Introduction
The Coronavirus Disease 2019 (COVID-19) epidemic began in Wuhan, China, in December 2019.1 On January 1st, 2020, WHO announced that this outbreak represents an international public health emergency, affecting 2,725,920 people by April 24, 2020, causing, 191,061 deaths.2 On February 11, The International Committee on Taxonomy of Viruses has made public the name of the virus causing COVID-19: severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).3
Transmission paths
The two modes of transmission are via aerosols, through drops of fluid spread by coughing, sneezing, and fecal-oral (digestive).1
Characteristics of COVID-19
The incubation period is 1–14 days, most commonly 3–7 days. Patients are contagious in the latency period. On average, a patient can infect another 2–2.5 people.4
The main symptoms are represented by:
-
•
Fever
-
•
Cough (especially dry)
-
•
Fatigue
-
•
Sputum
-
•
Shortness of breath
-
•
Dry throat
-
•
Headache
-
•
Digestive manifestations in a small percentage of patients1
The fraction of severe, critical cases and mortality rate is higher, compared to influenza. The number of deaths per day relative to the total number of cases gives us a percentage of 3–4%.4
Control of infection in oral healthcare settings
In light of the thread of COVID-19 pandemic, the conception of strict and efficient protocols for oral healthcare settings is of paramount importance. This specialty is prone to cross infection among patients and healthcare workers. This article provides recommendation on patient evaluation, treatment approach for dental emergencies and infection control protocols.
Screening for COVID-19 status and triaging for dental treatments
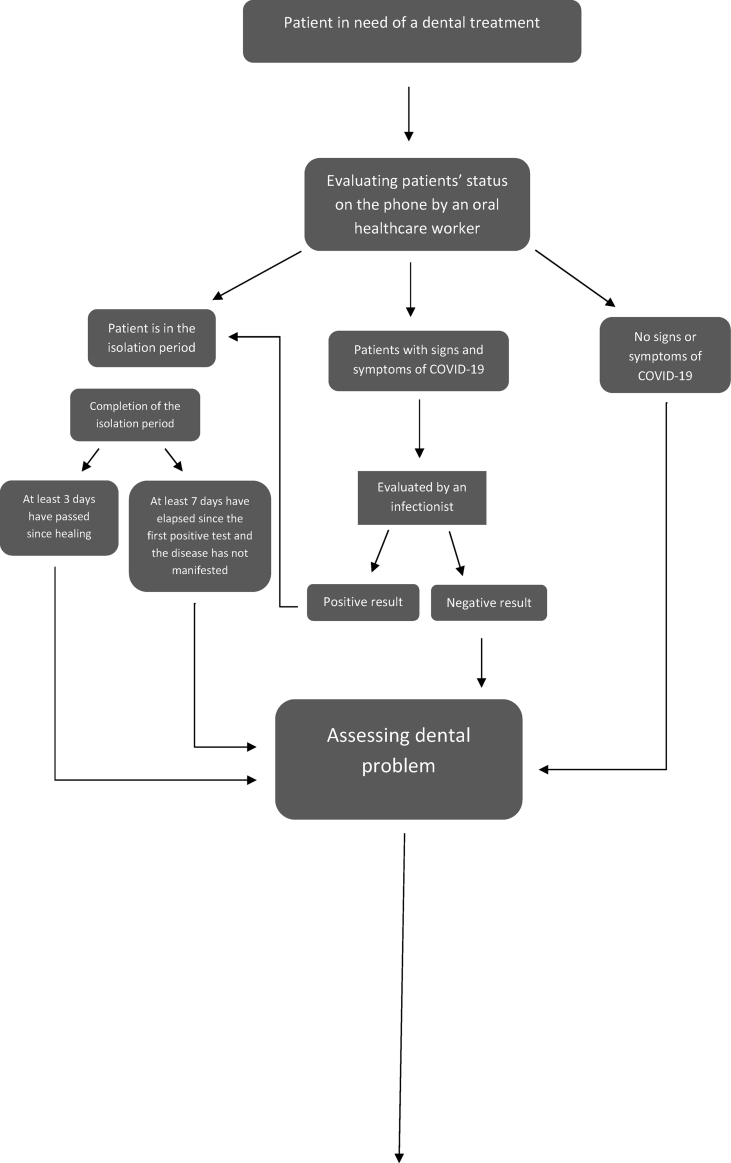
During the pandemic, it is recommended to perform exclusively emergency dental procedures to protect the medical personnel, the patients and to reduce as much as possible the consumption of personal protective equipment. Patients’ general health assessment before dental treatment is very important (Fig. 1), as dental health workers can identify undiagnosed COVID-19 patients. Emergency dental patients that test positive for SARS-CoV-2 should be referred for emergency care where appropriate Transmission-Based Precautions are available. The indication for SARS convalescing patients was to postpone dental treatments for 1 month.7 Same recommendation could be adopted for COVID-19 patients.
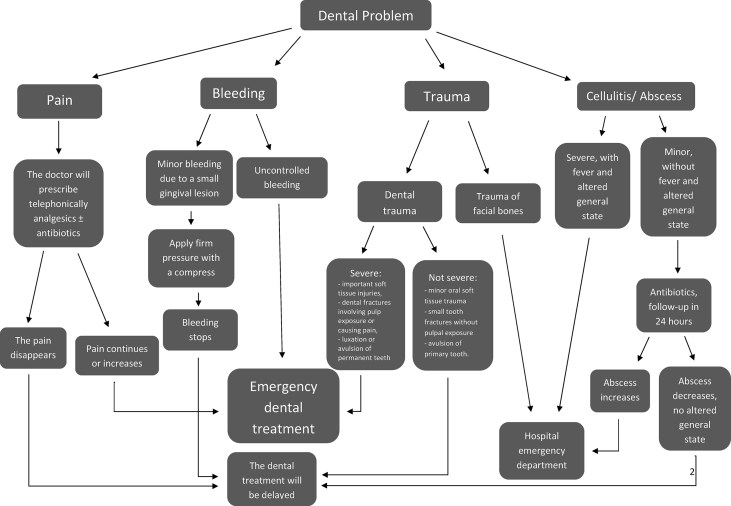
Figure 1.
Screening for COVID-19 status and triaging patients for dental treatments and guidelines of dental problem assessment.5,6
What is considered an emergency in dentistry, according to ADA?
Dental emergencies are those that put the patient's life at risk and require immediate treatment to stop bleeding, reduce pain and stop infection. The emergency dental cases are represented by:
-
•
Severe pain of pulp origin
-
•
Pericoronaritis, pain in the third molar region
-
•
Postoperative osteitis, dry alveolitis
-
•
Dental fractures causing pain or soft-tissue injuries caused by trauma
-
•
Luxations, dental avulsions
-
•
Dental treatments required before general medical procedures
-
•
Final cementation of crowns, decks if provisional restoration is lost, deteriorated or causes gum irritation
-
•
Biopsies
Other emergencies shall be considered as follows:
-
•
Extended cavities or damaged restorations causing pain (Temporary restorations are performed)
-
•
Suppression of suture threads
-
•
Dental treatments of oncology patients
-
•
Dental adjustments when function is impaired
-
•
Change of temporary fillings in endodontic access cavities, if they have caused pain
-
•
Adjustment of the orthodontic apparatus if it has caused pain or ulceration on the oral mucosa.8
Assessment of the gravity of the dental emergency is very important. The evaluation of the dental and general health status of the patient is based on the workflow in Fig. 1. Dental practitioners should aim to ease patients suffering and alleviate the burden that dental emergencies would place on hospital emergency departments.
Effective control of infection in the dental office
Social distancing protocol for patients should be adopted in the dental office. Appointments should be scheduled apart to minimize contact between patients. If this standard is not applicable, patients can wait in their personal vehicle, until it is their turn.
Since the main route of transmission of the virus is the aerial one, it is necessary to use personal protective equipment, gloves, face masks (N-95 or FFP2), goggles or facial shield to protect the skin and mucous membranes of the medical personnel as well as waterproof robes, jumpsuits. If the mask is damaged, or the doctor has difficulties breathing, the mask should be changed. Dental health worker should have a seasonal flu vaccine this year, ill-health status of medical personnel has to be assessed daily.
Rigorous hand hygiene and surfaces in the dental office is the most important measure of reducing the transmission of microorganisms to patients. Depending on surface type, temperature, humidity, SARS-CoV-2 may persist on surfaces from a few hours to a few days. All reading materials, magazines and toys should be removed from the dental office.
To minimize the formation of drops and aerosols, it is recommended to perform minimally invasive procedures, to use the surgical vacuum cleaner, 4-hand work, and rubber dam isolation of the operator field. Before dental procedures it is recommended that the patient rinses with antimicrobial oral solutions.9 Resorbable sutures after surgical procedures are recommended. Aerosol generating procedures should be scheduled at the end of the program. If procedures were performed without N95 masks, both the healthcare provider and the patient are at moderate risk for SARS-CoV-2 infection/transmission. Fourteen days of quarantine are recommended after this exposure. As intraoral x-ray can induce saliva secretion and coughing,10 extraoral radiographies (panoramic, Cone Beam Computer Tomography) are alternatives.
After providing dental care, facial protective equipment should be cleaned and disinfected. The X-ray equipment, the light and the dental chair should be disinfected according to the instructions of the manufacturer. The floors should also be disinfected. Handpieces must be sterilized after each patient. Frequently used surfaces such as: door handles, bathrooms, desks must be disinfected often.
In the areas severely affected by COVID-19, the patients arriving in the waiting room should receive protective masks.1
Conclusion
The COVID-19 pandemic represents a global challenge, given the increased contagiousness of SARS-CoV-2, dental healthcare providers have to adopt new protocols for a better infection prevention in the dental office and new working protocols aimed to prevent spreading the virus.
Declaration of Competing Interest
The authors have no conflicts of interest relevant to this article.
Acknowledgements
The authors received no funding for this work.
References
- 1.Meng L., Hua F., Bian Z. Coronavirus disease 2019 (COVID-19): emerging and future challenges for dental and oral medicine. J Dent Res. 2020;99:481–487. doi: 10.1177/0022034520914246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wordometer Reported cases and deaths by country, territory, or conveyance. https://www.worldometers.info/coronavirus/#countries Available at:
- 3.World Health Organization Naming the coronavirus disease (COVID-19) and the virus that causes it. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it Available at:
- 4.World Health Organization . 2020. Coronavirus disease 2019 (COVID-19) situation report 46.https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports Available at: [Google Scholar]
- 5.Scottish Cental Clinical Effectiveness Programme Management of acute dental problems during COVID-19 pandemic. http://www.sdcep.org.uk/published-guidance/acute-dental-problems-covid-19/ Available at:
- 6.American Dental Association ADA interim guidance for management of emergency and urgent dental care. https://www.ada.org/∼/media/CPS/Files/COVID/ADA_Int_Guidance_Mgmt_Emerg-Urg_Dental_COVID19.pdf Available at:
- 7.Samaranayake L., Reid J., Evans D. The efficacy of rubber dam isolation in reducing atmospheric bacterial contamination. ASDC J Dent Child. 1989;56:442–444. [PubMed] [Google Scholar]
- 8.American Dental Association What constitutes a dental emergency? https://success.ada.org/∼/media/CPS/Files/Open%20Files/ADA_COVID19_Dental_Emergency_DDS.pdf?_ga=2.253879752.110187285.1584496315-1622146531.1565271894 Available at:
- 9.Kohn W.G., Collins A.S., Cleveland J.L., Harte J.A., Eklund K.J., Malvitz D.M. Guidelines for infection control in dental health-care settings—2003. MMWR Recomm Rep. 2003;52:1–61. [PubMed] [Google Scholar]
- 10.Vandenberghe B., Jacobs R., Bosmans H. Modern dental imaging: a review of the current technology and clinical applications in dental practice. Eur Radiol. 2010;20:2637–2655. doi: 10.1007/s00330-010-1836-1. [DOI] [PubMed] [Google Scholar]