Transparency During a Health Care Crisis
In a time of crisis, such as the coronavirus disease 2019 (COVID-19) pandemic, the need for transparency from institutional and departmental leadership is amplified. Health care workers face increased stress, uncertainty about the future both at work and at home, a continuous onslaught of new information and policy changes, conflicting data sources, and the fear of exceeding the health care system’s capacity. Transparency and trust were found to be key elements in managing fear and uncertainty during a similar crisis, the severe acute respiratory syndrome (SARS) infectious outbreak in 2002 to 2004 [1].
Transparency from leadership requires openness, communication, and accountability in how the organization shares the current status and the algorithm for future decision making. Transparency is both informational, meaning the information supplied by leadership is truthful, and participatory, meaning stakeholders participate in identifying the information they need [2]. A health care crisis forces leaders to not just maintain but to increase transparency efforts. Designing and implementing communication methods that increase transparency during a pandemic can unify a department and build trust.
Communication Methods
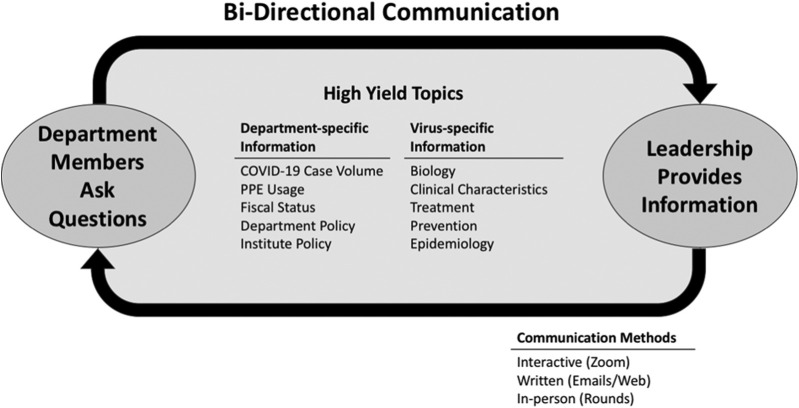
Our department quickly pivoted to new methods of regular, bidirectional department communication to (1) distribute the increased volume of information from a central source and (2) comply with physical distancing restrictions necessary to reduce viral spread. Communication includes a combination of interactive video conferences, written electronic communication, and in person, safely distanced chair “rounds” throughout the department. (See Fig. 1 .)
Fig 1.
Bidirectional communication to increase transparency. Bidirectional communication allows for a continuous flow of information between department members and leadership to meet the needs of the department. Communication centers on high-yield topics identified by department members. Bidirectional communication methods include interactive department meetings, electronic communication, and in person, safely distanced leadership rounds. COVID-19 = coronavirus disease 2019; PPE = personal protective equipment.
Interactive Zoom (San Jose, California) video conferences include weekly faculty conferences, twice-weekly section chief meetings, biweekly resident meetings, and section meetings held at each section’s discretion. Of importance, the Zoom platform is highly interactive and allows for bidirectional flow of information both from leadership to department members and from department members to leadership. Each meeting provides adequate time for follow-up question-and-answer sessions to ensure all faculty concerns are addressed.
Written communication from a central “radiology communication” source is distributed in the form of both daily updates and weekly summaries to supplement these video conferences. All video conferences, electronic communications, and current institution policies are hosted on a password-protected website available for reference at all times.
Furthermore, the department has ensured that leadership, extending to the chair, is accessible and approachable at all times via their mobile telephones.
Content
Our department’s transparency efforts have focused on providing clear, up-to-date, and accurate information that addresses the unanswered questions of our faculty members. Our faculty members informational needs fall into two main categories: (1) how the pandemic will affect our department and (2) what is currently known about the virus.
Regular interactive meetings, supplemented with daily and weekly written communication, provide an opportunity to discuss the current status of our department and institution and plans to move forward. The continuous, daily increases in available data regarding virus biology, clinical disease presentation, and potential treatment options necessitate this frequent department communication. We have recruited content experts from within and outside our institution to address the questions posed by our faculty through robust discussions at faculty meetings. Providing valid, accessible information through content experts has ensured that our department team members share common, reliable data sources.
Department-Specific Content
Volume of Cases
Regular status updates include the number of total and new infections and deaths at the international, national, local, and institution level. Detailed information on the number of COVID-19-related institution hospitalizations, intensive care unit (ICU) hospitalizations, and intubations or ventilated patients provides department team members with transparency on the institution’s current capacity. In addition to the distribution of hospital cases, updates include the number of available hospital beds, ICU beds, and plans for overflow if capacity is reached.
Personal Protective Equipment Status
We empowered the departmental quality and patient safety officer, a practicing interventional radiologist, to oversee personal protective equipment (PPE) policy and distribution. In addition to leading weekly discussions on current PPE guidelines, she is readily accessible at all times to answer questions from all department members. She maintains an open dialogue on the institution’s current supply of PPE and the backup plan should shortages arise.
Fiscal Impact
We provide faculty with the current fiscal impact of the pandemic and its potential impact on the health care system at the institution, department, and individual level to minimize speculation and rumor. During this stressful time when numerous businesses and health care systems across the country have announced layoffs and furloughs, we have found honest discussions about potential staffing changes to be helpful in alleviating undue department member stress.
Policy
Institution and department policies have changed rapidly throughout the COVID-19 pandemic. Regular discussions at the department and section level have been necessary to ensure that team members understand and implement policy change appropriately. This includes policy regarding which radiologic procedures and staff are considered essential versus nonessential, which procedures and diagnostic studies should be ordered and which should be placed on hold (and five guiding principles to help providers or staff make this decision), whether clinical research efforts may continue, and if faculty or staff might be repurposed to other duties to meet the needs of the institution.
Virus-Specific Content
Virus
The first cases of COVID-19, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), were initially reported in Wuhan, China in late December 2019. In the following weeks, SARS-CoV-2 spread rapidly across the globe. As of April 24, 2020, 2,682,225 cases and 187,329 deaths had been reported worldwide with 856,209 cases and 47,272 deaths reported in the United States alone [3].
SARS-CoV-2 is highly infectious and hypothesized to be spread primarily through large respiratory droplets [4]. Because SARS-CoV-2 is new to human beings, there is no current vaccine and there are no proven effective treatments.
Clinical Disease Characteristics
The initial clinical presentation often includes fever, shortness of breath, cough, myalgias, lethargy, diarrhea, and loss of smell or taste. Severe cases result in pneumonia, respiratory distress, septic shock, or multiple organ dysfunction [5]. Thrombotic events may be more common in patients with SARS-CoV-2 infection [6]. Data suggest that risk factors associated with worse outcomes include older age, male sex, underlying chronic disease conditions such as diabetes, cardiovascular disease, obesity, and hypertension [5]. Of concern, higher case rates and death rates have been observed in the African American population in the United States [7].
Clinical Care, Treatment, and Potential Therapies
Severe COVID-19 cases frequently require supportive respiratory care in the ICU setting with supplemental oxygen and intubation or mechanical ventilation for respiratory distress. The sheer number of cases requiring hospitalization, ICU care, and intubation or ventilation has the potential to overwhelm the health care system. Currently, there are no proven clinical treatments apart from supportive care, and there is no vaccine to impart immunity for SARS-CoV-2. However, there are several randomized controlled trials under way to identify therapeutic treatments and to develop effective vaccines.
Prevention and Infection Control in the Health Care Setting
Health care–associated transmission of SARS-CoV-2 is a major problem [4]. In addition to rigorous hand hygiene, health care workers should don appropriate PPE to minimize their own risk of acquiring infection. PPE includes gowns, gloves, masks or respirators, and eye protection. However, in many institutions, there is currently a shortage of PPE due to the overwhelming number of COVID-19 cases and the amount of PPE required by health care workers to protect themselves while caring for patients.
Epidemiology
Epidemiologic characterization of the frequency and pattern of health events such as viral pandemics uses a data-driven approach that incorporates time, place, and person. Providing department members with an epidemiologic perspective of SARS-CoV-2 and public health approaches to mitigation and containment is imperative for team members to understand department, institution, and government recommendations and policies.
Providing insight into epidemiology principles enables department team members to understand the strengths and limitations of the many models that have been generated to predict the future course of virus-associated infections and deaths. Models incorporating local data including reported cases, recoveries, deaths, transmission rates, and changes in mitigation policies (such as social distancing) likely have better descriptive and predictive projections compared with models lacking local information [8].
Furthermore, epidemiologic principles reinforce the importance of the public health approach to virus mitigation and containment through screening, testing, and isolation of identified cases.
Conclusion
During a pandemic, health care workers experience rapid, unexpected change. The resulting stress and the fear of the unknown can drive department members to envision a worst-case scenario. To alleviate department member stress and build trust, leadership can increase transparency through regularly scheduled, bidirectional communication. Although the necessary frequency of communications may decrease as this acute crisis phase passes, transparency and bidirectional communication will remain relevant and necessary tools for effective radiology leadership.
Footnotes
Dr Aronoff reports funding from National Center for Advancing Translational Sciences, Pfizer, Cayman Chemical Co, March of Dimes, National Institute of Allergy and Infectious Diseases, and Eunice Kennedy Shriver National Institute of Child Health and Human Development, and serves as an advisory board consultant for Summit Therapeutics, NAEJA-RGM Pharmaceuticals, BLC, Sanofi Pasteur, outside the submitted work. The other authors state that they have no conflict of interest related to the material discussed in this article. All authors are non-partnership track employees.
References
- 1.Menon K.U., Goh K.T. Transparency and trust: risk communications and the Singapore experience in managing SARS. Journal of Communication Management. 2005;9:375–383. [Google Scholar]
- 2.Balkin J.M. How mass media simulate political transparency. Cultural Values. 1999;3:393–413. [Google Scholar]
- 3.Johns Hopkins University of Medicine Coronavirus resource center. COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) https://coronavirus.jhu.edu/map.html Available at:
- 4.Hoe Gan W., Wah Lim J., Koh D. Preventing intra-hospital infection and transmission of COVID-19 in healthcare workers [E-pub ahead of print] Saf Health Work. 2020 doi: 10.1016/j.shaw.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grasselli G., Zangrillo A., Zanella A. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy [E-pub ahead of print] JAMA. 2020 doi: 10.1001/jama.2020.5394. Published Online: April 6, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kollias A., Kyriakoulis K.G., Dimakakos E., Poulakou G., Stergiou G.S., Syrigos K. Thromboembolic risk and anticoagulant therapy in COVID-19 patients: emerging evidence and call for action [E-pub ahead of print] Br J Haematol. 2020 doi: 10.1111/bjh.16727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yancy C.W. COVID-19 and African Americans [E-pub ahead of print] JAMA. 2020 doi: 10.1001/jama.2020.6548. Published Online: April 15, 2020. [DOI] [PubMed] [Google Scholar]
- 8.Vanderbilt School of Medicine Vanderbilt health policy COVID-19 modeling for Tennessee. https://www.vumc.org/health-policy/sites/default/files/public_files/COVID%20Modeling%20Release%204-10%20FINAL2.pdf Available at: