To the Editor
Over the last several months, severe acute respiratory syndrome coronavirus 2 (COVID-19) has continued to spread all over the globe at an alarming rate, with total disregard for patients’ pre-existing medical conditions, age, or other demographics.1 The mortality rate is substantially higher than influenza, and the death rate in the United States seems to be surpassing that of both China and Europe.2 Although healthcare professionals report for duty each morning and evening to care for an increasing number of patients with various gradations of disease, their own safety and health remain threatened. The medical community has experienced a sobering reality: there is an utter lack of resources for patients as well as for providers. In particular, personal protective equipment (PPE) is at a critically low supply, which puts patients and providers at unacceptable risk. In the 2002 coronavirus severe acute respiratory syndrome outbreak, healthcare workers comprised an alarming 21% of cases, a trend we aim to prevent.3 Many strategies have been implemented by various individuals and companies to meet these needs, or to improvise in the meantime.4 Without the equipment necessary to protect healthcare workers, not only is there significant disruption of hospital work and unobtainable pressure put on the supply chain, but there is also profound risk to the lives of the people meant to care for the rest of society.
The spread of COVID-19 is mediated by various contact with droplets as well as direct airborne exposure.5 Varying degrees of protection are necessary for a range of procedures and patient interactions.6 At a minimum, any provider taking care of a patient with suspected or proven infection must wear a gown, gloves, an N95 respirator, and an eye shield/facemask. Healthcare providers engaged in procedures involving the nose, mouth, or airway need even more aggressive protection from airborne viral particles, in the form of powered air-purifying respirators, or similar.3
There are a number of ways in which the healthcare professional may be exposed to viral particles, and therefore risk personal infection or infection of other patients. Proper PPE therefore is not a luxury but a requirement to prevent mass infection and continued spread. The equipment available at this time is insufficient for a number of reasons, but first and foremost, there is not enough of it. Hospitals’ employees in the United States are left to reuse single-use masks over a number of days. The Centers for Disease Control and Prevention has recommended the use of bandanas or scarves as an alternative to masks, should the supply diminish even further.6 These measures are inconceivable regarding healthcare provider safety, and place each subsequent patient with whom the under-protected provider interfaces at considerable risk.
Additionally, N95 masks require specific fit testing that is often out of date for many providers, is limited by sizes available or attributes of the wearer, and can result in an unreliable seal.7 These masks cannot be customized, are in short supply, and are currently being reused (when they are even available) in many institutions. In light of this crisis of lack of resources that is plaguing so many countries and healthcare systems, these authors propose a novel alternative PPE device that unites proven technology with an innovative system: the 3-dimensional (3D)-printed Oxyframe PPE (Fig 1 ).
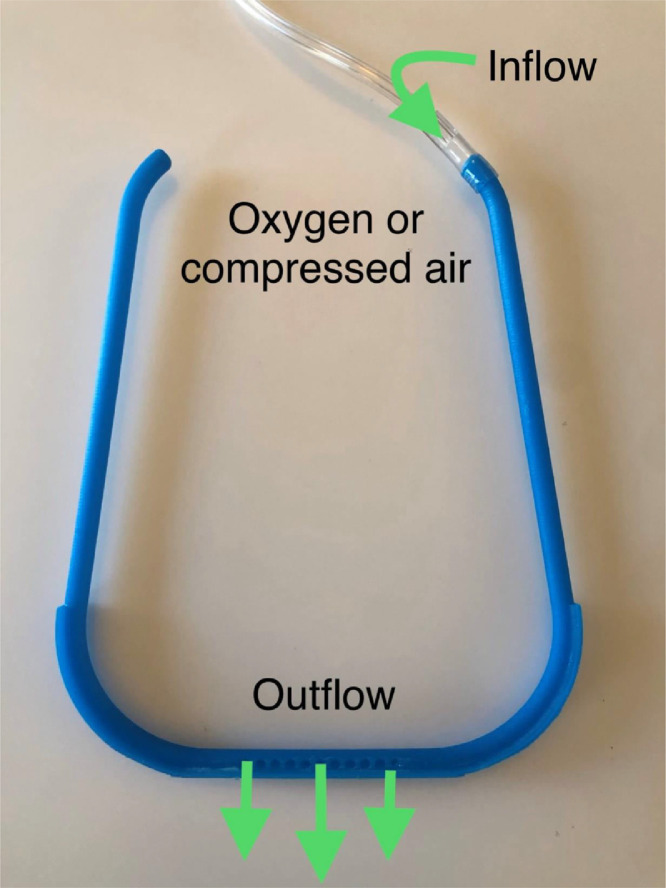
Fig 1.
3D printed frame that allows inflow of oxygen or compressed air behind the ear and outflow above the nose bridge. 3D, 3-dimensional.
Regarding design, we used SolidWorks (Dassault Systemes, France) for computer design, and the SLA Formlabs2 3D printer to generate the prototype. The printer uses resin as the base material, and we have tested both “Tough 1500” and “Draft resin.” The Tough resin produced a high-quality and durable part; the Draft resin allowed reasonable quality that can print with remarkable speed and efficiency—we were able to print 10 frames in 3.5 hours. There is no need for 3D printing support, and the front frame can be oriented directly on the printing platform (Fig 2 ). The current design is optimized for stereolithography 3D printing process, and would likely require different orientation on the building platform for fused deposition modeling or other 3D printing processes.
Fig 2.
Left: 10 printed frames without 3D printing supports being removed from the printing bed with a spatula. Right: 20 3D printed frames; note they come together and are easily detachable. 3D, 3-dimensional.
For specifications, each frame uses only 9.7 mL of the resin material. Therefore, 1 L of the resin could generate approximately 100 frames. The 3D printed parts need to be washed in an alcohol solution for 10 to 20 minutes subsequent to printing, and then must be cured in an ultraviolet light for 60 minutes to complete their processing. The frame can then be used to assemble face shields (Fig 3 ), or it can be used inside a plastic hood (Video 1). The frame is hollowed, and compressed air or oxygen enters on the back of the frame and exits above the bridge of the nose (Fig 1). The continuous airflow allows the provider to breathe comfortably inside the plastic hood, and simultaneously defogs the clear shield film (Video 1). Oxygen or compressed air is present in almost all hospital locations—standard on the medical floors, in intensive care units, and in operative rooms alike. Once connected to the compressed air or oxygen at 15 L/min, the air will flow from inside to outside of the hood, preventing the provider from inspiring aerosolized material from the patient. It is important to emphasize: 1- not to use the supplemental gas flow with the face shield configuration, this could potentially generate venturi effect and carry aerosolized particles to the providers face. 2- this PPE is not intended to substitute power air purified systems which can generate more than 100 liters per minute. 3- It should be used for short periods of time inside the hood with mask to prevent hypercapnia.
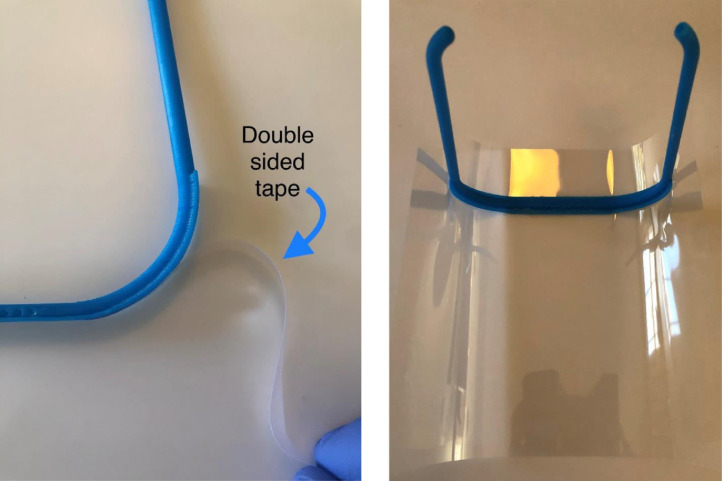
Fig 3.
Left: Assembly of a face shield using a double-sided tape. Right: Placement of the frame on the center of a transparency film.
We have attached the stereolithography file free to this letter. There are no studies about the efficacy or safety of this method. Like in any environment with a high oxygen atmosphere, fire risk is certainly a concern and should be discussed and mitigated, especially in the setting of electrocautery use. Some 3D printing processes require various chemical reagents, and skin allergies or reactions are possible. In the authors’ opinion, during the COVID-19 pandemic, all of the above risks are outweighed by the benefits of protecting healthcare professionals and enhancing patient safety during this national crisis.
Footnotes
L. Maracaja and D. L. V. Maracaja were responsible for designing, prototyping, and testing; D. Blitz: manuscript preparation and review; and C. A. Walker: manuscript preparation and reviewing literature, and submission.
Conflict of Interest: The authors declare no conflicts of interest.
Supplementary material associated with this article can be found in the online version at doi:10.1053/j.jvca.2020.04.004.
Appendix. Supplementary materials
Video 1. Oxyframe tested inside of a plastic hood using 10 L/min: Note the expansion of the hood showing positive pressure inside the hood and shield defogged owing to the outflow above the nose bridge.
References
- 1.MacIntyre C.R. Global spread of COVID-19 and pandemic potential. Global Biosecur. 2020;1 [Google Scholar]
- 2.Yee J., Unger L., Zadravecz F. Novel coronavirus 2019 (COVID-19): Emergence and implications for emergency care. J Am Coll Emerg Physicians Open. 2020 doi: 10.1002/emp2.12034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chang De, Xu H., Rebaza A. Protecting health-care workers from subclinical coronavirus infection. Lancet Respir Med. 2020;8:e13. doi: 10.1016/S2213-2600(20)30066-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chan J.F., Yuan S., Kok K.H. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: A study of a family cluster. Lancet. 2020;395:514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cheung J.C., Ho L.T., Cheng J.V. Staff safety during emergency airway management for COVID-19 in Hong Kong. Lancet Respir Med. 2020;8:e19. doi: 10.1016/S2213-2600(20)30084-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dwinell J. Bandanas can substitute as coronavirus masks as ‘a last resort,’ says CDC. Boston Herald. 2020 https://www.bostonherald.com/2020/03/23/bandanas-can-substitute-as-coronavirus-masks-as-a-last-resort-says-cdc/ Available at. Accessed March 27. [Google Scholar]
- 7.Coffey C.C., Campbell D.L., Zhuang Z. Simulated workplace performance of N95 respirators. Am Ind Hyg Assoc J. 1999;60:618–624. doi: 10.1080/00028899908984481. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video 1. Oxyframe tested inside of a plastic hood using 10 L/min: Note the expansion of the hood showing positive pressure inside the hood and shield defogged owing to the outflow above the nose bridge.