Abstract
Objective
We retrospectively analyzed the data of 32 hemodialysis patients with COVID-19 to clarify the epidemiological characteristics of this special population.
Method
The data of 32 hemodialysis patients with COVID-19, including epidemiological, demographic, clinical, laboratory, and radiological, were collected from the Blood Purification Department of Wuhan Fourth Hospital from February 3 to 16, 2020.
Results
Of the 32 patients, 23 were male, and the median age was 58 years; the median dialysis vintage was 33 months. Two groups were divided according to the patient’s primary renal disease: group 1 (16 patients with diabetic nephropathy), group 2 (12 patients with primary glomerulonephritis, 2 with obstructive kidney disease, 1 with hypertensive renal damage, and 1 with polycystic kidney). No significant differences were observed between the two groups in epidemiological characteristics, blood cell counts, and radiological performance. Hemodialysis patients are susceptible to COVID-19 at all ages, and patients with diabetes may be a high-risk population (50%). Common symptoms included fever (15 cases), cough (21 cases), and fatigue (7 cases). The blood lymphocyte count decreased in 84.6% of the patients (median: 0.765 × 109/L). Chest CT revealed ground-glass-like lesions in 18 cases, unilateral lung patchiness in 7 cases, bilateral lung patchiness in 7 cases, and pleural effusion in 2 cases.
Conclusion
Only 46.875% of the hemodialysis patients with COVID-19 had fever in the early stage; and diabetics may be the most susceptible population. A decrease in blood lymphocyte count and ground-glass opacity on chest CT scan is beneficial in identifying the high-risk population.
Keywords: Hemodialysis, Coronavirus disease 2019, Clinical features, Blood routine test, Chest CT scan
Introduction
An unknown infectious pneumonia outbreak occurred in Wuhan, Hubei province, China, since December 2019, which were found from the South China seafood market and spread to the entire country. The sequencing of the lower respiratory tract samples of infected patients confirmed that it is a novel type of coronavirus, which was subsequently named as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) by The International Committee on Taxonomy of Viruses (ICTV) [1–4]. Until February 21, 2020, a total of 75,571 individuals were definitely confirmed with coronavirus disease 2019 (COVID-19), and 2239 patients were deceased in China, while a total of 45,346 were confirmed cases and 1684 deaths in Wuhan [5]. Previous studies have shown that the basic reproductive number (R0) of 2019-nCOV is 2.68 [6], indicating that if the government exercises inadequate preventive measures, an outbreak of COVID-19 nationally and globally is inevitable. To effectively control the epidemic, the Chinese government has adopted rapid and comprehensive public health emergency intervention measures, and Hubei province also has adopted comprehensive and severe isolation measures. For the majority of the individuals, the comprehensive control measures did not affect their daily life. However, for hemodialysis patients, concentrated dialysis was required 2–3 times a week to sustain their lives. If patients suspected of COVID-19 infection cannot be identified in time, the risk of large-scale outbreaks of infection or even death is high. An outbreak of COVID-19 has been reported in two hospitals in Beijing, China [7]. The Blood Purification Department in the Gutian district of Wuhan Fourth Hospital, as the first designated unit for hemodialysis patients with COVID-19, received a large number of suspected or confirmed cases. Herein, we analyzed the clinical characteristics, chest imaging, and blood routine test of 32 confirmed cases of hemodialysis patients with COVID-19 to improve the clinicians’ awareness for this specific population.
Methods
-
Patients
In this retrospective study, a total of 32 patients with COVID-19 were diagnosed and collected in the Blood Purification Department of Gutian district of Wuhan Fourth Hospital from February 3 to 16, 2020.
-
Study method
The baseline data of the patients, including demographics, primary renal disease of uremia, whether combined with hypertension or kidney transplantation, dialysis vintage, previous dialysis mode, antihypertensive drug category, onset symptoms, onset pre-exposure history (visit to South China seafood market before the onset of illness), and the results of patient’s blood routine test, chest CT scan, and SARS-CoV-2 RNA real-time reverse transcription-polymerase chain reaction (RT-PCR), were collected through a brief interview between the doctors and patients.
-
Diagnostic criteria
The diagnostic criteria (trial version 5), published online on the National Health and Health Commission’s website on February 4, 2020, for the diagnosis and treatment of novel coronavirus pneumonia were as follows [4]: clinically diagnosed or suspected cases with one of the following etiological evidence, ① real-time fluorescent RT-PCR of respiratory tract or blood specimens was positive for SARS-CoV-2 nucleic acids; ② sequencing of viral genes in the respiratory or blood specimens is highly homologous to known SARS-CoV-2.
Grouping
Two groups were divided according to the patient’s primary renal disease: Group 1 included 16 patients with diabetic nephropathy; Group 2 included 12 patients with primary glomerulonephritis, 1 with hypertensive renal impairment, 2 with obstructive kidney disease, and 1 with polycystic kidney.
History of South China seafood market contact
This refers to the patient who entered the South China seafood market within 2 weeks before the onset of the disease.
Statistical analysis
Continuous variables were described by median, minimum, and maximum values, while percentages were used for categorical variables. The differences between the two groups were compared using rank-sum test. The statistical software package R version 3.6.0 was employed for analysis. Plots were constructed using GraphPad PRISM8 and Photoshop version 6.0.
Results
Analysis of epidemiological characteristics
A total of 32 hemodialysis patients diagnosed with COVID-19 were admitted to our Dialysis Center from February 3 to 16, 2020. Any significant difference was not detected in the epidemiological data among the two groups (Table 1). The youngest patient was 36 years old and the oldest was 83 years old, among them, 19 (59.375%) were between 36 and 60 years old, and 13 (40.625%) over 60 years old. The majority of the patients were male (23 cases, 71.875%). The longest dialysis vintage was 170 months, and the shortest was only 1 month. All the selected patients also presented hypertension. Two patients with primary glomerulonephritis had kidney transplantation before, and over 50% of the patients were treated with antihypertensive drugs, such as angiotensin-converting enzyme inhibitor (ACEI) or angiotensin receptor blocker (ARB). Group 1 had 2 patients with a history of exposure to South China seafood market within 2 weeks before the onset, while other patients did not have a similar history within 2 weeks before the onset of illness.
Table 1.
Demographic and clinical characteristics of the patients at baseline
| Characteristics | Total (N = 32) | Diabetes (N = 16) | Non-diabetes (N = 16) | P value |
|---|---|---|---|---|
| Dialysis vintage, median (range)-month | 33.5 (1–170) | 29.5 (3–125) | 39 (1–170) | 0.256 |
| Male sex-no., % | 0.694 | |||
| Male | 23 (71.9%) | 12 (75.0%) | 11 (68.8%) | |
| Age, median (range)-years | 58.5 (36–83) | 64.5 (41–83) | 56.5 (36–77) | 0.059 |
| Age groups-no., % | 0.072 | |||
| 30–60 years old | 19 (59.4%) | 7 (43.8%) | 12 (75.0%) | |
| ≥ 61 years old | 13 (40.6%) | 9 (56.2%) | 4 (25.0%) | |
| Kidney transplant-no., % | 2 (6.25%) | 0 (0.0%) | 2 (12.5%) | 0.144 |
| Hypertension-no., % | 32 (100%) | 16 (100%) | 16 (100%) | 1 |
| Use of ARB Antihypertensive drugs-no., % | 11 (34.375%) | 4 (25.0%) | 7 (43.8%) | 0.264 |
| Use of ACEI antihypertensive drugs-no., % | 15 (46.875%) | 6 (37.5%) | 9 (56.2%) | 0.288 |
| Huanan seafood wholesale market exposure-no., % | 2 (6.25%) | 2 (12.5%) | 0 (0.0%) | 0.144 |
| Signs and symptoms at admission | ||||
| Asymptomatic | 2 (6.25%) | 2 (12.5%) | 0 | 0.088 |
| Fever | 15 (46.875%) | 6 (37.5%) | 9 (56.25%) | 0.286 |
| Cough | 21 (65.625%) | 11 (68.75%) | 10 (62.5%) | 0.71 |
| Gasping | 2 (6.25%) | 1 (6.25%) | 1 (6.25) | 1 |
| Fatigue | 7 (21.875%) | 3 (18.75%) | 4 (25%) | 0.669 |
| Inappetence | 3 (9.375%) | 1 (6.25%) | 2 (12.5%) | 0.541 |
| Vomit | 1 (3.125%) | 0 | 1 (6.25%) | 0.234 |
| Diarrhea | 3 (9.375%) | 2 (12.5%) | 1 (6.25%) | 0.541 |
| Nausea | 3 (9.375%) | 2 (12.5%) | 1 (6.25%) | 0.541 |
| Muscular soreness | 2 (6.25%) | 1 (6.25%) | 1 (6.25) | 1 |
ACEI angiotensin-converting enzyme inhibitor, ARB angiotensin receptor blocker
Clinical features
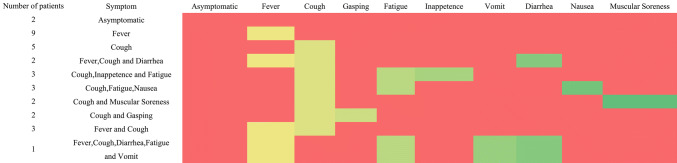
There were no symptoms in 2 of 32 patients, and further diagnosis was confirmed when hs-CRP or blood routine tests detected abnormalities in addition to physical examination. Only 15 (46.875%) patients had a fever, while 37.5% for the diabetic patients. Moreover, over 50% of the patients in the two groups experienced cough discomfort. Other symptoms, such as wheezing, fatigue, loss of appetite, vomiting, diarrhea, nausea, and muscle soreness, were rare (Table 1). Strikingly, 14 patients (43.75%) experienced a single discomfort feature, such as fever or cough, while the remaining 16 patients (50%) had 2 or more discomfort symptoms (Fig. 1).
Fig. 1.
Horizontal representation of symptoms of patients. Red indicates the patient does not have the symptom
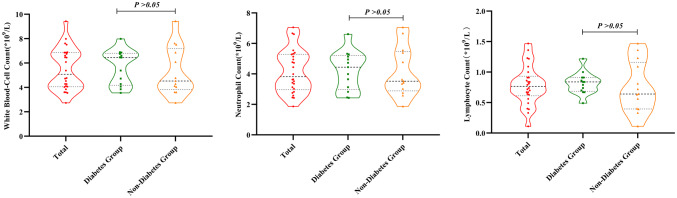
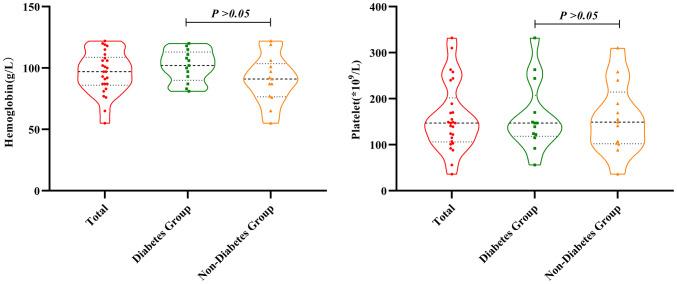
Blood routine test and chest CT scan features
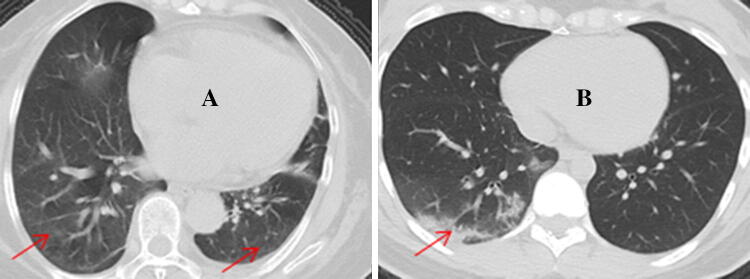
No significant differences were detected in the patient’s white blood cell count, neutrophil count, lymphocyte count, hemoglobin, platelet count, or chest CT scan abnormalities among the two groups (Table 2). The most specific change in 84.6% of the 32 patients in the blood routine test was the decrease in lymphocyte count. This decrease could as low as 10% of the normal value, while leukocyte counts and neutrophils did not show a distinct change, and neutrophil counts increased frequently. The hemoglobin and platelet changes in hemodialysis patients may be different from those of non-dialysis patients due to factors such as insufficient endogenous recombinant human erythropoietin (rHuEPO) production and the use of heparin anticoagulation (Figs. 2, 3). Chest CT scan showed 18 patients (56.25%) with ground-glass opacity in both lungs, 6 patients (18.75%) showed patchy shadowing in both lungs, 7 patients (21.875%) exhibited local patchy shadowing in unilateral lungs, and only 2 patients (6.25%) had pleural effusion (Fig. 4).
Table 2.
Blood routine examination and Chest CT scan findings of hemodialysis patients with COVID-19
| Characteristics | Total (N = 32) | Diabetes (N = 16) | Non-diabetes (N = 16) | P value |
|---|---|---|---|---|
| Blood routine | ||||
| Leucocytes (*109/L), median (range) | 5.08 (2.74–9.43) | 6.45 (3.55–7.99) | 4.53 (2.74–9.43) | 0.6 |
| Normal range | 3.5–9.5 | |||
| Neutrophils (*109/L), median (range) | 3.82 (1.87–7.06) | 4.44 (2.43–6.61) | 3.52 (1.87–7.06) | 0.855 |
| Normal range | 1.8–6.3 | |||
| Lymphocytes (*109/L), median (range) | 0.765 (0.11–1.47) | 0.84 (0.49–1.22) | 0.64 (0.11–1.47) | 0.592 |
| Normal range | 1.1–3.2 | |||
| Hemoglobin (g/L), median (range) | 97 (55–122) | 102 (81–120) | 91 (55–122) | 0.096 |
| Normal range | 130–175 | |||
| Platelets (*109/L), median (range) | 147 (36–332) | 147 (56–332) | 149 (36–310) | 0.89 |
| Normal range | 125–350 | |||
| Chest CT scan findings-no., % | 0.866 | |||
| Ground-glass opacity | 18 (56.25%) | 9 (56.25%) | 9 (56.25%) | |
| Local patchy shadowing | 7 (21.875%) | 3 (18.75%) | 4 (25%) | |
| Bilateral patchy shadowing | 7 (21.875%) | 4 (25%) | 3 (18.75%) |
Covid-19 coronavirus disease 2019
Fig. 2.
Display the count of white blood cell, neutrophils and lymphocytes in three groups. Black dot indicates the actual test value of the patient
Fig. 3.
Display the distribution of Hemoglobin and Platelet among three groups. Black dot indicates the actual test value of the patient
Fig. 4.
a Presents ground-glass opacity in the lower lobes of both lungs, and b presents local patchy shadowing in the right lung of lower lobes
Discussion
Herein, we reported the baseline clinical characteristics of 32 hemodialysis patients with COVID-19 confirmed by the nasopharyngeal test nucleic acid test. We found patients with diabetes accounted for 50%, suggesting that diabetes may be a predisposing factor, whether this is related to the prevalence of diabetic nephropathy in hemodialysis patients remains to be confirmed by large-scale sample study. There were more patients with cough than fever. The blood routine test and chest CT scan showed that lymphocyte count decreased and ground-glass opacity in both lungs has certain specificities.
Coronavirus is an enveloped RNA virus that belongs to the coronaviridae family and order nidovirales, which are widely distributed in humans and other mammals [8]. The six types of coronaviruses that are well known to cause human disease are HCoV-229E, HCoV-OC43, HCoV-NL63, HCoV-HKU1, and SARS-CoV, and MERS-CoV. The first four often cause common cold symptoms, and the latter two can cause fatal zoonotic diseases [9]. As a new type of coronavirus that has just been discovered, transmission mode, pathogenic mechanism, and effective treatment measures of COVID-19 are not yet known. Since February 21, 2020, the data published by the government showed that the number of patients diagnosed or suspected to be infected with COVID-19 in Wuhan reached 45,346, and the number of cumulative death was 1684. The overall prevalence reached 0.453%, and the mortality rate was 3.7% (the total population of Wuhan is calculated as 10 million) [5]. However, according to the data released by the Wuhan Hemodialysis Quality Control Center on February 21, 2020, there were 7203 hemodialysis patients in the city. Up to 626 dialysis patients (8.69%) were found to be suffering from or suspected to be infected with COVID-19, indicating that the infection rate in hemodialysis patients is much higher than that in the general population, a typical example is a single HD center in Renmin Hospital, Wuhan University, 37 HD out 230 HD patients, and 4 of 33 staff members developed COVID-19 infection between 14 January and 17 February 2020 [10]. Nonetheless, the cause of susceptibility in hemodialysis patients is yet unclear. Patients with uremia often have multiple complications such as cardiocerebral vascular disease and diabetes; the superposition of multiple underlying diseases leads to a decrease in resistance, which might be a susceptible factor for patients. Previous studies have shown that the risk of COVID-19 cross-infection in the hospital medical staff reaches 29% as compared to 12.3% for inpatients [11]. Whether the high prevalence of hemodialysis patients is related to nosocomial cross-infection caused by centralized dialysis, there is no relevant data for reference. In addition, some studies have shown that COVID-19 can invade the cells and cause infections in the body via human angiotensin-converting enzyme 2 (ACE2) receptors. Since ACE2 is widely expressed in renal proximal tubule cells in uremia patients, it may also be one of the susceptibility factors for uremia patients [12]. Therefore, timely identification, isolation, and treatment of high-risk groups in dialysis patients, can reduce the risk of nosocomial infections and family cluster infections, as well as the mortality rate of patients. Analysis of the 32 cases in this study showed that there are more male patients than females, which might be attributed to the X chromosome and sex hormones [13].
It was found, in the questionnaire survey of possible infection risk environment exposure of these patients before the onset of the disease, that the majority of patients did not have a history of exposure to the South China seafood market within 2 weeks before the onset of the disease. Since Wuhan is located in a high-risk area, patients may be infected by contact with infected people rather than wild animals. Regarding the clinical symptoms, fever only accounted for 46.875% population, which indicates that it is not a specific manifestation of infection in dialysis patients. However, the number of patients with cough discomfort reached 65.625%, albeit it is not known whether the symptom is related to the decline in the body’s immunity of dialysis patients. Our findings might have been attributable to that in the early stage of the disease, we collected the data of these hemodialysis patients, if we can continuously track the dynamic changes of the patient's examination data or symptoms, maybe this difference will appear. Although the sample size of our study is small, it is similar to the study by Guan et al. [14]. The results of the blood routine test revealed a decline in the lymphocyte count of most patients [14, 15], which was similar to the current findings. This is because, in addition to being targets of coronavirus attacks, the decline in the number of lymphocytes often reflects the severity of the disease [16]. Similar results were also founded by Naicker [17] HD patients with COVID-19 had less lymphopenia, lower serum levels of inflammatory cytokines and milder clinical disease than other patients with COVID-19 infection. The most common change in chest CT scan is the early ground-glass opacity in bilateral lungs, which is also basically consistent with the findings by Guan et al. [14]. Such lesions often indicate the invasion load of the virus and might affect the prognosis.
Importantly, the two patients in our study did not experience fever, cough, and diarrhea, after infection with COVID-19; only the blood lymphocyte count was significantly decreased or hs-CRP level was increased in routine physical examination. The diagnosis was confirmed by the chest CT scan and the nasopharyngeal SARS-CoV-2 nucleic acid test. Such patients are defined as asymptomatic infection, and a large domestic epidemiological study revealed that the proportion of this group is about 1.2% [18]. Asymptomatic infections significantly increase the risk of cluster infections in hospital hemodialysis patients and the difficulty in the identification and prevention of the disease.
The clinical characteristics of the small sample in this study may not be reliable. Nonetheless, we speculated that it is not feasible only to rely on body temperature monitoring as a screening for high-risk populations in the early stage due to the extremely atypical symptoms of hemodialysis patients. Thus, we strongly recommend that if conditions permit, all patients exposed to high-risk environments (such as Wuhan and other epidemic-prone areas) should undergo blood routine test and chest CT scan combined with the patient’s symptoms as a screening for high-risk groups, and if necessary, a nasopharyngeal SARS-CoV-2 nucleic acid test was used to confirm the diagnosis.
Nevertheless, the current study has some limitations. First, we only selected 32 confirmed patients and excluded a large number of suspected cases. Second, during the collection of patients’ epidemiological data, the onset symptoms may change with the course of the disease, and hence, the characteristics of the patient’s actual condition need to be observed and investigated in-depth. Third, while analyzing the clinical examination data of the patients, only the results of blood routine test, chest CT scan, and nasopharyngeal SARS-CoV-2 nucleic acid test could be collected, while the other baseline information could not be obtained.
In summary, the current study found that only 46.875% of hemodialysis patients with COVID-19 infection have fever symptoms in the early stage, and diabetics may be the most susceptible population. Reduced blood lymphocyte counts and ground-glass opacity on chest CT scan can be valuable in identifying the high-risk population.
Acknowledgements
This study was funded by Hubei Province Natural Science Fund 2014CFC1047.
Compliance with ethical standards
Conflict of interest
None to disclose.
Ethical approval
All procedures performed in accordance with the ethical standards of the institutional research committee at which the studies were conducted (IRB approval number KY 2020–007-01 at the ethics committee of Wuhan Fourth Hospital), and this study followed the ethical principles of the Declaration of Helsinki (https://www.wma.net/en/30publications/10policies/b3/index.html).
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Xingguo Du, Email: 928235298@qq.com.
Hua Li, Email: 15327238286@163.com.
Liping Dong, Email: zdhping@sina.com.
Xiaojie Li, Email: 121583642@qq.com.
Ming Tian, Email: patianm@sina.com.
Junwu Dong, Email: junwudong2017@163.com.
References
- 1.Na Z, Dingyu Z, Wenling W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020 doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. 2020;395(10224):e37–e38. doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tan W, Zhao X, Ma X, Wang W, Niu P, Wenbo Xu, et al. A novel coronavirus genome identified in a cluster of pneumonia cases—Wuhan, China 2019–2020. China CDC Wkly. 2020;2(4):61–62. doi: 10.46234/ccdcw2020.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gorbalenya AE, Baker SC, Baric RS, et al. The species Severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. 2020;5:536–544. doi: 10.1038/s41564-020-0695-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.http://www.hxnews.com/news/gn/shxw/202002/21/1862893.shtml. Accessed 21 Feb 2020.
- 6.Wu J, Leung K, Leung G. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet. 2020 doi: 10.1016/S0140-6736(20)30260-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.https://new.qq.com/omn/20200220/20200220A0NXKE00.html. Accessed 12 Mar 2020.
- 8.Richman DD, Whitley RJ, Hayden FG, editors. Clinical virology. 4. Washington: ASM Press; 2016. [Google Scholar]
- 9.Cui J, Li F, Shi ZL. Origin and evolution of pathogenic coronaviruses. Nat Rev Microbiol. 2019;17:181–192. doi: 10.1038/s41579-018-0118-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ma Y, Diao B, Lv X et al. 2019 novel coronavirus disease in hemodialysis (HD) patients: Report from one HD center in Wuhan, China. https://www.medrxiv.org/content/10.1101/2020.0 24.20027201v2. Accessed 02 Mar 2020.
- 11.Wang Dawei Hu, Chang BH, Fangfang Z, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020 doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zou X, Chen K, Zou J, et al. The single-cell RNA-seq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to Wuhan 2019-nCoV infection. Front Med. 2020 doi: 10.1007/s11684-020-0754-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jaillon S, Berthenet K, Garlanda C. Sexual dimorphism in innate immunity. Clin Rev Allergy Immunol. 2019;56:308–321. doi: 10.1007/s12016-017-8648-x. [DOI] [PubMed] [Google Scholar]
- 14.Guan W, Ni Z, Hu Y, Liang W, et al. Clinical characteristics of 2019 novel coronavirus infection in China. medRxiv. 2020 doi: 10.1101/2020.02.06.20020974. [DOI] [Google Scholar]
- 15.Huang C, Wang Y, Li X, et al. Clinical features of patients with 2019 novel coronavirus in Wuhan, China. Lancet. 2020 doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu WJ, Zhao M, Liu K, et al. Tcell immunity of SARSCoV: implications for vaccine development against MERSCoV. Antivir Res. 2017;137:82–92. doi: 10.1016/j.antiviral.2016.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Naicker S, Yang C-W, Coronavirus S-J, et al. Epidemic and Kidneys. Kidney Int. 2019 doi: 10.1016/j.kint.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Epidemiology Working Group for NCIP Epidemic Response, Chinese Center for Disease Control and Prevention The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) Chin J Epidemiol. 2019;2020(41):2. [Google Scholar]