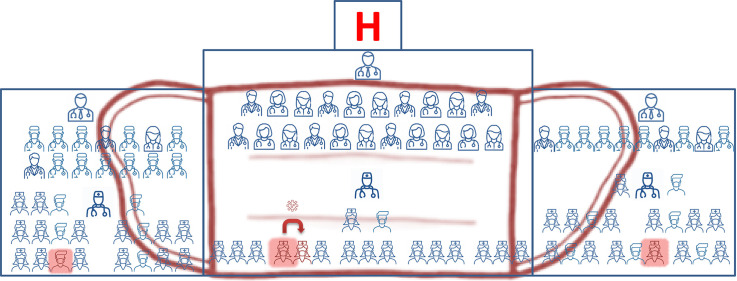
Graphical abstract
To the Editor,
Since February 2020, Italy has been facing a dramatic spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, mostly confined to the northern regions [[1], [2], [3]]. Such overwhelming diffusion of coronavirus disease 2019 (COVID-19) compelled national authorities to enforce an unprecedented restriction to citizen mobility and, most importantly, made the entire nation aware of the stringent need to act for the slowing of contagion [4].
Southern Italian regions had therefore more time to implement infection prevention and control measures, especially within hospitals and health-care facilities. Indeed, health-care personnel (HCP) immediately appeared to be among the categories at highest risk for contagion. Between 23 February and 5 March, the Monaldi Hospital in Naples, Italy, adopted a diffuse policy of infection prevention and control, specifically directed to SARS-CoV-2 containment among HCP, as well as patients. The infection prevention and control plan included: (a) an immediate halt to further admissions in wards with positive cases; (b) screening of all HCP and patients currently admitted to the index unit with nasal and oropharyngeal swabs for SARS-CoV-2 real-time RT-PCR detection, irrespective of symptoms, to be completed within 12 hours from activation of the plan; (c) reinforced personal protective equipment (PPE) use; (d) quarantine of SARS-CoV-2-positive cases only and further clinical assessment as per current protocols; (e) sanitation of the entire unit capacity with temporary patient removal; (f) restart of unit admissions with RT-PCR-negative staff and patients. The plan included standard precautions, contact precautions and droplet precautions, and led to a dramatic increase in the use of surgical face masks and hydro-alcoholic gel solutions. Despite that, on 16 March 2020, three nurses staffing the hospital were diagnosed with COVID-19. Here, we describe the results of the consequential epidemiological investigation.
All HCP/patients working/dwelling in the index clinical units underwent nasal and oropharyngeal swabs using Sigma Virocult Duo swabs (Medical Wire & Equipment, Corsham, UK). The preserving swab solution was used for the extraction of RNA that was subsequently used as a template in a multiplex, RT-PCR for screening and simultaneous confirmation of SARS-CoV-2 infection (Allplex 2019-nCoV assay, Seegene, Seoul, Republic of Korea). With this assay, molecular targets were those approved by the WHO, the US CDC and the Chinese CDC. Results were deemed positive when target detection occurred before 37 RT-PCR cycles.
Between 13 March and 16 March 2020, three HCP from three different hospital units (specialist medical unit, specialist surgical unit, general surgery unit) were found to be positive at SARS-CoV-2 swab after becoming symptomatic for COVID-19. Table 1 describes the clinical features and timing of the infection for these three individuals. Cases 1 and 2 were sisters, and had another sister who was diagnosed with COVID-19 during the same time frame. Case 3 had an unknown source of infection. The three individuals were deemed to have acquired the infection out of hospital. All actively worked during the pre-symptomatic phase for 4 days, and for one shift after becoming symptomatic. Therefore, there was enough time for SARS-CoV-2 to potentially spread in the three involved units.
Table 1.
Clinical and epidemiological features of SARS-CoV-2 infection in the three index cases
| Sex | Age | Role | Ward | Symptomsa |
Suspected source | Dates of potential contagion | Date of symptom onset | Days of symptoms before diagnosis/admission | Number of days on duty after potential contagion | Number of days on duty after symptom onset | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| F | C | M | D | A/D | |||||||||||
| Case 1 | Female | 61 | Nurse | Medical specialty | ✓ | ✓ | ✓ | ✗ | ✗ | Family outbreak | 1↔5/03/2020 | 08/03/20 | 7 | 4 | 1 |
| Case 2 | Female | 53 | Nurse | Surgical specialty | ✓ | ✓ | ✓ | ✗ | ✓ | Family outbreak | 6↔10/03/2020 | 13/03/20 | 1 | 4 | 1 |
| Case 3 | Male | 25 | Nurse | Surgery | ✓ | ✓ | ✓ | ✗ | ✗ | Unknown | 7↔11/03/2020 | 14/03/20 | 2 | 4 | 1 |
Symptoms: F, fever; C, cough; M, myalgia; D, diarrhoea; A/D, anosmia/dysgeusia.
SARS-CoV-2 screening swabs were performed on 17 March 2020, on all unit HCP (n = 107) as well as all current inpatients (n = 29). Only one additional nurse, who was working the same shifts as the index Case 1, was found to be positive for SARS-CoV-2 nasal/oropharyngeal swab. None of the 29 patients screened was positive. As of 23 April 2020, no additional HCP developed any sign or symptom suggestive of COVID-19 in the three index units.
Our results suggest that the propensity of SARS-CoV-2 to spread from person to person within an indoor environment characterized by obliged closed contacts is low, provided ordinary PPE are used and routine sanitation procedures are implemented. It should be noted that the time index cases remained at work after the event of contagion could only be estimated based on known average incubation times, i.e. 5 days [5]. In addition, the analysed sample size is relatively low and comes from a tertiary-care hospital not directly involved in triage of suspected/confirmed COVID-19 cases. Finally, because of the short time of index patient circulation after symptom onset, the actual intensity (number and duration) of contacts was probably limited.
Our observation may be of help in estimating the risk of intra-hospital spread of SARS-CoV-2 from HCP to other staff and admitted patients. Ordinary PPE may be effective to contain COVID-19 in the health-care setting when the local population incidence of infection is moderate. In light of the global shortage of PPE, our experience suggests that the use of fitted respirator masks as opposed to surgical masks may not be essential, provided gloves are also used and the HCP is not directly exposed to aerosol-generating procedures. Most importantly, there was absence of transmission between HCP wearing surgical masks and inpatients.
Contributions
EDM and RA worked on concept/design of the study; LB and FM worked on data collection; MB, MG, NC, CT, EF, ADS and MR performed laboratory work; MGR, LA and RZ worked on data analysis/interpretation; EDM and RZ drafted and critically revised the manuscript. All authors read and approved the final draft.
Funding
This work was supported by the AORN Ospedali dei Colli.
Transparency declaration
EDM received grant support and personal fees, outside of this work, from Roche, Pfizer, MSD, Angelini, Bio-Mérieux, Abbvie, Nordic Pharma, Sanofi-Aventis, Medtronic and DiaSorin. RZ and RA received personal fees, outside of this work, from Nordic Pharma. The other authors have no conflict of interest to disclose relevant to the content of this study.
Editor: L. Leibovici
References
- 1.Remuzzi A., Remuzzi G. COVID-19 and Italy: what next? Lancet. 2020;395:1225–1228. doi: 10.1016/S0140-6736(20)30627-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.http://www.salute.gov.it/portale/nuovocoronavirus/homeNuovoCoronavirus.html
- 3.Coronavirus latest: Italy death toll overtakes China’s. Nature NEWS; 20 March 2020. https://www.nature.com/articles/d41586-020-00154-w [Google Scholar]
- 4.Decreto del Presidente del Consiglio dei Ministri 09 marzo . Gazzetta Ufficiale Repubblica Italiana Serie Generale 2020. 2020. Ulteriori disposizioni attuative del decreto-legge 23 febbraio 2020, n. 6, recante misure urgenti in materia di contenimento e gestione dell'emergenza epidemiologica da COVID-19, applicabili sull'intero territorio nazionale; p. 62. [Google Scholar]
- 5.Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y., et al. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med. 2020;82:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]