abb6936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ong SW, Tan YK, Chia PY, Lee TH, Ng OT, Wong MS, et al. Air, Surface Environmental, and Personal Protective Equipment Contamination by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) From a Symptomatic Patient. JAMA. 2020 Mar; doi: 10.1001/jama.2020.3227. Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tran K, Cimon K, Severn M, Pessoa-Silva CL, Conly J. Aerosol-generating procedures and risk of transmission of acute respiratory infections: a systematic review. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health. 2011. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3579388/. [PubMed]
- 8.CDC − Centers for Disease Control and Prevention Interim infection prevention and control recommendations for patients with suspected or confirmed coronavirus disease 2019 (COVID-19) in healthcare settings (cited 2020 March 23) Available from: https://www.cdc.gov/coronavirus/2019-ncov/infection-control/control-recommendations.html.
- 9.World Health Organization Q&A on coronaviruses (COVID-19) (cited 2020 April 5) Available from: https://www.who.int/newsroom/q-a-detail/q-a-coronaviruses.
- 10.Zhang J, Tian S, Lou J, Chen Y. Familial cluster of COVID-19 infection from an asymptomatic. Crit Care. 2020 Mar;24((1)):119. doi: 10.1186/s13054-020-2817-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bai Y, Yao L, Wei T, Tian F, Jin DY, Chen L, et al. Presumed Asymptomatic Carrier Transmission of COVID-19. JAMA. 2020 Feb;323((14)):1406. doi: 10.1001/jama.2020.2565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Robert Koch Institut BMG/BMAS/ABAS/ RKI: Ressourcenschonender Einsatz von Mund-Nasen-Schutz (MNS) und FFPMasken (cited 2020 April 2) https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Ressourcen_schonen_Masken.pdf.
- 13.NICE − National Institute for Health and Care Excellence Coronavirus (COVID-19) (cited 2020 April 5) https://www.nice.org.uk/guidance/ng159.
- 14.Ding Q, Lu P, Fan Y, Xia Y, Liu M. The clinical characteristics of pneumonia patients coinfected with 2019 novel coronavirus and influenza virus in Wuhan, China. J Med Virol. 2020 doi: 10.1002/jmv.25781. DOI: 10.1002/jmv.25781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hellyer TP, McAuley DF, Walsh TS, Anderson N, Conway Morris A, Singh S, et al. Biomarker-guided antibiotic stewardship in suspected ventilator-associated pneumonia (VAPrapid2): a randomised controlled trial and process evaluation. Lancet Respir Med. 2020 Feb;8((2)):182–91. doi: 10.1016/S2213-2600(19)30367-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.CDC − Centers for Disease Control and Prevention Disinfection of healthcare equipment: guideline for disinfection and sterilization in healthcare facilities (2008) (cited2020 April) Available from: https://www.cdc.gov/infectioncontrol/guidelines/disinfection/healthcare-equipment.html.
- 17.DGP Empfehlung. Empfehlungen zur Durchführung einer Bronchoskopie in Zeiten der COVID-19-Pandemie (cited 2020 April 5) Available from: https://pneumologie.de/fileadmin/user_upload/Aktuelles/2020-03-21_DGP_Bronchoskopie_Covid-19.pdf. [DOI] [PMC free article] [PubMed]