Abstract
Introduction:
Residents do not feel confident or competent in leading inpatient resuscitations. This is a crucial part of training future internists. Our objective was to develop a low-cost intervention to improve resident confidence in leading cardiopulmonary resuscitations and patient outcomes.
Methods:
A “code-conference” including a lecture on a high-yield topic, a low-fidelity simulation, and review of resident-led resuscitations was created at our institution for the 2017-2018 academic year. Patient outcomes were assessed using objective measures of return of spontaneous circulation (ROSC) and survival to discharge (sDC). Confidence was assessed via survey before and after the intervention, with a focus on beginning postgraduate year 2 (PGY-2) residents.
Results:
In 2017, 8 out of 8 (100%) PGY-2 residents responded, while in 2018, 8 out of 10 (80%) responded. Patient outcomes did not show a statistically significant improvement. There was a trend toward positive outcomes in the resident group alone. Return of spontaneous circulation increased from 63% to 79% (P = .08, total n = 97). Resident confidence was not improved in a statistically significant way, but there was a trend toward improvement and residents agreed it was an important part of their training.
Discussion:
There was no statistically significant improvement in code-blue outcomes; however, there was a positive trend with increased ROSC and stable sDC for resident-led resuscitations, despite hospital-wide decreases in both. Resident confidence also showed a positive trend with no statistical significant changes. It is possible to institute a low-cost high-yield intervention to improved resident confidence in leading code-blue resuscitations. It may also improve patient outcomes; however, further studies are needed to determine if it can improve patient survival outcomes.
Keywords: Graduate medical education, cardiopulmonary resuscitation, internal medicine, simulation training
Introduction
There are nearly 300 000 inpatient cardiac arrests each year; 24.8% of which are survived.1,2 In most hospitals, inpatient resuscitations are led by physicians.3 These physicians are frequently internal medicine (IM) trained or IM residents.4-7 As more and more internists enter hospital medicine, it is vital that adequate training for leading resuscitation teams is provided. Decreased duty hours and increased prevalence of Do Not Resuscitate orders make it more difficult for residents to gain experience in leading resuscitations.8,9 Many programs adopt a “see one, do one, teach one” approach, which is dependent on the quality of the teacher as well as the motivation and experiences of the learner.4,7
Fifty percent to 80% of residents feel underprepared to lead resuscitation efforts.4,10,11 This may be due to lack of experience or lack of specialized training.4,6,7 Intentional practice, spaced learning, and immediate feedback can be used to develop resuscitation leaders and are likely more effective than the “see one, do one, teach one” approach.10,12 Resuscitation leaders must have the capacity to communicate well, understand complex medical patients in a brief amount of time, make decisions on therapies, facilitate transitions of care for critically ill patients, have situational awareness, and understand team dynamics (or have training in crisis resource management).13-15 In addition to this, resuscitation directors must also monitor the quality of the resuscitation. The American Heart Association recommends several small steps to ensure resuscitations are given the best chance at success including increasing the amount of time for ongoing compressions, ensuring compression depth and rate, and ensuring ventilation amount and rate.16
At our community-based institution, approximately half of our IM trainees pursue careers in hospital medicine. Prior to this intervention, interns were taught how to lead resuscitations by undergoing ACLS (Advanced Cardiovascular Life Support) certification, observing their upper levels, and then assuming leadership and teaching responsibilities on matriculation into their postgraduate year 2 (PGY-2). This inadequate training led to fear and anxiety when approaching resuscitations. This study aims to describe the results of a low-cost intervention to increase resident confidence and improve patient outcomes.
Methods
Study design
This is a before and after historical cohort study. Patient outcomes and resident confidence were measured before and after the introduction of a “Code Conference” (CC) described below. This research was reviewed by the Metro West Medical Center IRB and given exempt status.
Code conference
To better prepare physicians to lead resuscitations, we designed and instituted a CC which took place 8 times throughout the 2017-2018 academic year. This was attended by resident physicians, chief medical residents, an associate program director and faculty advisor (E.C.T.), critical care physicians and staff, clinical pharmacists, nurses, and nursing and medical students. The attendance at these meetings ranged from 20 to 45 residents and 10 to 20 attendings and other ancillary staff. These sessions would last 50 to 75 minutes. This would begin with a high-yield resuscitation topic lecture lasting 15 minutes. The topics included an orientation to the crash cart, overview of vasopressors, and review of cardiac rhythms. It also included discussions of when to stop a code, targeted temperature management, and how to gather information when resuscitating a patient who is not known to the provider. This was then followed by a low-fidelity resuscitation simulation led by an intern (PGY-1) lasting 15 to 20 minutes. The resuscitation team was made up of volunteers from those in attendance including pharmacists, nurses, other residents, and students. The simulation involved a mannequin (Laerdal Resusci Anne Basic—discontinued in 2013) for chest compressions, a manual resuscitator bag, and a PowerPoint slide that revealed different rhythms and other clinical information for the intern. When completed, there was an immediate debriefing with input from those who participated in the activity as well as the other observers lasting 15 to 20 minutes. This debriefing focused on the team management skills of the intern but also touched on cardiopulmonary resuscitation (CPR) quality, rhythm analysis, and other clinical decisions made in the course of the resuscitation simulation. The debriefers had no formal training but extensive clinical experience in leading resuscitations and teaching. Afterward, upper-level residents presented actual resuscitations they had completed in the preceding month for teaching, feedback, and evaluation by the assembled staff lasting approximately 15 minutes.
Patient outcomes
To assess the impact of CC on patient outcomes, we gathered data from the year prior to implementation as well as the academic year after the intervention. Data points included specification of who led the resuscitations, return of spontaneous circulation (ROSC), survival to discharge (sDC), time of day (7 am-7 pm or 7 pm-7 am), and location (intensive care unit [ICU] vs medical floor). Data were gathered from review of electronic health records for all inpatient resuscitations that IM residents respond to, excluding the neonatal intensive care unit, heart catheterization lab, operating room (OR), and the emergency department. If a patient coded multiple times throughout a hospitalization, the primary code was the only event included.
Confidence
To assess resident confidence, a survey (Table 1) was administered to the residents at the beginning of each academic year, before and after CC was implemented. There were 2 cohorts who had completed their intern year. One had completed their intern year prior to the intervention (group 1, n = 8). The other had completed their intern year while the intervention was ongoing (group 2, n = 8). The main focus of the intervention was on the confidence of PGY-2 residents, who at the times of the survey had been PGY-2 residents for approximately 30 days. We wanted to assess the impact on this group in particular, as they were the group transitioning from no resuscitation experience into leadership roles in resuscitations.
Table 1.
Survey questions.
| Question | Format |
|---|---|
| 1. How many resuscitations have you attended? | Numeric |
| 2. How many have you stayed the entire time? | Numeric |
| 3. How many have you played an active role? | Numeric |
| 4. How many have you led? | Numeric |
| 5. How many were you the first MD present? | Numeric |
| 6. How many did you delay/avoid arrival to avoid leading? | Numeric |
| 7. I do not feel anxious when approaching a resuscitation | 1-5 Likert-type scale |
| 8. I feel confident in my knowledge of ACLS protocols | 1-5 Likert-type scale |
| 9. I feel confident following orders during a resuscitation | 1-5 Likert-type scale |
| 10. I feel confident recognizing cardiac rhythms and responding appropriately | 1-5 Likert-type scale |
| 11. I feel confident leading a resuscitation team | 1-5 Likert-type scale |
| 12. I feel confident teaching others to lead a team | 1-5 Likert-type scale |
| Postintervention questions | |
| 13. Lectures preceding simulations were important for my education as an IM resident | 1-5 Likert-type scale |
| 14. The simulations were important for my . . . (see above) | 1-5 Likert-type scale |
| 15. Feedback after the simulations was important . . . | 1-5 Likert-type scale |
| 16. Space for comments regarding lectures, simulations, and feedback | Free text, long answer |
Abbreviations: ACLS, Advanced Cardiovascular Life Support; IM, internal medicine.
The first 6 questions asked about resident exposure to codes. The second 6 asked questions regarding their confidence in leading codes. A 5-point Likert-type scale was used to capture the response of residents (1, strongly disagree; 2, disagree; 3, neither agree nor disagree; 4, agree; 5, strongly agree). For questions 7 to 12, we did not expect to see a significant increase in questions 8, 9, and 10. We did expect to see an increase in question 7 reflecting increased confidence, question 11 reflecting leadership, and question 12 reflecting education.
Statistical analysis
Data were analyzed using SAS 9.4. Both ROSC and sDC were analyzed using a chi-square test for each group. Both ROSC and sDC were analyzed using a chi-square test to compare the groups of practitioners both before and after the intervention. Multivariate logistic regression analysis was run after review using Microsoft Excel to consider the confounding effect of location and time of day. Due to this being a single-center study with a limited number of events, a post hoc power analysis was performed using nQuery Advisor v7.
Due to the very low number of residents entering their PGY-2 year (8 before the intervention, 10 post intervention), these findings were presumed to be statistically non-significant. Normality was assessed using kurtosis and skewness. A chi-square test was used to evaluate the responses of the PGY-2 year. Standard deviation was calculated using Microsoft Excel.
Results
Prior to the intervention, 151 code-blue events were recorded. Residents led 49 resuscitations (32.5%), Intensivists led 46 (30.5%), and others led the remaining 56 (37.1%). Of the resident-led interventions, most were overnight (61.2%), and outside the ICU (55.3%); of all resuscitations outside the ICU, residents led most (21/38, 55.3%) (Table 2).
Table 2.
Demographics of inpatient resuscitations.
| Total | Resident | ICU MD | Other | |
|---|---|---|---|---|
| Pre-intervention (%) | 151 | 49 (32.5%) | 46 (30.5%) | 56 (37.1%) |
| Floor (%) | 38 | 21 (55.3%) | 3 (7.8%) | 14 (36.8%) |
| PM (7 pm-7 am) (%) | 70 | 30 (42.9%) | 8 (11.4%) | 32 (45.7%) |
| Post intervention (%) | 145 | 48 (33.1%) | 60 (41.3%) | 37 (25.5%) |
| Floor (%) | 63 | 28 (44.4%) | 11 (17.5%) | 24 (38.1%) |
| PM (7 pm-7 am) (%) | 62 | 32 (51.6%) | 14 (22.6%) | 16 (25.8%) |
Abbreviation: ICU, intensive care unit.
During the intervention, 145 code-blue events were recorded. Of these, residents led 48 (33.1%), intensivists led 60 (39.7%), and others led 37 (24.5%). Of resident-led resuscitations, most were overnight (51.6%) and in the ICU (55.6%); residents led most overnight resuscitations (51.6%)
Odds ratio for sDC in the ICU was 0.896 (95% confidence interval [CI], 0.092-8.707). For PM events odds ratio was 0.587 (95% CI, 0.298-1.156). For ROSC, odds ratio in the ICU was 0.651 (95% CI, 0.067-6.294) and PM events had an odds ratio of 0.893 (95% CI, 0.519-1.538).
No statistically significant changes in ROSC were found between any 2 variables (Table 3). There was a trend toward increased ROSC in resident-led resuscitations and a trend toward decreased ROSC and sDC for resuscitations led by the other groups. In the pre-intervention phase, resuscitations led on the floor were associated with a lower sDC compared with resuscitations led in the ICU (36% vs 16%, P = .041). There were no other statistically significant differences between 2 variables either pre- or post intervention (Table 3). Resident-led resuscitations maintained the same sDC despite a drop in the sDC in the other 2 groups.
Table 3.
Outcomes of inpatient resuscitations.
| Significance | Pre | Post | P value |
|---|---|---|---|
| Resident ROSC% | 63 | 79 | .08 |
| ICU MD ROSC% | 80 | 63 | .06 |
| Other ROSC% | 75 | 59 | .11 |
| Resident sDC% | 16 | 16 | .96 |
| ICU MD sDC% | 26 | 16 | .24 |
| Other sDC% | 21 | 13 | .33 |
Abbreviations: ICU, intensive care unit; ROSC, return of spontaneous circulation; sDC, survival to discharge. Italic font signifies P value.
Results from a multivariate logistical regression are shown in Table 4. The only statistical significance was found in the ability of resuscitation outside of the ICU to predict sDC (OR, 1.186; 95% CI, 1.166-1.207; P = .001). When controlling for other variables, nothing else was found to be statistically significant.
Table 4.
Results from multivariate logistical regression.
| Coefficients | P value | Odds ratio (95% CI) | |
|---|---|---|---|
| ROSC | |||
| Intercept | 0.75 | 1.12E-29 | – |
| PM | −0.03 | .25 | 0.974 (0.973-0.975) |
| Floor | −0.01 | .93 | 0.995 (0.994-0.995) |
| Group | −0.01 | .81 | 0.992 (0.991-0.992) |
| Intervention | −0.05 | .42 | 0.956 (0.951-0.961) |
| sDC | |||
| Intercept | 0.13 | .01 | – |
| PM | −0.03 | .14 | 0.973(0.972-0.974) |
| Floor | 0.17 | .001 | 1.186 (1.166-1.207) |
| Group | 0.05 | .08 | 1.053 (1.050-1.056) |
| Intervention | −0.09 | .06 | 0.916 (0.909-0.924) |
Abbreviations: CI, confidence interval; ROSC, return of spontaneous circulation; sDC, survival to discharge.
The survey shown in Table 1 was administered twice. In 2017, 8 out of 8 (100%) of PGY-2 residents responded. In 2018, 8 out of 10 (80%) of PGY-2 residents responded. For questions 1 to 6, no significant difference was seen (Figure 1).
Figure 1.
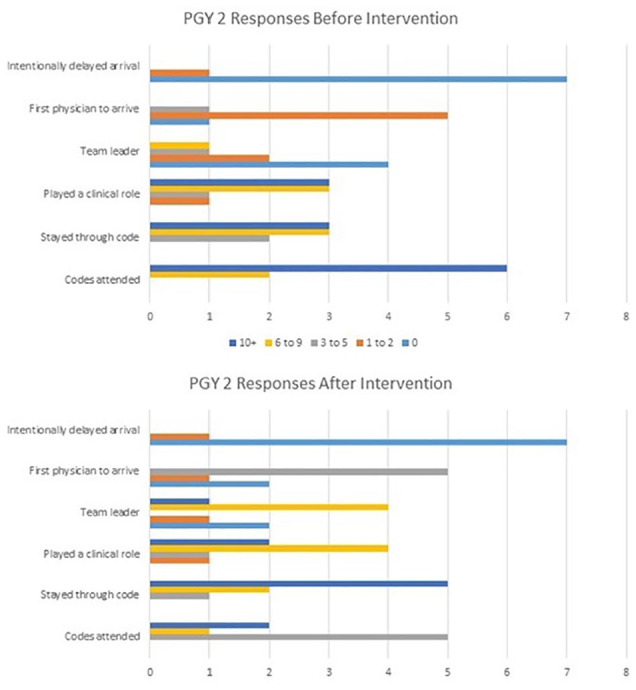
PGY-2 experiences before and after the intervention.
Results are displayed in Table 5. Residents did express a tendency toward increased confidence based on our survey data. There was no statistically significant change. We also gave an opportunity for the PGY-2 residents and PGY-3 residents to provide feedback on the importance of these interventions to their education using a 1 to 5 Likert-type scale. Those results are also displayed in Table 5.
Table 5.
PGY-2 survey responses.
| Average PGY-2 confidence | Pre (rising PGY-2) | Post (rising PGY-2) | Standard deviation | P value | Kurtosis (skewness) |
|---|---|---|---|---|---|
| 7. I do not feel anxious when approaching a resuscitation | 2.125 | 3.125 | Pre = 1.13 Post = 0.99 |
.63 | Pre = –0.99 (0.49) Post = 2.98 (–1.49) |
| 8. I feel confident in my knowledge of ACLS protocols | 3.375 | 3.875 | Pre = 1.19 Post = 0.83 |
.19 | Pre = 1.87 (0.97) Post = 4.97 (–1.69) |
| 9. I feel confident following orders during a resuscitation | 4.25 | 4.375 | Pre = 0.71 Post = 0.92 |
.26 | Pre = –0.23 (–0.40) Post = –1.04 (–1.00) |
| 10. I feel confident recognizing cardiac rhythms and responding appropriately | 3.25 | 3.75 | Pre = 1.16 Post = 0.71 |
.39 | Pre = 0.62 (–1.36) Post = –0.23 (0.40) |
| 11. I feel confident leading a resuscitation team | 2.50 | 3.625 | Pre = 1.20 Post = 0.92 |
.4 | Pre = –1.46 (0) Post = 0.42 (–0.49) |
| 12. I feel confident teaching others to lead a team. | 2.50 | 3.125 | Pre = 1.20 Post = 0.64 |
.19 | Pre = –1.46 (0) Post = 0.74 (–0.07) |
| Importance to education | PGY-2 | PGY-3 | |||
| High-yield resuscitation lectures | 4.25 | 3.875 | |||
| Low-fidelity simulations | 4.75 | 3.875 | Feedback after simulations | 4.50 | 4.00 |
Abbreviations: ACLS, Advanced Cardiovascular Life Support; PGY-2, postgraduate year 2.
Discussion
This low-cost intervention was designed and tested to see improvements in resident competence and confidence in leading resuscitations. Statistical significance was not achieved in any objective comparison between our pre-intervention and postintervention data. While previous completion of an accredited ACLS course has been shown to improve patient outcomes, it has proven difficult to improve outcomes further than this.17 There have been some successes with immediate feedback devices that communicate the quality of compressions and other objective measurements in the midst of a code; these efforts are usually combined with feedback on real resuscitations in a timely manner.18,19 These efforts are not always successful, however, and seem to depend largely on immediate feedback on quality of chest compressions.20 The use of simulation does not have robust evidence for increasing favorable patient outcomes, and many of these studies focus on resident confidence as subjectively reported.6,10,13
Resident success in obtaining ROSC greatly increased in our intervention period. This was despite a hospital-wide decrease in ROSC. The most likely reason for this, the changing role of intensivists during our intervention, is explored below. The residents were also not blinded to the intervention, and so the Hawthorne effect may have introduced some bias. This also correlates with a stable sDC in the resident group, despite a drop in these numbers throughout our institution. The answers to questions 8, 9, and 10 showed an increase less than or equal to 0.5 points when comparing the 2 groups, as we expected. Questions 7, 11, and 12 all increased by greater than 0.5 points. The PGY-2 residents who experienced the intervention rated all aspects of it with an average of greater than 4 on the 1 to 5 Likert-type scale. The PGY-3 residents who attended the conferences but did not participate (except to give feedback) rated all aspects as greater than 3 points on the 1 to 5 Likert-type scale. Our survey also discovered that residents would occasionally delay arrival to codes to avoid being the resuscitation leader. We hypothesize that this is secondary to lack of confidence, but it is possible that there are other reasons we did not uncover in our study. Our study did not show any substantial difference in the number of code experiences for the rising PGY-2 residents, but it did show an increase in subjective confidence. Whether or not this correlates to improved outcomes for patients cannot be evaluated, but is worth further study. While these results are interesting, ultimately our number of data points (n = 16) are too small to evaluate actual statistical significance.
This study has multiple limitations. It is an observational study and cannot prove causation, but only infer association. The retrospective chart review aspect made some data points difficult to gather, requiring the authors to evaluate multiple pieces of documentation from physicians, nurses, and other members of the care team to determine who led the code, where the code was, and what the outcomes were. Obviously there are many confounding factors that determine the success or failure of a resuscitation attempt. These can include patient age, comorbidities, location, time, initial rhythm (shockable or not), and duration of resuscitation. The only factors we captured were time and location. Finally, this was a single-center study with a set number of events per academic year. This led the study to be underpowered and prone to type 2 error.
Another limitation is the changing role of intensivists at our institution. Previously, resuscitations in all of the ICUs were announced via overhead page, and the on-call medicine resident was alerted by pager. Around the beginning of our intervention, codes in the cardiac and neurologic ICUs were no longer announced overhead or by pager, as the intensivist team always had members present in those ICUs. In addition, the intensivist team began leading some resuscitations on the floor at the beginning of our intervention.
Finally, there was no objective way to adequately capture the pre-arrest potential for a positive outcome or stratify the complexity and comorbidities of the resuscitation efforts. This makes it likely that as the intensivist took on more resuscitations outside and in the ICU, they took on more patients with poor prognoses at baseline, likely affecting their numbers as well as those of the residents.
Conclusions
We have described a low-cost, low-fidelity effort to increase resident confidence in leading code-blue resuscitations for IM residents in a community-based hospital program. While patient outcomes and resident confidence was not improved in a statistically significant way, there were trends noted toward positive outcomes in both categories. Ultimately the study was underpowered to detect a significant improvement in either endpoint.
Footnotes
Declaration of Conflicting Interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
Authors’ Note: This research was reviewed by the Metro West Medical Center IRB and given exempt status. If required by the IRB, patient consent was obtained.
Author Contributions: NTD conceived of the idea for this research. NTD and ECT designed and performed the intervention. NTD and CMM performed data entry and analysis. All authors discussed the results and contributed to writing and editing the manuscript.
ORCID iD: Nathan T Douthit  https://orcid.org/0000-0002-8314-4207
https://orcid.org/0000-0002-8314-4207
References
- 1. Ofoma UR, Basnet S, Berger A, Kirchner HL, Girotra S. Trends in survival after in-hospital cardiac arrest during nights and weekends. J Am Coll Cardiol. 2018;71:402-411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Holmberg MJ, Ross CE, Fitzmaurice GM, et al. Annual incidence of adult and pediatric in-hospital cardiac arrest in the United States. Circ Cardiovasc Qual Outcomes. 2019;12:e005580. [PMC free article] [PubMed] [Google Scholar]
- 3. Edelson DP, Yuen TC, Mancini ME, et al. Hospital cardiac arrest resuscitation practice in the United States: a nationally representative survey. J Hosp Med. 2014;9:353-357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dine CJ, Gersh RE, Leary M, Riegel BJ, Bellini LM, Abella BS. Improving cardiopulmonary resuscitation quality and resuscitation training by combining audiovisual feedback and debriefing. Crit Care Med. 2008;36:2817-2822. [DOI] [PubMed] [Google Scholar]
- 5. Hayes CW, Rhee A, Detsky ME, Leblanc VR, Wax RS. Residents feel unprepared and unsupervised as leaders of cardiac arrest teams in teaching hospitals: a survey of internal medicine residents. Crit Care Med. 2007;35:1668-1672. [DOI] [PubMed] [Google Scholar]
- 6. Cappelle C, Paul RI. Educating residents: the effects of a mock code program. Resuscitation. 1996;31:107-111. [DOI] [PubMed] [Google Scholar]
- 7. Lauridsen KG, Schmidt AS, Adelborg K, Løfgren B. Organisation of in-hospital cardiac arrest teams—a nationwide study. Resuscitation. 2015;89:123-128. [DOI] [PubMed] [Google Scholar]
- 8. Mickelsen S, McNeil R, Parikh P, Persoff J. Reduced resident “code blue” experience in the era of quality improvement: new challenges in physician training. Acad Med. 2011;86:726-730. [DOI] [PubMed] [Google Scholar]
- 9. Yang J, Howell MD. Commentary: is the glass half empty? Code blue training in the modern era. Acad Med. 2011;86:680-683. [DOI] [PubMed] [Google Scholar]
- 10. Stefan MS, Belforti RK, Langlois G, Rothberg MB. A simulation-based program to train medical residents to lead and perform advanced cardiovascular life support. Hosp Pract (1995). 2011;39:63-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Seethala RR, Esposito EC, Abella BS. Approaches to improving cardiac arrest resuscitation performance. Curr Opin Crit Care. 2010;16:196-202. [DOI] [PubMed] [Google Scholar]
- 12. Patocka C, Khan F, Dubrovsky AS, Brody D, Bank I, Bhanji F. Pediatric resuscitation training—instruction all at once or spaced over time? Resuscitation. 2015;88:6-11. [DOI] [PubMed] [Google Scholar]
- 13. Hunziker S, Bühlmann C, Tschan F, et al. Brief leadership instructions improve cardiopulmonary resuscitation in a high-fidelity simulation: a randomized controlled trial. Crit Care Med. 2010;38:1086-1091. [DOI] [PubMed] [Google Scholar]
- 14. Yeung JH, Ong GJ, Davies RP, Gao F, Perkins GD. Factors affecting team leadership skills and their relationship with quality of cardiopulmonary resuscitation. Crit Care Med. 2012;40:2617-2621. [DOI] [PubMed] [Google Scholar]
- 15. Joyce MF, Berg S, Bittner EA. Practical strategies for increasing efficiency and effectiveness in critical care education. World J Crit Care Med. 2017;6:1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Meaney PA, Bobrow BJ, Mancini ME, et al. CPR quality: improving cardiac resuscitation outcomes both inside and outside the hospital: a consensus statement from the American Heart Association. Circulation. 2013;128:417-435. [DOI] [PubMed] [Google Scholar]
- 17. Lockey A, Lin Y, Cheng A. Impact of adult advanced cardiac life support course participation on patient outcomes—a systematic review and meta-analysis. Resuscitation. 2018;129:48-54. [DOI] [PubMed] [Google Scholar]
- 18. Edelson DP, Litzinger B, Arora V, et al. Improving in-hospital cardiac arrest process and outcomes with performance debriefing. Arch Intern Med. 2008;168:1063-1069. [DOI] [PubMed] [Google Scholar]
- 19. Wolfe H, Zebuhr C, Topjian AA, et al. Interdisciplinary ICU cardiac arrest debriefing improves survival outcomes. Crit Care Med. 2014;42:1688-1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Couper K, Kimani PK, Abella BS, et al. The system-wide effect of real-time audiovisual feedback and postevent debriefing for in-hospital cardiac arrest: the cardiopulmonary resuscitation quality improvement initiative. Crit Care Med. 2015;43:2321-2331. [DOI] [PMC free article] [PubMed] [Google Scholar]


