Highlights
-
•
Transcatheter aortic valve implantation (TAVI) outcome is comparable to surgery.
-
•
How TAVI patients fare compared to the general population is not fully understood.
-
•
Relative survival was used to compare TAVI patients to the Dutch population.
-
•
Survival after TAVI is for patients >80 years similar to the general population.
-
•
Quality of life is comparable to that of the general population after TAVI.
Keywords: TAVI, Survival, Quality of life
Abbreviations: AS, Aortic valve Stenosis; CBS, Statistics Netherlands; NHR, Netherlands Heart Registration; RS, Relative Survival; SAVR, Surgical Aortic Valve Replacement; TAVI, Transcatheter Aortic Valve Implantation; QoL, Quality of Life
Abstract
Background
Little is known about survival and quality of life (QoL) of patients treated by transcatheter aortic valve implantation (TAVI) compared to the age- and sex-matched general population. In this study we compared subgroups of the National Heart Registration TAVI cohort to the Dutch age- and sex-matched population at the level of survival and QoL.
Methods and results
From the Netherlands Heart Registration (NHR) the TAVI cohort (5489 patients, period 2013–2017) was extracted. These data were compared to the national Dutch population data collected from the national statistics office, Statistics Netherlands (CBS). Subgroups were defined according to sex and age (<65, 65–80 and >80). For QoL analyses the age subgroups <65, 65–75 and >75 were used. Long term survival was significantly higher in the general population compared to the TAVI population. Elderly TAVI patients (>80 years) had the same survival as the age-matched general population (46vs43% at 5 years, respectively). Survival in women was better than in men in both the general population and the TAVI cohort. Patients treated by TAVI, aged 65 years and older had a comparable QoL to that of the general population.
Conclusions
This study shows that TAVI patients aged 80 years and older have a similar long-term survival as an age-matched general population. However, because of lower survival in under 80 TAVI patients, the overall long term survival of all TAVI patients is worse than that of the general population in the Netherlands. This study also suggests that QoL after TAVI treatment is comparable to QoL in the general population.
1. Introduction
Aortic valve stenosis (AS) is an insidious disease with high mortality when symptoms develop [1], [2]. The development of symptoms is an indication for interventional treatment [3]. Recent large randomized controlled trials revealed that transcatheter aortic valve implantation (TAVI) is a good alternative for surgery, even in low-risk patients [4], [5], [6]. This has led to TAVI being incorporated into the European and American guidelines for treatment of AS [7], [8].
The landmark PARTNER trial unveiled the survival benefit TAVI has compared to medical therapy in a high-risk population unsuited for surgery [9]. The cardiovascular death rates in this trial were significantly lower in the TAVI arm at 1 and 5 years compared to medical therapy (20.5% vs 44.6% and 71.8% vs 93.6% respectively). The high mortality rate of inoperable patients of over 90% at 5 years clearly illustrated the devastating effect of aortic valve stenosis when left untreated. When TAVI was first tested versus surgical aortic valve replacement (SAVR) in high-risk patients, the mortality rate at 1 year and 5 years was comparable (24.2% compared to 26.8% and 67.8% and 62.4%, respectively) [10], [11]. Meanwhile the procedural risk of TAVI decreased due to important technical improvements to the valve-implants and delivery systems, at least in part explaining the lower mortality rate of 6.7% in intermediate risk patients [4]. Recently in the PARTNER 3 and the Evolute TAVR trials, TAVI was investigated in the low-risk population, with an even lower mortality rate as a result (1.0–2.5%) [5], [6].
The aforementioned studies also investigated parameters regarding quality of life (QoL) after intervention; TAVI showed larger improvement in QoL than medical therapy and 1 year after intervention there was no difference in QoL between TAVI and SAVR [5], [6].
Based on the overwhelming evidence from large clinical trials, indication for TAVI is continuously expanding, culminating in globally increasing numbers of AS patients that are treated by intervention and by TAVI in particular. This expansion of treatment and subsequent increase in health care expenditure is inevitable and therefore raises important questions about using resources in proper patients subgroups, or in other words: do some patient subgroups benefit more from intervention by TAVI than other subgroups? From a Value Based Health Care standpoint impact of TAVI on survival but also on QoL in different subgroups compared to matched subgroups of the general population is of essence.
In this study we compared subgroups of the Netherlands Heart Registration (NHR) TAVI cohort to the Dutch age- and sex-matched population and compared the TAVI cohort subgroups to each other at the level of survival and QoL to see if particular subgroups benefit TAVI treatment.
2. Methods
2.1. TAVI data
TAVI data were extracted from the value-based healthcare (VBHC) program which is part of the Netherlands Heart Registration (NHR). In the program, that focusses on measuring and improving outcomes that matter most to patients, Dutch cardiac centres submit procedural, baseline characteristics and outcome data on all complex cardiac procedures. In total 12 out of 16 cardiac centres in the Netherlands participated in this study. Advanced and certified data quality control systems are in place to ensure completeness and quality of data with the last audit completed in 2017. Detailed information about the NHR has been published previously [12]. A total of >100 variables are recorded including patient demographics, procedural characteristics, procedural complications and outcome at 30 days and follow-up outcomes. For this analysis, the NHR TAVI data from 2013 to 2017 were extracted. Missing data and data before 2013, as it was not complete, were excluded. Mortality data was checked by the Dutch personal records database. QoL was assessed with the SF-36 questionnaire [13] and was available for 2017 in 4 centres.
2.2. General population data
The national statistics office, Statistics Netherlands (CBS) collects data from people, companies and institutions (for further information: microdata@cbs.nl). Anonymized mortality data and QoL for the general Dutch population were extracted from the CBS for the time period 2013–2017. The QoL questionnaire is based on questions developed by the CBS including health status.
2.3. Statistical methods
Three age groups were used for survival analysis starting with age older than 80 years corresponding to the big TAVI trials [9], [11]. Then 65–80 years as a middle-aged group and younger than 65 years, matching to the groups in the CBS database. Week by week mortality data were obtained from the life tables of the CBS for the different groups based on age and sex. From these numbers, life tables were created in Excel version 1905 (Microsoft, Redmond, Washington, United States). With the CBS and NHR TAVI database life tables survival curves were created. To statistically compare the separate survival curves between subgroups, the log-rank test was used. Analyses were conducted for the entire TAVI population and for age- and sex-subgroups at 5 years. For continuous time analyses see the relative survival analyses in the supplementary material. The TAVI subgroups were also compared to each other. Landmark analyses at 30 days after the procedure were performed to exclude procedural complications. Subgroup analyses were performed for two periods (2013–2014 and 2015–2017) to demonstrate potential differences in time as operator skill and devices improve over the years.
For the QoL comparison the age groups were divided differently into three age-groups (75 years and older, 65–75 years, and younger than 65) as these were the categories available in the CBS database. As the age limit in the guidelines [7], [8] is reduced to 75 this will give insight into current qualitative TAVI outcomes. Another analysis was performed to look at sex differences. QoL was based on the first question of the SF-36 as used by the NHR in the TAVI cohort, asking generally about the patients quality of life after 1 year of follow-up. The percentage of patients having ‘at least a good’ QoL was compared to the percentage of people having ‘at least a good QoL’ in the CBS database. Only descriptive results were reported regarding the QoL analysis.
Analyses were performed using R version 3.5.2 (R Foundation for Statistical Computing, Vienna, Austria). We employed standard statistical techniques. Applicable tests were two-tailed, and p < 0.05 was considered statistically significant. Multivariate analysis was performed with the transformation model as no assumptions are made about the relationship between observed and expected survival [14]. The study was in compliance with the Declaration of Helsinki.
3. Results
Between January 1, 2013 and December 31, 2017, data of 5498 patients were included. This is 76.96% of the total TAVI procedures performed in the Netherlands in this time period. Baseline characteristics are displayed in supplement Table 1. Mean age of the TAVI cohort was 80 ± 7 years, 50% was female. Mean follow-up was 1.95 years. Table 1 provides baseline characteristics for each TAVI age-group. In the older age group (>80 years) the percentage of women was higher (57.2% vs 46.2% vs 40.7%; p < 0.001). The patients <65 years had more often renal disease (p < 0.001), lower left ventricular ejection fraction (p < 0.001) and chronic obstructive pulmonary disease (p < 0.001) compared to the other age groups. Peripheral vascular disease was more frequently present in the 65–80 age cohort (p < 0.001), reflected by a higher percentage of transaortic or transapical TAVI in this group. The percentage EuroScore, reflecting procedural risk, was lower in the younger age group than in the older age group.
Table 1.
Baseline and procedural characteristics of the TAVI population across age subgroups.
| TAVI population |
||||
|---|---|---|---|---|
| Variable | Aged <65 y (n = 167) | Aged 65–80 y (n = 2268) | Aged >80 y (n = 3063) | p Value* |
| Age (years) | 60 ± 6 | 75 ± 4 | 85 ± 3 | <0.001 |
| Female | 68 (40.7%) | 1048 (46.2%) | 1753 (57.2%) | <0.001 |
| Risk factors | ||||
| Diabetes mellitus | <0.001 | |||
| Nondiabetic | 108 (65.9%) | 1485 (67.5%) | 2312 (78.2%) | |
| No treatment | 2 (3.7%) | 5 (0.2%) | 10 (0.3%) | |
| Dietary control | 8 (4.9%) | 123 (5.6%) | 112 (3.8%) | |
| Oral medication | 21 (12.8%) | 360 (16.4%) | 382 (12.9%) | |
| Insulin | 25 (15.2%) | 227 (10.3%) | 142 (4.8%) | |
| Renal function | <0.001 | |||
| GFR >60 | 103 (62.0%) | 1125 (49.8%) | 1357 (44.4%) | |
| GFR 30–59 | 37 (22.3%) | 963 (42.6%) | 1500 (49.1%) | |
| GFR 15–29 | 18 (10.8%) | 123 (5.4%) | 172 (5.6%) | |
| GFR <15 | 8 (4.8%) | 47 (2.1%) | 25 (0.8%) | |
| BMI (kg/m2) | 29.0 ± 6.7 | 28.2 ± 5.4 | 26.5 ± 4.1 | <0.001 |
| Cardiovascular and pulmonary disease | ||||
| Previous cardiac surgery | 43 (25.9%) | 709 (31.4%) | 477 (15.6%) | <0.001 |
| Previous cerebral vascular disease | 21 (12.6%) | 304 (13.4%) | 363 (11.9%) | 0.243 |
| Peripheral vascular disease | 35 (21.0%) | 607 (26.8%) | 538 (17.6%) | <0.001 |
| COPD | 62 (37.1%) | 624 (27.7%) | 556 (18.2%) | <0.001 |
| Ejection fraction | ||||
| Left ventricular EF | <0.001 | |||
| >50% | 84 (50.6%) | 1289 (57.9%) | 1969 (65.5%) | |
| 30–50% | 50 (30.1%) | 750 (33.7%) | 896 (29.8%) | |
| <30% | 32 (19.3%) | 186 (8.4%) | 143 (4.8%) | |
| Symptoms | ||||
| NYHA heart failure | 0.035 | |||
| class I | 15 (9.0%) | 253 (11.2%) | 356 (11.6%) | |
| class II | 32 (19.2%) | 430 (19.0%) | 634 (20.7%) | |
| class III | 84 (50.3%) | 1083 (47.8%) | 1465 (47.8%) | |
| class IV | 19 (11.4%) | 144 (6.4%) | 167 (5.5%) | |
| CCS angina class IV | 2 (1.2%) | 48 (2.1%) | 69 (2.3%) | 0.2 |
| Procedure | ||||
| Access route | <0.001 | |||
| TF access | 123 (73.7%) | 1710 (75.6%) | 2538 (82.9%) | |
| TA access | 19 (11.4%) | 257 (11.4%) | 203 (6.6%) | |
| TAo access | 16 (9.6%) | 260 (11.5%) | 276 (9.0%) | |
| Other access | 7 (4.2%) | 33 (1.5%) | 44 (1.4%) | |
| EuroSCORE I | <0.001 | |||
| low <10% | 104 (67.5%) | 780 (36.4%) | 451 (15.6%) | |
| intermediate 10–20% | 31 (20.1%) | 813 (37.9%) | 1454 (50.3%) | |
| high >20% | 19 (12.3%) | 550 (25.7%) | 985 (34.1%) | |
| EuroSCORE II | <0.001 | |||
| low <5% | 63 (70.8%) | 892 (62.9%) | 1137 (60.6%) | |
| intermediate 5–10% | 17 (19.1%) | 347 (24.5%) | 504 (26.9%) | |
| high >10% | 9 (10.1%) | 180 (12.7%) | 234 (12.5%) | |
Abbreviations: TAVI = Transcatheter Aortic Valve Implantation; GFR = Glomerular Filtration Rate; BMI = Body Mass Index; COPD = Chronic Obstructive Pulmonary Disease; EF = Ejection Fraction; NYHA = New York Heart Association; CCS = Canadian Cardiovascular Society; TF = Trans Femoral; TA = Trans Apical; TAo = Trans Aortic. Summary values represent number (%), mean ± standard deviation, or median (interquartile range, IQR).
Kruskal-Wallis and Chi-Squared test values.
In supplement Table 2 the TAVI cohort is divided by sex. The average age of men was lower (79 ± 7 vs 81 ± 6 years; p < 0.001). In the male patient cohort more patients were treated via the transapical route (p < 0.001) and a higher percentage had undergone cardiac surgery in the past (p < 0.001) compared to women.
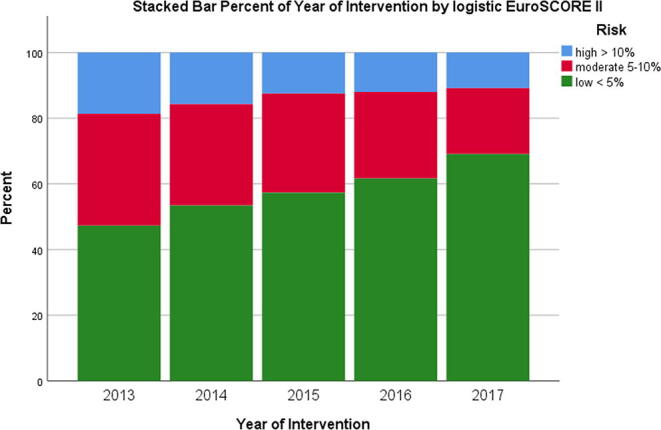
The different characteristics between the intervention periods are displayed in supplement Table 3. In the early intervention years, defined as the years 2013 and 2014, more often the transapical or transaortic route for TAVI was used (p < 0.001) and EuroScore was higher.
3.1. Survival analyses
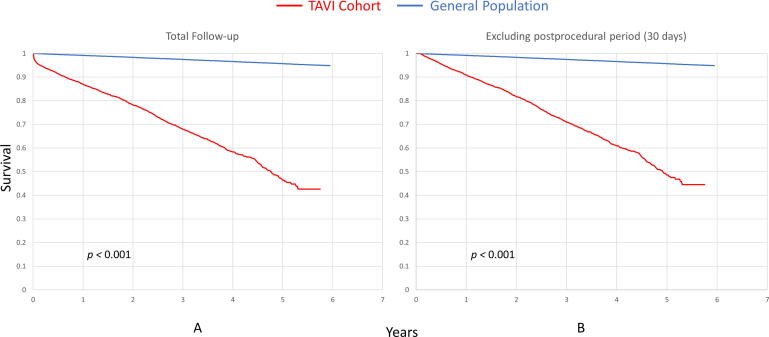
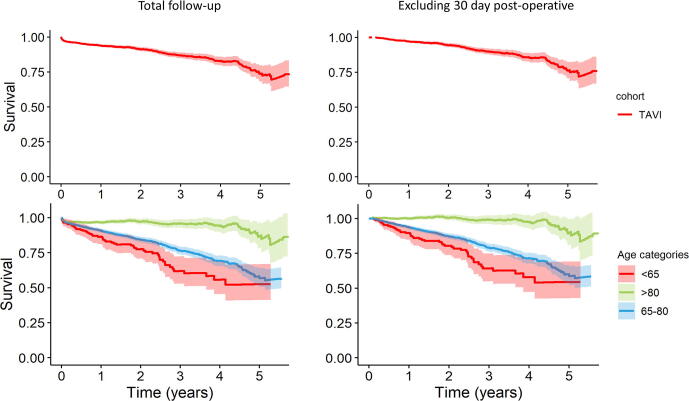
The survival rates of the NHR-TAVI cohort with that of the Dutch population are displayed in Fig. 1 and the relative survival in Figure Supplementary Fig. 1. The observed survival rate for the TAVI cohort at 30 days, 1-year and 5-years is 95.7%, 86.9% and 46.2%, respectively (supplement Table 5). The survival rate for TAVI patients is lower than that of the general.
Fig. 1.
Observed Survival in the TAVI Cohort versus the General Population. These survival curves reveal the difference in survival of the total transcatheter aortic valve implantation (TAVI) population versus the general Dutch population. In panel B the first 30 days of the postprocedural period are excluded to demonstrate the effect of improvements in pre-, peri- and postprocedural care. Differences shown as p values are calculated with the log-rank test.
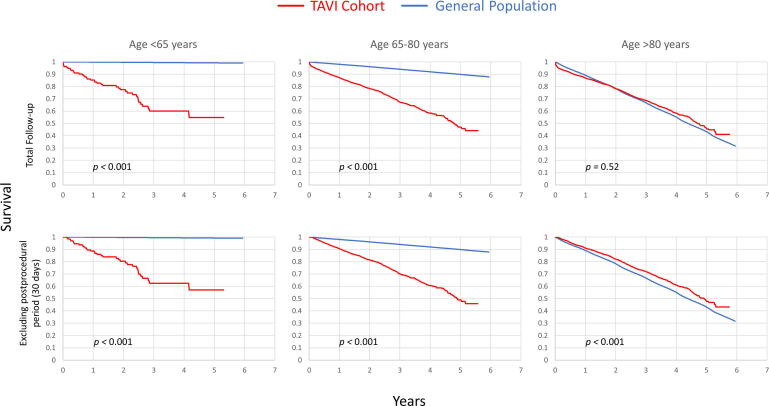
Fig. 2 shows the proportion of surviving patients in age-matched groups in the general population and in the TAVI cohort. Five year survival rate of the general population aged <65, 65–80, and >80 years was 99.2%, 89.9% and 43.2%, respectively. For the TAVI cohort this is 54.8%, 47.1% and 45.6%, respectively. There was a significantly lower mortality in the general population aged <65 and 65–80 groups compared to their respective counterparts in the TAVI population (log-rank test, p < 0.001 and p < 0.001 respectively). There was no significant difference in survival among the TAVI age groups; younger than 65 years, 65–80 years of age and older than 80 (p = 0.66, p = 0.81, and p = 0.73, respectively). When survival of the general population over 80 years of age was compared to the survival of the different TAVI age groups no significant difference was found (in order of increased age, p = 0.82, p = 0.47 and p = 0.52). The survival of the TAVI patients >80 at 5 years was 46% compared to 43% of the age-matched general population. Landmark analyses showed that survival in the TAVI cohort aged 65–80 and >80 was favorable compared to survival of the general population >80 years (p < 0.001 and p < 0.001, respectively). This difference was not seen in the younger than <65 group compared to the general population over 80 (p = 0.56).
Fig. 2.
Observed Survival in the TAVI Cohort versus the General Population Across Age Subgroups. These survival curves are subdivided into different age groups as visible in the top. In the bottom the postprocedural period is excluded to demonstrate the effect of improvements in pre-, peri- and postprocedural care. There is no difference in survival between the transcatheter aortic valve implantation (TAVI) group aged 80 years and older and the general population. Excluding the first 30 days reveal that the TAVI group aged 80 years and older does better. In all other cases the general population fairs better. Differences shown as p values are calculated with the log-rank test.
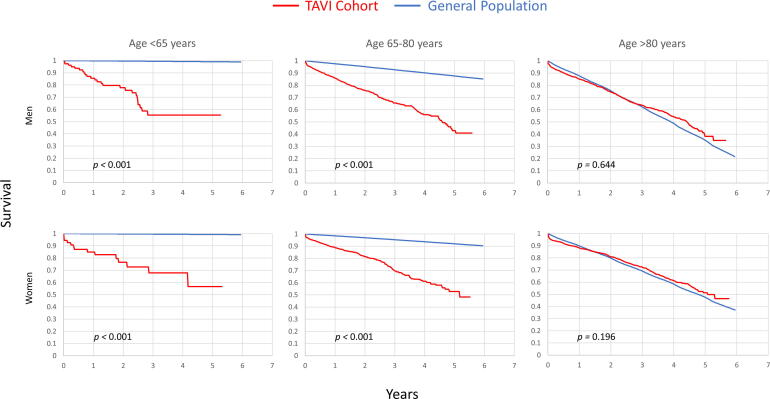
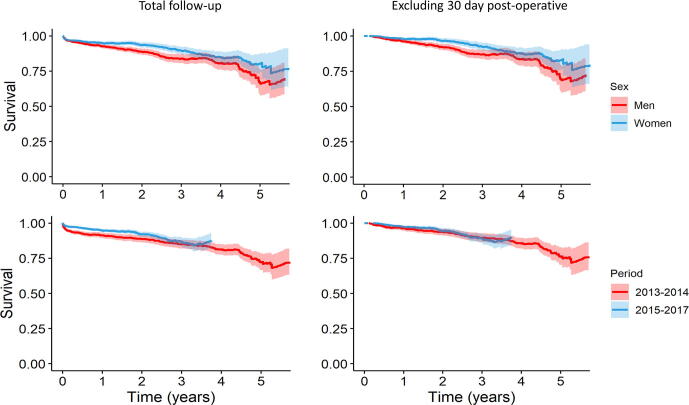
The differences in survival for men and women subdivided by age-groups undergoing TAVI are displayed in Fig. 3 and Figure Supplementary Fig. 2. Women do better than men (p < 0.001).
Fig. 3.
Observed Survival in the TAVI Cohort versus the General Population Across Sex and Age Subgroups. These survival curves are subdivided into different age groups as visible in the top and between men and women. There is no difference in survival between the transcatheter aortic valve implantation (TAVI) group aged 80 years and older and the general population in both men and women. Men in general do worse than women as is also visible in supplement Fig. 3. Differences shown as p values are calculated with the log-rank test.
The multivariate analysis (supplement Table 6) shows that older age groups and later intervention period have a positive influence on the survival rate.
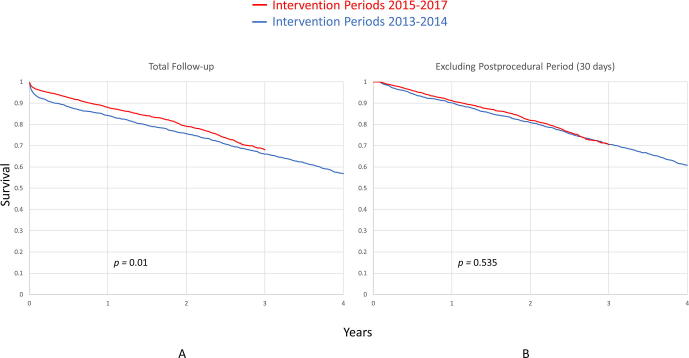
Figure Supplementary Fig. 3 shows the survival curves per intervention period. In the first period, 2013–2014, there is a higher mortality rate compared to that of the later years 2015–2017 (p = 0.01). Performing the same comparison but using a landmark analyses showed that both groups almost align (p = 0.535).
3.2. Quality of life analyses
The results of the QoL question are displayed in supplement Table 7. Only 7 patients answered the question in the age group younger than 65 from the TAVI cohort and these results were therefore not used for comparison. Health experience after TAVI was comparable between the age groups 65–75 and >75. Men, both in the TAVI cohort and in the general population, scored higher on the QoL question compared to women.
4. Discussion
In this study long-term survival in the TAVI population was lower than that of the general Dutch population. However, the matched age TAVI group of 80 years and older showed survival equal to the matched general population. Moreover, the survival of women seems better than that of men across each age group defined.
Potential mechanisms that might explain this prior finding are the fact that TAVI patients are thoroughly selected for treatment implying that people with a poor prognosis are therefore excluded from this cohort. Because we also know from randomized data in elderly patients that TAVI patients have better prognosis than elderly patients with severe, symptomatic AS that are treated conservatively, the relatively good survival for elderly TAVI patients compared to the general population enforces the current clinical opinion that TAVI should not be declined because of older age only [15]. When procedural related death was excluded from analysis, the results improved further restoring the normal life expectancy in the elderly TAVI patients. This finding illustrates that further improvements in the procedure and devices could realize an even greater survival benefit.
TAVI patients younger than 65 years and aged 65–80 did worse than their counterparts in the general population. They progressed the same way as the 80 years and older population. This is not surprising since previous guideline selection criteria state that patients younger than 80 are only eligible for TAVI if they are unable to undergo SAVR. This selection is associated with more comorbidities in the under 80 patients which consequently results in a lower survival rate. Another plausible explanation could be that younger patients are operated on in a later stage of the disease since they have more compensatory mechanisms than older patients, masking their symptoms. However, both described possible theories still unlikely explain the relatively high mortality rate in younger patients with AS fully. How to improve AS care in younger patients is one of the important questions for future research.
Overall women performed better than men with respect to long-term survival after TAVI. This finding was not an age-dependent phenomenon reflected in the fact that this trend was seen for each of these age subgroups (Fig. 3). In the general population men and women have a similar overall survival, but survival is better for women of older age.
When looking at survival based in different intervention time periods, the years 2013 and 2014 showed worse survival after TAVI than the years 2015 till 2017. First, this trend is in part explained by improvement in procedural technique and materials over time as shown by the decreasing percentage of post-procedural complications over the years as seen in a study by Arai et al. [16], [17]. The improvement in survival after TAVI is also in part explained by the fact that the less complex patients were increasingly accepted for treatment. Before 2014, only inoperable patients were selected for TAVI. After 2014, high risk patients were also accepted for intervention. This is reflected in the population, as the risk score is getting lower over the years (see supplement Table 3, Figure Supplementary Fig. 4 and Figure Supplementary Fig. 5). When the post-procedural period of 30 days after TAVI is excluded from analysis, survival curves in both intervention periods (2013–2014 and 2015–2017 respectively) align, implicating that mortality differences over time are most likely attributable to changes in TAVI procedure and patient management in the direct post-interventional period (Figure Supplementary Fig. 2 and Figure Supplementary Fig. 3). This was also visible in the multivariate analysis where age- and period-categories influence survival rate. Longer follow-up and device specific data are needed to explain these initial findings.
QoL, as assessed from a questionnaire 1 year after TAVI was comparable with the general population in the age groups 65 until 75 and 75 years and older (supplement Table 7). This finding is of great interest because we know from randomized trial data [5], [6] that QoL in severe AS patients pre-treatment is poor and the finding in this study that QoL 1 year after treatment is comparable to QoL in the general Dutch population indicates the important positive impact TAVI can have on QoL outcome. QoL is an important factor for patients and our findings suggest considering QoL when discussing AS treatment with TAVI, also in older patients.
4.1. Comparison to existing literature
In a study by Martin et al. [18] the national UK TAVI registry was used to calculate the relative survival after TAVI. They analyzed 6420 patients and compared them in three groups to the general population; aged younger than 80, between 80 and 85, and older than 85. The patients aged 85 and older approximated the survival of a matched general population within 3 years. The other age groups did worse than the general population. This is in part in line with the findings in our study, however, the 80 year and older cohort approximated the survival of the general population within roughly 1.5 years (survival of 84% vs 83%). Thereafter this cohort did even better than the general population with respect to survival. This could be explained by the different age groups definition. Furthermore, in our current study we investigated procedures from 2013 until 2017 with guideline criteria for undergoing TAVI. Martin et al used a dataset ranging from 2007 until 2014 including the beginning of the TAVI era (2007–2012) with lower operator skills and poorer device performance explaining difference in outcome with our study. Our study and the study by Martin et al. both conclude that older patients should not be denied treatment just because of age.
Another recent study analyzed SAVR patients from the SWEDEHEART registry [19] and compared them to the general population. The study included 23,528 patients undergoing SAVR between 1995 and 2013 with or without concomitant coronary artery bypass grafting. The mean follow-up time in this study was 6.8 years with a maximum of 19 years. The survival rate of patients 80 years and older at 5 years was 68.5% compared to 48% in our cohort. Survival in the lower age groups was even better. As our cohort includes patients that could not undergo SAVR this will predominantly explain the difference in survival rate between these studies. Presence of comorbidities was also higher in our cohort. Survival of patients with symptomatic severe AS if left untreated is lower than 50% at 2 years [20] enforcing that this devastating disease is better off with TAVI treatment.
4.2. Limitations and strengths
There are some limitations to our study. We did not exclude TAVI patients from the general population since this was not possible. This could be prone to bias but the impact of such a small cohort on the entire population is considered negligible (5490 vs 16,779,575 in the national cohort).
Strict guideline criteria were used to select patients for TAVI procedure which leads to lower comorbidity rates. This selection bias could not be excluded as the NHR population was deemed fit for TAVI treatment. The younger than 65 patients group did not contain all age ranges as in the Dutch general population under 65 years which is potential bias for the results of the younger age groups.
The QoL analyses were not based on full questionnaires because of different questionnaires used by NHR and CBS. We only used one comparable QoL question for our study. Only a small cohort in a couple of hospitals was available for the QoL analyses. Despite this aforementioned limitation we would like to point out that the strength of this study is that to our knowledge for the first time QoL after TAVI, an important determinant of treatment success, was compared to QoL in the general population in the Netherlands.
5. Conclusions
In conclusion, this study shows that patients of 80 years and older who were selected for TAVI treatment have a similar survival rate compared to an age- and sex-matched general population. It also suggests that QoL outcomes after TAVI are similar compared to the general population. Younger patients did not do so well compared to the general population. Whether this latter finding will change in the future in the positive direction for TAVI when low risk patients will be treated, is to be investigated.
Funding
None.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijcha.2020.100536.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
Supplementary Fig. 1.
Supplementary Fig. 2.
Supplementary Fig. 3.
Supplementary Fig. 4.

Supplementary Fig. 5.
References
- 1.Turina J., Hess O., Sepulcri F., Krayenbuehl H.P. Spontaneous course of aortic valve disease. Eur. Heart J. 1987;8:471–483. doi: 10.1093/oxfordjournals.eurheartj.a062307. [DOI] [PubMed] [Google Scholar]
- 2.Lancellotti P., Magne J., Dulgheru R., Clavel M.A., Donal E., Vannan M.A., Chambers J., Rosenhek R., Habib G., Lloyd G., Nistri S., Garbi M., Marchetta S., Fattouch K., Coisne A., Montaigne D., Modine T., Davin L., Gach O., Radermecker M., Liu S., Gillam L., Rossi A., Galli E., Ilardi F., Tastet L., Capoulade R., Zilberszac R., Vollema E.M., Delgado V., Cosyns B., Lafitte S., Bernard A., Pierard L.A., Bax J.J., Pibarot P., Oury C. Outcomes of patients with asymptomatic aortic stenosis followed up in heart valve clinics. JAMA Cardiol. 2018;3:1060–1068. doi: 10.1001/jamacardio.2018.3152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carabello B.A., Paulus W.J. Aortic stenosis. Lancet. 2009;373:956–966. doi: 10.1016/S0140-6736(09)60211-7. [DOI] [PubMed] [Google Scholar]
- 4.Cahill T.J., Chen M., Hayashida K., Latib A., Modine T., Piazza N., Redwood S., Prendergast B.D., Søndergaard L. Transcatheter aortic valve implantation: current status and future perspectives. Eur. Heart J. 2018;39:2625–2634. doi: 10.1093/eurheartj/ehy244. [DOI] [PubMed] [Google Scholar]
- 5.Popma J.J., Deeb G.M., Yakubov S.J., Mumtaz M., Gada H., O’Hair D., Bajwa T., Heiser J.C., Merhi W., Kleiman N.S., Askew J., Sorajja P., Rovin J., Chetcuti S.J., Adams D.H., Teirstein P.S., Zorn G.L., Forrest J.K., Tchétché D., Resar J., Walton A., Piazza N., Ramlawi B., Robinson N., Petrossian G., Gleason T.G., Oh J.K., Boulware M.J., Qiao H., Mugglin A.S., Reardon M.J. Transcatheter aortic-valve replacement with a self-expanding valve in low-risk patients. N. Engl. J. Med. 2019 doi: 10.1056/NEJMoa1816885. [DOI] [Google Scholar]
- 6.Mack M.J., Leon M.B., Thourani V.H., Makkar R., Kodali S.K., Russo M., Kapadia S.R., Malaisrie S.C., Cohen D.J., Pibarot P., Leipsic J., Hahn R.T., Blanke P., Williams M.R., McCabe J.M., Brown D.L., Babaliaros V., Goldman S., Szeto W.Y., Genereux P., Pershad A., Pocock S.J., Alu M.C., Webb J.G., Smith C.R. Transcatheter aortic-valve replacement with a balloon-expandable valve in low-risk patients. N. Engl. J. Med. 2019;NEJMoa1814052 doi: 10.1056/NEJMoa1814052. [DOI] [PubMed] [Google Scholar]
- 7.Nishimura R.A., Otto C.M., Bonow R.O., Carabello B.A., Erwin J.P., Fleisher L.A., Jneid H., Mack M.J., McLeod C.J., O’Gara P.T., Rigolin V.H., Sundt T.M., Thompson A. AHA/ACC focused update of the 2014 AHA/ACC guideline for the management of patients with valvular heart disease. J. Am. Coll. Cardiol. 2017;70(2017):252–289. doi: 10.1016/j.jacc.2017.03.011. [DOI] [PubMed] [Google Scholar]
- 8.Falk V., Baumgartner H., Bax J.J., De Bonis M., Hamm C., Holm P.J., Iung B., Lancellotti P., Lansac E., Muñoz D.R., Rosenhek R., Sjögren J., Tornos Mas P., Vahanian A., Walther T., Wendler O., Windecker S., Zamorano J.L. ESC/EACTS Guidelines for the management of valvular heart disease. Eur. J. Cardiothorac. Surg. 2017;52(2017):616–664. doi: 10.1093/ejcts/ezx324. [DOI] [PubMed] [Google Scholar]
- 9.Leon M.B., Smith C.R., Mack M., Miller D.C., Moses J.W., Svensson L.G., Tuzcu E.M., Webb J.G., Fontana G.P., Makkar R.R., Brown D.L., Block P.C., Guyton R.A., Pichard A.D., Bavaria J.E., Herrmann H.C., Douglas P.S., Petersen J.L., Akin J.J., Anderson W.N., Wang D., Pocock S. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N. Engl. J. Med. 2010;363:1597–1607. doi: 10.1056/NEJMoa1008232. [DOI] [PubMed] [Google Scholar]
- 10.Thourani V.H., Kodali S., Makkar R.R., Herrmann H.C., Williams M., Babaliaros V., Smalling R., Lim S., Malaisrie S.C., Kapadia S., Szeto W.Y., Greason K.L., Kereiakes D., Ailawadi G., Whisenant B.K., Devireddy C., Leipsic J., Hahn R.T., Pibarot P., Weissman N.J., Jaber W.A., Cohen D.J., Suri R., Tuzcu E.M., Svensson L.G., Webb J.G., Moses J.W., MacK M.J., Miller D.C., Smith C.R., Alu M.C., Parvataneni R., D’Agostino R.B., Leon M.B. Transcatheter aortic valve replacement versus surgical valve replacement in intermediate-risk patients: a propensity score analysis. Lancet. 2016;387:2218–2225. doi: 10.1016/S0140-6736(16)30073-3. [DOI] [PubMed] [Google Scholar]
- 11.Smith C.R., Leon M.B., Mack M.J., Miller D.C., Moses J.W., Svensson L.G., Tuzcu E.M., Webb J.G., Fontana G.P., Makkar R.R., Williams M., Dewey T., Kapadia S., Babaliaros V., Thourani V.H., Corso P., Pichard A.D., Bavaria J.E., Herrmann H.C., Akin J.J., Anderson W.N., Wang D., Pocock S.J. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N. Engl. J. Med. 2011;364:2187–2198. doi: 10.1056/NEJMoa1103510. [DOI] [PubMed] [Google Scholar]
- 12.NHR, NHR Publicatie Registratie, 2018. https://nederlandsehartregistratie.nl/wp-content/uploads/2018/12/NHR_Publicatie_Registratie_2018.pdf.
- 13.Ware J.E. SF-36 health survey update. Spine (Phila Pa. 1976) 2000;25:3130–3139. doi: 10.1097/00007632-200012150-00008. [DOI] [PubMed] [Google Scholar]
- 14.Stare J., Henderson R., Pohar M. An individual measure of relative survival. J. R. Stat. Soc. Ser. C (Appl. Stat.) 2005;54:115–126. doi: 10.1111/j.1467-9876.2005.00473.x. [DOI] [Google Scholar]
- 15.Vendrik J., van Mourik M.S., van Kesteren F., Henstra M.J., Piek J.J., Henriques J.P.S., Wykrzykowska J.J., de Winter R.J., Marije Vis M., Koch K.T., Baan J. Corrigendum to “Comparison of Outcomes of Transfemoral Aortic Valve Implantation in Patients <90 to Those >90 Years of Age” [American Journal of Cardiology (2018) 1581-1586] Am. J. Cardiol. 2018;122:2173–2175. doi: 10.1016/j.amjcard.2018.07.010. [DOI] [PubMed] [Google Scholar]
- 16.Arai T., Lefèvre T., Hovasse T., Hayashida K., Watanabe Y., O’Connor S.A., Benamer H., Garot P., Cormier B., Bouvier E., Morice M.C., Chevalier B. Evaluation of the learning curve for transcatheter aortic valve implantation via the transfemoral approach. Int. J. Cardiol. 2016;203:491–497. doi: 10.1016/j.ijcard.2015.10.178. [DOI] [PubMed] [Google Scholar]
- 17.van Kesteren F., van Mourik M.S., Wiegerinck E.M.A., Vendrik J., Piek J.J., Tijssen J.G., Koch K.T., Henriques J.P.S., Wykrzykowska J.J., de Winter R.J., Driessen A.H.G., Kaya A., Planken R.N., Vis M.M., Baan J. Trends in patient characteristics and clinical outcome over 8 years of transcatheter aortic valve implantation. Netherlands Hear. J. 2018;26:445–453. doi: 10.1007/s12471-018-1129-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Martin G.P., Sperrin M., Hulme W., Ludman P.F., de Belder M.A., Toff W.D., Alabas O., Moat N.E., Doshi S.N., Buchan I., Deanfield J.E., Gale C.P., Mamas M.A. Relative survival after transcatheter aortic valve implantation: how do patients undergoing transcatheter aortic valve implantation fare relative to the general population? J. Am. Heart Assoc. 2017;6 doi: 10.1161/jaha.117.007229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Glaser Natalie, Persson Michael, Jackson Veronica, Holzmann Martin J., Franco-Cereceda Anders, Sartipy Ulrik. Loss in life expectancy after surgical aortic valve replacement. J. Am. Coll. Cardiol. 2019;74(1):26–33. doi: 10.1016/j.jacc.2019.04.053. [DOI] [PubMed] [Google Scholar]
- 20.Rosenhek R., Zilberszac R., Schemper M., Czerny M., Mundigler G., Graf S., Bergler-Klein J., Grimm M., Gabriel H., Maurer G. Natural history of very severe aortic stenosis. Circulation. 2010;121:151–156. doi: 10.1161/CIRCULATIONAHA.109.894170. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.