Abstract
Objective: To analyze the clinical outcomes of patients with type 2 diabetes (T2D) before and after implementation of a personalized care plan in the primary health care setting. Design: Observational, retrospective, real-world study. Setting: All T2D patients with a care plan in Rovaniemi Health Center, Rovaniemi, Finland, for whom data were available from a baseline visit (in 2013-2015 during which the care plan was written) and from a follow-up visit, including an updated care plan by the year 2017. Subjects: In total, 447 patients were included. Mean age was 66.9 (SD 10.1) years, 58.8% were male, 15.4% were smokers, 33.1% had vascular disease, and 17.0% were receiving insulin treatment. The mean follow-up time was 14.4 months. Main Outcome Measures: Glycosylated hemoglobin A1 (HbA1c), low-density lipoprotein (LDL), blood pressure (BP), and body mass index (BMI). Clinical values were taken at both baseline and follow-up. Results: LDL decreased by 0.2 mmol/L, systolic blood pressure by 2.2 mm Hg, diastolic blood pressure by 1.5 mm Hg, and BMI by 0.5 kg/m2 (P < .05 for each). The decrease in HbA1c was 0.8 mmol/mol (P = .07). Conclusion: We observed statistically significant decreases in LDL, BP, and BMI. Our results indicate that, over 14 months of follow-up, implementation of a written care plan was associated with small improvements in the clinical outcomes of T2D patients in a primary health care study population in a real-world setting.
Keywords: health outcomes, managed care, patient-centeredness, prevention, primary care
Introduction
Type 2 diabetes (T2D) is major risk factor for cardiovascular disease. Therefore, one of the aims of its treatment is to maintain control of cardiovascular risk factors to prevent macro- and microvascular complications.1 Self-management is an important aspect of T2D treatment, and can be enhanced with the implementation of a personalized care plan.2 Personalized care plans draw upon the “chronic care model,”3,4 which regards the patients as experts in their own disease, and actively involves them in their own health care strategy. A care plan requires motivational discussion between care providers and the patient. It includes personalized goal setting and an action plan for treatment.2 Although legislative frameworks encourage the preparation of care plans for patients with chronic disease,5,6 only 3.3% of primary care patients in Great Britain5 and 16% of T2D patients in Finland7 have been reported to have a care plan in place. Limited availability of resources and other factors may prevent the implementation and utilization of care plans in clinical practice.8,9
A Cochrane review examined the application of care plan–related working methods (such as goal setting and patient-centric working) in the treatment of T2D.2 It found that such methodology was associated with improvements in glycosylated hemoglobin A1 (HbA1c) and systolic blood pressure (sBP).10,11 Additionally, studies have examined the effects of care plan–related working methods on low-density lipoprotein (LDL) levels in patients with T2D,10-14 but only 1 study reported an improvement.13 To date, no evidence has been published to show that personalized care planning can decrease body mass index (BMI) in T2D patients.12,14-16 However, it is difficult to compare the results of studies in this field because of variations in the terminology used, the intervention methods and their implementation, and in the selection of study populations (eg, variations in socioeconomic status and comorbidity profiles).2 Moreover, few studies have examined the impact on T2D patients’ clinical outcomes of the introduction of a care plan in the real-world clinical setting. In a study among primary care T2D patients, those who had a care plan were observed to have better control in sBP and LDL, and were more likely to use statins than T2D patients without a care plan.7
The present study aimed to evaluate the clinical outcomes (HbA1c, LDL, blood pressure [BP], and BMI) among T2D patients before, and during 14 months of follow-up after the commissioning of a care plan established according to national care plan instructions in a primary health care setting. The proportion of patients who achieved the recommended treatment targets for blood glucose and cardiovascular risk factors at baseline and follow-up were also examined. We hypothesized that in this real-world setting, this population of T2D patients all of whom received a care plan would demonstrate: (1) partial improvements in cardiovascular risk factors and (2) an increase in the proportion of patients achieving recommended European treatment targets for HbA1c, LDL, and BP.
Methods
This was a retrospective analysis of data on patients who were being treated for T2D at the Health Center of Rovaniemi, Finland. The study population included those with a care plan and relevant data available from clinical visits for the years 2013 to 2015, and additional updated care plan in 2016-2017.
In 2013, Rovaniemi Health Center introduced a care plan for use as a practical tool in the treatment of chronic conditions, including T2D. The care plan is a structured document, which gathers patients’ treatment information; it is accompanied by a comprehensive, structured care plan form, which is maintained in each patient’s records. Prior to the introduction of the care plan, all health care professionals were trained in care planning with the importance of its patient-centric approach and target-setting being highlighted. The implementation of the care plan was managed successfully by means of breakthrough method.17 In a breakthrough method, the implemented topic is predesigned and systematically highlighted in work community by selected peer-fellow workers during several month of period. The protocol includes also recurrent reporting of quality indicators to the whole work community.17 Subsequently our successful implementation offered us a possibility to do real-world research retrospectively, but correspondingly prevented us to establish the control group.
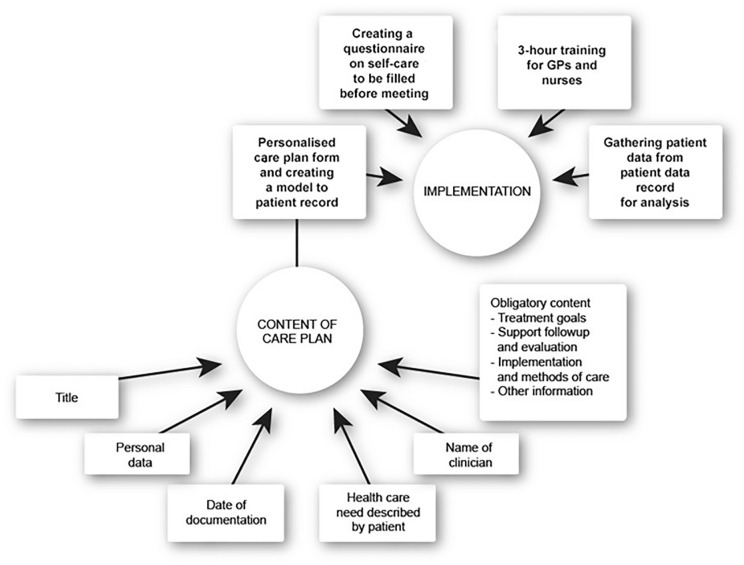
The care plan implemented in Rovaniemi Health Center is based on care plan form of the Finnish National Institute for Health and Welfare, which was designed for national use.18 This is a structured document, which includes subtopics as follows: (1) the need for treatment (described by a patient), (2) goals for treatment (which have been established via collaboration between the patient and the health care professional), (3) action plan to reach the goals, and (4) follow-up plan (following control visits, laboratory tests, etc). At the time of the care plan’s introduction, patients with T2D received a questionnaire on self-care, which they completed before their next follow-up visit to facilitate a patient-centric collaborative consultation. The completed questionnaires were used by the center’s 42 general practitioners and 29 nurses to draw up a baseline care plan for each patient. Figure 1 shows how a personalized care plan is implemented for a patient at the Rovaniemi Health Center, and what it contains. An example care plan can be found in the Supplementary appendix.
Figure 1.
Content and implementation of the personalized care plan used in Rovaniemi Health Center, Rovaniemi, Finland.
Study Protocol and Data Collection
This study followed retrospective and real-world protocol. The data were collected from patient records by 3 researchers. For the purposes of the study, the subjects were identified only by their assigned study ID. Due to the observational study setting, no randomization was performed. Study data parameters consisted only of information recorded as part of patients’ routine baseline and follow-up visits. Data were collected anonymously only for scientific purposes. Participants’ personal data were stored confidentially at the Rovaniemi Health Center. The study protocol was approved by the Ethics Committee of Lapland Central Hospital, Rovaniemi, Finland.
Study Subjects, Baseline Characteristics, and Outcome Measurements
The study subjects consisted of those T2D patients, who attended a T2D follow-up visit at the Health Center between March 1, 2016 and February 28, 2017, whose baseline care plans were drawn up between 2013 and 2015, and for whose updated care plans statistics had been compiled by health care professionals. No other inclusion or exclusion criteria were followed. If the same patient had more than one care plan, the earliest dated was considered to be the baseline care plan, and the latest dated the updated one. Data on clinical outcomes were collected both at baseline and during the follow-up study. No extra visits were organized for the purpose of this study. The protocol did not include standardization of the format of the care plans.
Data on age, sex, number of prescribed regular medications, and history of treatment for mental illness were collected from patient records. The number of medications and the use of insulin treatment were obtained from the medication list in the patient record. A patient was classified as having been treated for mental illness or addiction if their record documented contact with an appropriate clinic. The presence of vascular disease (coronary heart disease, peripheral vascular disease, previous stroke) and the number of years since T2D diagnosis were evaluated from the presence of relevant International Classification of Disease–10th Revision (ICD-10) codes or free text entries in patient records, respectively.
Clinical outcome data (HbA1c, LDL, BP, and BMI) were retrieved from patient records of the baseline and control visits. Changes in each of these variables were calculated by subtracting the baseline from the follow-up value. If available, the subjects’ current smoking status and the number of cigarettes smoked daily were gained from patient records. Those who reported smoking at least 1 cigarette per day, were categorized as smokers. Data on height and body weight were obtained if they were present in the patient record. The BMI was calculated as the weight (in kilograms) divided by the square of the height (in meters). Data on BP was also collected from patient records. As recommended by guidelines, BP was self-measured. The mean of 4 days’ double measurements was documented in patient records.19 If self-measured data were not available, the BP was measured by the health care professional during the routine visits.
Biochemical measurements for patients treated at the Rovaniemi Health Center are performed in a NordLab laboratory according to national quality standards. Each subject’s HbA1c level was quantitatively determined in whole blood samples using an Alere Afinion in vitro diagnostic test (Abbott, Abbott Park, IL, USA). Venous blood samples were drawn after overnight fast and LDL levels were measured using a homogeneous enzymatic colorimetric assay for LDLC3 (Roche/Hitatchi, Basel, Switzerland).
The study protocol specified the following clinical treatment targets: HbA1c < 53mmol/mol, LDL < 2.5 mmol/L, and sBP < 135 mm Hg.1 Total number of achieved targets (0, 1, 2, or 3) were calculated as the sum of aforementioned treatment targets at baseline and follow-up.
Statistical Methods
Clinical outcome measures were presented as mean and standard deviation (SD), categorical variables as proportions. The normality of the variables was tested with the Kolmogorov-Smirnov test. A paired t test was used to evaluate the difference between mean values at baseline and follow-up for HbA1c, LDL, BP, and BMI. The 2-sample t test (also called independent-samples t test) was used to compare the mean values of 2 groups. Where appropriate, a nonparametric test (Mann-Whitney U test) was used. Statistical analyses were performed using IBM SPSS Statistics for Macintosh, Version 24.0 (Release 2016; IBM Corp, Armonk, NY). A P value <.05 was considered statistically significant.
Results
Baseline characteristics of the study population (n = 447) with T2D are presented in Table 1. The mean age was 66.9 years (SD 10.1) and 58.8% were male. The number of medications for T2D was 7.4 (SD 3.0), and 17% of the study population used insulin. The mean (SD) duration of follow-up was 14.4 (SD 6.2) months.
Table 1.
Baseline Characteristics of the Study Population.
| Variable | All | Male | Female |
|---|---|---|---|
| Patients, % (n) | 100 (447) | 58.8 (263) | 41.2 (184) |
| Age (years), mean (SD) | 66.9 (10.1) | 65.7 (9.8) | 68.5 (10.4) |
| Number of prescribed regular medication, mean (SD) | 7.4 (3.0) | 7.4 (2.9) | 7.6 (3.0) |
| Smoking,(% (n) | 15.4 (69) | 17.5 (46) | 12.5 (23) |
| Vascular disease, % (n) | 33.1 (148) | 39.2 (103) | 24.5 (45) |
| Contact for treatment of mental health or substance abuse, % (n) | 19.4 (87) | 15.6 (41) | 25.0 (46) |
| T2D duration over 3 years, % (n) | 72.0 (322) | 73.0 (192) | 70.6 (130) |
| Insulin treatment, % (n) | 17.0 (76) | 17.9 (47) | 15.8 (29) |
Abbreviation: T2D, type 2 diabetes.
Table 2 presents the HbA1c, LDL, BP, and BMI values at baseline and corresponding changes between baseline and follow-up stratified by sex. At baseline, the mean LDL was 2.6 mmol/L (SD 1.0) and the mean sBP was 135.2 mm Hg (SD 14.6). The mean BMI among males was 30.7 kg/m2 (SD 5.1) and among females 31.4 kg/m2 (SD 6.2). Statistically significant decreases in LDL, sBP, and BMI were observed in the whole study population and in both sexes (P < .05 for all) (Table 2).
Table 2.
Anthropometric and Biochemical Measurements at Baseline and Corresponding Changes During 14-Month (SD 6.2) Follow-up, Stratified by Sex.
| Variable | Baseline, Mean (SD) | Change, Mean (SD) | P a |
|---|---|---|---|
| All | |||
| HbA1c, mmol/mol | 50.5 (12.3) | −0.8 (9.6) | .07 |
| LDL, mmol/L | 2.6 (1.0) | −0.2 (0.8) | <.05 |
| sBP, mm Hg | 135.2 (14.6) | −2.2 (13.9) | <.05 |
| dBP, mm Hg | 78.2 (8.9) | −1.5 (7.8) | <.05 |
| BMI, kg/m2 | 31.0 (5.5) | −0.5 (1.5) | <.05 |
| Males | |||
| HbA1c, mmol/mol | 50.7 (12.2) | −0.8 (9.1) | .14 |
| LDL, mmol/L | 2.5 (0.9) | −0.2 (0.7) | <.05 |
| sBP, mm Hg | 135.3 (14.5) | −2.1 (13.1) | <.05 |
| dBP, mm Hg | 79.0 (9.0) | −1.9 (7.8) | <.05 |
| BMI, kg/m2 | 30.7 (5.1) | −0.5 (1.4) | <.05 |
| Females | |||
| HbA1c, mmol/mol | 50.3 (12.4) | −0.8 (10.3) | .30 |
| LDL, mmol/L | 2.8 (1.0) | −0.2 (0.7) | <.05 |
| sBP, mm Hg | 135.0 (14.7) | −2.3 (14.9) | <.05 |
| dBP, mm Hg | 77.0 (8.6) | −0.9 (7.8) | .10 |
| BMI, kg/m2 | 31.4 (6.2) | −0.4 (1.6) | <.05 |
Abbreviations: HbA1c, glycosylated hemoglobin A1; sBP, systolic blood pressure; dBP, diastolic blood pressure; LDL, low-density lipoprotein; BMI, body mass index.
P from independent-samples t test.
The study population was divided into subgroups according to the T2D duration at baseline (<3 years or ≥3 years) (Table 3). The subgroup with T2D duration <3 years had higher LDL values at baseline and the change in LDL was significantly greater than that seen in the subgroup with T2D duration ≥3 years (both Ps < .05). However, at baseline the mean HbA1c was higher in patients with T2D duration ≥3 years than in those with duration <3 years (P < .05). There was a significant decrease in LDL and BMI in both subgroups (P < .05), and in BP in patients with T2D duration ≥3 years (P < .05). The decrease in HbA1c was 0.8 mmol/mol (P = .07).
Table 3.
Anthropometric and Biochemical Measurements at Baseline and Change During Follow-up Stratified by Duration of T2D at Baseline (<3 Years or ≥3 Years).
| Variable | Baseline, Mean (SD) | Change, Mean (SD) | P |
|---|---|---|---|
| T2D <3 years | |||
| HbA1c, mmol/mol | 46.3 (10.1) | −1.0 (11.0) | .36 |
| LDL, mmol/L | 2.8 (1.0) | −0.3 (1.0) | <.05 |
| sBP, mm Hg | 135.9 (15.5) | −2.6 (13.5) | .06 |
| dBP, mm Hg | 79.2 (9.5) | −1.0 (8.3) | .23 |
| BMI, kg/m2 | 31.0 (5.1) | −0.6 (1.7) | <.05 |
| T2D ≥3 years | |||
| HbA1c, mmol/mol | 52.0 (12.6) | −0.8 (9.1) | .14 |
| LDL, mmol/L | 2.6 (1.2) | −0.1 (1.1) | <.05 |
| sBP, mm Hg | 134.9 (14.3) | −2.0 (14.0) | <.05 |
| dBP, mm Hg | 77.7 (8.5) | −1.7 (7.5) | <.05 |
| BMI, kg/m2 | 31.0 (5.7) | −0.5 (1.4) | <.05 |
Abbreviations: HbA1c, glycosylated hemoglobin A1; sBP, systolic blood pressure; dBP, diastolic blood pressure; LDL, low-density lipoprotein; BMI, body mass index.
P from independent-samples t test.
All 3 laboratory variables from both visits were available from 387 patients (87%, of all study population). At baseline, the proportions of the T2D study participants who met only 0 or 1 target were 31.0%, while this decreased to 25.0% in follow-up (Table 4). Additionally, the proportions of participants who met 2 or 3 targets increased from 69.0% at baseline to 75.0% at follow-up.
Table 4.
Proportions of Patients (n = 387 of 447) Achieving Recommended Treatment Targets: HbA1c < 53 mmol/mol, LDL <2.5 mmol/L, and sBP < 135 mm Hg.
| No. of Achieved Targets | Baseline, % | Follow-up, % |
|---|---|---|
| 0 | 5.4 | 3.6 |
| 1 | 25.6 | 21.4 |
| 2 | 43.2 | 46.8 |
| 3 | 25.8 | 28.2 |
| Total | 100 | 100 |
Discussion
Statement of Principal Findings
Our novel finding was that a population of 447 T2D patients in a real-world primary care setting showed improvements in LDL, BP, and BMI after the implementation of a structured care plan. Furthermore, the proportions of patients reaching the recommended treatment targets according to European standards increased after the introduction of the care plan.
Findings in Relation to Other Studies
Previous studies have examined the role of patient-centric working methods in the primary care setting in relation to cardiovascular risk factors.8,10-13,15,16,20 However, our study differs in that the written care plans were drawn up as part of the patients’ routine clinical care; no study-specific interventions or resources were used. Our mean follow-up duration of 14 months was slightly longer than those of earlier studies with 6 months11,20 and 12 months8,10,12-14 of follow-up, and our study population was larger than those of previous studies.8,11-16 In general, care plan–related working methods have been associated with improvements in HbA1c levels according to Cochrane review2; however, some of its original trials showed statistically significant improvement in HbA1c levels,8,11,13,14,20 whereas others did not.10,12,16 We detected a nonsignificant decrease in HbA1c levels. These slight varieties may be due to the heterogeneity in study samples, interventions, follow-up times, baseline HbA1c levels, and confounding factors. Our findings align with those of previous studies that showed improvements in LDL13 and BP levels11,13,15 of T2D patients. Only a few studies,11,12 ours included, have simultaneously examined HbA1c, LDL, BP, and BMI among T2D patients. Ours shows statistically significant improvement in LDL, BP, and BMI levels. Given the variability in methodologies it is impossible to make direct comparisons between the results of different studies. Previous randomized controlled trials have given results of the effect of patient-centric working methods on cardiovascular risk factors,2 but ours demonstrates the benefits of structured care plans in a real-world setting.
Strengths and Weaknesses of the Study
The most important strength of this study is its observational real-world follow-up setting. Additionally, with many of our patients having comorbidities and using multiple medications, the study population reflects what is seen in clinical practice. One limitation is lack of consistency in the contents of the care plans, which is inevitable, since the plans were written by a total of 71 general practitioners and primary care nurses. In addition, the number of confounding factors is unlimited in the real-world studies. Despite on the one hand being a strength, our observational real-world setting can be also seen as a limitation since this design did not allow for a control group. Similarly, the successful introduction of the care plan is a strength in that it improved patient outcomes, but in terms of study design it can be seen as a weakness because its use in all patients meant that no control group was possible for study purposes.
Meaning of the Study
The results of the present study add knowledge about the benefits of care plan in the treatment of T2D patients in observational, longitudinal real-world setting. We believe that the improvements we saw in cardiovascular risk factors were mainly driven by the use of a patient-centric working method2 and patient-reported outcome measures,21 which link with the personalized care plan. In addition, we believe that the care plan can lead to improvements in the quality of care since it acts as a tool for professionals to adapt their knowledge of the guidelines to apply to each individual patient. This, in turn, may improve medication compliance, self-monitoring skills, and knowledge of nonmedical treatments. Shared decision making and personalized target setting are also a prominent part of care planning. Our study indicates that care planning may be a promising tool to improve the clinical outcomes of T2D patients in clinical practice. However, there is an urgent need for benchmarking controlled trials22 to add our knowledge on this issue.
The content of the care plan should be augmented through the continuation of active research. Since some patients benefit from care plans while others appear not to, individual patient outcomes could in future be improved by studies of levels of clinical response to care plans. Therefore, characterizing certain patient groups (ie, patients with mental disorders or multimorbidity) which might benefit most of the care plan would be of high importance. A further follow-up study of the same patient population would also provide additional information on whether the observed improvements in cardiovascular risk factors can be maintained over longer period.
Supplemental Material
Supplemental material, Supplementary_material_example_care_plan_ for Implementation of a Personalized Care Plan for Patients With Type 2 Diabetes Is Associated With Improvements in Clinical Outcomes: An Observational Real-World Study by Anni Vuohijoki, Ilona Mikkola, Jari Jokelainen, Sirkka Keinänen-Kiukaanniemi, Klas Winell, Lucia Frittitta, Markku Timonen and Maria Hagnäs in Journal of Primary Care & Community Health
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Finnish Cultural Foundation, Lapland Regional Fund, and the Finnish Medical Foundation.
ORCID iD: Ilona Mikkola  https://orcid.org/0000-0002-8248-5413
https://orcid.org/0000-0002-8248-5413
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Piepoli MF, Hoes AW, Agewall S, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: the Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J. 2016;37:2315-2381. doi: 10.1093/eurheartj/ehw106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Coulter A, Entwistle VA, Eccles A, Ryan S, Shepperd S, Perera R. Personalised care planning for adults with chronic or long-term health conditions. Cochrane Database Syst Rev. 2015;(3): CD010523. doi: 10.1002/14651858.CD010523.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wagner EH, Austin BT, von Korff M. Organizing care for patients with chronic illness. Milbank Q. 1996;74:511-544. doi: 10.2307/3350391 [DOI] [PubMed] [Google Scholar]
- 4. Vaez K, Diegel-Vacek L, Ryan C, Martyn-Nemeth P. Evaluating diabetes care for patients with serious mental illness using the chronic care model: a pilot study. Health Serv Res Manag Epidemiol. 2017;4:233339281773420. doi: 10.1177/2333392817734206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Care and Support Planning Working Group and Coalition for Collaborative Care. Personalised care and support planning handbook: the journey to person-centred care. https://www.england.nhs.uk/wp-content/uploads/2016/04/core-info-care-support-planning-1.pdf. Accessed November 5, 2018.
- 6. Finland Ministry of Social Affairs and Health. Health Care Act: No. 1326/2010. https://www.finlex.fi/en/laki/kaannokset/2010/en20101326_20131293.pdf. Accessed April 14, 2020.
- 7. Mikkola I, Hagnäs M, Hartsenko J, Kaila M, Winell K. A personalized care plan is positively associated with better clinical outcomes in the care of patients with type 2 diabetes: a cross-sectional real-life study. Can J Diabetes. 2020;44:133-138. doi: 10.1016/j.jcjd.2019.05.003 [DOI] [PubMed] [Google Scholar]
- 8. Naik AD, Palmer N, Petersen NJ, et al. Comparative effectiveness of goal setting in diabetes mellitus group clinics: randomized clinical trial. Arch Intern Med. 2011;171:453-459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Parchman ML, Zeber JE, Palmer RF. Participatory decision making, patient activation, medication adherence, and intermediate clinical outcomes in type 2 diabetes: a STARNet Study. Ann Fam Med. 2010;8:410-417. doi: 10.1370/afm.1161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Glasgow RE, Nutting PA, King DK, et al. Randomized effectiveness trial of a computer-assisted intervention to improve diabetes care. Diabetes Care. 2005;28:33–39. [DOI] [PubMed] [Google Scholar]
- 11. Hiss RG, Armbruster BA, Gillard ML, McClure LA. Nurse care manager collaboration with community-based physicians providing diabetes care a randomized controlled trial. Diabetes Educ. 2007;33:493-502. [DOI] [PubMed] [Google Scholar]
- 12. Frosch DL, Uy V, Ochoa S, Mangione CM. Evaluation of a behavior support intervention for patients with poorly controlled diabetes. Arch Intern Med. 2011;171:2011-2017. [DOI] [PubMed] [Google Scholar]
- 13. Katon WJ, Lin EH, Von Korff M, et al. Collaborative care for patients with depression and chronic illnesses. N Engl J Med. 2010;363:2611-2620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Thom DH, Ghorob A, Hessler D, Vore DD, Chen E, Bodenheimer TA. Impact of peer health coaching on glycemic control in low-income patients with diabetes: a randomized controlled trial. Ann Fam Med. 2013;11:137-144. doi: 10.1370/afm.1443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Liu S, Bi A, Fu D, et al. Effectiveness of using group visit model to support diabetes patient self-management in rural communities of Shanghai: a randomized controlled trial. BMC Public Health. 2012;12:1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Schillinger D, Handley M, Wang F, Hammer H. Effects of self-management support on structure, process, and outcomes among vulnerable patients with diabetes: a three-arm practical clinical trial. Diabetes Care. 2009;32:559-566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kilo CM. A framework for collaborative improvement: lessons from the Institute for Healthcare Improvement’s Breakthrough Series. Qual Manag Health Care. 1998;6:1-13. [DOI] [PubMed] [Google Scholar]
- 18. Komulainen J, Vuokko R, Mäkelä M. Rakenteinen terveys—ja hoitosuunnitelma [in Finnish].http://www.julkari.fi/handle/10024/80180. Accessed October 29, 2019.
- 19. Parati G, Stergiou GS, Asmar R, et al. European Society of Hypertension guidelines for blood pressure monitoring at home: a summary report of the Second International Consensus Conference on Home Blood Pressure Monitoring. J Hypertens. 2008;26:1505-1526. [DOI] [PubMed] [Google Scholar]
- 20. Wolever RQ, Dreusicke M, Fikkan J, et al. Integrative health coaching for patients with type 2 diabetes. Diabetes Educ. 2010;36:629-639. [DOI] [PubMed] [Google Scholar]
- 21. Skovlund SE, Lichtenberg TH, Hessler D, Ejskjaer N. Can the routine use of patient-reported outcome measures improve the delivery of person-centered diabetes care? A review of recent developments and a case study. Curr Diab Rep. 2019;19:84. doi: 10.1007/s11892-019-1190-x [DOI] [PubMed] [Google Scholar]
- 22. Malmivaara A. Benchmarking controlled trial—a novel concept covering all observational effectiveness studies. Ann Med. 2015;47:332-340. doi: 10.3109/07853890.2015.1027255 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplementary_material_example_care_plan_ for Implementation of a Personalized Care Plan for Patients With Type 2 Diabetes Is Associated With Improvements in Clinical Outcomes: An Observational Real-World Study by Anni Vuohijoki, Ilona Mikkola, Jari Jokelainen, Sirkka Keinänen-Kiukaanniemi, Klas Winell, Lucia Frittitta, Markku Timonen and Maria Hagnäs in Journal of Primary Care & Community Health