Abstract
The coronavirus disease-2019 (COVID-19) pandemic has caused an enormous strain on healthcare systems and society on a global scale. We report a new phenomenon of medical care avoidance among patients with acute coronary syndrome, which is due to concerns about contracting severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) infection during hospital stay, ultimately leading to dire clinical outcomes. (Level of Difficulty: Beginner.)
Key Words: acute coronary syndrome, complication, myocardial infarction
Abbreviations and Acronyms: COVID-19, coronavirus disease-2019; ECG, electrocardiography; EMS, emergency medical services; ICU, intensive care unit; LAD, left anterior descending artery; LV, left ventricular; MI, myocardial infarction; PCI, percutaneous coronary intervention; SARS-CoV-2, severe acute respiratory syndrome-coronavirus-2; STEMI, ST-segment elevation myocardial infarction
Graphical abstract
The coronavirus disease-2019 (COVID-19) pandemic has caused an enormous strain on health care systems and society on a global scale. We report a new…
The following patients came to our attention in March 2020, in the midst of the coronavirus disease-2019 (COVID-19) pandemic in the Lombardy region of Italy. None of them presented symptoms of COVID-19, and all tested negative for severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) infection.
Learning Objectives
-
•
To acknowledge the changes in healthcare utilization patterns and the existence of a medical care avoidance behavior among patients during the COVID-19 pandemic.
-
•
To appreciate the excess morbidity and mortality of the COVID-19 pandemic on non–COVID-19 patients.
Case Presentation
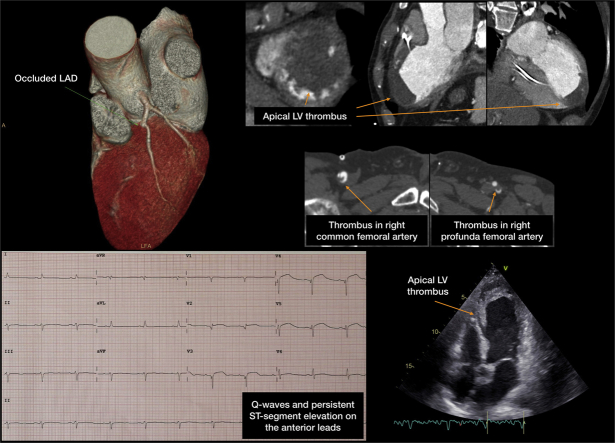
A 64-year-old man presented to the emergency department due to a 3-day history of worsening left lower limb pain, which was accompanied by cyanosis and paresthesia. Concomitantly, he also endorsed chest pressure and shortness of breath at rest for 10 days, for which he had been self-medicating with homemade natural remedies. Upon admission, critical left lower limb ischemia with skin mottling and cyanosis was noted. Fine crackles were audible throughout both lung fields, and jugular venous distension was noted. Electrocardiography (ECG) showed Q waves and ST-segment elevation on the anterior leads (Figure 1). Severe left ventricular (LV) dilation and systolic dysfunction with apical thrombosis were observed on transthoracic echocardiography (Video 1) and computed tomography angiography (Figure 1), which also revealed left anterior descending artery (LAD) occlusion, consistent with subacute anterior ST-segment elevation myocardial infarction (STEMI). Thromboembolic material was identified in both femoral arteries. Emergent amputation of the left lower limb was performed, which was complicated by cardiogenic shock necessitating inotropic and intra-aortic balloon pump. The patient slowly recovered and was discharged from the cardiac intensive care unit (ICU).
Figure 1.
Late-Presentation Anterior Myocardial Infarction Complicated by Apical Thrombosis With Systemic Embolization
Patient #1: electrocardiography computed tomography angiography, and echocardiography images showing late-presentation anterior myocardial infarction due to (sub)acute occlusion of the left anterior descending artery (LAD), with subsequent formation of an apical left ventricular (LV) thrombus, which induced thromboembolic showers into both femoral arteries, ultimately leading to critical limb ischemia in the left leg.
Online Video 1.
Transthoracic echocardiography of patient 1 showing severe left ventricular dilation and systolic dysfunction with apical thrombosis.
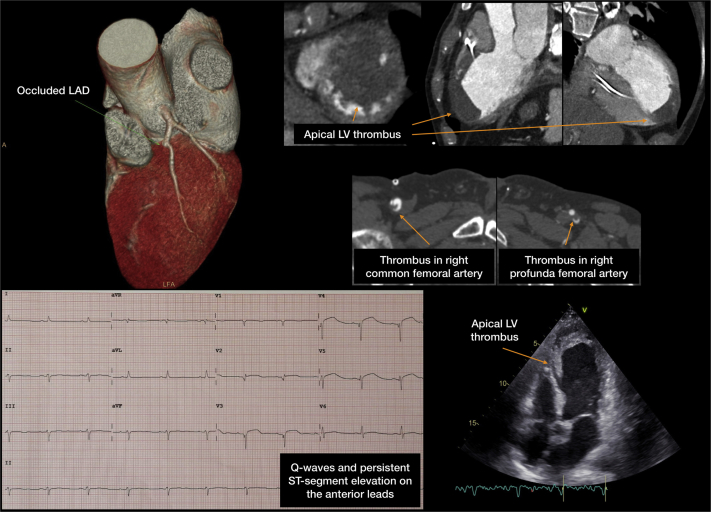
A 65-year-old woman presented to the emergency department with a 5-day history of progressive dyspnea and orthopnea, and was found to be hypotensive and in respiratory distress. A few days earlier, she had experienced a prolonged episode of epigastric tightness, which she had treated at home with antacids. Physical examination revealed bilateral crackles up to the apical regions, with abolished breath sounds at the bases bilaterally. Jugular venous distension was present, as well as bilateral pitting edema. Chest x-ray film was consistent with acute pulmonary edema. The ECG showed anterior lead ST-segment elevation and Q waves (Figure 2). Echocardiogram showed severe LV dysfunction with apical aneurysm and extensive anteroseptal and anteroapical dyskinesia (Video 2). Computed tomography angiography (Figure 2) confirmed the echocardiographic findings and demonstrated a critical stenosis of the LAD. The clinical picture was consistent with a late presentation of anterior myocardial infarction (MI). The patient was admitted to the cardiac ICU and required treatment with intravenous diuretics, inotropic support, and noninvasive ventilation, before being transferred to the cardiology ward.
Figure 2.
Late-Presentation Anterior Myocardial Infarction Complicated by Left Ventricular Aneurysm Formation
Patient #2: electrocardiography computed tomography angiography, and echocardiography images showing late-presentation anterior myocardial infarction (caused by plaque rupture on a long severe LAD lesion), with subsequent apical LV aneurysm formation. Abbreviations as in Figure 1.
Online Video 2.
Transthoracic echocardiography of patient 2 showed severe left ventricular dysfunction with apical aneurysm and extensive anteroseptal and anteroapical dyskinesia.
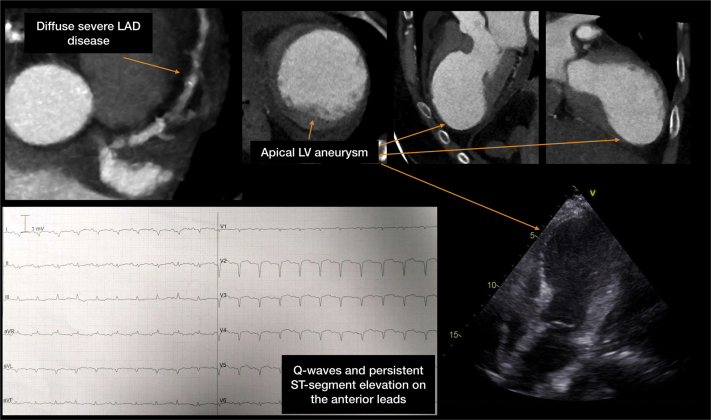
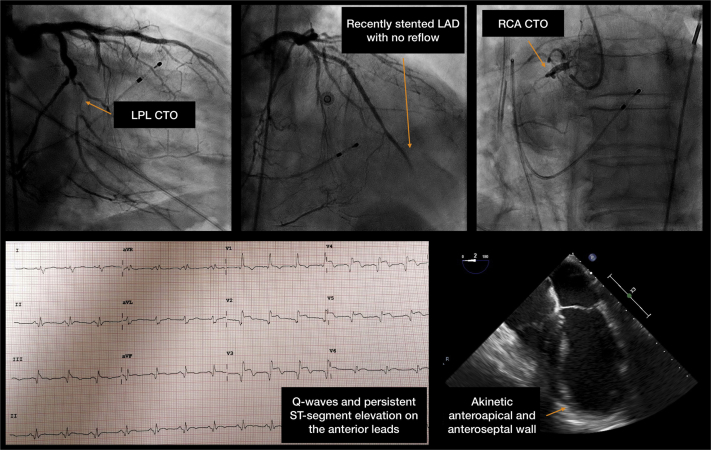
A 60-year-old man presented to the emergency department with hypotension, diaphoresis, and respiratory distress. He had experienced a 4-day history of crushing chest pain. The ECG showed ST-segment elevation and Q waves on the anterior leads (Figure 3), consistent with subacute anterior STEMI. Owing to ongoing pain and hypotension, he was transferred to the catheterization laboratory. Emergent coronary angiography (Figure 3) showed chronic total occlusion of the proximal right coronary artery and a left posterolateral branch, as well as acute thrombotic occlusion of the proximal LAD. He therefore underwent percutaneous coronary intervention (PCI) on the LAD. Upon stent implantation, the no-reflow phenomenon was observed (Video 3). The patient then suffered ventricular fibrillation and was defibrillated and intubated. After recovery of spontaneous circulation, he was in deep cardiogenic shock necessitating inotropes as well as mechanical circulatory support with Impella CP (Abiomed, Danvers, Massachusetts). Transesophageal echocardiography showed severe LV dysfunction, with anteroseptal, anteroapical, and lateral akinesia (Video 4). The patient subsequently presented multiorgan failure and died after few days.
Figure 3.
Late-Presentation Anterior Myocardial Infarction Complicated by Cardiogenic Shock
Patient #3: electrocardiography, coronary angiogram, and echocardiography images showing late-presentation anterior myocardial infarction in a patient with chronic total occlusion (CTO) of the left posterolateral branch (LPL) and proximal right coronary artery (RCA), as well as thrombotic occlusion of the mid LAD, which was treated with emergent percutaneous intervention and complicated with the no-reflow phenomenon and cardiac arrest. Transesophageal echocardiography showed extensive akinesia of the anteroseptal, anteroapical, and lateral wall and severe LV dysfunction. Abbreviations as in Figure 1.
Online Video 3.
The no-reflow phenomenon was observed in patient 3 upon stent implantation on the left anterior descending artery.
Online Video 4.
Transesophageal echocardiography of patient 3 showing severe left ventricular dysfunction, with anteroseptal, anteroapical, and lateral akinesia.
Discussion
The dramatic presentation of acute MI in these patients, as well as the permanent sequelae they will carry along, might have been reduced by an earlier referral to emergency medical services (EMS). Indeed, the impact of timing from symptoms onset to coronary reperfusion has been well established. Strategies to reduce ischemic time decrease mortality and the incidence of MI-related complications and, ultimately, heart failure (1). The creation of networks to provide around-the-clock fast access to primary PCI has improved STEMI outcomes (2). Furthermore, patient education programs can critically reduce total ischemic time by rising the awareness of ischemic symptoms and prompting rapid EMS contact (2).
However, in the cases presented previously, it was neither the absence of primary PCI programs nor the lack of patient education that led to delayed referral. In fact, all 3 subjects lived close to Milan, a province of Northern Italy heavily hit by the ongoing COVID-19 epidemic. When directly asked, the patients admitted having avoided seeking medical attention due to fear of acquiring SARS-CoV-2 infection in the hospitals, which were overwhelmed with COVID-19 patients. Fear is a well-known determinant of medical care avoidance, which, in turn, has been associated with a high toll in terms of health outcomes as well as financial costs (3). Fear of having a serious illness or undergoing medical tests and procedures (mainly owing to pain) has traditionally been identified as a barrier to pursue treatment (3). During epidemics, hospital avoidance behaviors have been reported, and were traditionally associated with misconceptions regarding disease severity and modes of transmission (4). The ongoing COVID-19 pandemic has received immense news coverage, and particular emphasis has been devoted to the description of the most common forms of contagion and places where SARS-CoV-2 spreads more easily. The 3 patients described previously lived in communities in which the magnitude of the COVID-19 outbreak was well over the national average, and they were very reluctant to seek medical attention. Specifically, on March 24, 2020 (the week when these 3 patients presented to our attention), 30,703 COVID-19 cases were present in Lombardy, which represented 44% of the 69,176 cases in Italy (5).
The burden associated with the treatment of subjects infected with SARS-CoV-2 may reduce the overall efficacy of a health care system facing multiple emergencies at once. EMS in Lombardy handled on average ∼2,500 missions/day before the pandemic, with time to first medical contact below 12 min for high-priority events. In contrast, in the third week of March 2020, EMS had to handle ∼3,200 missions/day (E. Ammirati, personal communication, March 2020). On the one hand, although data on time from call to first medical contact are not yet available, it is highly likely that ambulance wait times could have been prolonged due to the sudden increase in demand. Furthermore, given the overwhelming number of patients with critical SARS-CoV-2 infection, ICU bed shortage might prevent optimal care delivery to acute cardiovascular patients (6). On the other hand, ICU-sparing strategies are advocated to optimize resources when caring for cardiac patients (6). In this context, local government–led initiatives to concentrate all cardiovascular emergencies in few hub centers might be beneficial to keep emergency facilities rapidly available for cardiac patients while allowing most of other hospitals to focus on COVID-19 care. For confirmed or suspected SARS-CoV-2 patients, Chinese institutions have developed alternative protocols for acute MI, which favor fibrinolysis for STEMI and a delayed invasive or conservative strategy for non-STEMI (7), to decrease the risk of in-hospital spread of the virus. However, in Italy, health care authorities have preferred still guaranteeing the gold-standard primary PCI for all STEMI cases, following the strictest standards in terms of prevention of SARS-CoV-2 in-hospital spread.
Conclusions
Although utmost effort should be made to limit the propagation of the COVID-19 pandemic, attention should also be dedicated to not compromise acute cardiovascular care. In this difficult scenario, cardiologists can play a unique role in the (re-)education of patients to recognize symptoms of life-threatening cardiac conditions and seek appropriate care in a timely fashion. Late presenters may in fact pose a 2-fold problem: patients may experience worse prognosis and complications related to their underlying cardiac condition and, in turn, may require longer ICU and overall hospital stay. Priority should be given to less resource-consuming therapeutic options whenever possible, and novel organizational models are warranted to optimize cardiovascular care and outcomes during the COVID-19 emergency.
Footnotes
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the JACC: Case Reportsauthor instructions page.
Appendix
For supplemental videos, please see the online version of this paper.
References
- 1.Vogel B., Claessen B.E., Arnold S.V. ST-segment elevation myocardial infarction. Nat Rev Dis Prim. 2019;5:39. doi: 10.1038/s41572-019-0090-3. [DOI] [PubMed] [Google Scholar]
- 2.Antman E.M. Time is muscle: translation into practice. J Am Coll Cardiol. 2008;52:1216–1221. doi: 10.1016/j.jacc.2008.07.011. [DOI] [PubMed] [Google Scholar]
- 3.Kannan V.D., Veazie P.J. Predictors of avoiding medical care and reasons for avoidance behavior. Med Care. 2014;52:336–345. doi: 10.1097/MLR.0000000000000100. [DOI] [PubMed] [Google Scholar]
- 4.Lau J.T.F., Griffiths S., Choi K.C., Tsui H.Y. Avoidance behaviors and negative psychological responses in the general population in the initial stage of the H1N1 pandemic in Hong Kong. BMC Infect Dis. 2010;10:139. doi: 10.1186/1471-2334-10-139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.PCM-DPC dati forniti dal Ministero della Salute. Available at: http://www.salute.gov.it/imgs/C_17_pagineAree_5351_32_file.pdf. Accessed May 2020.
- 6.Driggin E., Madhavan M.V., Bikdeli B. Cardiovascular considerations for patients, health care workers, and health systems during the coronavirus disease 2019 (COVID-19) pandemic. J Am Coll Cardiol. 2020;75:2352–2371. doi: 10.1016/j.jacc.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zeng J., Huang J., Pan L. How to balance acute myocardial infarction and COVID-19: the protocols from Sichuan Provincial People’s Hospital. Intensive Care Med. 2020;46:1111–1113. doi: 10.1007/s00134-020-05993-9. [DOI] [PMC free article] [PubMed] [Google Scholar]