As noted by Darlenski and Tsankov, no specific skin changes had been described at the time of this letter due to COVID-19.1 A nonspecific viral eruption, however, can occur as the following case illustrates.
Case presentation
A 26-year-old American graduate student receiving adalimumab biweekly (at a dose of 40 mg, citrate-free, with the pen kit and no other medications) for Crohn’s disease in remission had close contact with persons documented to be infected with SARS-CoV-2. On March 13, 2020, he complained of a sore throat followed several days later by malaise, aches, and a mild nonproductive cough, plus loss of taste and smell. There was minimal chest congestion. Thirteen days after the onset of these findings, he developed for the first time a fever of 101°F (38.3°C). The next morning (day 14) he awoke with an asymptomatic facial eruption and consulted both of us through telemedicine.
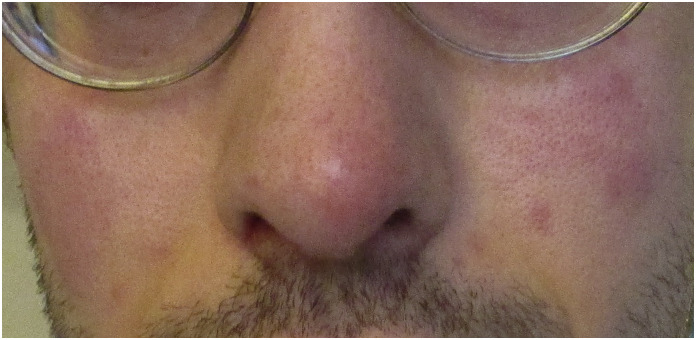
Examination of the facial photographs (Fig. 1, Fig. 2, Fig. 3 ) showed an erythematous, slightly edematous, malar eruption. No epidermal changes were noted. By day 15, the malar eruption had lightened, only to have spread to the temples (Fig. 4, Fig. 5 ). There was a low-grade fever, along with mildly tender cervical lymphadenopathy. The next day, the involved areas had become red, swollen, and tender (Figure 6 ). On day 18, the fever was gone, the malar eruption had resolved with slight skin peeling, the redness on the temples was fading, and the right ear had slightly lightened except for the ear lobe, which remained swollen with a slight exudate. The eruption had now spread to the right side of the neck (Fig. 7, Fig. 8 ). By day 20, the patient was asymptomatic, and the cervical nodes were no longer tender. The right ear was minimally tender, and the erythema was subsiding from the right ear and neck area.
Fig. 1.
The patient's mid-face on the first day of his eruption, front view.
Fig. 2.
The patient's right face on the first day of his eruption.
Fig. 3.
The patient's left face on the first day of his eruption.
Fig. 4.
The patient's left temple on the second day of his eruption.
Fig. 5.
The patient's right temple on the second day of his eruption.
Fig. 6.
Day three of the patient's eruption, now involving his right ear.
Fig. 7.
Day five of the patient's eruption, now involving his right neck.
Fig. 8.
Day five of the patient's eruption, now involving his right neck.
Discussion
In our opinion, the patient’s eruption was part of his presumptive diagnosis of COVID-19 infection. Due to shortages of SARS-CoV-2 testing kits, the patient has not as yet been tested and has been self-quarantining. He was advised to apply cool, wet compresses and reassured that once he was better, the eruption would go away.
Eruption associated with COVID-19 was found to occur in 2 out of 1099 (0.2%) patients in a study of patients of mainland China.2 The eruption, in another report, was described as being “faint.”3 In a case report from Thailand, a patient presented with a skin eruption, petechiae, and thrombocytopenia, for which he was initially misdiagnosed as having dengue but ultimately found to have COVID-19.4 In our case, the patient’s facial eruption was suggestive of pernio. A pernio-like lesion of the toes has been reported as a manifestation of COVID-19 [5]. The facial lesions in our patient have a distinctly violaceous color typical of pernio, and pernio is known to occur on the face, not just the distal extremities. It is possible that the patient’s ongoing treatment with adalimumab may have modified in some way the clinical presentation. The adalimumab treatments are currently on hold until the patient fully recovers from the viral infection.
As the SARS-CoV-2 pandemic intensifies in the United States and worldwide, dermatologists may increasingly be consulted on COVID-19 patients presenting with an eruption. Cutaneous manifestations of COVID-19 include erythematous eruptions, urticarial lesions, pernio and chicken-pox like vesicles [5], These skin findings may cause diagnostic confusion between COVID-19 and other viral infections having fever and eruption, such as dengue.
Conclusions
The sudden appearance of such an eruption may also alarm patients infected with SARS-CoV-2, who may not be aware that a viral eruption can be a part of the findings of COVID-19. Education of the public on COVID-19 should include mention that some patients may develop such an eruption, which will resolve.
Footnotes
Refers to document(s): CID 7436, S0738-081X(20)30049-3(10.1016/j.clindermatol.2020.03.012, FLA)
References
- 1.Darlenski R., Tsankov N. Covid-19 pandemic and the skin – what should dermatologists know? Clin Dermatol. 2020 doi: 10.1016/j.clindermatol.2020.03.012. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guan WJ., Ni ZY., Hu Y. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. Feb 28, 2020 doi: 10.1056/NEJMoa2002032. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.European Centre for Disease Prevention and Control Novel coronavirus (SARS-CoV-2): discharge criteria for confirmed COVID-19 cases – when is it safe to discharge COVID-19 cases from the hospital or end home isolation? https://www.ecdc.europa.eu/sites/default/files/documents/COVID-19-Discharge-criteria.pdf Available at:
- 4.Job B., Wiwanitkit V. COVID-19 can present with a rash and be mistaken for Dengue. J Am Acad Dermatol. May 2020;82(5) doi: 10.1016/j.jaad.2020.03.036. e177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Communique de presse Le 6 avril . 2020. Le Syndicat National des Dermatologues-Venereologues (SNDV) alerte sur les manifestations du COVID-19.www.syndicatdermatos.org/wp-content/uploads/2020/04/cp-covid-peau-6-avril (accessed April 13, 2020) [Google Scholar]