Highlights
-
•
Opt-in text messaging is a feasible option to promote the uptake of mailed FIT screening.
-
•
The addition of a lottery-based incentive did not improve screening completion rates.
-
•
Patients found text messaging to be acceptable and convenient.
Keywords: Colorectal cancer, Screening, Text messaging, Incentives
Abstract
Efforts to boost colorectal cancer (CRC) screening rates in underserved populations have been limited by effectiveness and scalability. We evaluate the impact of adding a lottery-based financial incentive to a text messaging program that asks patients to opt-in to receive mailed fecal immunochemical testing (FIT).
This is a two-arm pragmatic randomized controlled trial at a community health center in Southwest Philadelphia from April to July 2017. We included CRC screening-eligible patients between ages 50–74 years who had a mobile phone, active health insurance, and at least one visit to the clinic in the past 12 months. Patients received a text message about CRC screening with the opportunity to opt-in to receive mailed FIT. They were randomized 1:1 to the following: (1) text messaging outreach alone (text), or (2) text messaging with lottery for a 1-in-5 chance of winning $100 after FIT completion (text + lottery). The primary outcome was the percentage of patients completing the mailed FIT within 3 months of initial outreach.
281 patients were included in the intent-to-treat analysis. The FIT completion rate was 12.1% (95% CI, 6.7%–17.5%) in the text message arm and 12.1% (95% CI, 6.7%–17.5%) in the lottery arm, with no statistical difference between arms. The majority of post-intervention interview respondents found text messaging to be acceptable and convenient.
Opt-in text messaging is a feasible option to promote the uptake of mailed FIT screening, but the addition of a lottery-based incentive did not improve completion rates.
Trial Registration: clinicaltrials.gov (NCT03072095).
1. Introduction
Despite ongoing efforts to promote uptake, colorectal cancer (CRC) screening rates remain low, particularly at community health centers that care for underserved populations, where median practice screening rates are approximately 31% (Mandel et al., 1993, Schoen et al., 2012, Siegel et al., 2018, White et al., 2017, Baker et al., 2015). Screening in the United States is predominantly offered to patients in a clinic setting, but other clinical demands often compete, and many patients do not complete recommended testing. Outreach to patients has been shown to boost screening rates, often by mailing fecal immunochemical tests (FIT) to patients’ homes, but these often rely on conventional communication tools such as letters or phone calls, which can be inefficient or ineffective for underserved populations (Mehta et al., 2016a, Green et al., 2013, Dougherty et al., 2018, Coronado et al., 2018).
Text messaging has become a dominant form of modern communication, enabling asynchronous communication from just about anywhere, and transcending social and economic barriers (October, 2019). It has been used to improve health outcomes in areas such as weight loss, smoking cessation, and diabetes management (Cole-Lewis and Kershaw, 2010), and there is some evidence from interventions to improve CRC screening (Muller et al., 2017, Hagoel et al., 2016, Hirst et al., 2017). Instead of mailing out FIT kits to all patients, with the majority of kits not returned, there is an opportunity to use bidirectional text messages to engage patients in the process and distribute kits only to those requesting them. This may help to make FIT outreach more efficient, particularly for community health centers with limited resources.
Behavioral economic principles can be embedded in a text messaging and mailed FIT program to increase uptake of CRC screening. Behavioral economics offers insights about cognitive biases, and how these can be leveraged to improve health behavior (Tversky and Kahneman, 1981, Loewenstein et al., 2007, Mehta and Asch, 2014). By asking patients if they would like to participate in screening before sending the kit, we can leverage pre-commitment to potentially increase engagement (Schwartz et al., 2014, Gollwitzer and Sheeran, 2006). Prompting people to form plans about completing an intended behavior has been shown to increase participation in activities such as vaccination and cancer screening (Milkman et al., 2011, Milkman et al., 2013). Financial incentives can also be offered to patients to overcome present bias, and lottery-based incentives may be more motivating than fixed incentives of the same expected value, as people may overestimate their chances of winning (Volpp et al., 2009, Volpp et al., 2006, Volpp et al., 2008, Haisley et al., 2012). For example, a study offering a 1 in 10 chance of $50 for completion fecal occult blood testing had greater participation than fixed incentives (Kullgren et al., 2014).
In this study, we evaluated the impact of adding a lottery-based financial incentive to a bidirectional text messaging program that asks patients to opt-in to receive mailed FIT at a community health center with a baseline screening rate of approximately 19%.
2. Materials and methods
2.1. Study design
This was a two-arm pragmatic randomized controlled trial comparing the impact of bidirectional text messaging for mailed FIT alone or combined with a lottery-based financial incentive. The two arms included: (1) opt-in text messaging outreach alone (text), or (2) opt-in text messaging with a 1-in-5 chance of winning a $100 gift card after FIT completion (text + lottery). The University of Pennsylvania Institutional Review Board approved the study. A waiver of informed consent was obtained since the protocol posed no more than minimal risk to participants and could not be practicably carried out without the waiver (Asch et al., 2017). The protocol was registered at clinicaltrials.gov (NCT03072095), and the protocol and statistical analysis plan appear as a Supplement.
2.2. Study population
The study population included patients at Family Practice & Counseling Network/ Health Annex, a federally qualified community health center serving a socioeconomically underserved population in Southwest Philadelphia. The population is mainly black, insured by Medicaid, and has a household income less than $30,000 per year. Patients were identified via an automated data pull from the electronic health record (EHR) from February to April 2017. We included patients between ages 50–74 years who had a mobile phone enabled to send and receive text messaging, active health insurance, at least one visit to the clinic in the past 12 months, and were due for CRC screening. Screening eligibility was defined as not having had a colonoscopy in the past 10 years, flexible sigmoidoscopy in the last 5 years, or stool testing in the past 12 months. Chart review for all patients was performed by research staff after automated data pull to confirm eligibility. Exclusion criteria were: a personal history of CRC or other gastrointestinal cancer, inflammatory bowel disease, colon polyps, colectomy, Lynch Syndrome, familial adenomatous polyposis syndrome, iron-deficiency anemia, a recent history of lower gastrointestinal bleeding, or a first degree relative with colorectal cancer. Patients were also excluded if they had a diagnosis of metastatic cancer, end stage renal disease, congestive heart failure, dementia, or liver cirrhosis because such conditions may compromise life expectancy and outweigh the benefits of screening. The investigators were blinded to patient data and randomization, but the research staff were not blinded as they were administering the interventions.
2.3. Interventions
Eligible patients were randomized in a 1:1 ratio using a computerized random number generator. Patients in the text messaging arm received an outreach message via a text messaging platform (Care Message) from the clinic describing the importance of colorectal cancer screening and requesting participation (Appendix 1). This is a commonly used platform that automates text messaging outreach and tracking of responses. They were asked to respond “Yes” in order to receive a home test kit. Those in the lottery incentive received the same text message and additional content indicating that s/he would be entered in a lottery with a 1-in-5 chance of receiving $100 when the FIT kit is completed and returned. This is similar to an effective incentive in a prior study (Kullgren et al., 2014), and the amount was thought to be feasible by the community health center. After 3 business days, a reminder text message was sent to encourage subjects to respond to the initial outreach. A final text reminder was sent following another 3 business days if no response to the initial outreach or first reminder had been received.
If the participant responded yes, s/he received a FIT kit mailed to the home. The FIT kit contained a sample collection tube, instructions on how to collect and mail the sample, information about CRC screening, a requisition form, a pre-paid return envelope, and instructions to return the completed kit within 3 months. FIT kits were mailed in batches. Batch 1 included all participants who responded affirmatively to the initial outreach or the first reminder text. Batch 2 included participants who responded affirmatively to the second reminder text. Participants not returning the kit at 3 and 5 weeks after FIT mailing received follow-up text messages reminding them to complete and return their kit and, for subjects in the lottery arm, their chance at winning a $100 gift card for returning their completed kit (“We sent a colon cancer screening test–complete & return w/included pre-paid envelope! Complete for a 1 in 5 chance at $100. Questions: xxx-xxx-xxxx”). Those that completed the FIT kit and were selected in the lottery were subsequently sent a $100 gift card.
All FIT results were sent to the patient’s primary care clinician, and patients with negative results received a letter. For patients with positive results, clinic staff contacted the patient directly to coordinate follow-up diagnostic colonoscopy. If after 5 attempts clinic staff were unable to make contact with the patient by phone, s/he received a follow-up letter explaining their results and requesting the patient contact the clinic.
2.4. Post-intervention interviews
Six months after the intervention, a random subsample of 100 participants (50 from each arm) was selected to receive a follow up semi-structured phone interview. The participants were asked to describe their qualitative experience with the outreach materials and interventions. Research staff made up to three attempts to contact the selected participants.
2.5. Study outcomes
The primary outcome of interest was the percentage of patients completing the mailed FIT within 3 months of initial outreach. The secondary outcome was the percentage of patients opting into mailed FIT kit through text message response. We also tracked the outcomes of patients with positive FIT, including receipt of colonoscopy and findings during colonoscopy.
Outcome and demographic data were obtained from the EHR through medical record review by research staff. Race/ethnicity data was based on self-report. Household income was estimated using the American Community Survey 2012–2016 five-year estimate data for median income based on zip code of residence.
2.6. Statistical analysis
Based on preliminary data, it was anticipated that 320 subjects would be eligible, with participants enrolled evenly into each of two study arms. Estimating a base return rate of 5% in the text messaging only arm, we considered a meaningful increase in response rate to be 10 percentage points, which was based on a quality improvement pilot in the clinic population. Thus, we anticipated 80% power to detect an absolute 10 percentage point increase in response rate for text messaging and the lottery using a two-sided Type 1 error rate of 0.05. We used chi-squared tests of proportions to compare arms using intent-to-treat protocol. We also conducted a logistic regression adjusting for sex, age, race/ethnicity, insurance, and income. All analyses were performed in Stata version 15.0 (Stata Corp LP, College Station, Texas).
3. Results
3.1. Patient characteristics
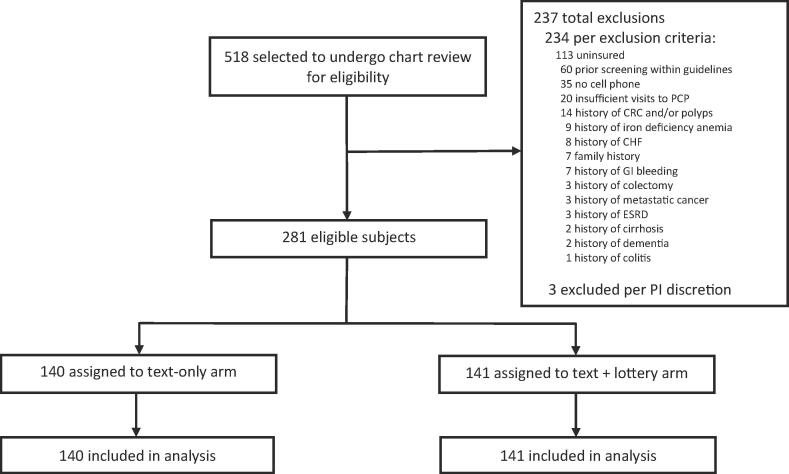
A total of 518 potentially eligible patients were identified through automated data extraction. After chart review, 281 of these were randomly allocated to the two study arms and included in the intent-to-treat analysis (Fig. 1). The intervention was conducted from April to July 2017, when 3-month follow-up was completed for all randomized participants.
Fig. 1.
Flow Diagram.
Overall, the majority of patients included in our study were women (n = 177, 63%) and of black race (n = 249, 89%). Most patients had Medicaid (n = 157, 56%) or commercial (n = 84, 30%) insurance; 11% (n = 32) had Medicare. Average household income was $32,694 (Table 1).
Table 1.
Demographic characteristics by study arm.
| Characteristics | Text-Only (n = 140) |
Text + Lottery (n = 141) |
P-value |
|---|---|---|---|
| Sex (%) | 0.65 | ||
| Women | 90 (64.3) | 87 (61.7) | |
| Men | 50 (35.7) | 54 (38.3) | |
| Age, Mean (SD) | 56.9 (5.4) | 57.1 (5.6) | 0.79 |
| Race/Ethnicity (%) | 0.52 | ||
| Non- Hispanic White | 6 (4.3) | 5 (3.5) | |
| Black | 122 (87.1) | 127 (90.1) | |
| Hispanic | 6 (4.3) | 3 (2.1) | |
| Asian | 2 (1.4) | 3 (2.1) | |
| Native American | – | 1 (0.7) | |
| Other | 4 (2.9) | 2 (1.4) | |
| Insurance type (%) | 0.54 | ||
| Commercial | 38 (27.1) | 46 (32.6) | |
| Medicare | 15 (10.7) | 17 (12.1) | |
| Medicaid | 84 (60) | 73 (51.8) | |
| Medicare & Medicaid | 3 (2.1) | 5 (3.5) | |
| Household Income, Median (IQR)* | $29,972 ($29,972–30,797) |
$29,972 ($29,972–30,797) |
0.36 |
Based on 2015 American Community Survey 2012–2016 5-Year Estimates data.
3.2. Response to outreach
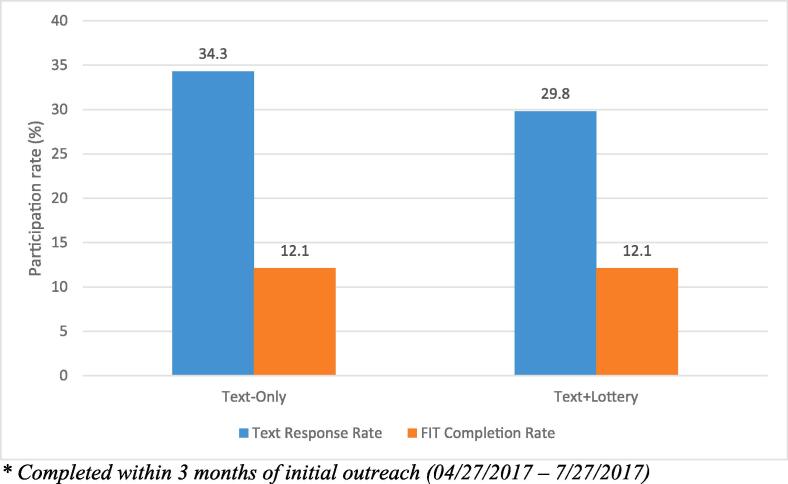
About 34.3% (95% CI, 26.5%–42.2%) in the text message arm and 29.8% (95% CI, 22.2%–37.3%) in the lottery arm responded affirmatively to text messaging, with no statistical difference between arms (Fig. 2). The 3-month FIT completion rate was 12.1% (95% CI, 6.7%–17.5%) in the text message only arm and 12.1% (95% CI, 6.7%–17.5%) in the text message with lottery arm, with no statistical difference between arms (Table 2). Adjusting for sex, age, race/ethnicity, insurance, and income, we also found no statistical difference comparing the text message with lottery arm to text message only arm (adjusted odds ratio: 1.09; 95% CI: 0.52–2.27; P = 0.83). The sociodemographic variables were not statistically significant.
Fig. 2.
Opt-in text response and FIT completion rates by study arm * Completed within 3 months of initial outreach (04/27/2017–7/27/2017).
Table 2.
Response to text outreach and completion of FIT.
| Text-Only (n = 140) |
Text + Lottery (n = 141) |
P-value | |
|---|---|---|---|
| Text message responses | |||
| Opt-in/FIT kits mailed | 48 (34.3) | 42 (29.8) | P = 0.42 |
| Stop | 7 (5.0) | 3 (2.1) | |
| Already Screened | 2 (1.4) | 3 (2.1) | |
| FIT kit completed (%)1 | 17 (12.1) | 17 (12.1) | P > 0.99 |
| Female (%) | 14 (15.6) | 11 (12.6) | |
| FIT results | |||
| Negative (%) | 15 (88.2) | 16 (94.1) | |
| Positive (%) | 2 (11.8) | 0 (0) | |
| Not Reported (%) | – | 1 (5.9) |
Completed within 3 months of initial outreach (04/27/2017–7/27/2017).
Among the 34 patients returning a FIT during the follow-up period, 2 (6%) had a positive result and both of those patients (100%) received a follow-up colonoscopy. One colonoscopy was normal and the other had a small tubular adenoma removed. 79 patients (72 requested a kit) responded to the initial text message, 20 (15 requested a kit) responded to the first reminder, and 6 (3 requested a kit) responded to the second reminder.
3.3. Post-intervention interviews
Of the 281 patients in the study, 100 (36%) were called to complete the post-intervention interview, and 38 (38%) agreed to participate. Nine (24%) of respondents reported receiving the FIT kit by mail, 6 (67%) of those reported returning the kit. Among the 38 patients who were interviewed, 11 (29%) reported receiving CRC screening in the past, most (n = 10, 91%) with colonoscopy.
Among 32 patients who responded, 5 (16%) were more likely to complete colonoscopy every 10 years, 17 (53%) were more likely to complete FIT every year, and 10 (32%) had no preference between the two screening options. Those that were more likely to complete colonoscopy cited that it has a less frequent timeline than FIT, it is more detailed and accurate, and they are more comfortable doing screening in a clinical setting. Those that were more likely to complete FIT described that it is easier than colonoscopy, they do not like procedures, and they would not need to do a preparation.
When asked which methods would be acceptable for CRC screening reminders, 18 (56%) described phone, 19 (59%) described mail, 17 (53%) described a clinic visit, 16 (50%) described text messaging, and 5 (16%) described email as a modality. When asked which method is preferable, 10 (31%) chose phone calls, 8 (25%) chose a clinic visit, 7 (22%) chose mail, 5 (16%) chose text messaging, and 2 (6%) chose email. Ten out of 17 (59%) described that text messaging was ‘very convenient’ or ‘convenient’ to respond to.
4. Discussion
In this study, we show that bidirectional text messaging is a feasible and acceptable modality to communicate with patients for mailed FIT outreach. However, the lottery-based incentive did not incrementally improve response or completion rate of mailed FIT.
This study adds to the literature about using text messaging to facilitate outreach for CRC screening. One prior study sent text messages to patients in Israel who were receiving mailed fecal occult blood testing (FOBT) kits, and found that interrogative text messages resulted in an increase in uptake of 1.3–1.8 percentage points as compared to a control group without text messaging (Hagoel et al., 2016). Another study among Alaska Native and Native American patients sent a series of 3 text messages with instructions to call a navigator, which found a 3.3 percentage point increase in screening participation. Another study from London showed that text messaging reminders did not increase overall return of mailed FOBT kits, but they increased uptake among first-time invitees by 5.6 percentage points (Hirst et al., 2017). In our study, 32% of patients responded affirmatively to the text messaging and were mailed FIT kits, and 12% of patients ultimately complete FIT. This is favorable compared to a 2% response rate to traditional text messaging that asks patients to come to the clinic for screening. We show that bidirectional text messaging should be linked to processes to facilitate screening, and it can also make mailed FIT more efficient by only sending kits to those that ask for it. Additionally, since the text messaging platform was already available at the clinic, there was minimal incremental cost to sending additional messages to patients.
We also find that the gift card lottery incentive of $20 expected value (1 in 5 participants receive $100) did not boost uptake of CRC screening in this population. This study does not suggest that financial incentives are ineffective—only that in this study they offered no incremental benefit over a program of text message-based opt in screening with text message reminders. Of note, patients in the trial were insured, and there was no cost to the patient for completing FIT. There are a few studies that have evaluated financial incentives for CRC screening, with mixed results. While one study in a clinic setting showed that a 1 in 10 chance of $50 lottery incentive increased participation (Kullgren et al., 2014), two other trials of mailed FIT with $5 and $10 financial incentives that evaluated different designs of incentives did not increase response rates (Gupta et al., 2016, Mehta et al., 2019). Finally, another trial in a health system employee population showed that a $100 incentive modestly increased completion of screening colonoscopy (Mehta et al., 2017).
The varying results from trials of financial incentives suggest that the design and framing of incentives may be just as important as the amount, which is supported by insights from behavioral economics (Thirumurthy et al., 2019). There are a few reasons why incentives may not have offered an incremental boost in our study. First, the incentive may not have been large enough to motivate patients, although the expected value of a 1 in 5 chance of $100 exceeds that of a 1 in 10 chance of $50 that was effective in the clinic context. However, community health programs may be unable to afford larger incentives. Second, the 1 in 5 chance of $100 lottery incentive design may not have been as effective as other incentive designs. While lotteries work in some contexts when people overestimate their chances of winning, this population may be more risk averse for a lottery that only provides a chance of winning as compared to a guaranteed incentive if they participate (Kahneman and Tversky, 1979, Holt and Laury, 2002). Another study showed a lower, although not statistically different, response rate to a lottery incentive as compared to the equivalent value guaranteed incentive (Mehta et al., 2019). Third, there may have been a lack of understanding about the lottery incentive, since it was communicated by text message without the opportunity to discuss or ask questions. This may have been the first text message received from the clinic for some patients. Finally, there is the possibility that financial incentives may not be sufficient to overcome the present- bias and lack of motivation by the patients to participate, particularly in an underserved population. Although not statistically significant, a greater proportion of patients who received the FIT kit in the text + lottery arm returned the kit compared to the text only arm (40% vs 35%), which may have resulted in fewer wasted kits.
This study has limitations. We only focused on FIT outreach, and we did not offer colonoscopy as an option, although the past reliance on colonoscopy may have explained the low baseline screening rates in this population. We followed patients for only 3 months, although the response rate to text messaging was typically within a few days. We did not complement text messaging with any phone calls, which may have explained the modest response rate as compared to other mailed FIT trials (Dougherty et al., 2018). More than half of people that responded affirmatively to the text message were sent the kit, but did not ultimately complete screening. A follow-up phone call or navigation could be helpful. Due to sample size limitations, we were not able to compare to usual care or mailed FIT without text messaging. Also, the response rate might be higher if FIT kits are sent to all patients that do not decline, as we have shown that switching from opt-in to opt-out can increase uptake (Mehta et al., 2018, Mehta et al., 2016b). We were not able to evaluate different incentive designs or amounts. Finally, there was a low response rate to the post-intervention interview (38%), and the respondents may not be representative of the overall population.
This study also has strengths, including its experimental design with individual-level randomization to account for unobserved confounding variables. As a pragmatic trial conducted in partnership with a community health center, the results are generalizable to similar clinics that reflect racial and socioeconomic disparities. The population was predominately Black with Medicaid, and the baseline screening rate in this clinic population was approximately 19%, which is similar to other community health centers, but much lower than the national rates of CRC screening (White et al., 2017, Baker et al., 2015). Text messaging is a new modality for engaging with patients, and due to its low cost to deliver, it has the potential to make CRC screening interventions more scalable.
In conclusion, we show that text messaging can be a reasonable approach to engagement with underserved populations about CRC screening. Although financial incentives were not effective as an adjunct to text messaging, it is important to complement screening interventions with insights from behavioral science and processes to make screening easier for patients.
Credit authorship contribution statement
Shivan J. Mehta: Conceptualization, Funding acquisition, Methodology, Resources, Supervision, Writing - original draft. Akinbowale Oyalowo: Conceptualization, Data curation, Writing - review & editing. Catherine Reitz: Conceptualization, Data curation, Formal analysis, Project administration, Writing - review & editing. Owen Dean: Data curation, Project administration, Writing - review & editing. Timothy McAuliffe: Data curation, Project administration, Writing - review & editing. David A. Asch: Methodology, Writing - review & editing. Chyke A. Doubeni: Conceptualization, Funding acquisition, Resources, Writing - review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgements
This trial was funded by a Patient Centered Outcomes Research Pilot from the Center for Therapeutic Effectiveness Research at the University of Pennsylvania. Dr. Mehta’s time was supported by grant number K08CA234326 and Dr. Doubeni’s time was supported by grant number R01CA213645 from the National Cancer Institute of the National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Dr. Asch is a partner at the behavioral economics consulting firm VAL Health. Dr. Doubeni is a member of the US Preventive Services Task Force (USPSTF). This article does not necessarily represent the views and policies of the USPSTF.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2020.101114.
Appendix A
Appendix 1. Text messaging language by arm
Initial Text Outreach
(4/18/2017 @10am) - Batch 1
Arm 1 (Text-Only)
Health Annex: You’re due for colon cancer screening. Text “Yes” to receive a free, simple home test kit, or “Stop.”
Arm 2 (Text + Lottery)
Health Annex: You’re due for colon cancer screening. Text “Yes” to receive a free, simple home test kit, or “Stop.” Complete it for a 1 in 5 chance at $100.
Outreach Reminder (x 2)
Non-responders 3 business days after initial outreach (4/24/2017 @ 3:30pm) – Batch 1
If still no response, 3 business days after first reminder (4/28/2017 @ 2pm) – Batch 2
Arm 1 (Text-Only)
Health Annex Reminder: You’re due for colon cancer screening. Text “YES” to get a free, simple, home test kit or “STOP.”
Arm 2 (Text + Lottery)
Health Annex Reminder: You’re due for colon cancer screening. Text “Yes” to get a free, simple home test kit, or “Stop.” Complete it for a 1 in 5 chance at $100.
FIT Reminder (x 2)
3 weeks after first kits mailed (Batch 1: 5/17/2017, Batch 2: 5/25/2017 @ 10am)
If still not received, 5 weeks after first kits mailed (Batch 1: 5/31/2017, Batch 2: 6/8/2017 @ 10am)
Arm 1 (Text-Only)
Health Annex: We sent a colon cancer screening test –complete & return w/included pre-paid envelope! Questions: xxx-xxx-xxxx.
Arm 2 (Text + Lottery)
Health Annex: We sent a colon cancer screening test–complete & return w/included pre-paid envelope! Complete for a 1 in 5 chance at $100. Questions: xxx-xxx-xxxx.
Appendix B. Supplementary data
The following are the Supplementary data to this article:
References
- Asch D.A., Ziolek T.A., Mehta S.J. Misdirections in informed consent - impediments to health care innovation. N. Engl. J. Med. 2017;377(15):1412–1414. doi: 10.1056/NEJMp1707991. [DOI] [PubMed] [Google Scholar]
- Baker D.W., Liss D.T., Alperovitz-Bichell K., Brown T., Carroll J.E., Crawford P. Colorectal cancer screening rates at community health centers that use electronic health records: a cross sectional study. J. Health Care Poor Underserved. 2015;26(2):377–390. doi: 10.1353/hpu.2015.0030. [DOI] [PubMed] [Google Scholar]
- Cole-Lewis H., Kershaw T. Text messaging as a tool for behavior change in disease prevention and management. Epidemiol. Rev. 2010;32:56–69. doi: 10.1093/epirev/mxq004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coronado G.D., Petrik A.F., Vollmer W.M., Taplin S.H., Keast E.M., Fields S. Effectiveness of a mailed colorectal cancer screening outreach program in community health clinics: the STOP CRC cluster randomized clinical trial effectiveness of a mailed colorectal cancer screening outreach program in community health clinics. JAMA Internal Med. 2018;178(9):1174–1181. doi: 10.1001/jamainternmed.2018.3629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dougherty M.K., Brenner A.T., Crockett S.D., Gupta S., Wheeler S.B., Coker-Schwimmer M. Evaluation of interventions intended to increase colorectal cancer screening rates in the United States: a systematic review and meta-analysis. JAMA Internal Med. 2018;178(12):1645–1658. doi: 10.1001/jamainternmed.2018.4637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gollwitzer, P.M., Sheeran, P, 2006. Implementation Intentions and Goal Achievement: A Meta‐analysis of Effects and Processes. Adv. Experimental Soc. Psychol. Academic Press. 38, 69–119.
- Green B.B., Wang C., Anderson M.L. An automated intervention with stepped increases in support to increase uptake of colorectal cancer screening: a randomized trial. Ann. Intern. Med. 2013;158(5_Part_1):301–311. doi: 10.7326/0003-4819-158-5-201303050-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta S., Miller S., Koch M., Berry E., Anderson P., Pruitt S.L. Financial incentives for promoting colorectal cancer screening: a randomized. Comparative Effect. Trial. Am. J. Gastroenterol. 2016;111(11):1630–1636. doi: 10.1038/ajg.2016.286. [DOI] [PubMed] [Google Scholar]
- Hagoel L., Neter E., Stein N., Rennert G. Harnessing the question-behavior effect to enhance colorectal cancer screening in an mHealth experiment. Am. J. Public Health. 2016;106(11):1998–2004. doi: 10.2105/AJPH.2016.303364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haisley E., Volpp K.G., Pellathy T., Loewenstein G. The impact of alternative incentive schemes on completion of health risk assessments. Am. J. Health Promotion: AJHP. 2012;26(3):184–188. doi: 10.4278/ajhp.100729-ARB-257. [DOI] [PubMed] [Google Scholar]
- Hirst Y., Skrobanski H., Kerrison R.S., Kobayashi L.C., Counsell N., Djedovic N. Text-message reminders in colorectal cancer screening (TRICCS): a randomised controlled trial. Br. J. Cancer. 2017;116(11):1408–1414. doi: 10.1038/bjc.2017.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt C.A., Laury S.K. Risk aversion and incentive effects. Am.Econom. Rev. 2002;92(5):1644–1655. [Google Scholar]
- Kahneman D., Tversky A. Prospect theory: an analysis of decision under risk. Econometrica. 1979;47(2):263–291. [Google Scholar]
- Kullgren J.T., Dicks T.N., Fu X., Richardson D., Tzanis G.L., Tobi M. Financial incentives for completion of fecal occult blood tests among veterans: a 2-stage, pragmatic, cluster, randomized, controlled trial. Ann. Intern. Med. 2014;161(10 Suppl):S35–S43. doi: 10.7326/M13-3015. [DOI] [PubMed] [Google Scholar]
- Loewenstein G., Brennan T., Volpp K.G. Asymmetric paternalism to improve health behaviors. JAMA. 2007;298(20):2415–2417. doi: 10.1001/jama.298.20.2415. [DOI] [PubMed] [Google Scholar]
- Mandel J.S., Bond J.H., Church T.R., Snover D.C., Bradley G.M., Schuman L.M. Reducing mortality from colorectal cancer by screening for fecal occult blood. Minnesota Colon Cancer Control Study. N. Engl. J. Med. 1993;328(19):1365–1371. doi: 10.1056/NEJM199305133281901. [DOI] [PubMed] [Google Scholar]
- Mehta S.J., Asch D.A. How to help gastroenterology patients help themselves: leveraging insights from behavioral economics. Clin. Gastroenterol. Hepatol. 2014;12(5):711–714. doi: 10.1016/j.cgh.2014.02.022. [DOI] [PubMed] [Google Scholar]
- Mehta S.J., Troxel A.B., Marcus N., Jameson C., Taylor D., Asch D.A. Participation rates with opt-out enrollment in a remote monitoring intervention for patients with myocardial infarction. JAMA Cardiol. 2016;1(7):847–848. doi: 10.1001/jamacardio.2016.2374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta S.J., Jensen C.D., Quinn V.P., Schottinger J.E., Zauber A.G., Meester R. Race/ethnicity and adoption of a population health management approach to colorectal cancer screening in a community-based healthcare system. J. Gen. Intern. Med. 2016;31(11):1323–1330. doi: 10.1007/s11606-016-3792-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta S.J., Feingold J., Vandertuyn M., Niewood T., Cox C., Doubeni C.A. Active choice and financial incentives to increase rates of screening colonoscopy-a randomized controlled trial. Gastroenterology. 2017;153(5) doi: 10.1053/j.gastro.2017.07.015. 1227 9.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta S.J., Khan T., Guerra C., Reitz C., McAuliffe T., Volpp K.G. A randomized controlled trial of opt-in versus opt-out colorectal cancer screening outreach. Am. J. Gastroenterol. 2018 doi: 10.1038/s41395-018-0151-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta S.J., Pepe R.S., Gabler N.B., Kanneganti M., Reitz C., Saia C. Effect of financial incentives on patient use of mailed colorectal cancer screening tests: a randomized clinical trial. JAMA Network Open. 2019;2(3) doi: 10.1001/jamanetworkopen.2019.1156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milkman K.L., Beshears J., Choi J.J., Laibson D., Madrian B.C. Using implementation intentions prompts to enhance influenza vaccination rates. PNAS. 2011;108(26):10415–10420. doi: 10.1073/pnas.1103170108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milkman K.L., Beshears J., Choi J.J., Laibson D., Madrian B.C. Planning prompts as a means of increasing preventive screening rates. Prev. Med. 2013;56(1):92–93. doi: 10.1016/j.ypmed.2012.10.021. [DOI] [PubMed] [Google Scholar]
- Muller C.J., Robinson R.F., Smith J.J., Jernigan M.A., Hiratsuka V., Dillard D.A. Text message reminders increased colorectal cancer screening in a randomized trial with Alaska Native and American Indian people. Cancer. 2017;123(8):1382–1389. doi: 10.1002/cncr.30499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- http://www.pewinternet.org/fact-sheets/mobile-technology-fact-sheet/ (accessed October 11, 2019).
- Schoen R.E., Pinsky P.F., Weissfeld J.L., Yokochi L.A., Church T., Laiyemo A.O. Colorectal-cancer incidence and mortality with screening flexible sigmoidoscopy. N. Engl. J. Med. 2012;366(25):2345–2357. doi: 10.1056/NEJMoa1114635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz J., Mochon D., Wyper L., Maroba J., Patel D., Ariely D. Healthier by precommitment. Psychol. Sci. 2014;25(2):538–546. doi: 10.1177/0956797613510950. [DOI] [PubMed] [Google Scholar]
- Siegel R.L., Miller K.D., Jemal A. Cancer statistics, 2018. CA Cancer J. Clin. 2018;68(1):7–30. doi: 10.3322/caac.21442. [DOI] [PubMed] [Google Scholar]
- Thirumurthy H., Asch D.A., Volpp K.G. The uncertain effect of financial incentives to improve health behaviors. JAMA. 2019;321(15):1451–1452. doi: 10.1001/jama.2019.2560. [DOI] [PubMed] [Google Scholar]
- Tversky A., Kahneman D. The framing of decisions and the psychology of choice. Science. 1981;211(4481):453–458. doi: 10.1126/science.7455683. [DOI] [PubMed] [Google Scholar]
- Volpp K.G., Gurmankin Levy A., Asch D.A., Berlin J.A., Murphy J.J., Gomez A. A randomized controlled trial of financial incentives for smoking cessation. Cancer Epidemiol. Biomarkers Prev. 2006;15(1):12–18. doi: 10.1158/1055-9965.EPI-05-0314. [DOI] [PubMed] [Google Scholar]
- Volpp K.G., Loewenstein G., Troxel A.B., Doshi J., Price M., Laskin M. A test of financial incentives to improve warfarin adherence. BMCHealth Serv. Res. 2008;8:272. doi: 10.1186/1472-6963-8-272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volpp K.G., Pauly M.V., Loewenstein G., Bangsberg D. P4P4P: an agenda for research on pay-for-performance for patients. Health Aff. 2009;28(1):206–214. doi: 10.1377/hlthaff.28.1.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White A., Thompson T.D., White M.C., Sabatino S.A., de Moor J., Doria-Rose P.V. Cancer screening test use - United States, 2015. MMWR Morb. Mortal Wkly. Rep. 2017;66(8):201–206. doi: 10.15585/mmwr.mm6608a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.